Abstract
Objectives
We aimed to determine the severity and co-occurrence of established and potential paraneoplastic conditions in pancreatic cancer (weight loss, new onset diabetes, fatigue, and depression) and their relation to patient characteristics.
Methods
Using information from personal interviews with 510 cases and 463 controls, we obtained adjusted odds ratios for weight loss, long-term and new-onset diabetes, fatigue and depression before diagnosis. Among cases, we investigated the extent to which these factors occurred together and the characteristics of those reporting them.
Results
The adjusted odds ratio (OR) for weight loss (>3% of usual weight) was 27.0 (95% confidence interval (CI) 17.1-42.6). Severe weight loss was common (21% of cases lost >15%), and was more common in those previously obese. Diabetes was more common in cases and was strongly associated with weight loss (P<0.0001). Diabetes in cases more often led to prescription of insulin, compared to controls.
Fatigue and depression were significantly more common in cases than controls but not related to weight loss or diabetes. These conditions were not related to stage at diagnosis.
Conclusions
Weight loss, often severe, and new onset diabetes frequently occur together before diagnosis of pancreatic cancer. Fatigue and depression are also potential precursors of diagnosis.
Keywords: pancreatic neoplasms, weight loss, diabetes mellitus, depression, fatigue, paraneoplastic conditions
Introduction
Pancreatic cancer is a lethal disease and most patients have very short survival. Patients are usually identified when the disease is advanced and treatment is of little effect. While pancreatic cancer appears to progress rapidly, recent studies have indicated that it may develop slowly over time, perhaps as long as 20 years1. This may provide a basis for identification of patients at an earlier stage of disease when treatment can be more successful. New-onset diabetes2-4 and weight loss5-7 are established paraneoplastic features of pancreatic cancer. The severity of these conditions, the degree to which they overlap, and which types of patients they affect, have not been studied in detail. In addition, there are some indications that depression and fatigue may precede a diagnosis of pancreatic cancer, but this has rarely been studied. In this report, we used data from a large hospital- based case-control study of pancreatic cancer to investigate in more detail the severity of weight loss, timing of onset and severity of diabetes, depression/sadness and fatigue prior to diagnosis, and to investigate whether these factors occur together.
Materials and Methods
Study population
The pancreatic cancer case-control study at Memorial Sloan Kettering Cancer Center (MSKCC) is part of the Pancreatic Tumor Registry, established in 2002. Cases are eligible if they have pathologically or cytologically confirmed pancreatic adenocarcinoma and speak English. For this study, we excluded 1 case and 4 controls who did not provide complete data on weight. Cases in this analysis (n=510) were interviewed within 2.5 months of their diagnosis. They were identified when seen by clinicians for initial consultation and diagnosis, follow-up after surgery, or chemotherapy. Controls (n=463) were eligible if they spoke English and had no personal history of cancer other than non-melanoma skin cancer. Controls were either visitors accompanying patients to other MSKCC clinics (n=316) or spouses of patients with pancreatic cancer (n=147). Cases and controls who agreed to take part signed Informed Consent and were personally interviewed to determine lifestyle and environmental risk factors for pancreatic cancer. Interviews for the present analysis took place between December 2004 and August 2010. Among cases approached, 13% were ineligible (primarily because they did not speak English); of those eligible, 79% took part. Among controls approached, 15% were ineligible (primarily because of history of cancer); of those eligible, 59% took part. The study was reviewed by the institutional review board at MSKCC.
Data collection
Questions on body size included usual adult weight, weight at the time of interview, and height, allowing us to determine weight changes and calculate body mass index (BMI, weight (kg)/height (m2)). We asked whether respondents were ever told they had diabetes, and if so, the age at diagnosis and the type of treatment recommended. We also asked: thinking back over the past year or so (before you got sick, for cases), have you had greater fatigue than usual; found it hard to concentrate; or felt depressed or sad for no apparent reason? Interviewers recorded “yes” or “no” answers for each of these items. In a separate part of the questionnaire on medications, respondents were asked whether they ever used antidepressants. For 492 (96%) cases, we obtained the non- fasting glucose measure (mg/dL) at the time of diagnosis from their medical record.
