Abstract
Introduction
Intravenous administration of parecoxib could provide significant pain relief in surgical operations that require additional forms of analgesia. However, very little is known about its effects on the anxiety levels of patients before a surgical procedure. The aim of this prospective study was to investigate whether intravenous parecoxib, pre-emptively administered, has an effect on anxiety levels experienced post-surgically after total knee arthroplasty (TKA) and if it influences the reported pain of the procedure itself.
Methods
A total of 90 patients who underwent TKA under spinal anesthesia were included in the study. Prior to TKA, all patients received continuous femoral nerve block (CFNB) and were randomized into two groups: Group D consisted of 45 patients who received the drug parecoxib intravenously in addition to CFNB, whereas Group P consisted of 45 patients who received a placebo drug (N/S 0.9 %) intravenously instead of parecoxib. All patients were asked to fill in the questionnaires STAI1 and STAI2 in order to evaluate anxiety levels pre- and post-surgically, respectively. One of the main aims was to distinguish personality-trait anxiety from state anxiety, i.e., anxiety experience due to the actual perioperative events and the actual pain endured.
Results
The group receiving parecoxib had statistically significant lower anxiety levels both for personality trait anxiety and state anxiety, as compared to the placebo group.
Conclusions
Based on our findings, parecoxib had both analgesic and anxiolytic effects in patients undergoing TKA with CFNB.
Trial Registration
Current Controlled Trials: NCT02185924.
Keywords: Analgesia, Anxiety, Knee arthroplasty, Pain relief, Parecoxib, STAI1, STAI2
Introduction
Anxiety sensitivity is defined as the trait tendency to be fearful of anxiety-related sensations and is also regarded as an important factor closely associated with the experience of pain [1]. More specifically, this unpleasant feeling is commonly referred by patients during the preoperative period making them vulnerable to severe pain following surgery [2]. Patients with greater pain-related anxiety tend to over-estimate the intensity of new onset of pain, thus increasing the likelihood of reported pain [3–7]. In other words, anxiety sensitivity is not only related to greater pain experience, but it also predisposes patients towards more negative sensations of painful stimuli and, hence, towards a higher intensity of reported pain.
Continuous femoral block affords a commonly performed practice in surgical procedures of total knee arthroplasty (TKA) as an effective means of providing postoperative analgesia, while at the same time it reduces side effects and accelerates functional recovery [8, 9]. Earlier studies highlighted that patients with pain-related anxiety may benefit from sedatives and/or tranquilizers during a painful nerve block procedure [10–13], whereas others indicated the potential serious complications that may be caused from the routine use of benzodiazepines, opioids, and ketamine or fentanyl, such as prolonged sedation and amnesic effect after cessation, and hemodynamic instability among others [10, 14–16].
The analgesic effects of parecoxib administered perioperatively have been well documented [17]. Based on data from clinical trials, the peak serum concentrations of parecoxib occur approximately 30 min following intravenous administration and 1 h after intramuscular injection [18]. However, very little is known about the effects of parecoxib on the anxiety levels of patients, when regularly being administered during the perioperative period. The aim of this clinical study was to investigate the effects of intravenous parecoxib, pre-emptively administered, on the anxiety levels experienced during the perioperative period.
Methods
Ethics Statement
Informed written consent was given by all the patients prior to enrolment in the study. The study was also reviewed and approved by the Institutional Review Board and the Local Ethics Committee on human research and human studies at Aretaieion University Hospital with reference code S-138/15-06-10, and with the Helsinki Declaration of 1964, as revised in 2013. Each patient was assigned a code and all data were analyzed anonymously.
Patients
A total of 90 patients were included in the study, all of whom underwent TKA under spinal anesthesia. Prior to this, all patients received continuous femoral nerve block under neurostimulation guidance. Patients were randomly allocated into two groups in relation to the placebo/parecoxib administration, as follows: Group D (n = 45) had parecoxib 40 mg intravenously every 12 h. The first dose was administered 20 min prior to surgery completion and for every 12 h within a 48-h period. Group P (n = 45) received the placebo drug (N/S 0.9 %) intravenously, instead of parecoxib.
