Abstract
Patients who experience distal biceps tendon avulsions generally benefit from surgical intervention. Compared with nonoperative treatment, surgery has shown improved muscle endurance as well as increased flexion and supination strength. Although a number of surgical techniques exist, repair of the distal biceps through a single incision is gaining popularity. This may be due in part to patient preference and emerging technologies such as cortical button fixation, suture anchors, and intraosseous screws. In this report, we present a simple technique for anatomically repairing distal biceps injuries using an intramedullary tenodesis button. This technique has the benefit of using a single unicortical drill hole in the radius while allowing the surgeon to sequentially tighten the tendon to its desired level of tension. When appropriate surgical steps are followed, it can be completed in a reliable, safe, and efficient manner through a single incision.
Rupture of the distal tendon of the biceps brachii is a relatively rare injury that predominantly occurs in male patients between the ages of 30 and 60.1 The annual incidence of distal biceps tears is 1.2 cases per 100,000 patients with 86% occurring in the dominant extremity.2 Although several treatment options, both operative and nonoperative, have been described for these injuries, surgical repair has become the standard of care. This is due in large part to the fact that multiple studies have shown superior functional outcomes after surgical treatment such as increased supination and flexion strength and decreased fatigability.3, 4, 5, 6
Although operative treatment has shown improved outcomes, the optimal technique for distal biceps tendon repair remains controversial. Anatomic repair can be performed through a 1-incision approach or a 2-incision approach. Because the original 1-incision technique developed by Dobbie7 resulted in an unacceptably high incidence of neurologic injury, the 2-incision technique popularized by Boyd and Anderson8 became the procedure of choice for several decades. Although this technique may have reduced the risk of nerve injury, it requires dissection through the radioulnar synostosis, increasing the risk for heterotopic ossification that could potentially limit forearm rotation.9 More recently, with the advent of improved techniques and implants such as suture anchors, intraosseous screws, and suspensory cortical buttons, single-incision techniques have once again gained popularity.
Currently there is no clear consensus regarding the ideal method of tendon fixation. A systematic review by Watson et al.10 showed that bone tunnel and cortical button methods resulted in significantly lower complication rates compared with suture anchor and intraosseous screw techniques. In another systematic review, Chavan et al.11 found that cortical button fixation provided higher load to failure and stiffness compared with bone tunnels, intraosseous screws, and suture anchors. The purpose of this work was to describe a technique for distal biceps tendon repair using a single-incision approach with intramedullary cortical button fixation. When precise surgical steps are followed (Table 1), this technique allows for reliable, efficient, and safe repair of distal biceps tendon injuries. The procedure is described in detail here and in the accompanying video (Video 1, Table 2).
Table 1.
Key Points
|
|
|
|
|
Table 2.
Equipment Required
Arthrex Inc., Naples, FL.
Technique
Patient History and Examination
Patients with distal biceps avulsions typically report acute onset of anterior elbow pain that occurs while trying to lift a heavy object with the elbow flexed. They often feel a pop or snap in the elbow. Occasionally, patients may have a history of antecedent anterior elbow pain that precedes the acute injury. This may be indicative of chronic tendinopathy or prior partial tear. On physical examination, ecchymosis may be present in the antecubital fossa, and a retracted biceps muscle (“Popeye sign”) may be present. Patients frequently have an increased distance from the inferior extent of the biceps muscle to the elbow flexion crease when compared with the contralateral, uninjured side. The Hook test is used to confirm the injury as it has been shown to be the most specific and sensitive physical examination test for diagnosing a distal biceps disruption.12
Surgical Timing
For patients with acute distal biceps disruptions, it is generally preferred to perform surgery as soon as the surrounding soft tissues permit. Ideally, this is accomplished in the first 1 to 2 weeks from injury. Injuries present for greater than 4 weeks often retract and scar proximally in the arm making surgery more difficult and are associated with higher complication rates.
Surgical Technique
The patient is placed in the supine position with the arm out on a hand table. The surgeon is typically seated between the patient's arm and body. A sterile or nonsterile tourniquet is used. Before insufflation, the arm can be milked distally to prevent entrapment of the biceps. The upper extremity is then exsanguinated with an Eshmarch bandage, and the tourniquet is inflated. For most cases, a single 4-cm transverse incision in the region of the radial tuberosity that is approximately 3 to 4 cm distal to the flexion crease of the antecubital fossa is used. For chronic cases in which scarring and retraction are likely, an “S”-shaped incision can be extended proximally and distally. After sharp dissection through skin, dissection scissors are used to develop a plane to the biceps tendon stump. Great care should be taken to preserve neurovascular structures, as the lateral antebrachial cutaneous nerve and cephalic vein are often encountered. Once the stump is located, it should be mobilized and freed from surrounding scar tissue or adhesions. In chronic cases, extensive dissection may be required.