Statistical analysis
Weight change was the difference in pounds between the usual adult weight and weight at the time of interview. For comparing cases and controls, we considered 3 groups: those whose weight at interview was within ±3% of their usual adult weight (stable weight); those who gained >3%; and those who lost >3%. For examining weight change in relation to other variables among the cases, we considered 3 groups among those who lost weight: lost >3% but <10%; lost ≥10% but <15%; and lost ≥15%. We also evaluated weight change in pounds. Individuals who were diagnosed with diabetes when they were the same age as their pancreatic cancer diagnosis (cases) or age at interview (controls), or one or two years younger, were considered to have new-onset diabetes6,8. We determined the degree of association between the variables of interest by cross-tabulating pairs of variables and using X2 tests. Among the cases, we determined whether these variables were related to other characteristics: age, gender, education, BMI, smoking history, and stage of disease.
For comparing cases to controls, adjusted odds ratios were estimated from logistic regression. The model included age (continuous), gender, education (high school or less, college, graduate school), smoking (never, former, current), and BMI (<25, 25 to <30, ≥30, based on usual adult weight). For fatigue, inability to concentrate, and depression/sadness, we included a model with all of these variables to provide an indication of their independence from each other. We repeated these analyses with the exclusion of patients with prior cancer, since there were no controls with prior cancer. Analyses were performed in SAS Version 9.2 (SAS Institute Inc.). Results were considered statistically significant if the two-sided P value was <0.05.
We were concerned that questions on fatigue, concentration, and depression/sadness before diagnosis might be difficult to answer accurately for patients who were likely to have some of these conditions as a result of their diagnosis. To partially address this possibility, we investigated whether the time between diagnosis and interview was related to weight loss, new-onset diabetes, fatigue, concentration, or depression/sadness, as an indication of whether recall of these conditions was different in those who answered these questions further from the time of diagnosis.
Results
Respondent characteristics
Cases were older than controls: the mean age of cases was 64.3 (standard deviation (SD),11.0) and of controls, 59.5 (SD, 11.6) (Table 1). Controls were somewhat better educated than cases. Usual adult BMI was higher in cases, with 22% classified as obese (BMI ≥30) compared to 12% of controls. Fifteen per cent of the cases had a history of prior cancer. Pancreatic cancer stage distribution was: 17% stage IA-IIA; 24% Stage IIB; 19% stage III; 41% stage IV.
Table 1. Characteristics of Cases and Controls.
| Cases N=510 |
Controls N=463 |
|
|---|---|---|
|
| ||
| n (%) | n (%) | |
| Age, years | ||
| <50 | 53 (10) | 90 (19) |
| 50-59 | 107 (21) | 129 (28) |
| 60-69 | 173 (34) | 160 (35) |
| ≥70 | 177 (35) | 84 (18) |
| Mean age (SD) | 64.3 (11.0) | 59.5 (11.6) |
| Gender | ||
| Male | 275 (54) | 239 (52) |
| Female | 235 (46) | 224 (48) |
| Race | ||
| White | 453 (89) | 405 (87) |
| Black | 24 (5) | 23 (5) |
| Asian | 22 (4) | 20 (4) |
| Other or mixed | 11 (2) | 15 (3) |
| Education | ||
| High school or less | 113 (22) | 78 (17) |
| College | 225 (44) | 204 (44) |
| Graduate school | 171 (34) | 181 (39) |
| Smoking | ||
| Never | 246 (48) | 236 (51) |
| Former | 227 (45) | 197 (43) |
| Current | 37 (7) | 30 (6) |
| Usual adult BMI | ||
| <25 | 176 (35) | 230 (50) |
| 25-<30 | 223 (44) | 176 (38) |
| ≥30 | 111 (22) | 57 (12) |
| Pancreatic cancer in first degree relative | ||
| Yes | 47 (9) | 22 (5) |
| No | 461 (91) | 441 (92) |
| History of prior cancer | ||
| Yes | 78 (15) | NA |
| No | 432 (85) | |
| Stage of disease | ||
| Stage IA to IIA | 84 (17) | NA |
| Stage IIB | 122 (24) | |
| Stage III | 94 (19) | |
| Stage IV | 208 (41) | |
Numbers may not add to total because of missing values.
