Abstract
Interest and knowledge on the anatomy, function, and biomechanical properties of the anterolateral ligament has led to the recognition of the importance of this structure in rotational control of the knee. This article describes a technique that allows for a combined anterior cruciate ligament (ACL) and anterolateral reconstruction, using an Iliotibial band (ITB) autograft. The graft is detached from the vastus lateralis from proximal to distal, at the center portion from ITB, preserving its distal insertion on the Gerdy tubercle. Its width is 1 cm for the distal part, used for the anterolateral ligament reconstruction, and 3 cm for the proximal part. An outside-in femoral tunnel is drilled respecting both the preferred favorable isometric femoral insertion site and the femoral ACL footprint. An ACL reconstruction combined with a lateral tenodesis with a continuous ITB graft respects the anatomical and isometric rules providing superior internal rotational control of the knee in comparison with a stand-alone ACL reconstruction.
During the last few years, an increasing number of anatomical and biomechanical studies on the anterolateral structures have renewed the scientific interest on extra-articular tenodesis (EAT). Internal rotational control in relation to the anterolateral structures was suggested in the publications by Segond,1 Hughston et al.,2 and Muller,3 following the description of the extra-articular procedures by Lemaire4 and MacIntosh and Darby.5
The debate on deficient internal rotational control6 provided by an isolated anterior cruciate ligament (ACL) reconstruction led to the identification of the anterolateral ligament (ALL).7
Our purpose is to describe a technique of arthroscopic reconstruction of the ACL in combination with a lateral tenodesis using an iliotibial band (ITB) autograft.
Surgical Technique
This technical note describes step by step our technique of combined anterior and anterolateral stabilization of the knee with an continue ITB autograft (Video 1). Advantages, risks and limitations are summarized in Table 1.
Table 1.
Advantages, Risks and Limitations of the Techniques
| Advantages | Risks and Limitations |
|---|---|
| ACL and ALL reconstruction with a unique autologous graft | Hematoma lateral part of the thigh |
| Low morbidity of ITB harvesting | Muscular hernia on the proximal part of harvesting |
| Minimally invasive (skin incision, arthroscopic technique) | Limitation ROM in case of the nonisometric placement of the graft |
| Minimal additional operative time and equipment | Graft too short or too thin |
ACL, anterior cruciate ligament; ALL, anterolateral ligament; ITB, iliotibial band; ROM, range of motion.
Patient Positioning
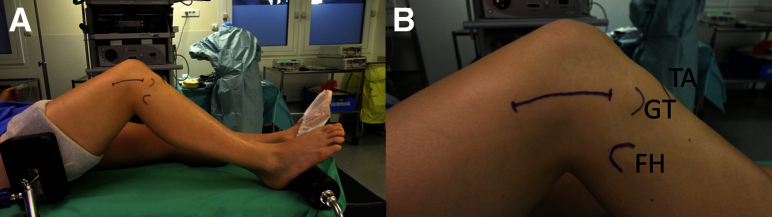
The patient is placed in the supine position with the knee flexed at 70°, stabilized with a lateral post (Maquet Getinge Group, Rastatt, Germany) and a foot bar (Maquet Getinge Group) so that the knee can be mobilized from full extension up to 120° flexion. A tourniquet is applied at the upper thigh (Fig 1A).
Fig 1.
(A) Patient positioning. (B) Surface making of the skin incision—fibular head (FH), Gerdy's tubercle (GT), and tibial anterior tuberosity (TA).
Harvesting the Iliotibial Band
The skin incision begins 2 cm proximal to the Gerdy tubercle (GT), approximately 10 cm in length. As the knee is flexed, the incision is curved slightly on its distal part so it becomes straight when the knee is in extension (Fig 1B).
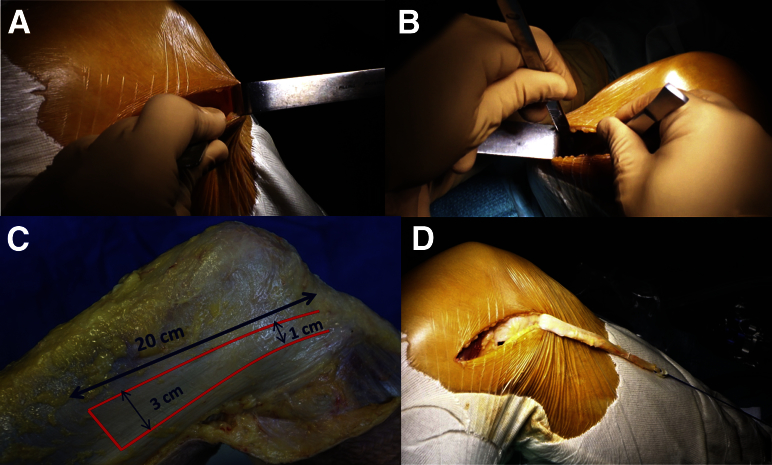
Harvesting of the ITB begins at the GT. Exposure is achieved with a Farabeuf retractor (Landanger, Chaumont, France) (Fig 2A) and the posterior ridge from the GT is incised with a No. 23 blade and extended proximally after the posterior part of the ITB for 5 to 6 cm; a second incision is made 1 cm anterior and parallel to the previous incision, so the graft width is 1 cm at this distal part.