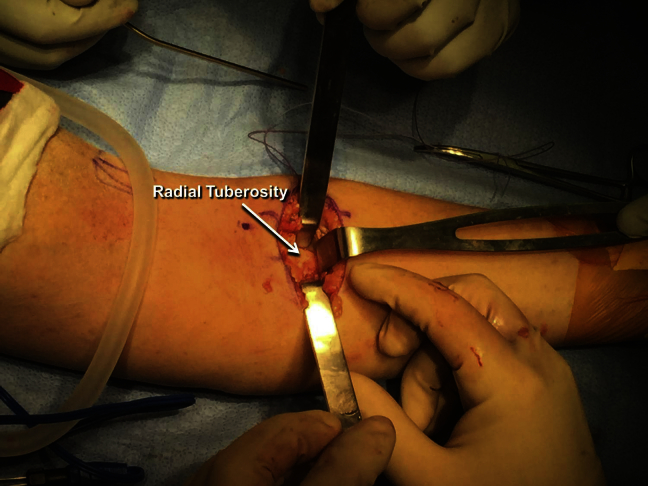
After identification and mobilization of the tendon stump, attention should be turned to the insertion site on the radial tuberosity. Generally, a plane from the stump to the tuberosity can readily be dissected with a finger or other blunt instrument. Using Hohmann retractors as needed, the footprint of the biceps tendon on the radial tuberosity should be visualized (Fig 1). To ensure that the tendon stump has been sufficiently mobilized, it should be pulled down to the radial tuberosity with an Allis clamp. If it is able to reach the tuberosity with the elbow in less than 30° of flexion, it is likely mobilized adequately. If not, additional mobilization may be required. If the tendon does not reach the footprint despite full mobilization, augmentation with allograft tissue may be required.
Fig 1.
Viewing the anterior aspect of the left arm with the elbow extended and the forearm in full supination, the radial tuberosity can be identified by following the natural anatomic path of the biceps tendon. This area should be cleaned and the entire biceps tendon footprint fully visualized before tendon reattachment.
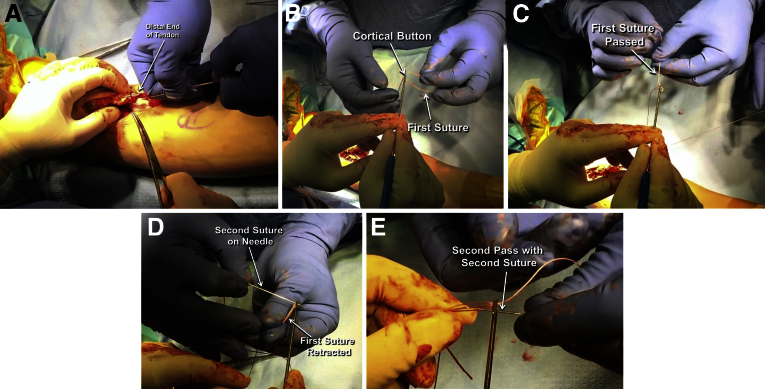
To prepare the tendon for repair, the frayed end should be debrided by sharply excising the very distal aspect. An Allis clamp is then placed on the tendon and a 2-0 looped Fiberwire on a straight needle (Arthrex, Naples, FL) is used to place a standard looped baseball stitch in the tendon. This begins approximately 4 to 5 cm proximal to the distal end of the tendon and proceeds distally. The suture is locked by passing the final 1 to 2 throws proximal to the distal most pass (Fig 2A). The clamp can be removed and the suture cut leaving 2 long free ends. These ends are threaded into a Proximal Tenodesis Button (Arthrex). One suture is passed through one eye of the button and out the other. The second suture is then passed in the opposite direction (Fig 2B-E). The free ends of the suture are clamped and set aside.
Fig 2.
(A) A 2-0 Fiberwire looped suture is used to place a baseball stitch into the free end of the tendon. This provides control of the tendon and creates a secure construct for repair back down to the radial tuberosity. To thread the Proximal Tenodesis Button onto the sutures of the biceps tendon, (B) the first suture is passed by an assistant through one eye of the button and (C) out the other. (D) The first suture is retracted as the second suture is passed into the eye where the first suture exits, and (E) back through to exit through the eye where the first suture enters. The free ends of each suture should not be exiting from the same hole. This permits tensioning of the construct once the button is passed.
