Abstract
Alteration in self-perception is a salient feature in major depression. Hyperactivity of anterior cortical midline regions has been implicated in this phenomenon in depressed adults. Here, we extend this work to depressed adolescents during a developmental time when neuronal circuitry underlying the sense of self matures by using task-based functional magnetic resonance imaging (fMRI) and connectivity analyses. Twenty-three depressed adolescents and 18 healthy controls (HC) viewed positive and negative trait words in a scanner and judged whether each word described them (‘self’ condition) or was a good trait to have (‘general’ condition). Self-perception scores were based on participants’ endorsements of positive and negative traits during the fMRI task. Depressed adolescents exhibited more negative self-perceptions than HC. Both groups activated cortical midline regions in response to self-judgments compared to general-judgments. However, depressed adolescents recruited the posterior cingulate cortex/precuneus more for positive self-judgments. Additionally, local connectivity of the dorsal medial prefrontal cortex was reduced during self-reflection in depressed adolescents. Our findings highlight differences in self-referential processing network function between depressed and healthy adolescents and support the need for further investigation of brain mechanisms associated with the self, as they may be paramount to understanding the etiology and development of major depressive disorder.
Keywords: Self-esteem, Adolescence, Depression, Medial prefrontal cortex, Default mode network
1. Introduction
Adolescence is a sensitive period of development characterized in part by maturation of neuronal circuitry related to emotional processing and the sense of self (Giedd, 2004, Sebastian et al., 2008). It is during this stage that many psychiatric conditions first emerge, including major depressive disorder (MDD), an illness characterized by feelings of worthlessness and low self-esteem (Manani and Sharma, 2013, Wilburn and Smith, 2005). Adolescent MDD is a major public health concern, associated with severe consequences including suicide, the second leading cause of death in this age group (Perou et al., 2013). Relatedly, longstanding evidence suggests low self-esteem is linked to suicidal behavior (Lewinsohn et al., 1994, Manani and Sharma, 2013, McGee and Williams, 2000, Mitsui et al., 2014, Overholser et al., 1995, Wilburn and Smith, 2005). Thus, research that targets brain mechanisms associated with self-referential processing in depressed adolescents is paramount to understanding the etiology and development of the disorder.
It has been suggested that regions within the ‘default mode network’ (DMN) are active in the resting brain when thoughts are often introspective and self-reflective but are typically deactivated during more goal-directed tasks (Andrews-Hanna et al., 2010, Raichle et al., 2001). However, this is still a topic of active investigation as the existence of a passive state of brain function and its interaction with task-positive networks is not fully understood. The DMN includes cortical midline structures, such as the medial prefrontal cortex (MPFC), anterior cingulate cortex (ACC), posterior cingulate cortex (PCC), and precuneus, as well as the inferior parietal cortex, lateral temporal cortex, and hippocampus (Andrews-Hanna et al., 2010, Buckner et al., 2008). While regions within this network have been associated with several cognitive domains such as the memory and attention systems, among others (Broyd et al., 2009, Buckner et al., 2008), recent work has implicated the DMN in affective cognition due to its connections with brain regions involved in emotion and salience, such as the amygdala and insula (Ho et al., 2014a, Sambataro et al., 2013, Uddin, 2015). For example, the midline core (i.e. MPFC, ACC, PCC, precuneus) has been shown to be activated during self-referential processing in both healthy adults (Andrews-Hanna et al., 2010, Denny et al., 2012, Kelley et al., 2002, Lemogne et al., 2012, Northoff et al., 2006) and adolescents (Pfeifer et al., 2007, Pfeifer et al., 2009). Alterations in these regions may consequently underlie self-referential processing deficits that manifest as low self-esteem and feelings of worthlessness in affective disorders (Ho et al., 2014a).
Currently, studies investigating self-referential processing deficits in depression have focused on adults. Findings appear conflicting, with reports of both increased (Lemogne et al., 2009, Lemogne et al., 2010, Yoshimura et al., 2010) and decreased (Grimm et al., 2009, Johnson et al., 2009) activation of the MPFC during self-reflection (Nejad et al., 2013). One theory postulates that hyperactivity of anterior cortical midline regions during negative self-reflection contributes to ruminations about the self in depression (Lemogne et al., 2009, Lemogne et al., 2010, Lemogne et al., 2012, Yoshimura et al., 2010, Yoshimura et al., 2014). For example, Yoshimura et al. (2010) found that negative thoughts in particular increased activity in the dorsal medial prefrontal cortex (dMPFC) and ventral ACC in depressed adults compared to healthy controls, whereas activity in these areas was similar in both groups for positive self-thoughts (Yoshimura et al., 2010). Johnson et al. (2009) similarly found that the dMPFC was activated in healthy controls and depressed adults in response to positive thoughts like personal hopes and dreams. However, depressed adults showed less deactivation (higher signal) of this region when prompted to have non-self-referential thoughts, suggesting depressed individuals may have difficulty disengaging from negative self-focused ruminations. An alternate theory proposes that cortical midline regions are not necessarily hyperactivated during active self-reflection in depressed adults, but rather that resting-state activity in these regions is abnormally increased (Greicius et al., 2007), which leads to reduced signal changes in these regions during self-reflection tasks and appears as hyperactivity (Grimm et al., 2009, Northoff et al., 2011).
While studies of depressed adults have begun to tease apart the brain regions involved in self-reflection and negative rumination, few have investigated the connectivity of these regions to better understand self-referential processing network function. Task-dependent functional connectivity analyses may help clarify the relationships between regions within this network. Only two studies to date have specifically examined task-dependent connectivity between cortical midline structures during self-referential processing in MDD, and both were also in adults. Lemogne et al. (2009) found increased connectivity between the posterior cingulate cortex and anterior regions of the DMN, including the dMPFC and ACC in depressed patients, while Yoshimura et al. (2010) found increased connectivity between the ACC, MPFC, and amygdala. One caveat of both studies was that patients were treated with psychotropic medications.
Based on the above observations, the current study extends this line of work and examines self-referential processing in psychotropic medication-free adolescents with depression, as well as task-dependent connectivity of cortical midline regions within the DMN during self-referential thought. We hypothesized that adolescents with MDD would exhibit more negative self-perceptions compared to healthy controls—scores that were based on participants’ endorsement and rejection of positive and negative trait words in the scanner. Additionally, we predicted depressed adolescents would show increased activity and connectivity of cortical midlines regions (e.g., MPFC, ACC, PCC, precuneus), similarly to depressed adults (Lemogne et al., 2009, Lemogne et al., 2010, Lemogne et al., 2012, Yoshimura et al., 2010, Yoshimura et al., 2014). Furthermore, we expected neural activity and connectivity in these regions to negatively correlate with self-esteem scores.
2. Material and methods
2.1. Participants
The sample consisted of 23 adolescents with MDD and 18 healthy controls (HC), all right-handed and group matched on age and sex. Six individuals were excluded from all fMRI analyses, 5 for excessive motion and 1 for image distortion. The final imaging sample consisted of 20 adolescents with MDD and 15 HC. Depressed adolescents were recruited from the New York University (NYU) Child Study Center, the Bellevue Hospital Center Department of Psychiatry, and through local advertisements. Healthy controls were recruited through local advertisements. An Institutional Review Board (IRB) approved the study, and written informed consent was obtained from participants age 18 and older; those under age 18 provided signed assent and a parent provided signed informed consent.
Participants ranged in age from 12 to 20 years old and did not present with any significant medical or neurological conditions. Participants were screened for pubertal stage using the Tanner Scale (Tanner, 1962) and were all required to be at least a 4. Exclusion criteria included a low IQ (<80), MRI contraindications, a positive urine toxicology test, or a positive pregnancy test in women. Depressed adolescents met the Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision (DSM-IV-TR) criteria for diagnosis of MDD, with a current episode of at least 8 weeks in duration, and a minimum raw score of 36 on the Children's Depression Rating Scale-Revised [CDRS-R; Poznanski et al., 1985]. All participants were free of psychotropic medication for at least seven half-lives of the drug. Furthermore, adolescents with MDD could not have a current diagnosis of post-traumatic stress disorder or an eating disorder, or a current or past DSM-IV-TR diagnosis of bipolar disorder, schizophrenia, pervasive developmental disorder, panic disorder, obsessive-compulsive disorder, conduct disorder, Tourette's disorder, or a substance-related disorder in the past year. Healthy control adolescents did not meet the criteria for any current or past DSM-IV-TR diagnosis and were psychotropic medication-naïve.
2.2. Clinical assessments
A board-certified child/adolescent psychiatrist or clinical psychologist performed psychiatric assessments using the Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present and Lifetime Version [KSADS-PL; Kaufman et al., 1997], a semi-structured interview conducted with both the participant and their parents. Depression severity was assessed using the self-rated Beck Depression Inventory-Second Edition [BDI-II; Beck et al., 1997] and the clinician-rated CDRS-R. Anxiety was assessed using the Multidimensional Anxiety Scale for Children, while suicidality was quantified using the Beck Scale for Suicidal Ideation [BSSI; Beck et al., 1979]. Lastly, IQ was estimated using the Kaufman Brief Intelligence Test (Kaufman and Kaufman, 1990).