Fig 2.
Harvesting iliotibial band (ITB). (A) Distal exposure. (B) Proximal exposure. (C) Size of the graft. (D) Tubulization of the graft.
The proximal part of the ITB is then exposed (Fig 2B), on its center portion, with a large retractor (B Braun Aesculap, Tuttlingen, Germany) for adequate exposure, and proximal extension of the posterior incision is performed with a No. 11 blade with a long handle, to obtain a total graft length of approximately 20 cm. The anterior incision is then made to obtain a 3-cm-wide graft on its proximal part (Fig 2C).
The distal part of the ITB is separated from its deep fibers with a No. 23 blade, keeping in mind that the graft must be kept attached to its insertion on GT.
The fat pad is cleared from the graft and “tubulization” performed with No. 2-0 Vicryl sutures (Ethicon, Somerville, NJ) at the free end proximally for approximately 3 cm. A No. 2 Vicryl suture (Ethicon) is passed through the free margin of the ITB as traction suture (Fig 2D).
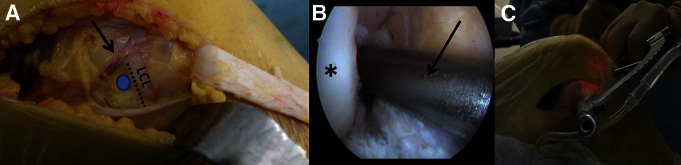
Extra-articular Landmark of the Femoral Tunnel
This point is located 5 mm proximal and posterior to the lateral epicondyle, at the lateral collateral ligament insertion, just under genicular vessels (Fig 3A). It will constitute the femoral attachment for the ALL. The landmark is marked with an electric cautery. Graft isometry can be tested by using 2 K-wires placed at the GT and at the femoral point; a suture is looped around the K-wires and flexion and/or extension of the knee is performed to determine the best femoral placement of the tunnel.
Fig 3.
Femoral tunnel. (A) Extra-articular femoral landmark—lateral collateral ligament (LCL). The arrow indicates the Lemaire vessels; the blue circle shows the landmark. (B) Intra-articular femoral guide positioning. The asterisk indicates the lateral condyle; the arrow indicates the femoral guide. (C) Extra-articular femoral guide fixation.
Tunnels
Femoral Tunnel
The tip of the guide (FH Orthopedics, Heimsbrunn, France) is inserted into the medial portal and placed so that the intra-articular guide pin enter 5 mm distal to the notch outlet between 10 and 11 o'clock on the right knee (Fig 3B) and between 1 and 2 o'clock on the left knee.
The guide is fixed over the extra-articular femoral landmark previously set (Fig 3C). Care must be taken to ensure that the guide is horizontal in the sagittal plane and perpendicular to the femoral condyle in the axial and/or transverse plane. The drill is then pushed through the guide and a 7-mm reamer (Orthomed SAS, St Jeannet, France) is used to prepare the tunnel.
Tibial Tunnel
The angle of the tibial guide (Orthomed SAS) is set to 45°. The tip of the guide is placed just medial to the lateral tibial spine and anterior to the posterior cruciate ligament, centering the ACL remnant (Fig 4A). The extra-articular guide is positioned on the medial cortex through a small skin incision, approximately 15 mm above the anterior tibial tuberosity (Fig 4B). Tibial tunnel drilling is done with a 6- or 7-mm reamer (Orthomed SAS) depending of the graft size (Fig 4C).
Fig 4.
Tibial tunnel. (A) Intra-articular tibial guide positioning (asterisk shows the lateral tibial spine). (B) Extra-articular tibial guide positioning. (C) Intra-articular tunnel placement.
