Abstract
This technical note discusses the arthroscopic coracoid cerclage technique for double-bundle coracoclavicular ligament reconstruction in patients with nonacute symptomatic high-grade acromioclavicular separation injuries. This technique allows for an anatomic graft reconstruction of the coracoclavicular ligaments through an arthroscopic approach without the requirement to drill into the coracoid process. Early results are promising with high patient satisfaction and excellent reported clinical and radiographic outcomes. We believe this technique to be an anatomic, less invasive alternative to a complex shoulder procedure while sparing the structural integrity of the coracoid process and also allowing the surgeon to convert easily to a more traditional open surgical technique as necessary.
Blunt injuries to the acromioclavicular (AC) joint are among the more common injury patterns to the shoulder in athletes leading to pain, disability, and associated decreased function and performance.1 Typically resulting from a direct blow to the acromion, these injuries result in increasing degrees of AC displacement and ligament disruption having been historically classified as type I to type VI.2 Type I and II injuries have minimal AC joint displacement, the coracoclavicular (CC) ligaments are characteristically intact, and these injuries tend to heal uneventfully with nonoperative management. Types III to VI are higher energy injuries that result in significant displacement of the AC joint representing complete disruption of the CC ligament complex, considerable pain, disability, and deformity.1, 3 Types IV to VI are typically treated surgically, whereas type III injuries are still being debated for a consensus on optimal treatment.4, 5
A wide variety of CC ligament reconstruction techniques have been developed in an effort to identify an optimal approach to this challenging shoulder injury. The current techniques described are both arthroscopic and open using either allograft or autograft tissue. They include anatomic versus nonanatomic configurations and varying degrees of coracoid drilling techniques. Although many of these techniques have shown good results, they each have advantages and disadvantages with regard to risk, patient satisfaction, and functional outcomes.3, 6, 7, 8
We present an all-arthroscopic “coracoid cerclage” technique for patients with high-grade, type IV to VI, AC separations that are greater than 4 weeks from injury. The described technique carries the advantages of a completely arthroscopic procedure and an anatomic graft reconstruction of the CC ligaments without the associated risk of coracoid drilling. Early reports from the use of this technique suggest a low complication rate, reliable maintenance of AC joint reduction, excellent functional outcomes, and patient satisfaction.9
Surgical Technique
The patient is placed in the beach chair position using a Spider hydraulic arm holder (Tenet Medical, Calgary, Alberta, Canada). A 30° arthroscope (Smith and Nephew, Andover, MA) is inserted into the glenohumeral joint through a posterior portal. An anterior rotator interval portal is established with an outside-in technique using a spinal needle to verify position. The needle is replaced with an 8.25-mm Smith and Nephew Clear Trac threaded arthroscopic shoulder cannula.
A complete diagnostic arthroscopy of the glenohumeral joint is performed. Associated intra-articular pathology is documented and addressed as indicated. A motorized shaver blade (Smith and Nephew) is introduced through the anterior cannula and used to debride the rotator interval until the base of the coracoid can be visualized (Fig 1, Video 1). A 70° arthroscope is used to visualize and expose the coracoid base (Table 1). For direct trajectory toward the coracoid base, an anterior-lateral portal is established using a spinal needle in line with the subscapularis tendon. The needle is replaced with an 8.25-mm arthroscopic cannula. Through this portal a motorized shaver blade and radiofrequency device are used to fully expose the inferior base of the coracoid process.