2.3. Word task
Similar to past research (Fossati et al., 2003, Yoshimura et al., 2009, Yoshimura et al., 2010, Yoshimura et al., 2014), participants were presented with positive or negative trait adjectives (e.g., positive = calm, intelligent, likeable, kind; negative = obnoxious, messy, greedy, dumb) and had to answer one of three questions: (1) general-judgments (“Is this a good trait?”); (2) self-judgments (“Does this describe you?”); (3) letter-judgments (“Is there a letter E?”). Positive and negative trait valences were experimenter assigned. Each trial began with the presentation of a 500 ms fixation cross, followed by a trait adjective for 3500 ms, and a 500 ms intertrial interval (ITI). Participants made “yes” or “no” responses during the 3500 ms presentation of the trait using a button box. Two runs were completed, each beginning and ending with 24 s of fixation, and consisting of 6 blocks, 2 blocks of each type of judgment (i.e., general, self, letter). For each block, the participant first viewed instructions for 4 s, followed by the pseudo-random intermixed presentation of 5 positive adjectives, 5 negative adjectives, and 5 catch-trials. The catch-trials were presentations of a blank screen for the same length of time as the word trials (3500 ms) and were included to increase jitter. The trait adjectives were randomly selected without replacement. Overall, subjects saw 40 trait adjectives (20 positive and 20 negative) for each of the 3 types of judgments (i.e., general, self, letter).
2.4. Behavioral analyses
A measure of positive perception was calculated for both self- and general-judgments by averaging the percentage of “yes” responses to positive traits (out of 20 positive traits) and “no” responses to negative traits (out of 20 negative traits). Similarly, a measure of negative perception was calculated by averaging the percentage of “no” responses to positive traits and “yes” responses to negative traits. Self-judgment scores were used as a measure of self-esteem, while general-judgment scores indicated the accuracy of participants’ identification of traits as negative or positive compared to the labeling of the words and thus assessed their more global perception of personality traits. Demographic, clinical, and behavioral data were evaluated for normality and outliers. When parametric assumptions were not reasonably met, non-parametric analogs were used. Self- and general-judgment trait ratings and response times were each submitted to 2 (group: MDD, HC) × 2 (category: self, general) × 2 (valence: positive, negative) mixed model ANCOVAs, controlling for age and gender. Valence of the traits in the ANCOVA model was experimenter assigned and not based on how participants endorsed the words. Group differences in accuracy and reaction time on the letter “E” control task were examined separately using 2 (group: MDD, HC) × 2 (valence: positive, negative) mixed model ANCOVAs, controlling for age and gender. Lastly, Pearson's correlations assessed relationships between self- and general-perception scores, response times, and clinical variables. Significance was two-tailed with p < 0.05.
2.5. Neuroimaging acquisition and analysis
Imaging data were acquired at the NYU Center for Brain Imaging on a Siemens Allegra 3T scanner, with a single-channel head coil. High-resolution T1-weighted anatomical images were acquired using a magnetization-prepared rapid gradient-echo sequence (TR = 2530 ms; TE = 3.25 ms; TI = 1100 ms; flip angle = 7°; 128 slices; FOV = 256 mm; voxel size = 1.3 mm × 1 mm × 1.3 mm). Functional T2*-weighted gradient echo images were acquired over 2 runs with 40 contiguous axial interleaved slices with a 0 mm gap (TR = 2000 ms; TE = 25 ms; flip angle = 80°; FOV = 192; 64 × 64 matrix size; voxel size = 3 mm × 3 mm × 3 mm).
All neuroimaging analyses were performed using FSL (FMRIB Software Library) version 5.0.7 [www.fmrib.ox.ac.uk/fsl; Jenkinson et al., 2012, Smith et al., 2004, Woolrich et al., 2009]. Preprocessing was carried out using FEAT (FMRI Expert Analysis Tool) and included slice-timing correction, motion correction with MCFLIRT (Jenkinson et al., 2002), brain extraction (Smith, 2002), and volume registration. Registration of structural, functional, and standard space templates was carried out using both linear (FLIRT) and nonlinear (FNIRT) transformation tools (Greve and Fischl, 2009, Jenkinson et al., 2002, Jenkinson and Smith, 2001). Lastly, data were smoothed with a 6 mm FWHM Gaussian kernel. Motion plots were examined and if they showed more than 2 degrees of rotation or 3 mm of translation then participants were excluded from further analysis. In order to estimate task-related changes in blood-oxygen-level dependent (BOLD) signal, each judgment type (i.e. general positive and negative, self positive and negative, and letter positive and negative) was included as a regressor of interest in a general linear model (GLM). Responses were convolved with a double-gamma hemodynamic response function. Additionally, the instruction screens and extended motion parameters were included as regressors of no interest. First-level contrast estimates of each stimulus type for each subject were computed, treating each run as a fixed effect.
Group analyses treated each subject as a random effect using FSL's FLAME (FMRIB's local analysis of mixed effects). A whole-brain 2 (group: MDD, HC) × 2 (category: self, general) × 2 (valence: positive, negative) mixed model analysis of covariance (ANOCVA), controlling for age and gender, assessed group differences in neural activation related to self- and general-judgments. Contrasts of interest examined main effects of judgment category (self > general), valence (negative traits > positive traits), and group (MDD > HC), as well as interactions between all three variables. T-contrasts of interest were also examined to compare groups on all four self- and general-judgment types (i.e., MDD self + > HC self +; MDD self − > HC self −; MDD general + > HC general +; MDD general − > HC general −). Z-statistic images were thresholded using clusters determined by Z > 2.3 and an FDR corrected cluster significance threshold of p < 0.05. Significant clusters were further explored by extracting beta values using FSL's Featquery to determine the direction of activation differences. Time series data was extracted from all subjects in the model, regardless of whether or not a subject had significant task-related activation in the ROI. Correlations assessed the relation between brain activity, self-perception, and illness severity scores.
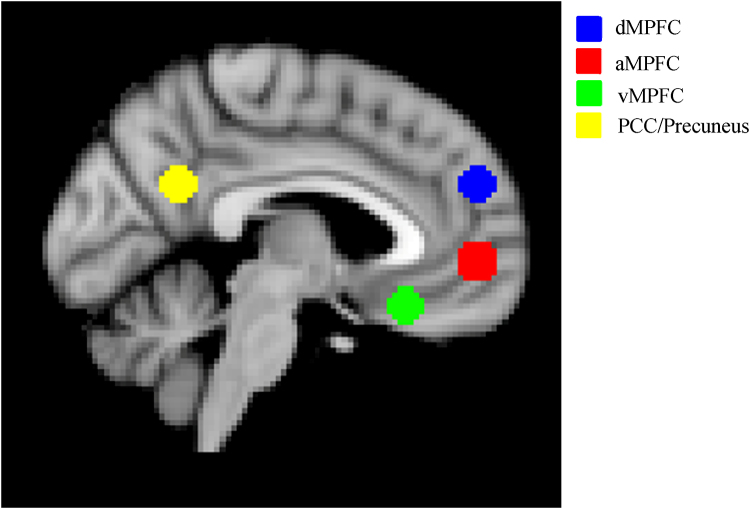
A psychophysiological interaction (PPI) analysis examined task-dependent changes in functional connectivity between groups. The PPI analysis was carried out using 4 cortical DMN seeds—the anterior medial prefrontal cortex, dorsal medial prefrontal cortex, ventral medial prefrontal cortex, and posterior cingulate cortex/precuneus. The seed regions of interest (ROIs) were chosen based on the prominent pattern of medial prefrontal cortex and PCC/precuneus activity seen in our whole-brain ANCOVA analysis. Due to the large size of these clusters, smaller spheres of equal size (8 mm diameter) were created in standard space centered around DMN coordinates obtained from Andrews-Hanna et al. (2010). The use of ROIs that were based on our own data-driven findings, as well as coordinates from the literature allowed us to more precisely examine common regions within our own activation maps that have been implicated in self-referential processing (Fig. 1). The spherical ROIs were transformed into individual subject space and the mean temporally filtered time series extracted for each ROI using terminal commands. Four PPI analyses, one for each seed, were carried out for the self versus general subtraction contrast in order to compare connectivity during self-referential processing with general trait processing. The interaction regressor was computed as the product of the mean extracted timeseries for the seed ROI and the contrast of interest (self vs. general). The PPI results reflect areas of activation that show different functional connectivity with each seed ROI for the self-judgment condition compared to the general judgment condition. A more conservative threshold was used to account for the total number of seed regions and therefore PPI analyses performed. Z-statistic images were thresholded using clusters determined by Z > 2.3, and an FDR corrected cluster significance threshold of p < 0.0125 (0.05/4 seeds) was used. Parameter estimates were extracted for significant PPI interactions using FSL's Featquery, and group differences in connectivity were reported. Dimensional relationships between connectivity and symptomatology were also explored through correlations between connectivity, self-perception, and illness severity scores.
Fig. 1.