Abbreviations: SD-Standard Deviation, BMI-Body Mass Index, NA-Not Applicable
Weight loss, new-onset diabetes, fatigue, concentration, and depression/sadness in cases and controls
Weight loss from the usual adult weight to weight at the time of interview was highly prevalent in the pancreatic cancer patients, with 71% of the patients losing >3% of their usual adult weight. In contrast, only 7% of controls had lost this much weight (OR=27.0, 95% CI 17.1-42.6). The amount of weight lost by patients was considerable: 42% lost 10% of their body weight or more, including 21% who lost 15% or more (Table 2). In pounds, 22% of patients lost 25 pounds or more. The mean (SD) number of pounds lost by all male patients was 17.1 (17.1), and by all the females, 10.5 (18.4).
Table 2. Percent Weight Change, Diabetes, and Fatigue, Difficulty Concentrating, and Depression/Sadness in Cases and Controls.
| Cases N=510 |
Controls N=463 |
Adjusted ORa |
95% CI | |
|---|---|---|---|---|
|
| ||||
| n (%) | n (%) | |||
| Percent weight change | ||||
| Gained >3% | 55 (11) | 209 (45) | 0.59 | 0.39-0.88 |
| Stable weight (±3%) | 93 (18) | 223 (48) | 1 | |
| Lost >3% | 362 (71) | 31 (7) | 27.0 | 17.1-42.6 |
| >3 - <10% | 147 (29) | |||
| ≥10% - <15% | 108 (21) | |||
| ≥15% | 107 (21) | |||
| Diabetes | ||||
| No | 371 (73) | 428 (92) | 1 | |
| ≥3 years before cancer diagnosis/interview | 64 (13) | 23 (5) | 2.28 | 1.35-3.86 |
| <3 years before cancer diagnosis/interview | 75 (15) | 12 (3) | 6.40 | 3.37-12.2 |
| Other conditionsb | ||||
| Fatigue | 206 (40) | 141 (30) | 1.67 | 1.26-2.21 |
| Concentration | 116 (23) | 90 (19) | 1.41 | 1.01-1.96 |
| Depression/sadness | 81 (16) | 37 (8) | 2.18 | 1.41-3.36 |
Abbreviations: OR-Odds Ratio, CI-Confidence Interval
ORs adjusted for age, gender, education, smoking, BMI
Reference category for each condition is those without that condition
New-onset diabetes was common in cases, 15% compared to 3% in controls, with an adjusted odds ratio of 6.40 (95% CI 3.37-12.2) compared to those with no history of diabetes. Longer-standing diabetes was also more common in cases (OR=2.28, 95% CI 1.35-3.86). Glucose measures in cases reflected self-reported diabetes status, with mean values of 133.3 mg/dL (SD 46.9, n=358) among those with no diabetes, 179.3 mg/dL (SD 66.5, n=73) among those with new onset diabetes, and 214.1 mg/dL (SD 69.0, n=61) in those with long-standing diabetes (P<.0001, data not shown in tables).
Cases were significantly more likely than controls to have experienced fatigue (OR=1.67, 95% CI 1.26-2.21), difficulty concentrating (OR=1.41, 95% CI 1.01-1.96), or depression/sadness (OR=2.18, 95% CI 1.41-3.36) in the year before diagnosis (Table 2). When these variables were included in the same model, ORs were slightly attenuated for fatigue (OR=1.59, 95% CI 1.05-2.41) and depression/sadness (OR=2.0, 95% CI1.09-3.57), while concentration became non-significant (OR=1.13, 95% CI 0.69-1.84). Results were the same when we restricted these analyses to cases who had not had a previous cancer (n=432) (not shown in tables). Among those who reported depression/sadness (102 cases, 38 controls), use of antidepressant medications was considerably less common in cases than controls (adjusted OR=0.42, 95% CI 0.15-1.15, not shown in tables). There was no indication that reporting of weight change, new-onset diabetes, fatigue, concentration, or depression/sadness differed according to time between diagnosis and interview (data not shown).