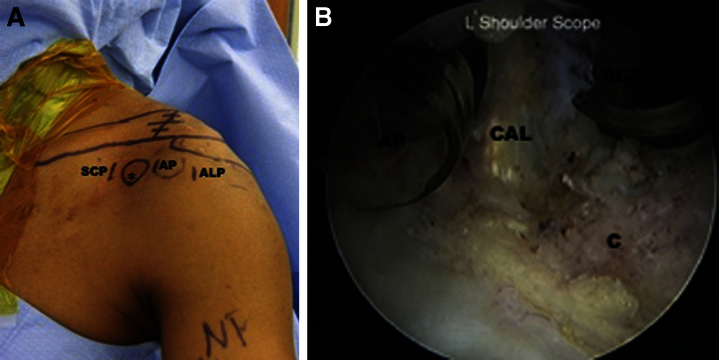
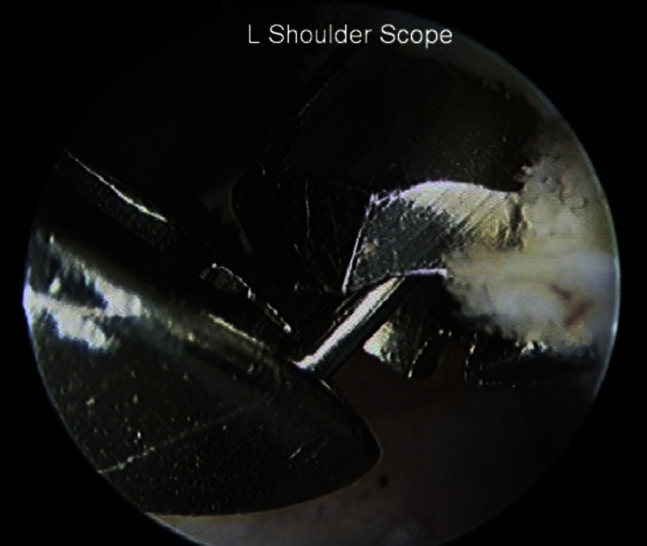
Fig 1.
The rotator interval is resected to expose the base of the coracoid. (L, left.)
Table 1.
Pearls, Pitfalls, Key Points, and Indications
| Pearls |
|---|
| Use of a 70° arthroscope can be very helpful in visualization near the base of the coracoid. |
| The anterolateral portal provides an optimal trajectory for clearing away the soft tissue from the base of the coracoid. |
| Be familiar with the order of placement of and passing of the shuttling devices and sutures to allow an uncomplicated graft passage around the coracoid. |
| Meticulous preparation of the leading end of the graft will ease its passage around the coracoid. |
| It is helpful to have an experienced assistant perform the drilling of the conoid and trapezoid guidewires and tunnels while the surgeon visualizes his or her approach to the guide target. |
| During the tensioning of the graft around the coracoid, use simultaneous downward displacement of the clavicle with superior displacement of the scapulohumeral complex to minimize any excess slack in the graft before fixation. |
| During the fixation of the graft in the clavicular tunnels, pull the graft superiorly and in line with both its tunnel and 5.5-mm PEEK (polyether ether ketone) screw to minimize the risk of graft tearing between the bone and the screw. |
| Verify an acceptable position of the reduced acromioclavicular joint with a Zanca radiograph before fixation with the second PEEK screw. |
| Place the patient in a gunslinger brace before awaking from anesthesia to minimize undue stress to the reconstruction. |
| Pitfalls |
| Debridement near the base of the coracoid poses particular risk to the musculocutaneous nerve if dissection drifts medially or inferiorly. |
| Anterior and anterolateral 8.25-mm cannulated portals placed too close together in the anterior shoulder can cause crowding of the cannulas making coracoid dissection difficult. |
| A suboptimally prepared graft without a smooth contoured leading edge will more easily be caught up in the soft tissues during passage around the coracoid. |
| The surgeon should be familiar with the detailed anatomy of the anterior shoulder as well as the open approach technique for coracoclavicular ligament reconstruction before use of this technique. |
| Key Points |
| This technique carries the advantages of an arthroscopic approach to anatomic coracoclavicular ligament reconstruction while preserving the structural integrity of the coracoid process. |
| If necessary this approach can be extended to a traditional open approach at any stage during the procedure. |
| Indications |
| This technique is indicated for chronic (>4 weeks) type III to V acromioclavicular joint separations. |
PEEK, polyether ether ketone.
At this point the supracoracoid (anterior-medial) portal is established using a spinal needle with an outside-in technique. The portal is placed in line with the medial border of the coracoid, midway between the coracoid and the clavicle along the medial border of the coracoacromial ligament. An 8.25-mm arthroscopic cannula is placed through this portal (Fig 2). A 45° suture shuttling device (Arthrex, Naples, FL) is used through the supracoracoid portal and placed down the medial border of the coracoid until identified about the coracoid base. The shuttle suture is retrieved via the anterior portal to shuttle a suture loop below the coracoid (Fig 3).