Region of interest (ROI) placement for psychophysiological interaction (PPI) analysis. This figure illustrates the placement of the four ROIs (dMPFC = dorsal medial prefrontal cortex; aMPFC = anterior medial prefrontal cortex; vMPFC = ventral medial prefrontal cortex; PCC = posterior cingulate cortex).
3. Results
3.1. Participants
Age [t(39) = −0.748, p = 0.46, d = 0.24], with 95% CI [−1.87, 0.86], gender [χ2(1) = 0.004, p = 0.95], and ethnicity (i.e. Caucasian, African American, Other) [χ2(2) = 1.19, p = 0.55] were not significantly different between depressed adolescents and healthy controls. Four depressed adolescents (17%) had comorbid diagnoses of ADHD, 10 (43%) had generalized anxiety disorder (GAD), and 5 (22%) had other anxiety disorders. Demographic and clinical characteristics are summarized in Table 1.
Table 1.
Demographic and clinical characteristics.
| MDD (n = 23) |
Healthy controls (n = 18) |
|
|---|---|---|
| Age [M ± SD] (range) | 16.62 ± 2.51 (12–20) | 16.12 ± 1.54 (13–19) |
| Gender [N female/male] (%) | 13/10 (57/43%) | 10/8 (56/44%) |
| Ethnicity [N Caucasian/African American/Hispanic/Asian/other] (%)a | 10/4/7/0/2 (43/17/30/0/9%) |
6/6/1/3/2 (33/33/6/17/11%) |
| Illness history | ||
| Episode duration mos. [M ± SD] (range) | 19.22 ± 15.85 (4–72) | 0 |
| Number of depression episodes [N 0/1/2] | 0/19/4 | 18/0/0 |
| Number of suicide attempts [N 0/1/2] | 19/2/2 | 18/0/0 |
| Med-naïve/Med-free/Medicated [N] (%) | 19/3/1 (83/13/4%) | 18/0/0 (100/0/0%) |
| CDRS-Rb [M ± SD] (range) | 49.22 ± 7.21 (38–64) | 19.56 ± 2.53 (17–27) |
| BDI-IIc [M ± SD] (range) | 22.7 ± 12.44 (1–45) | 2.67 ± 2.91 (0–10) |
| Anhedonia [M ± SD] (range) | 6.22 ± 2.61 (1–10) | 1.56 ± 0.71 (1–3) |
Note. MDD = major depressive disorder.
Respective percentages do not add up to 100% due to rounding.
Children's Depression Rating Scale – Revised.
Beck Depression Inventory, 2nd ed.
3.2. Self-perception
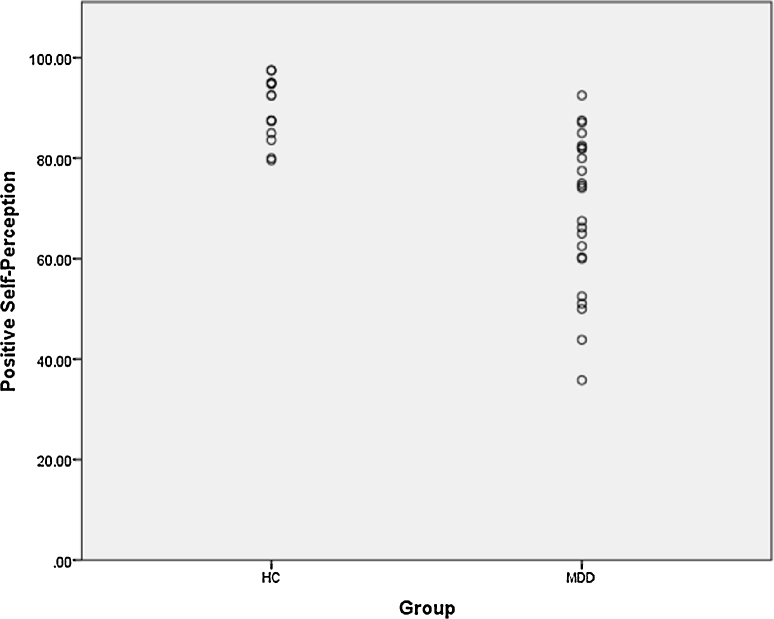
Positive self-perception scores were normally distributed in the depressed group, with a wide range between 35.82 and 92.5. Scores in healthy controls were approximately normally distributed, with a more restricted, but still varied range between 79.61 and 97.50. There was overlap in the distributions of depressed and healthy adolescents, demonstrating the heterogeneity of the depressed group, with some individuals demonstrating high self-esteem, while others were more severely impaired (illustrated in Fig. 2). Positive self-perception in the depressed group was significantly correlated with clinician-rated depression severity [CDRS-R; r(23) = −0.55, p = 0.007], self-related depression severity [BDI; r(23) = −0.58, p = 0.003], social anxiety [r(22) = −0.49, p = 0.02], overall anxiety [r(22) = −0.44, p = 0.04], irritability [r(23) = −0.70, p < 0.0005], and marginally with anhedonia [r(23) = −0.41, p = 0.05].
Fig. 2.
Distribution of positive self-perception scores. This graph illustrates the distributions of self-perception scores in the healthy control (HC) and depressed (MDD) groups.
3.3. Group differences in trait judgments
The 2 (group: MDD, HC) × 2 (category: self, general) × 2 (valence: positive, negative) mixed model ANCOVA, controlling for age and gender, yielded a significant three-way interaction between group, category, and valence [F(1,37) = 18.52, p < 0.0005, ηp2 = 0.33]. Depressed adolescents had lower positive self-perceptions [MHC = 90.49 (2.88); MMDD = 69.38 (2.55)] and higher negative self-perceptions [MHC = 9.51 (2.88); MMDD = 30.62 (2.55)] than healthy controls [F(1,37) = 29.93, p < 0.0005, ηp2 = 0.45]. Additionally, depressed adolescents labeled fewer general traits as positive [MHC = 96.27 (1.12); MMDD = 92.39 (0.99)] and more general traits as negative [MHC = 3.73 (1.12); MMDD = 7.61 (0.992)] than healthy controls [F(1,37) = 6.66, p = 0.01, ηp2 = 0.15]. There was also an interaction between group and valence [F(1,37) = 34.20, p < 0.0005, ηp2 = .48] such that depressed adolescents expressed fewer positive perceptions than HCs, and a main effect of valence [F(1,37) = 11.54, p = 0.002, ηp2 = 0.24] in which more positive traits were endorsed overall. Taken together, these findings confirm that depressed adolescents rate themselves less favorably than HC. Additionally, these results show that depressed adolescents are less accurate at labeling traits as positive and categorize personality traits more negatively in general. Trait responses are presented in Table 2.
Table 2.
Behavioral trait ratings (%).
| Self |
General |
Letter |
||||
|---|---|---|---|---|---|---|
| Positive | Negative | Positive | Negative | Positive | Negative | |
| HC | 90.57 (5.92) | 9.43 (5.92) | 95.89 (4.28) | 4.11 (4.28) | 98.33 (4.20) | 96.83 (4.45) |
| MDD | 69.32 (15.37) | 30.68 (15.37) | 92.68 (6.12) | 7.31 (6.12) | 96.46 (6.14) | 95.82 (5.37) |
Note. Mean percentages are reported followed by (SD). The self and general categories indicate the percentage of positive perceptions (yes to positive traits, no to negative traits) and negative perceptions (no to positive traits, yes to negative traits) that were endorsed. The letter category indicates percent accuracy in detecting a letter ‘E’ in a trait word. HC = healthy controls; MDD = major depressive disorder.
Response times were similarly submitted to a 2 (group: MDD, HC) × 2 (category: self, general) × 2 (valence: positive, negative) mixed model ANCOVA, controlling for age and gender, in which depressed adolescents were slower overall than healthy controls [F(1,37) = 11.29, p = 0.002, ηp2 = 0.23]. There was also a significant group by category interaction [F(1,37) = 7.00, p = 0.01, ηp2 = 0.16]. Depressed adolescents were slower at making both self-judgments (p = 0.001) and general-judgments (p = 0.009) than healthy controls (Table 3). Additionally, self-judgments were slower than general trait judgments in both the depressed group (p < 0.0005) and in healthy controls (p = 0.02).
Table 3.
Behavioral response times (ms).
| Self |
General |
Letter |
||||
|---|---|---|---|---|---|---|
| Positive | Negative | Positive | Negative | Positive | Negative | |
| HC | 990.72 (226.29) | 1085.85 (233.10) | 946.35 (234.04) | 1033.39 (222.21) | 816.81 (208.76) | 869.43 (249.65) |
| MDD | 1271.50 (231.14) | 1332.95 (220.98) | 1099.49 (207.41) | 1237.14 (226.63) | 916.21 (233.75) | 981.20 (247.85) |
Note. Behavioral response times (ms) for positive and negative traits are reports followed by (SD). HC = healthy controls; MDD = major depressive disorder.