The randomization process was performed on the morning of surgery, where patients were randomized to one of the two aforementioned groups using computer-generated tables and sealed drawing-coded opaque envelopes. All drug solutions were prepared under aseptic conditions. All persons involved in the clinical care (surgeons, anesthesiologists and nurses) and all the patients remained blinded to the substance and the treatment group assignment.
Exclusion criteria for both groups included: age younger than 40 years old or older than 80 years old; ASA >III, obesity (>140 kg body weight); allergy to local anesthetics, history dependence on opioids, contraindications for subarachnoid anesthesia or femoral block (coagulopathy, local infection, pre-existing neurological problems, patient refusal); contraindications to the administration of parecoxib, severe hepatic or renal disease (serum creatinine ≥1.7 mg/dl).
Continuous Femoral Nerve Block Under Neurostimulation Guidance
Local anesthesia with lidocaine 1 % (0.5 mg/kg) was used to achieve generous skin and subcutaneous tissue infiltration before the needle was inserted just inferior to the inguinal crease, aiming at approximately 45° cephalad. Simultaneously, sedation with intravenous midazolam 0.05 mg/kg was administered. Continuous femoral nerve block was placed in a sterile fashion with neurostim guidance. Then a SAB (spinal) was placed in a standard and sterile fashion. Twenty milliliters of ropivacaine 0.75 % were injected as a bolus single shot. Later, in recovery following TKA, a 200-ml pump was connected to facilitate an infusion of 0.2 % at 10 ml/h.
Pain and Anxiety Visual Analog Scales
The evening prior to continuous femoral block placement, all patients were introduced to using a 10-cm visual analog scale (VAS) for procedural pain (0 = no pain at all to 10 = worst pain imaginable), and got familiar with the Spielberger State-Trait Anxiety Inventory (STAI) for adults [19]. More specifically, the level of pain was assessed and recorded on preset and agreed times (4, 8, 12, 36, 48 h postoperatively) whereas approximately 36–48 h following surgery, while under the influence of parecoxib, all patients were also requested to fill in a questionnaire, in order to evaluate anxiety levels pre- and post-surgically; STAI1 and STAI2, respectively. Of note, all patients were under the supervision of an anesthetist blinded to the substance administered, fully conscious and in stable clinical condition at the time of the questionnaire ‘assessment’. The aim of the questionnaire was to distinguish personality- or trait-anxiety (T-anxiety) i.e., measure via self-report the presence and severity of a generalized propensity to be anxious, from state anxiety (S-anxiety), i.e., anxiety experience due to the actual anesthetic/analgesic procedure and the actual pain endured. Therefore, in our study, T-anxiety can be excluded from the anxiety experienced because of the perceived threat. The questionnaire consisted of 20 questions (State-based) where answers were graded from 1 to 4 (4 = not at all, 3 = somewhat, 2 = moderately so, 1 = very much so) and 20 questions (behavior-based) where answers also graded from 1 to 4 (4 = almost never, 3 = sometimes, 2 = often, 1 = almost always). Patients were asked to circle a number as an answer to each question and the total sum of numbers in each questionnaire was used to compare anxiety levels among patients.
Statistical Analysis
The non-parametric Mann–Whitney test was performed to verify statistically significant differences between the two groups pre- and post-operatively, using the IBM SPSS Statistics program (IBM Corp. Released 2010, IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp).