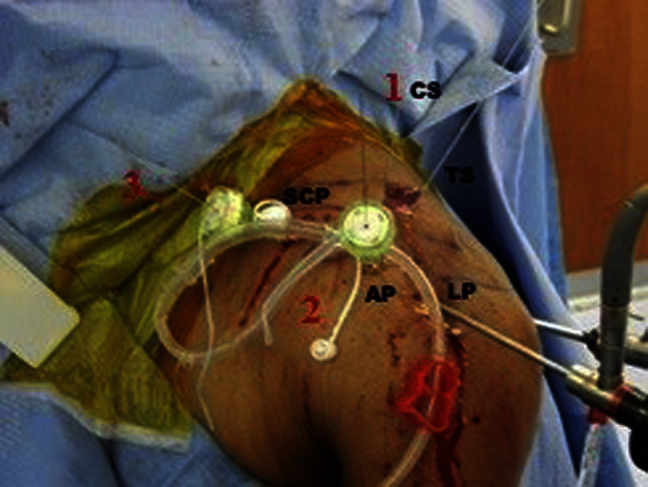
Fig 2.
(A) The anatomic landmarks and portal positions are marked. The SCP is located between the coracoid (asterisk) and the clavicle on the palpable medial border of the coracoid. This is always made using the outside-in technique. (B) An 8.25-mm arthroscopic cannula is placed through the supracoracoid portal while viewing from the posterior portal using a 70° arthroscope. The supracoracoid portal is placed along the medial border of the coracoacromial ligament. (ALP, anterior lateral portal; AP, anterior portal; C, coracoid bone; CAL, coracoacromial ligament; L, left; SCP, supracoracoid portal.)
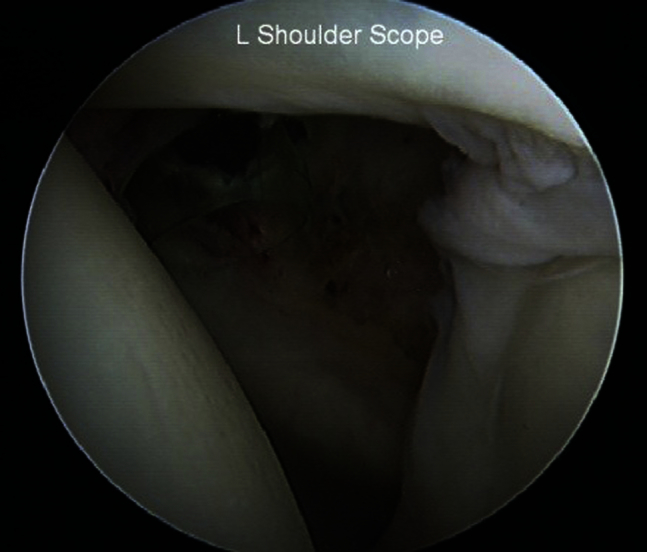
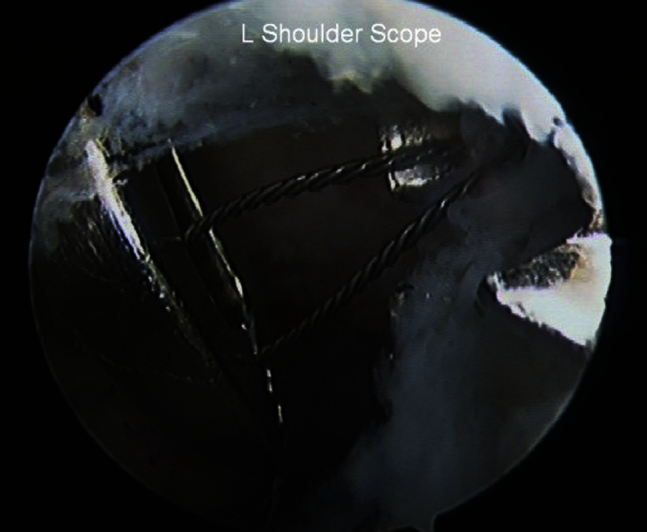
Fig 3.
A 45° suture shuttling device is used through the supracoracoid portal to shuttle a suture loop below the coracoid while viewing through the posterior portal using a 70° arthroscope. (C, coracoid.)
