Abstract
Objective
The aim of this study was to use path analysis methods to determine if health literacy mediates the relationship between race and patient activation.
Methods
We performed a secondary analysis of data from a randomized controlled trial in elderly, urban, minority patients using path analysis. Path analysis was used to evaluate the mediation of race on patient activation through different variables. Several models were tested for best fit for their effects on patient activation.
Results
Across all models, significant mediation paths were identified from race to lower patient activation through health literacy. This relationship remained significant throughout alternative model testing for covariate combinations. The best-fit model included an indirect effect of sex on patient activation through health literacy indicating that the mediation effect of health literacy on patient activation was most profound for African American males. Health literacy had a bigger influence on patient activation for participants with a greater comorbidity than for those with fewer conditions. No significant direct effect was shown between race and patient activation in any of the models.
Conclusion
Racial disparities in patient activation were fully mediated by health literacy skills.
Practice implications
Future interventions to improve racial disparities in patient activation need to be targeted at improving health literacy.
Keywords: Path analysis, Patient activation, Health literacy, Health disparities
Introduction
Patient activation is a person’s willingness to manage his or her own health [1]. As patients are required to manage complex medical decisions, the concept of empowering patients for effective self-care has become increasingly acknowledged as a critical goal [2–4]. Studies have shown that being an actively engaged participant in one’s care has been associated with better health outcomes [5]. Higher levels of activation have been associated with healthier behaviors and better health related outcomes whereas lower levels of activation have been associated with worse physical health, depression and anxiety, and readmission within 30 days of hospital discharge [3,6–9]. The concept of activation has important ramifications, as being an effective, informed manager of one’s own health can influence the process and outcomes of care and reduce health care costs [3,10].
Hibbard et al. devised the Patient Activation Measure (PAM) to measure activation, and studies have linked health literacy and patient activation [1,11,12]. Activation involves the empowerment and motivation needed to manage one’s health. Health literacy involves an array of skills needed to promote health, including not only the capacity to derive meaning from written words, numbers, documents, and images, but also, the capacity to fulfill self-care tasks, gather information, and interact successfully in health care contexts [13]. An integral component to being more activated is seeking and using relevant health information [7]. Therefore, being able to understand and process health information becomes important. Both health literacy and patient activation have been found to influence decision making in older adults [4].
Patient activation has been shown to differ by race and ethnicity: African Americans have demonstrated lower levels of patient activation than whites, even after controlling for other characteristics [11]. Activation has been shown to be lower in medically underserved populations [7,14]. The etiology of this relationship between race and activation has not been elucidated. Resolving the gaps in activation has been proposed as one strategy for reducing racial disparities in health outcomes [11].
As health literacy has been linked both to race [15] and patient activation, health literacy may be an important mechanism residing within this causal pathway. Therefore, we performed path analyses to evaluate the direct and indirect relationships between race and patient activation, examining health literacy as a mediator of this relationship [16].
2. Methods
Participant recruitment, data collection procedures and the majority of the measures used in our current analyses have been previously described in the Steps to Health study [16]. Race was categorized into a three-level variable: Black or African–American, White, and Other (including American Indian/Alaskan Native, Asian, multi-racial, and unknown), with White as the referent group. We examined the normality of continuous endogenous variables such as literacy score and PAM by comparing kernel density estimates to ideal normal curves. We also compared the sample means and medians to assess the symmetry of the distributions. We found that these variables were sufficiently distributed for use to model linear relationships.
Health literacy was measured using the short version of the Test of Functional Health Literacy in Adults (S-TOFHLA) [17,18]. This validated test consists of two parts, the first part measures reading comprehension with regards to medical topics. Scores ranged from 0 to 36. We analyzed literacy scores as a continuous variable.
Patient activation was measured using the validated Patient Activation Measure (PAM) and was evaluated during the baseline assessment of the Steps to Health Study [1]. The PAM is a 21-item questionnaire that is scored on a scale of 0–100, 0 = the lowest possible activation and 100 = the highest possible activation [1]. We analyzed PAM scores as a continuous variable in our models.