3.4. Group differences in the letter “E” task
Due to the highly skewed distributions of the letter accuracy data, a 2 (group: MDD, HC) × 2 (valence: positive, negative) mixed model rank-based ANCOVA, controlling for age and gender, examined accuracy differences on the letter “E” control task. There were no significant differences between depressed adolescents and healthy controls on accuracy [Table 2; F(1,37) = 1.84, p = 0.183, ηp2 = 0.05]. There was also no interaction between group and valence [F(1,37) = 0.544, p = 0.466, ηp2 = 0.01] or a main effect of valence [F(1,37) = 0.152, p = 0.70, ηp2 = 0.004].
A 2 (group: MDD, HC) × 2 (valence: positive, negative) mixed model ANCOVA, controlling for age and gender, examined reaction time differences on the letter “E” control task. There were no significant differences in reaction time between depressed adolescents and healthy controls [Table 3; F(1,37) = 2.19, p = 0.148, ηp2 = 0.06]. There was also no interaction between group and valence [F(1,37) = 0.621, p = 0.436, ηp2 = 0.02]. However, there was a main effect of valence [F(1,37) = 9.77, p = 0.003, ηp2 = 0.21], such that participants took longer to identify whether negative trait adjectives (M = 924.73, SE = 39.64) had a letter “E” than positive trait words (M = 866.41, SE = 36.00). Given that there were no significant differences in accuracy or reaction time between depressed adolescents and healthy controls on this control task, no further analysis of this condition was done, as it is not the focus of this study; subsequent analyses focused only on differences between the self- and general-judgment conditions.
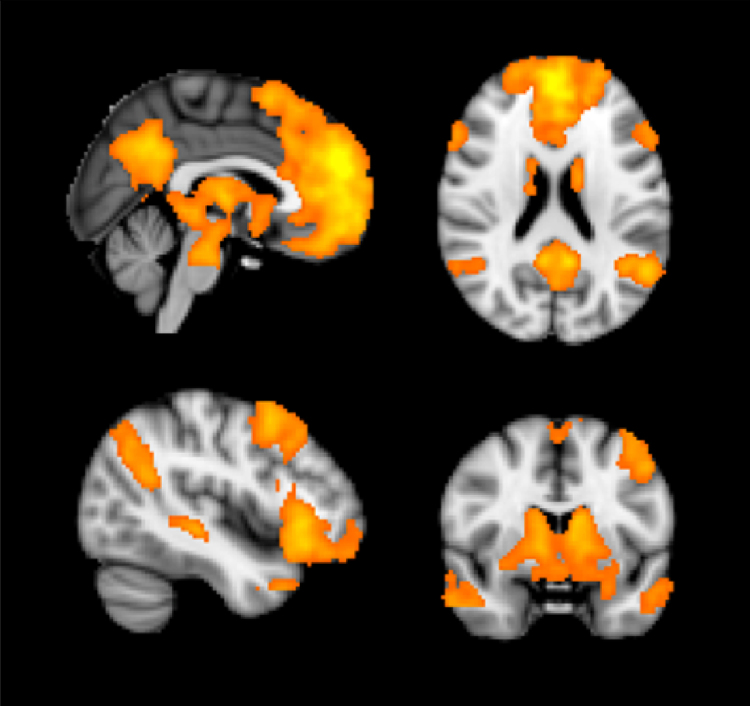
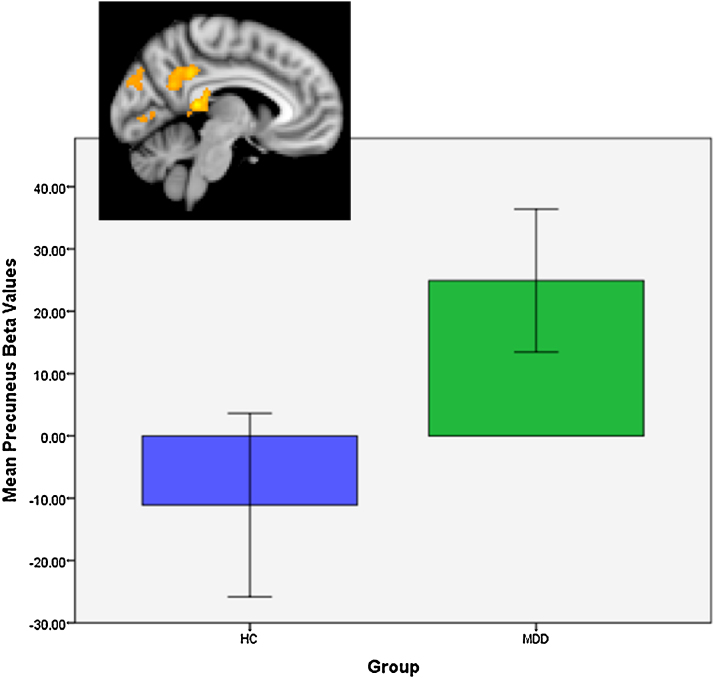
3.5. Neural responses to traits
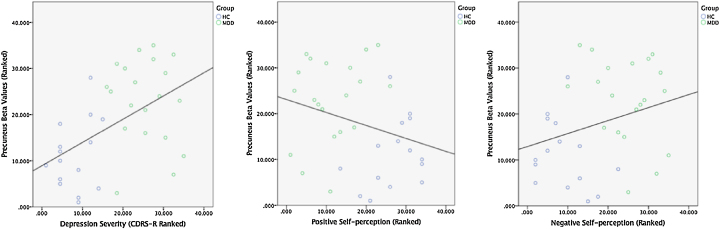
The whole-brain 2 × 2 × 2 ANCOVA showed a robust main effect of category such that self-judgments prompted greater activity throughout the cortex compared to general-judgments in the MPFC, ACC, VLPFC, PCC/precuneus, thalamus, striatum, middle temporal cortex, inferior parietal lobe, and the lateral occipital cortex (see Table 4 and Fig. 3). No activity for the overall main effect of group or valence survived the whole-brain corrected threshold. However, there were significant group differences in the PCC/precuneus for self-judgments of positive trait words (Table 4). Beta values extracted from this region showed that depressed adolescents activated the PCC/precuneus when making self-judgments, while healthy controls deactivated this region (Fig. 4). In the entire imaging sample (n = 35), two-tailed Spearman correlations showed that PCC/precuneus activity was not correlated with positive [ρ(35) = −0.28, p = 0.100] or negative [ρ(35) = 0.28, p = 0.100] self-perception scores, although these relationships trended toward significance. However, PCC/precuneus activity was correlated with depression severity [ρ(35) = 0.50, p = 0.002]; greater activity in the PCC/precuneus was associated with more severe depression (Fig. 5). Alternately, within just the MDD group (n = 20), PCC/precuneus activity was not correlated with positive [ρ(20) = 0.27, p = 0.248] or negative [ρ(20) = −0.27, p = 0.248] self-perception, or depression severity [ρ(20) = −0.12, p = 0.628]. Additionally, there were group differences in both negative self-judgments and positive general-judgments, whereby healthy controls activated left and right middle and lateral occipital regions respectively compared to depressed adolescents (Table 4). No activity for the group × category or group × valence interactions [e.g. MDD (positive self > negative self) > HC (positive self > negative self)] survived the whole-brain corrected threshold.
Table 4.
Activations for main effects of category, valence, and group.
| Region | Side | k | Z | X | Y | Z |
|---|---|---|---|---|---|---|
| Category: Self ≥ General | ||||||
| MPFC/VLPFC/Caudate/Putamen/Thalamus/Middle temporal gyrus/ACC/PCC/Precuneus | L/R | 35,608 | 6.17 | 2 | 52 | 26 |
| Inferior parietal (Angular gyrus)/lateral occipital gyrus | L | 1234 | 4.68 | −54 | −58 | 24 |
| Inferior parietal (Angular gyrus)/lateral occipital gyrus | R | 519 | 4 | 50 | −58 | 30 |
| Valence: Positive ≥ Negative | None | |||||
| Group: MDD ≥ HC | None | |||||
| Group: MDD (Self ±) ≥ HC (Self ±) | ||||||
| PCC/Precuneus | L/R | 1208 | 3.94 | 4 | −42 | 4 |
| Cuneus | L/R | 491 | 3.82 | 0 | −82 | 34 |
| Group: HC (Self −) ≥ MDD (Self −) | ||||||
| Middle occipital gyrus | L | 477 | 4.01 | −24 | −92 | 12 |
| Group: HC (General ±) ≥ MDD (General ±) | ||||||
| Lateral occipital cortex | R | 530 | 3.92 | 34 | −86 | 0 |
| Group: HC (General −) ≥ MDD (General −) | None | |||||
Note. Z statistic images were thresholded using clusters determined by Z > 2.3 and a corrected cluster significance of p < 0.05. Peak x, y, z coordinates are in MNI space. R = right. L = left. MPFC = medial prefrontal cortex. ACC = anterior cingulate cortex. PCC = posterior cingulate cortex. VLPFC = ventrolateral prefrontal cortex.
Fig. 3.
Main effect of category activation pattern. This figure illustrates the activation pattern for the contrast of self-judgments vs. general-judgments across all participants.
Fig. 4.
Group comparison of positive self-judgments. This figure illustrates the activation pattern and parameter estimates elicited by the contrast of positive self-judgments in the depressed (MDD) group vs. positive self-judgments in the healthy control (HC) group.