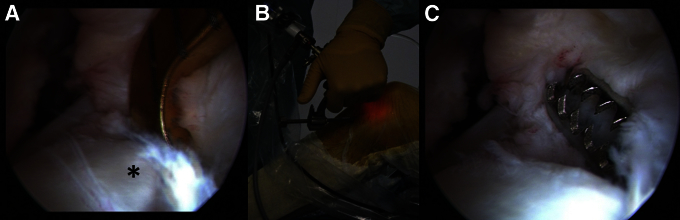
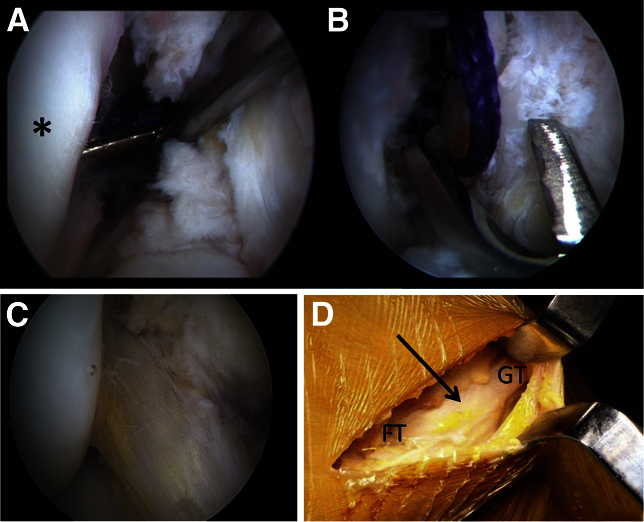
Passage of the Graft
The traction suture is passed through the femoral tunnel, in an outside-in direction and then recovered with a grasper through the medial portal (Fig 5A). It is then placed close to the intra-articular hole of the tibial tunnel and subsequently pulled out of the tibial tunnel with an arthroscopic grasper (Fig 5B). Care should be taken to avoid twisting of the extra-articular part of the graft. Adequate placements of the ACL reconstruction (Fig 5C) and the ALL reconstruction (Fig 5D) are checked.
Fig 5.
Graft passage. (A) Femoral recovering of the puller suture (asterisk indicates the lateral condyle). (B) Arthroscopic grasper trough the tibial tunnel. (C) Anterior cruciate ligament (ACL) reconstruction. (D) Anterolateral ligament (ALL) reconstruction. The arrow indicates the anterolateral ligament. (FT, femoral tunnel; GT, Gerdy tubercle.)
Fixation of the Graft
Before fixation, graft isometry is tested by bending the knee from 120° of flexion to full extension. Variation of length during range of motion (ROM) should not exceed 2 or 3 mm. The knee is maintained in 30° of flexion and neutral rotation (Fig 6) during graft fixation.
Fig 6.
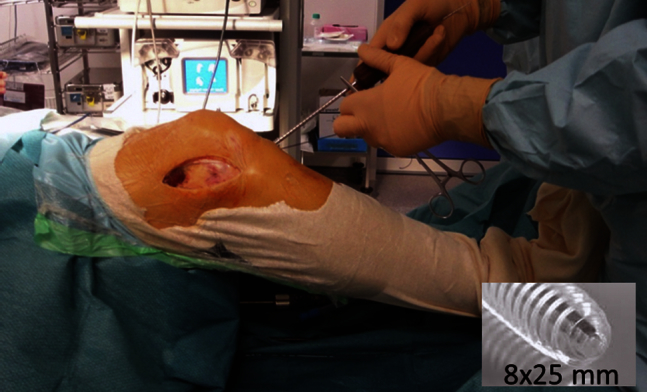
Tibial fixation of the graft at 30° flexion and neutral rotation with an 8 × 25 mm bioasorbable interference screw—lateral view.
The guide pin is inserted in the tibial tunnel, and an 8- or 9-mm bioabsorbable interference screw (FH Orthopedics) is placed in the tibial tunnel. Tension of the graft is checked using a clamp placed at the extra-articular part of the graft at 90° and 30° flexion. Ideally, the graft must be tensed at 30° and slightly relaxed at 90°.
There is usually no fixation for the ALL graft on the femur: this is a combined ACL and ALL reconstruction using a continue ITB graft. The 2 fixation points are the tibial tunnel with a bioabsorbable screw and the natural attachment from the ITB on the GT. However, an additional 8-mm-diameter screw can be added on the femoral tunnel.