In order to produce the most parsimonious model both the direct and indirect effects were examined for each of the following covariates: race, age, gender, Patient Health Questionnaire 9 (PHQ9) score for depression and number of comorbidities. Path analysis was performed through maximum likelihood estimation using MPLUS software, version 7.3 [19]. Race was included in the models as an exogenous variable while education, literacy score, and PAM were treated as endogenous variables. We allowed for correlation between education and literacy score. Model fit was evaluated using the chi-square statistic, Akaike Information Criterion (AIC), root mean square error of approximation (RMSEA), and comparative fit index (CFI). Initially, all direct paths were included in the model. At each step of the modeling procedure, paths with p > 0.05 were removed and model fit was evaluated resulting in the final model. Standardized path coefficients are presented.
3. Results
The analytic cohort for these analyses was taken from the Steps to Health Study (n = 263), excluding non-English speakers (n = 15) and, as per scoring guidelines, excluding those who answered “strongly agree” to every question on the PAM questionnaire (n = 25), leaving 225 people included in the analyses. Characteristics of this sample are presented in Table 1. Mean age was 71, 40.9% male, 26.2% White, 67% Black, and 6.7% classified as other race. Approximately forty five percent reported having greater than high school education and forty one percent had low literacy based on the S-TOFHLA. Twenty seven percent had greater than two comorbidities. Compared to Whites, Blacks were more likely to be female (p < 0.001), have completed less than high school regarding education (p = 0.0003) and have lower health literacy (p < 0.001).
Table 1.
Basic demographics of the study population.
| Variable | All N = 225 |
Black/African American N = 151 |
White N = 59 |
Other Race N = 15 |
p-Value | ||
|---|---|---|---|---|---|---|---|
| Gender | N (%) | Male | 92 (40.9) | 48 (31.8) | 38 (64.4) | 6 (40.0) | <0.0001 |
| Female | 133 (59.1) | 103 (68.2) | 21 (35.6) | 9 (60.0) | |||
| Age at enrollment | N | 225 | 151 | 59 | 15 | 0.3694 | |
| Mean (SD) | 71.3 (5.4) | 71.0 (5.5) | 71.9 (5.5) | 71.9 (4.5) | |||
| Median (IQR) | 70.0 (67.0, 75.0) | 70.0 (67.0, 74.0) | 71.0 (67.0, 76.0) | 72.0 (69.0, 74.0) | |||
| Age at enrollment (grouped) | N (%) | 65–69 | 102 (45.3) | 72 (47.7) | 24 (40.7) | 6 (40.0) | 0.9024 |
| 70–74 | 65 (28.9) | 42 (27.8) | 17 (28.8) | 6 (40.0) | |||
| 75–79 | 40 (17.8) | 25 (16.6) | 13 (22.0) | 2 (13.3) | |||
| 80+ | 18 (8.0) | 12 (7.9) | 5 (8.5) | 1 (6.7) | |||
| Highest grade completed | N (%) | <HS | 51 (22.7) | 42 (27.8) | 6 (10.2) | 3 (20.0) | 0.0003 |
| HS or GED | 73 (32.4) | 57 (37.7) | 12 (20.3) | 4 (26.7) | |||
| >HS | 101 (44.9) | 52 (34.4) | 41 (69.5) | 8 (53.3) | |||
| Literacy level | N (%) | Low | 93 (41.3) | 82 (54.3) | 7 (11.9) | 4 (26.7) | <0.0001 |
| High | 132 (58.7) | 69 (45.7) | 52 (88.1) | 11 (73.3) | |||
| Total number of comorbidities | N (%) | [0] None | 97 (43.1) | 60 (39.7) | 32 (54.2) | 5 (33.3) | 0.0715 |
| [1] 1 | 67 (29.8) | 43 (28.5) | 16 (27.1) | 8 (53.3) | |||
| [2] 2+ | 61 (27.1) | 48 (31.8) | 11 (18.6) | 2 (13.3) |
All models included one exogenous variable, racial status (White, Black or other), with three endogenous variables: highest grade achieved, health literacy score, PAM. We found a suggestive association, though not statistically significant, in the bivariate model between race and patient activation (path coefficient −0.129, SE 0.71, p = 0.068). With the addition of literacy score and highest grade achieved, we found significant path coefficients along the indirect pathway from race through literacy score to patient activation, though the direct path from race to patient activation was not significant. Both a significant negative effect between race and highest grade achieved and a significant positive effect between literacy score and highest grade achieved existed in most alternate models tested. These effects were not changed when models were tested with the addition of the covariates of age and PHQ9 score.