Fig. 5.
Correlations between brain activity and symptoms. Graphs of the correlations between precuneus activity and depression severity and self-perception scores in the total sample (n = 35).
3.6. Functional connectivity of DMN seeds
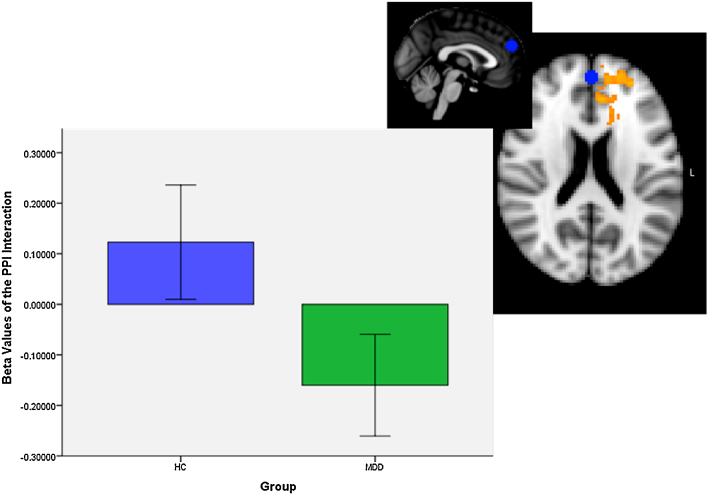
There was a significant PPI interaction for the dMPFC seed (Table 5 and Fig. 6). No other seed region showed altered connectivity during self-judgments compared to general-judgments. Parameter estimates were extracted from the significant PPI interaction cluster to examine the direction of the group difference. Depressed adolescents showed reduced connectivity (negative Beta values) between the dMPFC and local left-sided prefrontal regions, including the ACC, frontal pole, and orbitofrontal cortex during self-referential processing (Fig. 6). In the total imaging sample (n = 35), beta values were significantly correlated with illness severity [ρ(35) = −0.53, p = 0.001], and both positive [ρ(35) = 0.51, p = 0.002] and negative [ρ(35) = −0.51, p = 0.002] self-perception. However, in just the MDD group (n = 20), connectivity was not significantly correlated with illness severity [ρ(20) = 0.061, p = 0.798], positive [ρ(20) = 0.27, p = 0.248], or negative [ρ(20) = −0.27, p = 0.248] self-perception.
Table 5.
PPI connectivity differences between self- and general-judgments.
| Contrast/region | Side | k | Z | X | Y | Z |
|---|---|---|---|---|---|---|
| dMPFC Seed: MDD vs. HC | ||||||
| Frontal pole/ACC/Orbitofrontal cortex | L | 1038 | 4 | −28 | 46 | 14 |
| vMPFC seed: MDD vs. HC | None | |||||
| aMPFC seed: MDD vs. HC | None | |||||
| PCC/Precuneus seed: MDD vs. HC | None | |||||
Note. Z statistic images were thresholded using clusters determined by Z > 2.3 and an FDR corrected cluster significance of p < 0.0125 (0.05/4 seeds). Peak x, y, z coordinates are in MNI space. R = right. L = left. dMPFC = dorsal medial prefrontal cortex; vMPFC = ventral medial prefrontal cortex; aMPFC = anterior medial prefrontal cortex; PCC = posterior cingulate cortex.
Fig. 6.
Functional connectivity results. This figure illustrates the connectivity of the dMPFC seed. The blue circle indicates the dMPFC seed region. The depressed (MDD) group showed reduced local frontal connectivity with the dMPFC seed during self-referential processing compared to general trait processing.
4. Discussion
As expected, we replicated previous behavioral findings that depressed adolescents perceive themselves more negatively that healthy youth and are slower to make self-referential judgments (Gara et al., 1993, Grimm et al., 2009, Lemogne et al., 2009, Lemogne et al., 2010, Yoshimura et al., 2010). Moreover, in the entire sample, lower positive self-perceptions were related to higher depression severity, irritability, social anxiety, and anhedonia scores, emphasizing the importance of examining dimensional relationships in psychiatric research since symptoms exist along a continuum, even in the “healthy” population and are not simply present or absent. Furthermore, the depressed group was less accurate at identifying positive traits as such and categorized them more negatively, suggesting depressed adolescents may have a more globally negative perspective on personality traits in general. Additionally, despite our hypothesis that depressed adolescents would show increased activation and connectivity of cortical midline regions in response to self-referential processing, we found that all adolescents, depressed and healthy, strongly activated anterior and posterior regions within the DMN in response to self-judgments. The only region that was activated more in depressed adolescents was the PCC/precuneus in response to positive traits. Dimensional analyses revealed a significant correlation between PCC/precuneus activity and depression severity in the entire sample, further supporting the need for dimensional investigations of psychopathology. Lastly, functional connectivity of the dMPFC with local left-sided frontal regions was reduced in depressed adolescents, and was related to both illness severity and self-esteem scores in the entire sample.
4.1. Behavioral findings
Our study replicates prior behavioral findings in depressed adults (Grimm et al., 2009, Lemogne et al., 2009, Lemogne et al., 2010), showing increased reaction times during self-attribute rating tasks in the depressed group compared to controls. Importantly, in the current study, four adolescents with MDD carried a co-morbid diagnosis of ADHD, which may have contributed to this finding. However, adolescent major depression is a heterogeneous disorder and ADHD is highly comorbid in this population; rates of co-occurrence of ADHD in adolescent MDD range up to 50% (Angold et al., 1999, Luby et al., 2003, Turgay and Ansari, 2006). More importantly, concentration difficulties as a symptom, is highly prevalent in depression and is considered one of the associated symptoms of major depression under the DSM-IV-TR criteria (American Psychiatric Association, 2000). Moreover, there were no significant differences in accuracy or reaction time between groups on the letter “E” control task, further suggesting that these differences in self-rating reaction time are related specifically to the self-perception task and not a general cognitive slowing or attentional impairment. Therefore, we believe that the behavioral findings are related to the overall neural consequences of major depression, rather than the contribution of 4 patients with co-morbid ADHD diagnoses in our sample.
4.2. Group differences in self-perception
Group differences in response to self-judgments were only found in one region, the PCC/precuneus; depressed adolescents activated this region, while healthy controls deactivated it in response to self-judgments of positive traits. Studies of the neural processing of emotional valence in healthy adults have shown that the posterior cingulate cortex/precuneus is often activated in attentional and emotional tasks (Posner et al., 2009, Posner and Dehaene, 1994), specifically in reference to self-judgment (Cavana and Trimble, 2006, Ochsner et al., 2004). Furthermore, Posner et al. (2009) documented a positive correlation between activation of the posterior cingulate cortex/precuneus and increasingly aversive, negatively valenced emotional stimuli. Posner et al. (2009) suggests that the recruitment of this region may be due to the greater emotional salience of negatively valenced words, which results in the subsequent recruitment of greater attentional resources when processing these stimuli. This finding is supported by studies that demonstrate the PCC's role in the modulation of emotionally salient memories (Maddock, 1999, Maddock and Buonocore, 1997, Maddock et al., 2003), given its strong connections to regions underlying both emotional processing (Allison et al., 2000, Carmichael and Price, 1995), and memory (Bentovoglio et al., 1993). Thus, depressed adolescents in our sample may find personality traits that are typically considered to be positive, more aversive due to their altered self-perception and more negative perception of personality traits in general. This theory is supported by the behavioral data (Table 2); depressed adolescents endorsed fewer positive traits than healthy adolescents and had a more globally negative view on personality traits, as they were less accurate at labeling positive traits as such in the general-judgment condition. Their more negative view of positive stimuli may have resulted in the recruitment of the PCC/precuneus when processing these words. Alternately, healthy adolescents endorsed more positive traits and were more accurate at viewing them as positively valenced, as is evidenced by their higher positive self-perception scores; therefore, they may not have recruited this region during self-judgment of positive traits because the majority of this group did not view these traits as aversive. Lastly, this finding of increased PCC/precuneus activity during self-focused thought in adolescent depression is also consistent with research in adult MDD. Depressed adults exhibit greater activity in both anterior and posterior cortical midline structures, including the PCC/precuneus, during self-referential processing, compared to healthy controls (Grimm et al., 2009, Lemogne et al., 2009, Yoshimura et al., 2010, Zhu et al., 2012).
Our isolated group differences limited to activity in the PCC/precuneus, and not in other anterior DMN regions, may also suggest the influence of developmental processes. The posterior cortices develop during childhood and early adolescence, with myelination and synaptic pruning of the prefrontal cortex (PFC) continuing throughout the twenties (Giedd, 2004, Paus, 2005, Shaw et al., 2008). These developmental differences in the PFC can be seen in patterns of neural recruitment during cognitive processing. For example, adults show reduced activity in the MPFC compared to adolescents during self-reflection tasks (Pfeifer et al., 2007, Pfeifer et al., 2009); less activity is associated with more efficient processing in adulthood (Sebastian et al., 2008). Therefore, our lack of group differences between depressed and healthy adolescents in anterior cortical midline regions could reflect heightened MPFC activity throughout the adolescent period in general. Further support for this conclusion comes from our evidence of robust activation of both anterior and posterior DMN regions in response to self-judgments in depressed adolescents and healthy controls; both groups activated a large network in response to self-reflection, with differences only apparent in the PCC/precuneus. These differences in the PCC/precuneus were associated with illness severity and not self-perception scores, suggesting that this posterior region may have a specific role early in the course of MDD. However, it is not yet clear whether changes in MPFC activity that have been documented among adults with MDD are compensatory rather than causal, given early involvement of the PCC/precuneus.