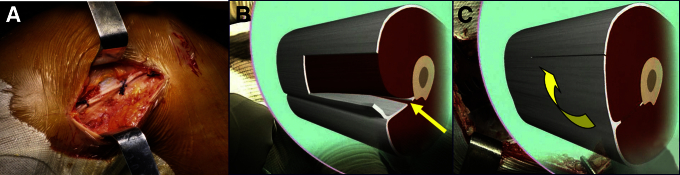
Wound Closure
The tourniquet is deflated and meticulous hemostasis is achieved, especially the bleeding from the vessels deep to the ITB, just behind the lateral condyle. The ITB is closed with an absorbable No. 2 Vicryl sutures (Ethicon) (Fig 7A). In cases of a bulky vastus lateralis, closure can be facilitated by sectioning the intermuscular septum (Figs 7 B and C). Subcutaneous and skin layers are closed with an absorbable suture. Adhesives dressing (Smith & Nephew, Andover, MA) on the lateral skin incision (ITB harvesting) and arthroscopic portals are applied and a compression stocking is applied from the foot to the upper thigh.
Fig 7.
(A) Iliotibial band (ITB) closure. (B) Intermuscular septum section (yellow arrow). (C) ITB anterior translation (yellow arrow).
Postoperative Management
The rehabilitation program included full weight bearing and immediate mobilization without limitation (flexion and extension); brace and crutches are recommended for 15 days (brace only for walking). Return-to-sports is gradual with home trainer at 6 weeks, swimming and bicycle at 3 months, running at 4 months, pivoting and noncontact sports at 6 months, and pivoting and contact sporting activities at 8 months.
Pearls and pitfall of this technique are summarized in Table 2.
Table 2.
Pearls and Pitfall of the Technique
| Surgical Steps | Pearls | Pitfalls |
|---|---|---|
| Identifying the bony landmarks | Recognition of the femoral LCL insertion site and genicular vessels will help in determining the best femoral extra-articular placement | Difficulty in identifying these individual points in bulky patients |
| Isometry testing | A suture is looped around the K-wire and the isometry tested through ROM | Inappropriate selection of isometric points results in great length variability throughout ROM |
| Graft harvest | While harvesting the ITB care should be taken not to cut the vessels posterior to the lateral condyle | Postop hemorrhage due to excessive bleeding from the severed vessels |
| Graft fixation | Maintaining the knee between 30° flexion and full extension while fixing the graft to the tibia | Inappropriate knee position while fixing the graft may lead to a nonisometric reconstruction |
| ITB closure | Tight closure of the fascia lata with a No. 2 suture at the end of the surgical procedure | Closure of the fascia lata using the Jaeger artifice13 may be helpful in cases of bulky vastus lateralis |
ITB, iliotibial band; LCL, lateral collateral ligament; ROM, range of motion.
Discussion
Developments of isolated arthroscopic ACL reconstructions should provide control of anterior and rotational laxity of the knee and have overthrown EAT procedures in the past few decades. But insufficient rotational control may be as high as 15% to 20% with isolated ACL reconstructions.6 Also, controversy on the ability of a double-bundle technique to control rotational laxity has been suggested in recent studies.8
Many authors have now described the ALL that was first described by Segond in 1870,1 and many established its value in controlling the internal rotation of the knee.9, 10, 11 It has been proposed that, because of its structure and location, the ALL limits internal tibial rotation and that a disruption contributes to the pivot shift phenomenon.10
In addition to this anatomic argument, there are biomechanics advantages for using an EAT. After an ACL rupture, the center of rotation of the knee shifts medially, so an EAT, which is peripheral to the center of rotation of the knee, has a better lever arm than that provided by an intra-articular reconstruction for the rotary control. Moreover, Engebretsen et al.12 showed that the combination of a lateral tenodesis to a single ACL procedure reduces the tension on the ACL by approximately 43%.
The femoral attachment of the ALL is still controversial. The first descriptions accounted for an attachment that was anterior and distal to the lateral epicondyle. However, recent studies describe its attachment to be posterior and proximal to the lateral femoral epicondyle.10, 11 Femoral attachment is crucial for an isometric reconstruction of the ALL, because a nonisometric reconstruction may lead to limitation of the normal ROM. Anterior and distal femoral tunnel attachment may lead to lengthening of the graft in flexion if it is fixed in extension, thereby producing stiffness and increased pressure in the lateral compartment. If the graft is fixed in flexion, it may lead to a laxity in extension and an ineffective reconstruction. In a posterior and proximal femoral attachment with graft fixation in full extension ensures an isometric reconstruction where a minimal graft length change is observed; the graft is tight in extension and lax in flexion. As knee flexion increases, the graft progressively becomes more lax, allowing full ROM and internal rotation. The reconstruction technique we propose fully addresses these anatomical requirements, thus becoming a possible alternative to the already described ACL combined anterolateral reconstruction techniques.