A 2-cm incision is made perpendicular to the clavicular axis 3.5 cm medial to the AC joint. The deltotrapezial fascia is released off the clavicle to obtain access to the superior cortex. Up to 8 mm of the distal clavicle may be removed using an arthroscopic or open technique if there is evidence of AC joint arthrosis or hyperostosis on preoperative radiographs.
The arthroscope is placed through the anterolateral portal to improve visualization of the coracoid base. The target end of the drill guide (Arthrex) for the clavicle bone tunnels is placed through the anterior portal just lateral to the base of the coracoid. The drill sleeve of the guide is positioned over the posterior third of the clavicle approximately 4.5 cm medial to the distal clavicle edge. A guide pin is used for placement of the conoid tunnel. Once the guide pin is inserted in the direction of the eventual bone tunnel and its tip is visualized at the desired position, the 5.5-mm cannulated headed reamer is used over the guide pin to fashion the bone tunnel. The guide pin is removed and the nonlooped end of a flexible nitinol passing wire is delivered through the cannulated reamer and retrieved via the anterior portal before removal of the reamer (Fig 4).
Fig 4.
A guide pin is used for the placement of the conoid tunnel approximately 4.5 cm medial to the distal clavicle edge. The nonlooped end of a flexible nitinol passing wire is delivered through the cannulated reamer and retrieved via the anterior portal. (L, left.)
The target end of the drill guide is then placed via the supracoracoid portal or anterior portal just superior to the coracoid. The drill sleeve of the guide is positioned over the middle third of the clavicle approximately 2.5 cm medial to the distal clavicle edge. A guide pin is used for placement of the trapezoid tunnel. Once the guide pin is inserted in the direction of the eventual bone tunnel and its tip is visualized at the desired position, the 5.5-mm cannulated headed reamer is used over the guide pin to fashion the bone tunnel. The guide pin is removed and a flexible nitinol passing wire is delivered through the reamer and retrieved via the supracoracoid portal before removal of the cannulated reamer (Fig 5). Figure 6 illustrates all passing wires and sutures in place before graft passage.
Fig 5.
A guide pin is used for placement of the trapezoid tunnel approximately 2.5 cm medial to the distal clavicle edge. The looped end of a flexible nitinol passing wire is delivered through the cannulated reamer and retrieved via the supracoracoid portal. (L, left.)
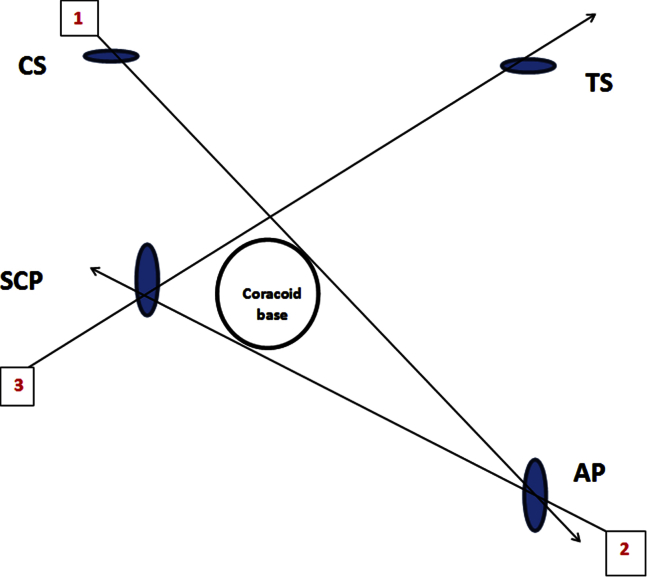
Fig 6.
Wires and sutures are in position for graft shuttling. (AP, anterior portal; CS, conoid tunnel; LP, anterolateral portal; SCP, supracoracoid portal; TS, trapezoid tunnel.)
Reproduced with permission.9
A soft tissue auto or allograft (commonly nonirradiated semitendinosis) is prepared on the back table. Several running locked sutures are placed in the leading free end of the graft. The graft length should be a minimum of 10 cm, and the graft should pass through a 5.5-mm sizing block.