Alternately, differences in medication status could also contribute to differences between our findings in adolescents and the adult literature. Participants in the current study were all unmedicated, while previous studies in adults have included individuals treated with psychotropic medications (Johnson et al., 2009, Grimm et al., 2009, Yoshimura et al., 2010, Yoshimura et al., 2014). Previous studies of healthy individuals who were given controlled doses of citalopram, fluvoxamine, as well as other psychotropic medications, showed drug-related variations in neural activation during a variety of fMRI tasks, suggesting that these medication may affect global network function. Additionally, there is evidence that psychotropic medications specifically affect neural recruitment during emotional processing and induce positive mood responses and affect recall of negative emotions (Cerqueira et al., 2014). Therefore, while developmental alterations in the self-referential processing network from adolescence into adulthood is likely, medication effects should also not be ignored when interpreting these differences.
4.3. Functional connectivity of DMN regions
Despite our hypothesis that connectivity of cortical midline regions would be increased during self-reflection in depression, adolescents with MDD exhibited reduced functional connectivity of the dMPFC with local left-sided prefrontal regions, including the ACC and orbitofrontal cortex. Dimensional analyses yielded significant correlations between connectivity and both illness severity and self-perception scores across the entire sample, such that depressed adolescents and those with lower self-esteem exhibited reduced local dMPFC connectivity. Our findings are supported by both resting-state (Connolly et al., 2013, Cullen et al., 2009, Davey et al., 2012, Gabbay et al., 2013, Hulvershorn et al., 2011, Jiao et al., 2011, Pannekoek et al., 2014) and emotion-dependent functional connectivity studies (Ho et al., 2014a, Ho et al., 2014b, Perlman et al., 2012) that show directionally variant changes in connectivity in depressed adolescents. Work in our laboratory has also documented reduced white matter integrity of the genu, which connects prefrontal and orbitofrontal cortices, further supporting this finding (Henderson et al., 2013).
No studies to date have specifically examined task-dependent connectivity during self-referential processing in depressed adolescents. However, two studies in depressed adults, which guided our hypothesis, reported increased connectivity between the dMPFC and PCC (Lemogne et al., 2009), and between the MPFC, ACC, and amygdala (Yoshimura et al., 2010). These opposite patterns of connectivity between depressed adults and our findings in adolescents with depression may further reflect developmental differences. The resting-state theory of depression suggests that due to heightened baseline activity in cortical midline regions, ruminations and self-focused thoughts are intensified (Northoff et al., 2006, Northoff et al., 2011) and manifest through this increased activity and connectivity. However, since we report decreased connectivity between the dMPFC, ACC, and orbitofrontal cortex in depressed adolescents, it is not clear whether this shift in connectivity in adulthood is due to the neurobiological underpinnings of the illness or compensatory mechanisms. Given that the MPFC continues to develop after the onset of illness in adolescence, increased connectivity in adulthood may be the product of compensatory mechanisms in response to other early alterations within the DMN. Further examination of resting-state data, coupled with task-dependent connectivity is needed to more clearly discern the specific effects of aging and chronicity in depression.
4.4. Limitations
Although this is the first study to examine task-dependent functional connectivity during self-referential processing in adolescent depression, our results must be interpreted in light of several limitations. Our lack of interaction effects in the whole-brain analysis, as well as non-significant correlations between task activity and connectivity and symptomatology in the depressed group alone, could be due to low statistical power as a result of the small sample size. Future studies with larger medication-free samples are therefore warranted. Importantly, the depressed group manifested a normally distributed, wide range of self-esteem scores that overlapped with the healthy control group. This heterogeneity of self-esteem within the depressed group could have also contributed to our limited group differences, as 8 out of 20 depressed adolescents had self-esteem scores within the healthy control range. This point further underscores the importance of accounting for inter-variability in symptom severity in psychiatric research, which our lab has documented in adolescent MDD (Gabbay et al., 2015, Henderson et al., 2013, Henderson et al., 2014). Additionally, while dimensional analyses assessed the relation between each individual's positive and negative trait ratings and significant neural activity, individual endorsements could not be taken into account in the whole-brain 2 × 2 × 2 ANCOVA analysis due to methodological constraints of the mixed design and the individuals sampled. For example, many of the healthy control participants did not endorse negative traits or reject positive traits. Thus, we could not create conditions in the GLM according to how traits were positively or negatively viewed, which would ideally give additional insight into the neural mechanisms of self-perception. Lastly, the use of a single channel head coil may have reduced the sensitivity of our imaging protocol to detect differences in the hemodynamic response. Future studies using more advance multichannel, multiband imaging are warranted.
4.5. Conclusions
Despite these limitations, this study offers important preliminary information about neural mechanisms of self-perception and task-dependent connectivity of the DMN in medication-free adolescents with depression. Our findings of increased activity in the PCC/precuneus during self-judgment and decreased functional connectivity of local left-sided prefrontal regions, highlight possible developmental differences in disease progression between adolescents and adults. Given that these changes occur at a critical developmental juncture, it is important to further investigate the specific neurobiological mechanisms through which these alterations occur.
Conflict of interest
All authors report no conflicts of interest.
Acknowledgments
This study was supported by grants from the National Institute of Mental Health to VG (MH095807, MH101479). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH. The NIMH had no further role in the design, collection, management, analysis, and interpretation of data, or preparation of the manuscript.
References
- Allison T., Puce A., McCarthy G. Social perception from visual cues: role of the STS region. Trends Cogn. Sci. 2000;4:267–278. doi: 10.1016/s1364-6613(00)01501-1. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . 4th ed., Text Revision. American Psychiatric Association; Washington, DC: 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Andrews-Hanna J.R., Reidler J.S., Sepulcre J., Poulin R., Buckner R.L. Functional-anatomic fractionation of the brain's default network. Neuron. 2010;65:550–562. doi: 10.1016/j.neuron.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A., Costello E.J., Erkanli A. Comorbidity. J. Child Psychol. Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- Beck A.T., Guth D., Steer R.A., Ball R. Screening for major depression disorders in medical inpatients with the Beck Depression Inventory for Primary Care. Behav. Res. Ther. 1997;35:785–791. doi: 10.1016/s0005-7967(97)00025-9. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Kovacs M., Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J. Consult. Clin. Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Bentovoglio M., Kultas-Ilinsky K., Ilinsky I. Limbic thalamus: structure, intrinsic organization, and connections. In: Vogt B.A., Gabriel M., editors. Neurobiology of Cingulate Cortex and Limbic Thalamus. Birkhauser; Boston: 1993. pp. 71–122. [Google Scholar]
- Broyd S.J., Demanuele C., Debener S., Helps S.K., James C.J., Sonuga-Barke E.J.S. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci. Biobehav. Rev. 2009;33:279–296. doi: 10.1016/j.neubiorev.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Buckner R.L., Andrews-Hanna J.R., Schacter D.L. The brain's default network: anatomy, function, and relevance to disease. Ann. N. Y. Acad. Sci. 2008;1124:1–38. doi: 10.1196/annals.1440.011. [DOI] [PubMed] [Google Scholar]