Results
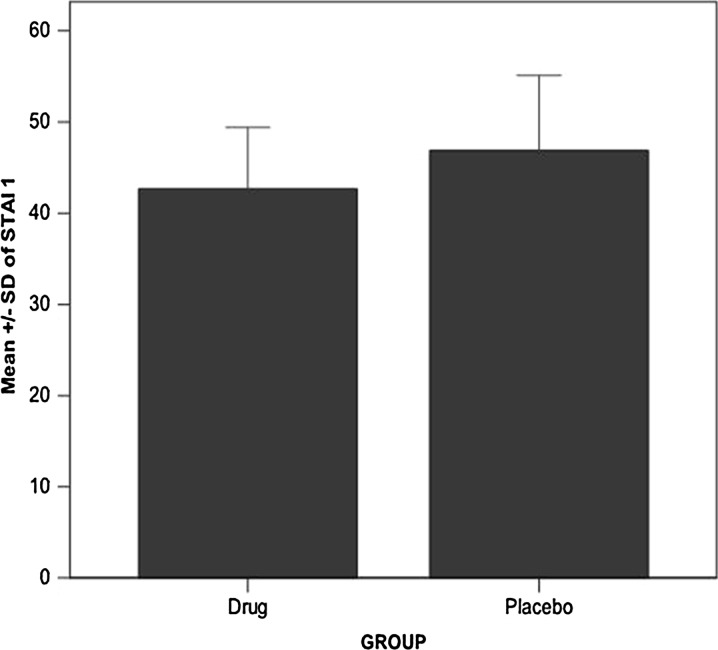
In the current study, a total of 90 patients were randomized to placebo (n = 45) and parecoxib (n = 45). No patient was withdrawn from the study (Fig. 1). The physical characteristics of the study groups were comparable; most patients were female (83.3 %) and all were Caucasians (100 %). In general, parecoxib provided greater relief than placebo following TKA; data not shown. Anxiety levels in both patient groups are shown in Figs. 2 and 3. More specifically, anxiety levels of the pre-surgical state (STAI1) are shown in Fig. 2, whereas anxiety levels of the post-surgical state (STAI2) are shown in Fig. 3. Overall, the group receiving parecoxib had lower anxiety levels both pre- and post-surgically, as compared to the placebo group, with statistical significance p = 0.012 and p = 0.002, respectively (Table 1). Precisely, we demonstrated that 40 mg of intravenous, even pre-emptively administered parecoxib improved the anxiety levels experienced during the perioperative period of TKA. Consequently, this led to better satisfaction scores and overall experience for the patients, regarding pre- and post-procedural pain, as well as pre- and post-interventional anxiety. Herein, it should be noted that STAI2 afforded the more appropriate tool to evaluate the anxiety levels during the current perioperative period, which undoubtedly can be very stressful for any individual. Nevertheless, we considered the use of STAI1 valuable to extract information about the patient’s personality, in general. For example, how patients can cope with stress and anxiety under normal circumstances.
Fig. 1.
Consort flow diagram for the study
Fig. 2.
Anxiety levels of the pre-surgical state (STAI1) between the group receiving parecoxib and the group receiving placebo. The group receiving parecoxib has statistically significant lower anxiety levels than the placebo group (p = 0.012)
Fig. 3.
Anxiety levels of the post-surgical state (STAI2) between the group receiving parecoxib and the group receiving placebo. The group receiving parecoxib has statistically significant lower anxiety levels than the placebo group (p = 0.002)
Table 1.
.
| Dynastat | STAI1 | STAI2 |
|---|---|---|
| Drug | ||
| N | 45.00 | 45.00 |
| Mean | 42.67 | 39.89 |
| SD | 6.73 | 5.07 |
| Placebo | ||
| N | 44.00 | 44.00 |
| Mean | 46.89 | 44.07 |
| SD | 8.20 | 7.65 |
| Test statistics | ||
| Mann–Whitney U | 683.000 | 617.500 |
| Wilcoxon W | 1718.000 | 1652.500 |
| Z | 2.525 | −3.067 |
| Asymp. sig. (two-tailed) | 0.012 | 0.002 |
Discussion
The type of anesthesia affords an imperative risk factor for postoperative anxiety and, as it has previously been shown, specifically the neural blockade could effectively protect patients from postoperative anxiety through superior postoperative pain control [2]. In the current study, we have shown that administration of parecoxib had statistically significantly improved anxiety levels for both trait and state anxiety levels, as compared to the placebo. Nevertheless, the evaluation of the state anxiety was the most interesting and relevant to the current study. This difference, however, may not have been directly attributed to parecoxib, at least not post-surgically, as anxiety reduction might have been due to the reduction in procedural pain, i.e., the pain acting as the mediator, and not due to the drug itself. At the same time, since we observed reduced anxiety levels in the pre-surgical state as well, we proposed that the drug exerted a positive anxiolytic influence, whether this was indirectly via reduction of procedural pain, or directly acting on anxiety levels, or both. Premedication with midazolam as well as concomitant use of additional drugs including opioids and other analgesics given perioperatively was unlikely to have any direct impact on anxiolytic effects, since patients were asked to fill in the questionnaires approximately 48 h following surgery, which was at least 12 h following opioid administration and while patients had adequate plasma levels of parecoxib following regular administration. Midazolam was given even before the block. On the other hand, it should be noted that patients were still under parecoxib effect when asked to fill in the questionnaires.