Leading end graft sutures are loaded on the flexible loop on the previously placed passing wire. The graft is first pulled through the conoid clavicle tunnel exiting the anterior portal. Using the suture loop that was previously placed under the coracoid, the leading end of the graft is then shuttled from lateral to medial below the coracoid exiting the supracoracoid portal. The graft is then shuttled through the supracoracoid portal, exiting the trapezoid clavicle tunnel, creating a crossing pattern (Fig 7). Figure 8 is a schematic representation of the sequence used for graft passage in the technique.
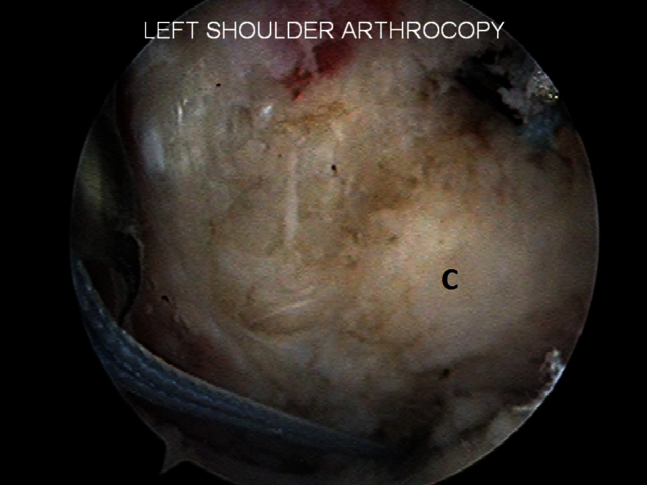
Fig 7.
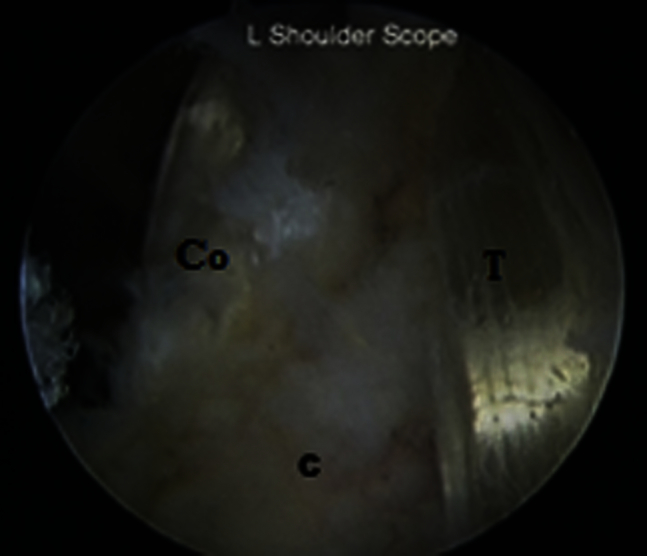
The graft is shuttled around the coracoid and through the clavicle tunnels in a crossing pattern. (C, coracoid; Co, conoid; L, left; T, trapezoid.)
Reproduced with permission.9
Fig 8.
Schematic representation of graft transfer sequence for the coracoid cerclage technique. Step 1: the leading end graft sutures are pulled through the conoid clavicle tunnel exiting the anterior portal. Step 2: using the suture loop that was previously placed under the coracoid; the leading end of the graft is then shuttled from lateral to medial below the coracoid exiting the supracoracoid portal. Step 3: the graft is shuttled through the supracoracoid portal exiting the trapezoid clavicle tunnel creating a crossing pattern. (AP, anterior portal; CS, conoid tunnel; SCP, supracoracoid portal; TS, trapezoid tunnel.)
Reproduced with permission.9
Simultaneous superior displacement of the scapulohumeral complex and inferior displacement of the clavicle reduces the AC joint. At this point, both graft ends are advanced superiorly through the tunnels confirming maximal tightness. Once reduction is confirmed via intraoperative Zanca radiograph, a 5.5 mm × 8 mm PEEK (polyether ether ketone) tenodesis screw (Arthrex) is placed in the conoid bone tunnel. After verification that initial screw fixation has been successful, the second PEEK tenodesis screw is placed in the trapezoid bone tunnel (alternatively a square knot tied with both free graft ends can be used). The remaining portions of the tendon graft are then sewn to each other using a No. 2 nonabsorbable braided suture. The graft ends are then be placed laterally and secured with a No. 2 nonabsorbable braided suture to the AC joint capsule. The arthroscopic portals are closed with interrupted subcutaneous monofilament sutures, whereas the clavicular wound is closed in layers.