Associations among weight loss, diabetes, fatigue, concentration and depression/sadness in cases
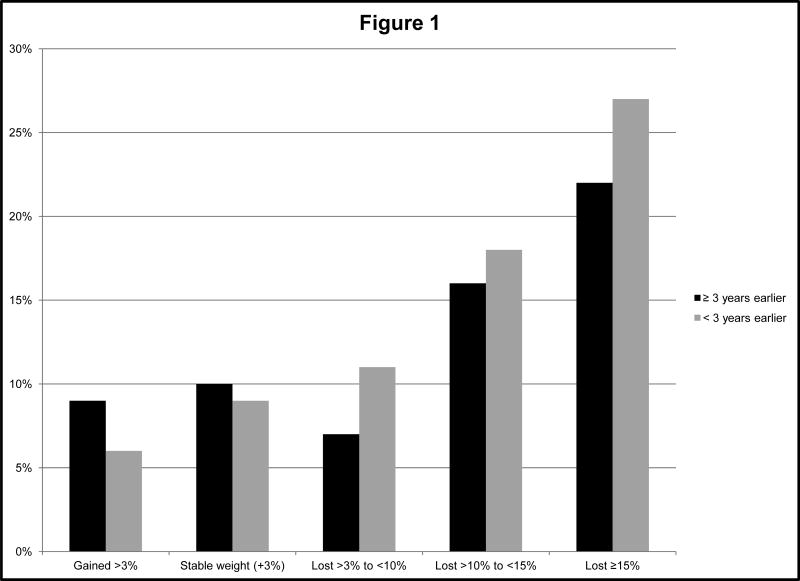
Weight loss of ≥10% was strongly related to new-onset diabetes in cases (Table 3). In those with weight gain, stable weight, or loss of <10%, 6-11% were newly diagnosed with diabetes; in contrast, among those with weight loss of ≥10% to <15% or weight loss of ≥15%, the proportions newly diagnosed were 18% and 27%, respectively (Table 3, Figure 1). Cases with greater weight loss were also more likely to have long-standing diabetes (overall P<.0001). There were no statistically significant associations between weight loss and measures of fatigue, concentration, or depression/sadness among the cases, except that a higher proportion of those who gained weight mentioned feeling fatigued. There was no relationship between weight loss and stage at diagnosis.
Table 3. Associations among Weight Loss, Diabetes, Fatigue, Concentration, Depression/Sadness, and Stage in Pancreatic Cancer Cases.
| Gained >3% | Stable weight (±3%) | Lost >3% to <10% | Lost ≥10% to <15% | Lost ≥15% | P value | No diabetes | ≥ 3 years earlier | < 3 years earlier | P value | |
|---|---|---|---|---|---|---|---|---|---|---|
| N=55 | N=93 | N=147 | N=108 | N=107 | N=370 | N=64 | N=75 | |||
|
| ||||||||||
| % | % | % | % | % | % | % | % | |||
| No diabetes | 85 | 82 | 82 | 67 | 51 | <0.0001 | ||||
| ≥ 3 years earlier | 9 | 10 | 7 | 16 | 22 | |||||
| < 3 years earlier | 6 | 9 | 11 | 18 | 27 | |||||
| Fatigue | 55 | 38 | 34 | 47 | 37 | 0.04 | 38 | 48 | 45 | 0.19 |
| Concentration | 29 | 22 | 17 | 29 | 22 | 0.18 | 21 | 31 | 24 | 0.19 |
| Depression/sadness | 20 | 13 | 12 | 16 | 22 | 0.24 | 14 | 22 | 20 | 0.15 |
| Stage IA-IIA | 11 | 22 | 16 | 18 | 15 | 0.48 | 16 | 19 | 17 | 0.48 |
| Stage IIB | 27 | 16 | 23 | 26 | 28 | 26 | 14 | 21 | ||
| Stage III | 22 | 19 | 20 | 11 | 22 | 19 | 20 | 16 | ||
| Stage IV | 40 | 43 | 42 | 44 | 36 | 39 | 47 | 45 | ||
Figure 1.