Potential limitations of the current protocol should be also taken into consideration. For instance, one could argue that the anxiety levels measured were indeed associated with the personality characteristics and not the procedure followed, although especially for this reason STAI was the method of choice. Nonetheless, the current findings are in agreement with our previous study that investigated whether parecoxib, preemptively administrated, had an effect on anxiety levels during epidural catheter placement for surgical operations. More specifically, we have previously shown that 40 mg of parecoxib, administered intravenously 20 min before the interventional technique, could improve patients’ anxiety levels, experienced prior to an epidural catheter placement [17].
Collectively, since intravenous infusion of parecoxib has been shown to provide non-steroidal anti-inflammatory drug-mediated central hyperanalgesia, attributed to central COX-2 inhibition [20], it is possible that it also exerts a positive anxiolytic effect prior to a distressing and painful procedure such as TKA. In addition, taking into account the fact that in anxiety the prefrontal cortex and amygdala, which are involved in analgesia and hyperanalgesia demonstrate concurrent areas of activation in the brain [21], it was only rational to assume that pre-emptively administered parecoxib was capable of having an anxiolytic effect prior to surgery.
Conclusions
Our study demonstrated that parecoxib has an anxiolytic effect in patients undergoing TKA with continuous femoral block. Nevertheless, additional studies are necessitated to unravel the complex relationship and the mechanisms underlying the association between anxiety and pain, so as to be able to introduce parecoxib as a new prophylactic regime or treatment modality in the management of pain-related anxiety.
Author Contribution
Authorship All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Medical writing, editorial, and other assistance DGS participated in the design of the study, performed all experiments, collected and evaluated patients’ clinical data, and drafted the manuscript. GC and CA assisted in the performance of experiments. MB performed data analyses and interpretation, and assisted in drafting the manuscript. IS and AV conceived, designed, and coordinated the study and revised the manuscript draft.
Disclosures
D. G. Sarridou, C. Georgia, B. Maria, S. Ioanna, A. Chrisi and V. Athina claim no conflict of interest. No funding or sponsorship was received for this study or publication of this article.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
References
- 1.Mok LC, Lee IF. Anxiety, depression and pain intensity in patients with low back pain who are admitted to acute care hospitals. J Clin Nurs. 2008;17:1471–1480. doi: 10.1111/j.1365-2702.2007.02037.x. [DOI] [PubMed] [Google Scholar]
- 2.Ciccozzi A, Marinangeli F, Colangeli A, Di Stefano L, Antonucci S, Pilerci G, Varassi G. Anxiolysis and postoperative pain in patients undergoing spinal anesthesia for abdominal hysterectomy. Minerva Anesthesiol. 2007;73:387–393. [PubMed] [Google Scholar]
- 3.McCracken LM, Gross RT, Sorg PJ, Edmands TA. Prediction of pain in patients with chronic low back pain: effects of inaccurate prediction and pain-related anxiety. Behav Res Ther. 1993;31:647–652. doi: 10.1016/0005-7967(93)90117-D. [DOI] [PubMed] [Google Scholar]
- 4.Keogh E, Cochrane M. Anxiety sensitivity, cognitive biases, and the experience of pain. J Pain. 2002;3:320–329. doi: 10.1054/jpai.2002.125182. [DOI] [PubMed] [Google Scholar]
- 5.Thomas JS, France CR. Pain-related fear is associated with avoidance of spinal motion during recovery from low back pain. Spine (Phila Pa 1976). 2007;32:E460–6. [DOI] [PubMed]