Postoperatively, the patient is placed into a gunslinger brace for 6 weeks. The patient is allowed to elbow range of motion in the supine position. Active and passive motion is allowed after 6 weeks. From 6 to 12 weeks rehabilitation is focused on gradual regaining of normal shoulder mechanics and range of motion. Resistance exercises are allowed after 12 weeks. Contact athletics are allowed after 6 months.
Discussion
Biomechanical and clinical studies have shown superiority of anatomic reconstructions of the CC ligaments using free tendon grafts in comparison with nonanatomic ligamentoplasty procedures. Anatomic reconstructions more closely reproduce the function of the native ligaments and show greater stability and load to failure.10 However, the open technique as described by Carofino and Mazzoca11 carries several potential risks including extensive soft tissue dissection, detachment of the deltoid from the clavicle for graft transfer around the coracoid base, and suboptimal visibility around the coracoid process during the graft transfer that may endanger the neurovascular structures.
To overcome the above-noted challenges, several arthroscopic techniques have been developed and are widely used today.3, 6, 7, 8 These techniques may permit greater visibility of the base of the coracoid with less soft tissue dissection; all but 1 of these techniques use a single clavicular tunnel and require drilling of the coracoid base for graft fixation. This creates risk of coracoid fracture, as the high load to failure of the graft or fixation device may exceed load to failure of cortical bone before device breakage. In fact, Coale et al.12 found in their study that transclavicular-transcoracoid reconstructive techniques cannot restore the footprint of the conoid and trapezoid ligaments without significant risk of cortical breach and fracture. Once the integrity of the coracoid is compromised, it may not be wise to pass a graft under the coracoid and fix it under tension with a tunnel drilled through any portion of it that gives limited options to salvage the reconstruction in the same operation.
Complications of coracoid fracture and/or early failure have been reported in multiple studies for these reconstructive techniques. Milewski et al.13 reported an 80% complication rate in the coracoid tunnel group with 20% being coracoid fractures. Cook et al.14 reported 80% early failure with CC ligament reconstruction using the GraftRope technique.
In contrast, Carofino and Mazzoca11 had 17 patients who underwent open anatomic CC reconstruction using the coracoid cerclage technique. They did not report any coracoid fractures and only 1 failure of reduction. In our experience with young military patients using the CC ligament double-bundle coracoid cerclage technique, there have been no failures of reduction or coracoid fractures.
The greatest advantage of an arthroscopic anatomic reconstruction of the CC ligaments using a cerclage technique is the avoidance of drilling the coracoid bone. The technique uses the supracoracoid portal that is located midway between the medial border of the coracoid and the clavicle. Lo et al.15 showed in their study on neurovascular structures around the coracoid that this area is safe. We use an outside-in technique to optimize the placement of this portal.
Another advantage of the current technique is that it reproduces the anatomic insertion of the 2 CC ligaments on the clavicle. This insertion is accomplished by using 2 bone tunnels to fix the tendon graft to the clavicle. The tunnels are well within the area found by Geaney et al.16 to have optimal bone density (between 25 and 50mm from the lateral edge of the clavicle).
The described coracoid cerclage technique incorporates potential benefits of an all-arthroscopic approach, anatomic graft reconstruction, and maintains the structural integrity of the coracoid. Moreover, should the surgeon encounter challenges with the procedure, the approach can be easily converted to a traditional open approach. Although we believe that our technique offers considerable advantages with excellent early follow-up, it can be technically challenging. This technique should be attempted by surgeons who are familiar with the anatomy of the anterior shoulder and who are competent in both arthroscopic and open reconstruction techniques.
Footnotes
The authors report that they have no conflict of interest in the authorship and publication of this article.
Supplementary Data
Arthroscopic reconstruction of a high-grade acromioclavicular (AC) separation in a left shoulder using an arthroscopic coracoid cerclage technique. The patient is in the beach chair position and the primary viewing portal is posterior. A diagram of the graft passage sequence is included.