Association between weight change in patients with pancreatic cancer and presence of long-standing (≥3 years) and new-onset (<3 years) diabetes.
There were no associations between diabetes and fatigue, concentration, or depression/sadness among the patients (Table 3). Diabetes was not related to stage (Table 3), nor was fatigue, concentration, or depression/sadness (data not shown).
Characteristics of cases with weight loss, diabetes, fatigue, concentration, and depression/sadness
The amount of weight lost was strongly related to usual adult BMI, with 23% of those who lost 10-<15% and 44% of those who lost ≥15% being obese. Cases who gained weight were more likely to be women. Cases with diabetes, either new-onset or long-standing, were more likely to be males and to have been obese at their usual adult weight (Table 4). Reports of difficulty concentrating and depression/sadness were more common in women than in men. Difficulty concentrating was more often mentioned by those in their fifties, while reports of depression/sadness were more frequent among those who were obese (Table 5). Weight change and diabetes were not related to cases' education or smoking history (data not shown).
Table 4. Characteristics of Pancreatic Cancer Cases with Weight Loss and Diabetes.
| Gained >3% | Stable weight (±3%) | Lost >3% to <10% | Lost ≥10% to <15% | Lost ≥15% | P value | No diabetes | ≥ 3 years earlier | < 3 years earlier | P value | |
|---|---|---|---|---|---|---|---|---|---|---|
| N=55 | N=93 | N=147 | N=108 | N=107 | N=371 | N=64 | N=75 | |||
|
| ||||||||||
| % | % | % | % | % | % | % | % | |||
| Age | ||||||||||
| <50 | 11 | 11 | 11 | 12 | 7 | 1.0 | 11 | 6 | 9 | 0.59 |
| 50-59 | 24 | 19 | 20 | 22 | 22 | 21 | 16 | 27 | ||
| 60-69 | 33 | 33 | 34 | 31 | 37 | 34 | 39 | 31 | ||
| ≥70 | 33 | 37 | 35 | 34 | 34 | 34 | 39 | 33 | ||
| Gender | ||||||||||
| Male | 33 | 53 | 59 | 57 | 56 | 0.02 | 51 | 66 | 60 | 0.04 |
| Female | 67 | 47 | 42 | 43 | 44 | 49 | 34 | 40 | ||
| Usual adult BMI | ||||||||||
| <25 | 38 | 40 | 42 | 28 | 24 | <0.0001 | 39 | 17 | 27 | <0.0001 |
| 25-<30 | 45 | 48 | 45 | 49 | 32 | 46 | 39 | 39 | ||
| ≥30 | 16 | 12 | 13 | 23 | 44 | 15 | 44 | 39 | ||
Abbreviation: BMI-Body Mass Index
Table 5. Characteristics of Pancreatic Cancer Cases with Fatigue, Difficulty Concentrating, and Depression/Sadness.
| Fatigue | Concentration | Depression/Sadness | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Yes N=206 |
No N=303 |
P value | Yes N=116 |
No N=393 |
P value | Yes N=81 |
No N=428 |
P value | |
|
| |||||||||
| % | % | % | % | % | % | ||||
| Age | |||||||||
| <50 | 10 | 11 | 0.07 | 11 | 10 | 0.01 | 17 | 9 | 0.07 |
| 50-59 | 25 | 18 | 30 | 18 | 25 | 20 | |||
| 60-69 | 37 | 32 | 35 | 34 | 26 | 36 | |||
| ≥70 | 29 | 39 | 23 | 38 | 32 | 35 | |||
| Gender | |||||||||
| Male | 50 | 56 | 0.15 | 46 | 56 | 0.04 | 43 | 56 | 0.04 |
| Female | 50 | 44 | 54 | 44 | 57 | 44 | |||
| Usual adult BMI | |||||||||
| <25 | 35 | 34 | 0.30 | 35 | 34 | 0.53 | 27 | 36 | 0.02 |
| 25-<30 | 40 | 46 | 40 | 45 | 40 | 44 | |||
| ≥30 | 25 | 20 | 25 | 21 | 33 | 20 | |||
Abbreviation: BMI-Body Mass Index
Among those who ever were diagnosed with diabetes (n=139 cases, n=35 controls), more controls than cases were advised to go on a diet to lose weight (89% vs 55%, p<0.001), while cases were more likely to have been prescribed insulin (37% vs 9%, p<0.01) (data not shown in tables).