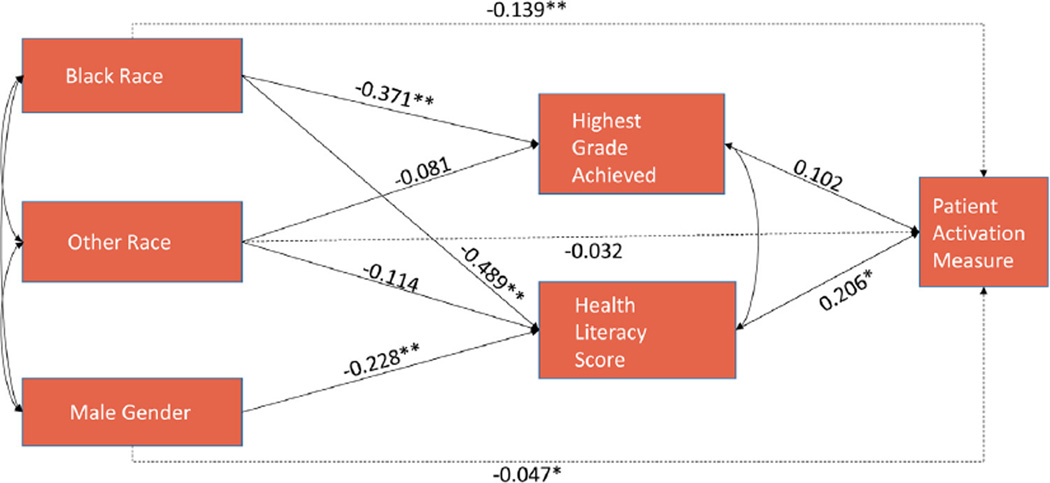
The best fit model included gender as an additional exogenous variable (Fig. 1) (χ2 = 1.801, p = 0.7723). In this model the indirect effect of gender through literacy score to PAM was examined while dropping the direct effect of gender on PAM. The indirect effect of race on literacy score was about two times the effect of gender on literacy score. Furthermore, the effect of literacy score on activation was about two times the effect of grade on activation although the effect of grade on PAM was not statistically significant. The indirect effects for this model are summarized in Table 2. Gender had a significant negative effect with PAM through literacy (indirect effect −0.047, SE = 0.020, p = 0.020). In addition race continued to have a negative indirect association with PAM through literacy score (indirect effect −0.139, SE = 0.036, p < 0.001).
Fig. 1.
Best fit model. Coefficients are standardized path coefficients. For tests of significance of individual paths,*p < 0.01; **p < 0.001. Overall model fit: N = 225, χ2(df = 4) = 1.801, p = 0.7723, RMSEA = 0.000 (95% CI: 0.000,0.068).
Table 2.
Statistics for the indirect effects of the best fit model.
| Path | Indirect effect (SE) | p-value |
|---|---|---|
| Black race through highest grade achieved | −0.038 (0.028) | 0.178 |
| Black race through literacy score | −0.101 (0.038) | 0.008 |
| Sum of indirect effects from black race to PAM | −0.139 (0.036) | <0.001 |
| Other race through highest grade achieved | −0.008 (0.009) | 0.364 |
| Other race through literacy score | −0.024 (0.016) | 0.134 |
| Sum of indirect effects from other race to PAM | −0.032 (0.019) | 0.091 |
| Male gender through literacy score | −0.047 (0.020) | 0.02 |
| Sum of indirect effects male gender to PAM | −0.047 (0.020) | 0.02 |
To assess whether number of comorbidities would be an effect modifier, we stratified our best fit model according to the number of comorbidities, coded into a low category (0–1) and a high category (greater than 2). In the low comorbidity group, literacy no longer had a significant effect on PAM (path coefficient = 0.119, p = 0.18) while in the high comorbidity group, the effect size of literacy score on PAM approximately doubled and remained statistically significant (path coefficient = 0.420, p < 0.001). Other path coefficient sizes and directions were roughly similar between the two comorbidity groups. This suggests that the effect of literacy on PAM may be stronger among patients with two or more comorbidities.