- 6.Poiraudeau S, Rannou F, Baron G, Le Henanff A, Coudeyre E, Rozenberg S, Le Henanff A, Coudeyre E, Rozenberg S, et al. Fear-avoidance beliefs about back pain in patients with subacute low back pain. Pain. 2006;124:305–311. doi: 10.1016/j.pain.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 7.Edwards RR, Klick B, Buenaver L, Max MB, Haythornthwaite JA, Keller RB, Atlas SJ. Symptoms of distress as prospective predictors of pain-related sciatica treatment outcomes. Pain. 2007;130:47–55. doi: 10.1016/j.pain.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 8.Capdevila X, Biboulet P, Morau D, Bernard N, Deschodt J, Lopez S, et al. Continuous three-in-one block for postoperative pain after lower limb orthopedic surgery: where do the catheters go? Anesth Analg. 2002;94:1001–6 (table of contents). [DOI] [PubMed]
- 9.Morin AM, Kratz CD, Eberhart LH, Dinges G, Heider E, Schwarz N, et al. Postoperative analgesia and functional recovery after total-knee replacement: comparison of a continuous posterior lumbar plexus (psoas compartment) block, a continuous femoral nerve block, and the combination of a continuous femoral and sciatic nerve block. Reg Anesth Pain Med. 2005;30:434–445. doi: 10.1016/j.rapm.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 10.Oda A, Iida H, Dohi S. Patient anxiety scores after low-dose ketamine or fentanyl for epidural catheter placement. Can J Anaesth. 2000;47:910–913. doi: 10.1007/BF03019675. [DOI] [PubMed] [Google Scholar]
- 11.Nishiyama T. Propofol infusion for sedation during spinal anesthesia. J Anesth. 2007;21:265–269. doi: 10.1007/s00540-006-0489-3. [DOI] [PubMed] [Google Scholar]
- 12.Halim B, Schneider I, Claeys MA, Camu F. The use of midazolam and flumazenil in locoregional anaesthesia: an overview. Acta Anaesthesiol Scand Suppl. 1990;92:42–46. doi: 10.1111/j.1399-6576.1990.tb03181.x. [DOI] [PubMed] [Google Scholar]
- 13.Rama-Maceiras P, Gomar C, Criado A, Arízaga A, Rodríguez A, Marenco ML. Sedation in surgical procedures using regional anesthesia in adult patients: results of a survey of Spanish anesthesiologists. Rev Esp Anestesiol Reanim. 2008;55:217–226. doi: 10.1016/S0034-9356(08)70552-8. [DOI] [PubMed] [Google Scholar]
- 14.Koyama S, Ohashi N, Kurita S, Nakatani K, Nagata N, Toyoda Y. Conscious sedation and amnesic effect of intravenous low-dose midazolam prior to spinal anesthesia. Masui. 2008;57:713–718. [PubMed] [Google Scholar]
- 15.Hidaka S, Kawamoto M, Kurita S, Yuge O. Comparison of the effects of propofol and midazolam on the cardiovascular autonomic nervous system during combined spinal and epidural anesthesia. J Clin Anesth. 2005;17:36–43. doi: 10.1016/j.jclinane.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Shafer A. Complications of sedation with midazolam in the intensive care unit and a comparison with other sedative regimens. Crit Care Med. 1998;26:947–956. doi: 10.1097/00003246-199805000-00034. [DOI] [PubMed] [Google Scholar]
- 17.Vadalouca A, Moka E, Chatzidimitriou A, Siafaka I, Sikioti P, Argyra E. A randomized, double-blind, placebo-controlled study of preemptively administered intravenous parecoxib: effect on anxiety levels and procedural pain during epidural catheter placement for surgical operations or for chronic pain therapy. Pain Pract. 2009;9:181–194. doi: 10.1111/j.1533-2500.2009.00271.x. [DOI] [PubMed] [Google Scholar]
- 18.Baharuddin KA, Rahman NH, Wahab SF, Halim NA, Ahmad R. Intravenous parecoxib sodium as an analgesic alternative to morphine in acute trauma pain in the emergency department. Int J Emerg Med. 2014;7:2. doi: 10.1186/1865-1380-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spielberger C, Gorsuch R, Lushene R. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire). In: Alto P, editor. CA: Consulting Psychologists Press; 1970.
- 20.Jain NK, Patil CS, Kulkarni SK, Singh A. Modulatory role of cyclooxygenase inhibitors in aging- and scopolamine or lipopolysaccharide-induced cognitive dysfunction in mice. Behav Brain Res. 2002;133:369–376. doi: 10.1016/S0166-4328(02)00025-6. [DOI] [PubMed] [Google Scholar]
- 21.Symreng I, Fishman S. Anxiety and pain. In: Pain clinical updates, vol. XII. Settle: International Association for the Study of Pain—IASP; 2004. p. 1–6.