Discussion
Weight loss was frequently reported in the cases in our case-control study: overall, 42% of patients lost at least 10% of their weight, far more than in controls. Our findings on differences between cases and controls in the prevalence of weight loss are generally similar to those in two earlier studies5,9, although our study provides greater detail on the amount of weight lost. Since weight loss is uncommon in adults, this could potentially alert clinicians to the need for consideration of pancreatic cancer.
Fifteen percent of the cases reported diabetes diagnosed within three years of their pancreatic cancer diagnosis, in addition to 13% who had been diagnosed with diabetes at an earlier time. These measures were more common in cases than in controls. Earlier findings from case-control studies have agreed,9 although not consistently.5 A study among diabetics with and without pancreatic cancer also found more new-onset diabetes in those with cancer10. The 28% of cases who reported having diabetes (either new-onset or long standing) in our study was similar to that in an earlier study, also based on self-report11. In contrast, a case-control study at Mayo Clinic identified diabetes in 47% of cases, based on elevated fasting blood glucose at the time of interview or usage of diabetic medication9, indicating that patients in our study may not have been aware of the presence of diabetes. Our finding that cases with diabetes were considerably more likely than controls to have been prescribed insulin indicates that their diabetes was more severe and difficult to control; this is similar to findings reported in an earlier study12. Pancreatic cancer cases with existing diabetes have been found to have both weight loss and worsening of diabetes prior to cancer diagnosis10.
We also found a strong association between weight loss and diabetes, with patients who lost 10% or more of their usual adult weight the most likely to have been diagnosed with diabetes, either within the years shortly before cancer diagnosis or at an earlier time. The study from the Mayo Clinic9 also reported that weight loss and diabetes were related, with patients with diabetes experiencing greater weight loss, while a study of pancreatic cancer patients at MD Anderson found a less strong association11. Our more detailed analysis indicates that there may be a threshold effect, with increasing likelihood of new onset diabetes mainly among those with more severe weight loss (≥10% of usual adult weight).
In our study and others, patients' perceived reasons for weight loss were not queried; they might include loss of appetite5 because of mild symptoms, poor absorption leading to weight loss with normal caloric intake13, or trying to lose weight as a way of controlling new-onset diabetes. We also do not have information on when the weight loss occurred in the patients in our study.
We noted that cases were more likely than controls to report fatigue and depression/sadness in the year before their diagnosis (cases) or interview (controls). While this has rarely been addressed in large case-control studies, earlier studies using various methods have also reported that depression can precede the appearance of other symptoms or diagnosis in some pancreatic cancer patients14; fatigue before diagnosis has also been reported as distinguishing cases from controls5. In our study, results were similar when we analyzed the data according to the number of weeks between diagnosis and interview. The finding that cases in our study were less likely than controls to be taking antidepressants may indicate that their condition was relatively mild. This is consistent with reports of “malaise” noted in medical records of 5% of patients in the year before diagnosis, about twice as common in cases as in controls7.
A potential mechanism for depression and fatigue as precursors of pancreatic cancer diagnosis is the presence of elevated levels of cytokines, produced by cancer cells and inflammatory cells15-17. IL-6 is linked to both pancreatic cancer18-20 and to fatigue and depression16,19,21. Elevated levels of IL-6 have been found to be associated with clinical depression in patients with other cancers15,22,23,24. It seems possible that depression and fatigue could represent part of a paraneoplastic syndrome associated with this disease, with cytokines released by an undiagnosed tumor leading to fatigue and depression before diagnosis. In our study presence of these conditions was independent of recognized paraneoplastic conditions, weight loss and new-onset diabetes. Overall, the possibility that depression/sadness and fatigue precede pancreatic cancer warrants further study.