4. Discussion and conclusion
4.1. Discussion
We demonstrated that racial disparities in patient activation are fully mediated by health literacy. Our data suggests that these relationships are particularly important for males and for people with a greater number of comorbidities, as these factors were found to be associated with larger patient activation deficits.
We used path analyses to model complex, multilevel interactions between an array of different variables including race, gender, highest grade achieved, health literacy score, and Patient Activation Measure (PAM). Path analyses have been used to identify important mediators of racial differences in diabetes preventive care, adolescent substance use, attitudes toward mental health treatment, and HIV medication management [20–23]. Path analysis has also been used to deconstruct the social cognitive factors related to racial differences in physical activity [24]. Finally, these methods have been used to confirm that health literacy was a mediator in racial disparities in diabetes-related medication adherence [25]. Given the complex interactions between race, gender, literacy, educational attainment, and patient activation, path analyses are well suited to elucidate any mediators in racial differences in patient activation.
Furthermore, the present study suggests that those with a greater burden of comorbidities are more adversely affected, with respect to patient activation, by lower health literacy than those with less or no comorbidities. One potential explanation for this observation is that with increased burden of illness, one’s role and engagement in personal health becomes more challenging. As one becomes more involved in their health, one needs to have a greater degree of health literacy to navigate the complexities of addressing their complex health. Thus, those who are sicker may not be able to keep up with this demand for greater literacy and thus become less engaged in their own health care.
The concept of patient activation can also be viewed within the broader concept of self-efficacy. Self-efficacy theory asserts that “personal mastery expectations are the primary determinants of behavior change” and are influenced by past experiences and one's history of successes and failures [26]. Although some studies have found no relationship between literacy and self-efficacy, others have shown that levels of health literacy can impact self-efficacy [27,28]. Self-efficacy has been shown to be an independent, direct predictor of health status [13]. Path analysis has been used to show significant links between one’s knowledge and self-efficacy, with health literacy being indirectly related to self-efficacy through knowledge [13]. Self-efficacy has been defined as having an integral role in activation as well as in designing interventions to improve self-management behaviors [1,2].
The concepts of patient activation and self-efficacy are increasingly becoming pertinent to changes within the health care system. Higher levels of activation have been associated with lower health care costs and lower utilization of emergency departments and inpatient admissions [3,10]. Increasing activation may be an effective way of reducing racial and ethnic health disparities. Previous studies have shown that those with higher levels of activation have fewer problems with access to care and that conversely those with lower activation are less likely to engage in health promoting behaviors and to be passive regarding their health [7]. The present study suggests that one method for improving activation would be developing policies and interventions to improve health literacy. Effective health literacy interventions need to be embedded into care delivery structures. For example, a recent study showed that a literacy-sensitive, self-management teaching program led to improvement in patients with Chronic Obstructive Pulmonary Disease (COPD) [29]. Incorporation of disease-specific video and booklet educational media has been demonstrated to improve activation and patients with low health literacy may derive benefit from such interventions [30]. Other studies for such chronic conditions such as diabetes indicate that literacy-targeted interventions improved self-efficacy and outcomes [31,32]. Furthermore, the Affordable Care Act incorporated several new provisions to address health literacy including professional training and streamlining enrollment into Medicaid, the Children’s Health Insurance Program and the insurance exchanges [33].
Our data demonstrate that the mediating influence of health literacy on the relationship between race and patient activation is independent from the influence of educational attainment. As health reforms continue to require patients to be more actively engaged in their own care, removing unnecessary complexities from the health care system and designing a system that is favorable to those of all literacy levels will improve this sense of patient engagement. Higher patient activation has been linked to better clinical outcomes and engagement in healthier behaviors [5,6,9]. For example, higher patient activation has been associated with better medication adherence and glycemic control in diabetic patients [6]. However, all studies to date have been observational; interventions that evaluate if improvement in activation leads to improved outcomes are needed. Furthermore, our findings suggest that future interventions to improve activation risk worsening existing racial disparities if they are not sensitive to the impact of health literacy.