References
- 1.Mazzocca A.D., Arciero R.A., Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35:316–329. doi: 10.1177/0363546506298022. [DOI] [PubMed] [Google Scholar]
- 2.Rockwood C.J., Williams G., Young D. Disorders of the acromioclavicular joint. In: Rockwood C.J., Matsen F.A. III, editors. The shoulder. Ed 2. WB Saunders; Philadelphia: 1998. pp. 483–553. [Google Scholar]
- 3.DeBerardino T.M., Pensak M.J., Ferreira J., Mazzocca A.D. Arthroscopic stabilization of acromioclavicular joint dislocation using the AC graftrope system. J Shoulder Elbow Surg. 2010;19:47–52. doi: 10.1016/j.jse.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 4.De Carli A., Lanzetti R.M., Ciompi A., Lupariello D., Rota P., Ferretti A. Acromioclavicular third degree dislocation: Surgical treatment in acute cases. J Ortho Surg Res. 2015;10:13–20. doi: 10.1186/s13018-014-0150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stucken C., Cohen B. Management of acromioclavicular joint injuries. Ortho Clin N Am. 2015;1:57–66. doi: 10.1016/j.ocl.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Scheibel M., Ifesanya A., Pauly S., Haas N.P. Arthroscopically assisted coracoclavicular ligament reconstruction for chronic acromioclavicular joint instability. Arch Orthop Trauma Surg. 2008;128:1327–1333. doi: 10.1007/s00402-007-0547-9. [DOI] [PubMed] [Google Scholar]
- 7.Salzmann G.M., Walz L., Buchmann S., Glabgly P., Venjakob A., Imhoff A.B. Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med. 2010;38:1179–1187. doi: 10.1177/0363546509355645. [DOI] [PubMed] [Google Scholar]
- 8.Yoo Y.S., Seo Y.J., Noh K.C., Patro B.P., Kim D.Y. Arthroscopically assisted anatomical coracoclavicular ligament reconstruction using tendon graft. Int Orthop. 2011;35:1025–1030. doi: 10.1007/s00264-010-1124-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parnes N., Friedman D., Phillips C., Carey P. Outcome after arthroscopic reconstruction of the coracoclavicular ligaments using a double-bundle coracoid cerclage technique. Arthroscopy. 2015;31:1933–1940. doi: 10.1016/j.arthro.2015.03.037. [DOI] [PubMed] [Google Scholar]
- 10.Thomas K., Litsky A., Jones G., Bishop J.Y. Biomechanical comparison of coracoclavicular reconstructive techniques. Am J Sports Med. 2011;39:804–810. doi: 10.1177/0363546510390482. [DOI] [PubMed] [Google Scholar]
- 11.Carofino B.C., Mazzocca A.D. The anatomic coracoclavicular ligament reconstruction: Surgical technique and indications. J Shoulder Elbow Surg. 2010;19:37–46. doi: 10.1016/j.jse.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Coale R.M., Hollister S.J., Dines J.S., Allen A.A., Bedi A. Anatomic considerations of transclavicular-transcoracoid drilling for coracoclavicular ligament reconstruction. J Shoulder Elbow Surg. 2013;22:137–144. doi: 10.1016/j.jse.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Milewski M.D., Tompkins M., Giugale J.M., Carson E.W., Miller M.D., Diduch D.R. Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2012;40:1628–1634. doi: 10.1177/0363546512445273. [DOI] [PubMed] [Google Scholar]
- 14.Cook J.B., Shaha J.S., Rowles D.J., Bottoni C.R., Shaha S.H., Tokish J.M. Early failures with single clavicular transosseous coracoclavicular ligament reconstruction. J Shoulder Elbow Surg. 2012;21:1746–1752. doi: 10.1016/j.jse.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 15.Lo I.K., Burkhart S.S., Parten P.M. Surgery about the coracoid: Neurovascular structures at risk. Arthroscopy. 2004;20:591–595. doi: 10.1016/j.arthro.2004.04.060. [DOI] [PubMed] [Google Scholar]
- 16.Geaney L.E., Beitzel K., Chowaniec D.M. Graft fixation is highest with anatomic tunnel positioning in acromioclavicular reconstruction. Arthroscopy. 2013;29:434–439. doi: 10.1016/j.arthro.2012.10.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic reconstruction of a high-grade acromioclavicular (AC) separation in a left shoulder using an arthroscopic coracoid cerclage technique. The patient is in the beach chair position and the primary viewing portal is posterior. A diagram of the graft passage sequence is included.