There was no indication that weight loss, new onset diabetes, fatigue, or depression/sadness was related to stage at diagnosis. Similar results have been reported for diabetes in other studies9,11. Gobbi et al25 reported that patients with weight loss at the time of initial presentation had longer delay between first noticing this sign and cancer diagnosis than patients with other symptoms; this may indicate that earlier recognition of weight loss as a symptom might lead to earlier diagnosis. While it is possible that greater awareness of these paraneoplastic conditions on the part of the public or primary care physicians could lead to earlier diagnosis of pancreatic cancer, it is not clear whether this would improve outcomes.
In summary, our study confirms the association of weight loss and diabetes in the years leading up to the clinical presentation of pancreatic ductal adenocarcinoma. Pancreatic cancer patients who were obese demonstrated the greatest weight loss. Unfortunately the onset of weight loss and diabetes is not specific and cannot be used routinely as a reason to evaluate patients for the possibility of pancreatic cancer. Hopefully these findings coupled with the development of biomarkers will enable early detection of this lethal disease.
Acknowledgments
Funding support: NIH P30CA008748; Goldstein Fund for Prevention, Control, and Population Research
Abbreviations
- BMI
body mass index
- CI
confidence interval
- IL-6
interleukin-6
- mg/dL
milligrams per deciliter
- MSKCC
Memorial Sloan Kettering Cancer Center
- OR
odds ratio
- SD
standard deviation
Contributor Information
Sara H. Olson, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY.
Youming Xu, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY.
Keri Herzog, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, NY.
Amethyst Saldia, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY.
Ersilia M. DeFilippis, Weill Cornell Medical College, New York, NY.
Peter Li, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY.
Peter J. Allen, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, NY.
Eileen M. O'Reilly, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, NY.
Robert C. Kurtz, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, NY.
References
- 1.Yachida S, Jones S, Bozic I, et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature. 2010;467:1114–1117. doi: 10.1038/nature09515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aggarwal G, Kamada P, Chari ST. Prevalence of diabetes mellitus in pancreatic cancer compared to common cancers. Pancreas. 2013;42:198–201. doi: 10.1097/MPA.0b013e3182592c96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raghavan SR, Ballehaninna UK, Chamberlain RS. The impact of perioperative blood glucose levels on pancreatic cancer prognosis and surgical outcomes: an evidence-based review. Pancreas. 2013;42:1210–1217. doi: 10.1097/MPA.0b013e3182a6db8e. [DOI] [PubMed] [Google Scholar]
- 4.Sah RP, Nagpal SJ, Mukhopadhyay D, et al. New insights into pancreatic cancer-induced paraneoplastic diabetes. Nat Rev Gastroenterol Hepatol. 2013;10:423–433. doi: 10.1038/nrgastro.2013.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holly EA, Chaliha I, Bracci PM, et al. Signs and symptoms of pancreatic cancer: a population-based case-control study in the San Francisco Bay area. Clin Gastroenterol Hepatol. 2004;2:510–517. doi: 10.1016/s1542-3565(04)00171-5. [DOI] [PubMed] [Google Scholar]