The present study contributes to untangling the complex interaction between number of comorbidities, health literacy and patient activation through the use of path analyses. Limitations of this study include the restricted study population of older, community-dwelling, urban adults who participated in a walking intervention, which limits the generalizability of the results. In addition, the constructs of patient activation and health literacy were each defined in our analyses by a single measurement tool. While this is typical, such an approach is inherently limited and curtailed our capacity to appreciate complexity or nuance within each of these latent traits. Furthermore, while we tested a broad array of relevant variables, unmeasured confounders of these relationships may certainly exist. Finally, our categorization of race within the structure of these analyses certainly does not capture the significant diversity that exists within broad racial categories. Our study was underpowered to undertake a more refined approach. Future work is needed to further identify people who are most at risk of having low activation, the clinical sequelae that result, and methods upon which to intervene.
4.2. Conclusion
The relationship between African American race and lower patient activation was fully mediated by health literacy. Path analysis can be a useful tool in restructuring and refining conceptual frameworks. Future interventions to improve racial disparities in patient activation should include elements targeted at improving health literacy and removing complexity from health systems.
4.3. Practice implications
As consumers are increasingly being required to become more involved in their health care, interventions to improve activation are needed. Health literacy is an important target to mitigate racial disparities in patient activation.
Acknowledgments
This study was supported by 1R01HL116630-01A1 (Paasche-Orlow, Wolf) NHLBI, Refining Conceptual Models for the Role of Health Literacy in Health Outcomes. The funder had no role in the data analysis or interpretation of the data.
Footnotes
Conflict of interest
None.
References
- 1.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv. Res. 2004 Aug;39(4 Pt. 1):1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002 Nov;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 3.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J. Gen. Intern. Med. 2012 May;27(5):520–526. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greene J, Hibbard JH, Tusler M. How Much Do Health Literacy and Patient Activation Contribute to Older Adults’ Ability to Manage Their Health? Washington, DC: AARP Public Policy Institute; 2005. [Google Scholar]
- 5.Mosen DM, Schmittdiel J, Hibbard J, Sobel D, Remmers C, Bellows J. Is patient activation associated with outcomes of care for adults with chronic conditions? J. Ambul. Care Manage. 2007;30(1):21–29. doi: 10.1097/00004479-200701000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann. Fam. Med. 2010 Sep-Oct;8(5):410–417. doi: 10.1370/afm.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care and why does it matter? Washington DC: Research Brief, Center for Health Systems Change; 2008. [October 2008]. Report No.: 8. [PubMed] [Google Scholar]
- 8.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv. Res. 2007;42(4):1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff. (Millwood) 2013 Feb;32(2):207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 10.Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients’ ‘scores’. Health Aff. (Millwood) 2013 Feb;32(2):216–222. doi: 10.1377/hlthaff.2012.1064. [DOI] [PubMed] [Google Scholar]
- 11.Hibbard JH, Greene J, Becker ER, Roblin D, Painter MW, Perez DJ, et al. Racial/ethnic disparities and consumer activation in health. [09/01];Health Aff. 2008 27(5):1442–1453. doi: 10.1377/hlthaff.27.5.1442. [DOI] [PubMed] [Google Scholar]
- 12.Smith SG, Curtis LM, Wardle J, von Wagner C, Wolf MS. Skill set or mind set? Associations between health literacy, patient activation and health. PLoS One. 2013;8(9):e74373. doi: 10.1371/journal.pone.0074373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osborn CY, Paasche-Orlow MK, Bailey SC, Wolf MS. The mechanisms linking health literacy to behavior and health status. Am. J. Health Behav. 2011 Jan-Feb;35(1):118–128. doi: 10.5993/ajhb.35.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lubetkin EI, Lu WH, Gold MR. Levels and correlates of patient activation in health center settings: building strategies for improving health outcomes. J. Health Care Poor Underserved. 2010 Aug;21(3):796–808. doi: 10.1353/hpu.0.0350. [DOI] [PubMed] [Google Scholar]