- Carmichael S.T., Price J.L. Limbic connections of the orbital and medial prefrontal cortex in macaque monkeys. J. Comp. Neurol. 1995;363:615–641. doi: 10.1002/cne.903630408. [DOI] [PubMed] [Google Scholar]
- Cavana A.E., Trimble M.R. The precuneus: a review of its functional anatomy and behavioral correlates. Brain. 2006;129:564–583. doi: 10.1093/brain/awl004. [DOI] [PubMed] [Google Scholar]
- Cerqueira C.T., Sato J.R., de Almeida J.R.C., Amaro E., Leite C.C., Gorenstein C., Gentil V., Busatto G.F. Healthy individuals treated with clomipramine: an fMRI study of brain activity during autobiographical recall of emotions. Transl. Psychiatry. 2014;4:1–7. doi: 10.1038/tp.2014.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly C.G., Wu J., Ho T.C., Hoeft F., Wolkowitz O., Eisendrath S., Frank G., Hendren R., Max J.E., Paulus M.P., Tapert S.F., Banerjee D., Simmons A.N., Yang T.T. Resting-state functional connectivity of subgenual anterior cingulate cortex in depressed adolescents. Biol. Psychiatry. 2013;74:898–907. doi: 10.1016/j.biopsych.2013.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen K.R., Gee D.G., Klimes-Dougan B., Gabbay V., Hulvershorn L., Mueller B.A., Camchong J., Bell C.J., Houri A., Kumra S., Lim K.O., Castellanos F.X., Milham M.P. A preliminary study of functional connectivity in comorbid adolescent depression. Neurosci. Lett. 2009;460:227–231. doi: 10.1016/j.neulet.2009.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey C.G., Yucel M., Allen N.B., Harrison B.J. Task-related deactivation and functional connectivity of the subgenual cingulate cortex in major depressive disorder. Front. Psychiatry. 2012;3:14. doi: 10.3389/fpsyt.2012.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denny B.T., Kober H., Wager T.D., Ochsner K.N. A meta-analysis of functional neuroimaging studies of self- and other judgments reveals a spatial gradient for mentalizing in medial prefrontal cortex. J. Cogn. Neurosci. 2012;24:1742–1752. doi: 10.1162/jocn_a_00233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossati P., Hevenor S.J., Graham S.J., Grady C., Keightley M.L., Craik F., Mayberg H. In search of the emotional self: an fMRI study using positive and negative emotional words. Am. J. Psychiatry. 2003;160:1938–1945. doi: 10.1176/appi.ajp.160.11.1938. [DOI] [PubMed] [Google Scholar]
- Gabbay V., Ely B.A., Li Q., Bangaru S.D., Panzer A.M., Alonso C.M., Castellanos F.X., Milham M.P. Striatum-based circuitry of adolescent depression and anhedonia. J. Am. Acad. Child Adolesc. Psychiatry. 2013;52 doi: 10.1016/j.jaac.2013.04.003. 628–641 e613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbay V., Johnson A.R., Alonso C.M., Evans L.K., Babb J.S., Klein R.G. Anhedonia, but not irritability, is associated with illness severity outcomes in adolescent major depression. J. Child Adolesc. Psychopharmacol. 2015 doi: 10.1089/cap.2014.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gara M.A., Woolfolk R.L., Cohen B.D., Goldston R.B., Allen L.A., Novalany J. Perception of self and other in major depression. J. Abnorm. Psychol. 1993;102:93–100. doi: 10.1037//0021-843x.102.1.93. [DOI] [PubMed] [Google Scholar]
- Giedd J.N. Structural magnetic resonance imaging of the adolescent brain. Ann. N. Y. Acad. Sci. 2004;1021:77–85. doi: 10.1196/annals.1308.009. [DOI] [PubMed] [Google Scholar]
- Greicius M.D., Flores B.H., Menon V., Glover G.H., Solvason H.B., Kenna H., Reiss A.L., Schatzberg A.F. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol. Psychiatry. 2007;62:429–437. doi: 10.1016/j.biopsych.2006.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greve D.N., Fischl B. Accurate and robust brain image alignment using boundary-based registration. Neuroimage. 2009;48:63–72. doi: 10.1016/j.neuroimage.2009.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm S., Ernst J., Boesiger P., Schuepbach D., Hell D., Boeker H., Northoff G. Increased self-focus in major depressive disorder is related to neural abnormalities in subcortical–cortical midline structures. Hum. Brain Mapp. 2009;30:2617–2627. doi: 10.1002/hbm.20693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson S.E., Johnson A.R., Vallejo A.I., Katz L., Wong E., Gabbay V. A preliminary study of white matter in adolescent depression: relationships with illness severity, anhedonia, and irritability. Front. Psychiatry. 2013;4:152. doi: 10.3389/fpsyt.2013.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson S.E., Vallejo A.I., Ely B.A., Kang G., Krain Roy A., Pine D.S., Stern E.R., Gabbay V. The neural correlates of emotional face-processing in adolescent depression: a dimensional approach focusing on anhedonia and illness severity. Psychiatry Res. 2014;224:234–241. doi: 10.1016/j.pscychresns.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho T.C., Connolly C.G., Henje Blom E., LeWinn K.Z., Strigo I.A., Paulus M.P., Frank G., Max J.E., Wu J., Chan M., Tapert S.F., Simmons A.N., Yang T.T. Emotion-dependent functional connectivity of the default mode network in adolescent depression. Biol. Psychiatry. 2014 doi: 10.1016/j.biopsych.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho T.C., Yang G., Wu J., Cassey P., Brown S.D., Hoang N., Chan M., Connolly C.G., Henje-Blom E., Duncan L.G., Chesney M.A., Paulus M.P., Max J.E., Patel R., Simmons A.N., Yang T.T. Functional connectivity of negative emotional processing in adolescent depression. J. Affect. Disord. 2014;155:65–74. doi: 10.1016/j.jad.2013.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulvershorn L.A., Cullen K., Anand A. Toward dysfunctional connectivity: a review of neuroimaging findings in pediatric major depressive disorder. Brain Imaging Behav. 2011;5:307–328. doi: 10.1007/s11682-011-9134-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkinson M., Bannister P., Brady M., Smith S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage. 2002;17:825–841. doi: 10.1016/s1053-8119(02)91132-8. [DOI] [PubMed] [Google Scholar]
- Jenkinson M., Beckmann C.F., Behrens T.E., Woolrich M.W., Smith S.M. FSL. Neuroimage. 2012;62:782–790. doi: 10.1016/j.neuroimage.2011.09.015. [DOI] [PubMed] [Google Scholar]
- Jenkinson M., Smith S. A global optimisation method for robust affine registration of brain images. Med. Image Anal. 2001;5:143–156. doi: 10.1016/s1361-8415(01)00036-6. [DOI] [PubMed] [Google Scholar]
- Jiao Q., Ding J., Lu G., Su L., Zhang Z., Wang Z., Zhong Y., Li K., Ding M., Liu Y. Increased activity imbalance in fronto-subcortical circuits in adolescents with major depression. PLoS ONE. 2011;6:e25159. doi: 10.1371/journal.pone.0025159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.K., Nolen-Hoeksema S., Mitchell K.J., Levin Y. Medial cortex activity, self-reflection and depression. Soc. Cogn. Affect. Neurosci. 2009;4:313–327. doi: 10.1093/scan/nsp022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman A.S., Kaufman N.L. American Guidance Service; MN: 1990. Manual for the Kaufman Brief Intelligence Test. [Google Scholar]
- Kaufman J., Birmaher B., Brent D., Rao U., Flynn C., Moreci P., Williamson D., Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kelley W.M., Macrae C.N., Wyland C.L., Caglar S., Inati S., Heatherton T.F. Finding the self? An event-related fMRI study. J. Cogn. Neurosci. 2002;14:785–794. doi: 10.1162/08989290260138672. [DOI] [PubMed] [Google Scholar]
- Lemogne C., Delaveau P., Freton M., Guionnet S., Fossati P. Medial prefrontal cortex and the self in major depression. J. Affect. Disord. 2012;136:e1–e11. doi: 10.1016/j.jad.2010.11.034. [DOI] [PubMed] [Google Scholar]
- Lemogne C., le Bastard G., Mayberg H., Volle E., Bergouignan L., Lehericy S., Allilaire J.F., Fossati P. In search of the depressive self: extended medial prefrontal network during self-referential processing in major depression. Soc. Cogn. Affect. Neurosci. 2009;4:305–312. doi: 10.1093/scan/nsp008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemogne C., Mayberg H., Bergouignan L., Volle E., Delaveau P., Lehericy S., Allilaire J.F., Fossati P. Self-referential processing and the prefrontal cortex over the course of depression: a pilot study. J. Affect. Disord. 2010;124:196–201. doi: 10.1016/j.jad.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Lewinsohn P.M., Rohde P., Seeley J.R. Psychosocial risk factors for future adolescent suicide attempts. J. Consult. Clin. Psychol. 1994;62:297–305. doi: 10.1037//0022-006x.62.2.297. [DOI] [PubMed] [Google Scholar]
- Luby J.L., Heffelfinger A.K., Mrakotsky C., Brown K.M., Hessler M.J., Wallis J.M., Spitznagel E.L. The clinical picture of depression in preschool children. J. Am. Acad. Child Adolesc. Psychiatry. 2003;42(3):340–348. doi: 10.1097/00004583-200303000-00015. [DOI] [PubMed] [Google Scholar]
- Maddock R.J. The retrosplenial cortex and emotion: new insights from functional neuroimaging of the human brain. Trends Neurosci. 1999;22:310–316. doi: 10.1016/s0166-2236(98)01374-5. [DOI] [PubMed] [Google Scholar]