- 6.Pannala R, Leibson CL, Rabe KG, et al. Temporal association of changes in fasting blood glucose and body mass index with diagnosis of pancreatic cancer. Am J Gastroenterol. 2009;104:2318–2325. doi: 10.1038/ajg.2009.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stapley S, Peters TJ, Neal RD, et al. The risk of pancreatic cancer in symptomatic patients in primary care: a large case-control study using electronic records. Br J Cancer. 2012;106:1940–1944. doi: 10.1038/bjc.2012.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chari ST, Leibson CL, Rabe KG, et al. Pancreatic cancer-associated diabetes mellitus: prevalence and temporal association with diagnosis of cancer. Gastroenterology. 2008;134:95–101. doi: 10.1053/j.gastro.2007.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pannala R, Leirness JB, Bamlet WR, et al. Prevalence and clinical profile of pancreatic cancer- associated diabetes mellitus. Gastroenterology. 2008;134:981–987. doi: 10.1053/j.gastro.2008.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mizuno S, Nakai Y, Isayama H, et al. Risk factors and early signs of pancreatic cancer in diabetes: screening strategy based on diabetes onset age. J Gastroenterol. 2013;48:238–246. doi: 10.1007/s00535-012-0622-z. [DOI] [PubMed] [Google Scholar]
- 11.Sahin IH, Shama MA, Tanaka M, et al. Association of diabetes and perineural invasion in pancreatic cancer. Cancer Med. 2012;1:357–362. doi: 10.1002/cam4.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang F, Gupta S, Holly EA. Diabetes mellitus and pancreatic cancer in a population-based case-control study in the San Francisco Bay Area, California. Cancer Epidemiol Biomarkers Prev. 2006;15:1458–1463. doi: 10.1158/1055-9965.EPI-06-0188. [DOI] [PubMed] [Google Scholar]
- 13.Bond-Smith G, Banga N, Hammond TM, et al. Pancreatic adenocarcinoma. BMJ. 2012;344:e2476. doi: 10.1136/bmj.e2476. [DOI] [PubMed] [Google Scholar]
- 14.Green AI, Austin CP. Psychopathology of pancreatic cancer. A psychobiologic probe. Psychosomatics. 1993;34:208–221. doi: 10.1016/S0033-3182(93)71882-4. [DOI] [PubMed] [Google Scholar]
- 15.Lotrich FE. Inflammatory cytokine-associated depression. Brain Research. 2014 doi: 10.1016/j.brainres.2014.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reyes-Gibby CC, Wu X, Spitz M, et al. Molecular epidemiology, cancer-related symptoms, and cytokines pathway. Lancet Oncol. 2008;9:777–785. doi: 10.1016/S1470-2045(08)70197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Torres C, Perales S, Alejandre MJ, et al. Serum cytokine profile in patients with pancreatic cancer. Pancreas. 2014;43:1042–1049. doi: 10.1097/MPA.0000000000000155. [DOI] [PubMed] [Google Scholar]
- 18.Blogowski W, Deskur A, Budkowska M, et al. Selected cytokines in patients with pancreatic cancer: a preliminary report. PLoS One. 2014;9:e97613. doi: 10.1371/journal.pone.0097613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breitbart W, Rosenfeld B, Tobias K, et al. Depression, cytokines, and pancreatic cancer. Psychooncology. 2014;23:339–345. doi: 10.1002/pon.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shaw VE, Lane B, Jenkinson C, et al. Serum cytokine biomarker panels for discriminating pancreatic cancer from benign pancreatic disease. Mol Cancer. 2014;13:114. doi: 10.1186/1476-4598-13-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dahl J, Ormstad H, Aass HC, et al. The plasma levels of various cytokines are increased during ongoing depression and are reduced to normal levels after recovery. Psychoneuroendocrinology. 2014;45:77–86. doi: 10.1016/j.psyneuen.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Bower JE, Ganz PA, Irwin MR, et al. Cytokine genetic variations and fatigue among patients with breast cancer. J Clin Oncol. 2013;31:1656–1661. doi: 10.1200/JCO.2012.46.2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jehn CF, Kuehnhardt D, Bartholomae A, et al. Biomarkers of depression in cancer patients. Cancer. 2006;107:2723–2729. doi: 10.1002/cncr.22294. [DOI] [PubMed] [Google Scholar]
- 24.Miura T, Mitsunaga S, Ikeda M, et al. Characterization of Patients With Advanced Pancreatic Cancer and High Serum Interleukin-6 Levels. Pancreas. 2015;44:756–63. doi: 10.1097/MPA.0000000000000335. [DOI] [PubMed] [Google Scholar]
- 25.Gobbi PG, Bergonzi M, Comelli M, et al. The prognostic role of time to diagnosis and presenting symptoms in patients with pancreatic cancer. Cancer Epidemiol. 2013;37:186–190. doi: 10.1016/j.canep.2012.12.002. [DOI] [PubMed] [Google Scholar]