- 15.Kutner M, Greenburg E, Jin Y, Paulsen C. The health literacy of america's adults: results from the 2003 national assessment of adult literacy, NCES 2006-483. Washington DC: National Center for Education Statistics; 2006. [September 2006]. Report No.: NCES 2006-483. [Google Scholar]
- 16.Bickmore TW, Silliman RA, Nelson K, Cheng DM, Winter M, Henault L, et al. A randomized controlled trial of an automated exercise coach for older adults. J. Am. Geriatr. Soc. 2013 Oct;61(10):1676–1683. doi: 10.1111/jgs.12449. [DOI] [PubMed] [Google Scholar]
- 17.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J. Gen. Intern. Med. 1995 Oct;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 18.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ. Couns. 1999 Sep;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 19.Muthén L, Muthén B. Mplus User’s Guide. 7th. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 20.Pu J, Chewning B. Racial difference in diabetes preventive care. Res. Soc. Adm. Pharm. 2013 Nov-Dec;9(6):790–796. doi: 10.1016/j.sapharm.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Shih RA, Miles JN, Tucker JS, Zhou AJ, D’Amico EJ. Racial/ethnic differences in adolescent substance use: mediation by individual, family, and school factors. J. Stud. Alcohol Drugs. 2010 Sep;71(5):640–651. doi: 10.15288/jsad.2010.71.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Conner KO, Koeske G, Brown C. Racial differences in attitudes toward professional mental health treatment: the mediating effect of stigma. J. Gerontol. Soc. Work. 2009 Oct;52(7):695–712. doi: 10.1080/01634370902914372. [DOI] [PubMed] [Google Scholar]
- 23.Waldrop-Valverde D, Osborn CY, Rodriguez A, Rothman RL, Kumar M, Jones DL. Numeracy skills explain racial differences in HIV medication management. AIDS Behav. 2010 Aug;14(4):799–806. doi: 10.1007/s10461-009-9604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rogers LQ, McAuley E, Courneya KS, Humphries MC, Gutin B. Racial differences in physical activity associations among primary care patients. Ethn. Dis. 2007 Autumn;17(4):629–635. [PubMed] [Google Scholar]
- 25.Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL, et al. Health literacy explains racial disparities in diabetes medication adherence. J. Health Commun. 2011;16(Suppl 3):268–278. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The self efficacy scale: construction and validation T. Psychol. Rep. 1982;51(2):663–671. 10/01; 2015/02. [Google Scholar]
- 27.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am. J. Health Behav. 2007 Sep-Oct;31(Suppl. 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 28.DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. Am. J. Health Behav. 2007 Sep-Oct;31(Suppl. 1):S27–S35. doi: 10.5555/ajhb.2007.31.supp.S27. [DOI] [PubMed] [Google Scholar]
- 29.Kiser K, Jonas D, Warner Z, Scanlon K, Shilliday BB, DeWalt DA. A randomized controlled trial of a literacy-sensitive self-management intervention for chronic obstructive pulmonary disease patients. J. Gen. Internal Med. 2012;27(2):190–195. doi: 10.1007/s11606-011-1867-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eckman MH, Wise R, Leonard AC, Dixon E, Burrows C, Khan F, et al. Impact of health literacy on outcomes and effectiveness of an educational intervention in patients with chronic diseases. Patient Educ. Couns. 2012;87(2):143–151. doi: 10.1016/j.pec.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 31.Cavanaugh K, Wallston KA, Gebretsadik T, Shintani A, Huizinga MM, Davis D, et al. Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care. 2009 Dec;32(12):2149–2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kandula NR, Nsiah-Kumi PA, Makoul G, Sager J, Zei CP, Glass S, et al. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Educ. Couns. 2009;75(3):321–327. doi: 10.1016/j.pec.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Somers S, Mahadevan R. Health Literacy Implications for Health Care Reform: Workshop Summary. Washington, D.C: National Academies Press; 2011. Health literacy implications of the affordable care act, Institute of Medicine; pp. 69–100. [Google Scholar]