- Maddock R.J., Buonocore M.H. Activation of left posterior cingulate gyrus by the auditory presentation of threat-related words: an fMRI study. Psychiatry Res. 1997;75:1–14. doi: 10.1016/s0925-4927(97)00018-8. [DOI] [PubMed] [Google Scholar]
- Maddock R.J., Garrett A.S., Buonocore M.H. Posterior cingulate cortex activation by emotional words: fMRI evidence from a valence decision task. Hum. Brain Mapp. 2003;18:30–41. doi: 10.1002/hbm.10075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manani P., Sharma S. Self esteem and suicidal ideation: a correlational study. MIER J. Educ. Stud. Trends Pract. 2013;3:75–83. [Google Scholar]
- McGee R., Williams S. Does low self-esteem predict health compromising behaviours among adolescents? J. Adolesc. 2000;23:569–582. doi: 10.1006/jado.2000.0344. [DOI] [PubMed] [Google Scholar]
- Mitsui N., Asakura S., Shimizu Y., Fujii Y., Toyomaki A., Kako Y., Tanaka T., Kitagawa N., Inoue T., Kusumi I. The association between suicide risk and self-esteem in Japanese university students with major depressive episodes of major depressive disorder. Neuropsychiatr. Dis. Treat. 2014;10:811–816. doi: 10.2147/NDT.S59349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nejad A.B., Fossati P., Lemogne C. Self-referential processing, rumination, and cortical midline structures in major depression. Front. Hum. Neurosci. 2013;7:666. doi: 10.3389/fnhum.2013.00666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northoff G., Heinzel A., de Greck M., Bermpohl F., Dobrowolny H., Panksepp J. Self-referential processing in our brain – a meta-analysis of imaging studies on the self. Neuroimage. 2006;31:440–457. doi: 10.1016/j.neuroimage.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Northoff G., Wiebking C., Feinberg T., Panksepp J. The ‘resting-state hypothesis’ of major depressive disorder-a translational subcortical–cortical framework for a system disorder. Neurosci. Biobehav. Rev. 2011;35:1929–1945. doi: 10.1016/j.neubiorev.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Ochsner K.N., Knierim K., Ludlow D.H., Hanelin J., Ramachandran T., Glover G., Mackey S.C. Reflecting upon feelings: An fMRI study of neural systems supporting the attribution of emotion to self and other. J. Cogn. Neurosci. 2004;16(10):1746–1772. doi: 10.1162/0898929042947829. [DOI] [PubMed] [Google Scholar]
- Overholser J.C., Adams D.M., Lehnert K.L., Brinkman D.C. Self-esteem deficits and suicidal tendencies among adolescents. J. Am. Acad. Child Adolesc. Psychiatry. 1995;34:919–928. doi: 10.1097/00004583-199507000-00016. [DOI] [PubMed] [Google Scholar]
- Pannekoek J.N., van der Werff S.J., Meens P.H., van den Bulk B.G., Jolles D.D., Veer I.M., van Lang N.D., Rombouts S.A., van der Wee N.J., Vermeiren R.R. Aberrant resting-state functional connectivity in limbic and salience networks in treatment – naive clinically depressed adolescents. J. Child Psychol. Psychiatry. 2014;55:1317–1327. doi: 10.1111/jcpp.12266. [DOI] [PubMed] [Google Scholar]
- Paus T. Mapping brain maturation and cognitive development during adolescence. Trends Cogn. Sci. 2005;9:60–68. doi: 10.1016/j.tics.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Perlman G., Simmons A.N., Wu J., Hahn K.S., Tapert S.F., Max J.E., Paulus M.P., Brown G.G., Frank G.K., Campbell-Sills L., Yang T.T. Amygdala response and functional connectivity during emotion regulation: a study of 14 depressed adolescents. J. Affect. Disord. 2012;139:75–84. doi: 10.1016/j.jad.2012.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perou R., Bitsko R.H., Blumberg S.J., Pastor P., Ghandour R.M., Gfroerer J.C., Hedden S.L., Crosby A.E., Visser S.N., Schieve L.A., Parks S.E., Hall J.E., Brody D., Simile C.M., Thompson W.W., Baio J., Avenevoli S., Kogan M.D., Huang L.N. Mental health surveillance among children – United States, 2005–2011. MMWR Surveill. Summ. 2013;62(Suppl. 2):1–35. [PubMed] [Google Scholar]
- Pfeifer J.H., Lieberman M.D., Dapretto M. “I know you are but what am I?!”: neural bases of self- and social knowledge retrieval in children and adults. J. Cogn. Neurosci. 2007;19:1323–1337. doi: 10.1162/jocn.2007.19.8.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeifer J.H., Masten C.L., Borofsky L.A., Dapretto M., Fuligni A.J., Lieberman M.D. Neural correlates of direct and reflected self-appraisals in adolescents and adults: when social perspective-taking informs self-perception. Child Dev. 2009;80:1016–1038. doi: 10.1111/j.1467-8624.2009.01314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner J., Russell J.A., Gerber A., Gorman D., Colibazzi T., Yu S., Wang Z., Kangarlu A., Zhu H., Peterson B.S. The neurophysiological bases of emotion: an fMRI study of the affective circumplex using emotion-denoting words. Hum. Brain Mapp. 2009;30(3):883–895. doi: 10.1002/hbm.20553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner M.I., Dehaene S. Attentional networks. Trends Neurosci. 1994;17:75–79. doi: 10.1016/0166-2236(94)90078-7. [DOI] [PubMed] [Google Scholar]
- Poznanski E., Freeman L., Mokros H. Children's depression rating scale-revised. Psychopharmacol. Bull. 1985;21:979–989. [Google Scholar]
- Raichle M.E., MacLeod A.M., Snyder A.Z., Powers W.J., Gusnard D.A., Shulman G.L. A default mode of brain function. Proc. Natl. Acad. Sci. U. S. A. 2001;98(2):676–682. doi: 10.1073/pnas.98.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sambataro F., Wolf N.D., Pennuto M., Vasic N., Wolf R.C. Revisiting default mode network function in major depression: evidence for disrupted subsystem connectivity. Psychol. Med. 2013:1–11. doi: 10.1017/S0033291713002596. [DOI] [PubMed] [Google Scholar]
- Sebastian C., Burnett S., Blakemore S.J. Development of the self-concept during adolescence. Trends Cogn. Sci. 2008;12:441–446. doi: 10.1016/j.tics.2008.07.008. [DOI] [PubMed] [Google Scholar]
- Shaw P., Kabani N.J., Lerch J.P., Eckstrand K., Lenroot R., Gogtay N., Greenstein D., Clasen L., Evans A., Rapoport J.L., Giedd J.N., Wise S.P. Neurodevelopmental trajectories of the human cerebral cortex. J. Neurosci. 2008;28:3586–3594. doi: 10.1523/JNEUROSCI.5309-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S.M. Fast robust automated brain extraction. Hum. Brain Mapp. 2002;17:143–155. doi: 10.1002/hbm.10062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S.M., Jenkinson M., Woolrich M.W., Beckmann C.F., Behrens T.E., Johansen-Berg H., Bannister P.R., De Luca M., Drobnjak I., Flitney D.E., Niazy R.K., Saunders J., Vickers J., Zhang Y., De Stefano N., Brady J.M., Matthews P.M. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23(Suppl. 1):S208–S219. doi: 10.1016/j.neuroimage.2004.07.051. [DOI] [PubMed] [Google Scholar]
- Tanner J.M. Thomas; Springfield, IL: 1962. Growth at Adolescence. [Google Scholar]
- Turgay A., Ansari R. Major depression with ADHD: in children and adolescents. Psychiatry (Edgmont) 2006;3(4):20–32. [PMC free article] [PubMed] [Google Scholar]
- Uddin L.Q. Salience processing and insular cortical function and dysfunction. Nat. Rev. Neurosci. 2015;16:55–61. doi: 10.1038/nrn3857. [DOI] [PubMed] [Google Scholar]
- Wilburn V.R., Smith D.E. Stress, self-esteem, and suicidal ideation in late adolescents. Adolescence. 2005;40:33–45. [PubMed] [Google Scholar]
- Woolrich M.W., Jbabdi S., Patenaude B., Chappell M., Makni S., Behrens T., Beckmann C., Jenkinson M., Smith S.M. Bayesian analysis of neuroimaging data in FSL. Neuroimage. 2009;45:S173–S186. doi: 10.1016/j.neuroimage.2008.10.055. [DOI] [PubMed] [Google Scholar]
- Yoshimura S., Okamoto Y., Onoda K., Matsunaga M., Okada G., Kunisato Y., Yoshino A., Ueda K., Suzuki S., Yamawaki S. Cognitive behavioral therapy for depression changes medial prefrontal and ventral anterior cingulate cortex activity associated with self-referential processing. Soc. Cogn. Affect. Neurosci. 2014;9:487–493. doi: 10.1093/scan/nst009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshimura S., Okamoto Y., Onoda K., Matsunaga M., Ueda K., Suzuki S., Shigetoyamawaki Rostral anterior cingulate cortex activity mediates the relationship between the depressive symptoms and the medial prefrontal cortex activity. J. Affect. Disord. 2010;122:76–85. doi: 10.1016/j.jad.2009.06.017. [DOI] [PubMed] [Google Scholar]
- Yoshimura S., Ueda K., Suzuki S., Onoda K., Okamoto Y., Yamawaki S. Self-referential processing of negative stimuli within the ventral anterior cingulate gyrus and right amygdala. Brain Cogn. 2009;69:218–225. doi: 10.1016/j.bandc.2008.07.010. [DOI] [PubMed] [Google Scholar]
- Zhu X., Wang X., Xiao J., Liao J., Zhong M., Wang W., Yao S. Evidence of a dissociation pattern in resting-state default mode network connectivity in first-episode, treatment-naive major depression patients. Biol. Psychiatry. 2012;71:611–617. doi: 10.1016/j.biopsych.2011.10.035. [DOI] [PubMed] [Google Scholar]