In addition to the limitation of the full ROM by the inadequate placement of the graft, the others specific risks are hematoma on the lateral part of the thigh and muscular hernia on the proximal part of harvesting. If the graft is too short or too thin, gracilis or semitendinous can be used to extend or strength the graft.
Next to these risks, this technique presents several advantages (Table 1). The most important is to permit both ACL and ALL reconstruction with a unique autologous graft. As the ITB is closed at the end of the procedure, the morbidity of its harvesting is probably less than harvesting hamstrings tendons or one-third of the patellar tendon. In the case of a revision procedure from other techniques, it presents with the advantage of not having to harvest grafts from the contralateral knee. Morbidity related to skin incision can be reduced with mini lateral approach incision for graft harvesting and other several artifices described.13 The ITB needs to be closed at the end of the surgery. In some bulky patients, this can be challenging, for which, we recommend using the technique of sectioning the intermuscular septum, which enables the advancement of the posterior fascia.14
This technique provides an alternative to other mixed reconstruction techniques and grafts described in the anterolateral reconstruction. Further studies are needed to determine the role and indications for reconstruction of the anterolateral structures with isometric extra-articular procedures.
Footnotes
The author reports the following potential conflict of interest or source of funding: B.S-C. receives support from Arthrex.
Supplementary Data
Key steps of a combined anterior and anterolateral stabilization of the knee with the iliotibial band.
References
- 1.Segond P. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. Progrés Med. 1879;7:297–341. [in French] [Google Scholar]
- 2.Hughston J., Andrews J., Cross M., Moschi A. Classification of knee ligament instabilities: Part I. Medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58:159–172. [PubMed] [Google Scholar]
- 3.Muller W. Springer Verlag; New York: 1983. The knee. [Google Scholar]
- 4.Lemaire M. Ruptures anciennes du ligament croisé antérieur. Fréquence clinique traitement Chir. 1967;93:311–320. [in French] [Google Scholar]
- 5.MacIntosh D.L., Darby T.A. Lateral substitution reconstruction. J Bone Joint Surg Br. 1976;58:142. doi: 10.1302/0301-620X.70B4.3403611. [DOI] [PubMed] [Google Scholar]
- 6.Crawford S.N., Waterman B.R., Lubowitz J.H. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1566–1571. doi: 10.1016/j.arthro.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu M., Gao S., Zeng C. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: Meta-analysis of 19 randomized controlled trials. Arthroscopy. 2013;29:357–365. doi: 10.1016/j.arthro.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 9.Sonnery-Cottet B., Archbold P., Rezende F.C., Neto A.M., Fayard J.M., Thaunat M. Arthroscopic identification of the anterolateral ligament of the knee. Arthrosc Tech. 2014;3:e389–e392. doi: 10.1016/j.eats.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dodds A.L., Halewood C., Gupte C.M., Williams A., Amis A.A. The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Joint J. 2014;96:325–331. doi: 10.1302/0301-620X.96B3.33033. [DOI] [PubMed] [Google Scholar]
- 11.Kittl C., Halewood C., Stephen J.M. Length change patterns in the lateral extra-articular structures of the knee and related reconstructions. Am J Sports Med. 2015;43:354–362. doi: 10.1177/0363546514560993. [DOI] [PubMed] [Google Scholar]
- 12.Engebretsen L., Lew W., Lewis J.L., Hunter R.E. The effect of an iliotibial tendesis an intra-articular graft forces and knee joint motion. Am J Sports Med. 1990;18:169–176. doi: 10.1177/036354659001800210. [DOI] [PubMed] [Google Scholar]
- 13.Khiami F., Wajsfisz A., Meyer A., Rolland E., Catonné Y., Sariali E. Anterior cruciate ligament reconstruction with fascia lata using a minimal invasive arthroscopic harvesting technique. Orthop Traumatol Surg Research. 2013;99:99–105. doi: 10.1016/j.otsr.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 14.Jaeger J.H., Van Hille W., Lutz C., Villeminot J. Springer; Paris: 2003. Ligamentoplastie du ligament croisé antérieur au fascia lata selon la technique de Mac Intosh modifiée. In: Landreau P, Christel P, Djian P, eds. Pathologie ligamentaire du genou; pp. 399–409. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Key steps of a combined anterior and anterolateral stabilization of the knee with the iliotibial band.