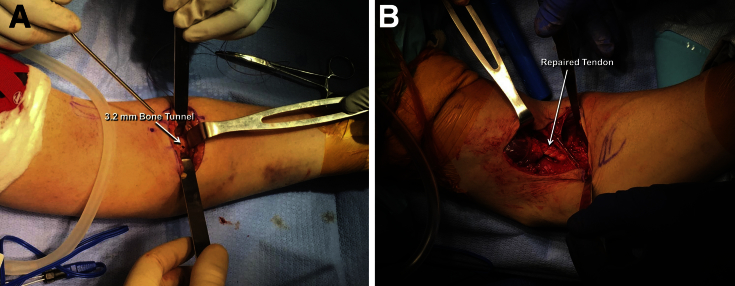
Attention is turned to the preparation of the footprint of the biceps tendon on the radial tuberosity. With the arm maximally supinated, the radial tuberosity is brought into view (Fig 1). It is debrided of soft tissue to provide a suitable surface for tendon healing. Once the site is prepared, a 3.2-mm drill (Arthrex) is used to create a unicortical drill hole in the center of the radial tuberosity (Fig 3A). The sutures are unclamped and excessive slack is removed. The button is placed directly into the unicortical drill hole and deployed by turning the knob on the handle of the button holder (Arthrex). It is important to pass the tendon through its normal anatomical plane so as to avoid entangling neurovascular structures. Once the button is deployed, the button holder is removed and the sutures are sequentially tensioned. Tensioning of the sutures flips the button within the medullary canal so that it abuts the inner surface of the bone cortex. The elbow is ideally placed in 30° to 45° of flexion and the sutures are final-tightened until the tendon is firmly in contact with the radial tuberosity. The sutures are tied in place (Fig 3B). If desired, a free needle can be used to pass the 2-0 Fiberwire back through the tendon, but this is typically not required. The wound is copiously irrigated, hemostasis is obtained, and the wound is closed in layers. The patient is placed in a posterior splint and a sling with the elbow in approximately 70° of flexion. An example of a postoperative radiograph is included in Figure 4.
Fig 3.
Looking at the anterior aspect of this left arm, the radial tuberosity is again exposed after the button has been threaded onto the sutures of the tendon. (A) A 3.2-mm hole is drilled in the center of the footprint through the near cortex only. With the elbow in approximately 30° of flexion, the button is advanced into the intramedullary canal of the radius. It is then flipped and the sutures are sequentially tightened. This secures the tendon to its native footprint on the radial tuberosity. The sutures are then securely tied and cut. (B) This figure shows the final appearance of the tendon after repair.
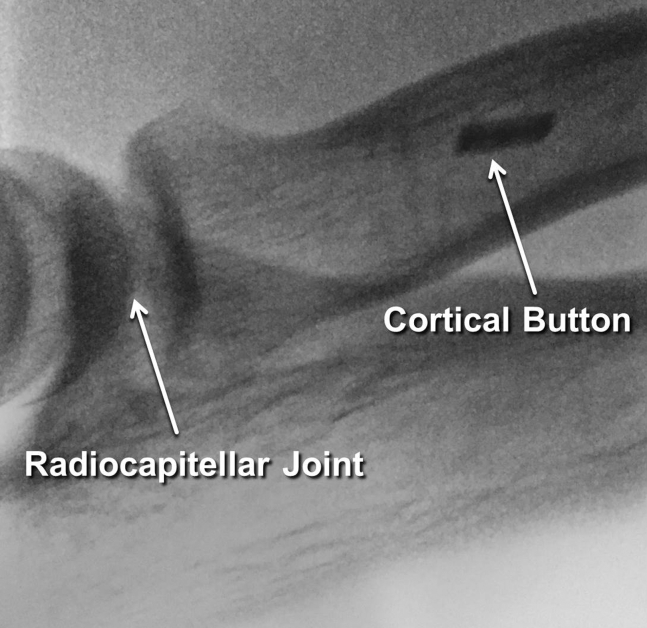
Fig 4.
Postoperative lateral fluoroscopic radiograph of a patient undergoing single-incision intramedullary cortical button repair of a ruptured biceps tendon. Note the intramedullary location of the button. The far cortex remains unviolated as the button rests securely against the inner aspect of the near cortex.
Postoperative Rehabilitation
After surgery, the splint is removed in the first week and very gentle passive elbow range of motion is permitted as soon as the patient is able to tolerate it. This is gradually increased week by week with a goal of obtaining full range of motion by the end of week 6. Although active elbow extension is allowed, active elbow flexion is avoided for the first 6 weeks. From weeks 6 to 12, active elbow flexion is gradually increased. Lifting is increased approximately 5 pounds per week during this time. If the patient is doing well at the 12-week mark, he or she is allowed to gradually return to all activities as tolerated without restriction.
Discussion
Although distal biceps injuries are relatively rare, surgery is typically warranted for patients desiring optimal flexion strength, supination strength, and muscle endurance. Historically, most injuries were repaired through a dual incision approach; however, as technology and fixation constructs improve, the single-incision technique is once again gaining popularity. The technique presented here relies on an intramedullary cortical button to anatomically reduce and fix the distal biceps tendon to its footprint on the radial tuberosity. It has the benefits of allowing the surgeon to control the tension of the repair, using a single incision, and only requiring a small 3.2-mm drill hole through a single cortex. Use of only a single drill hole minimizes the risk of fracture through the proximal radius. Other benefits of the single-incision technique include improved cosmesis, preservation of the radioulnar synostosis, and ease of patient positioning. Potential drawbacks include risk to the lateral antebrachial cutaneous nerve and potentially difficult exposure of the radial tuberosity in cases of excessive scarring (Table 3). Ultimately, this repair technique can be performed in a safe, efficient, and reliable manner when appropriate surgical steps are followed.
Table 3.
Benefits and Potential Pitfalls of Performing the Single-Incision Cortical Button Distal Biceps Repair Technique
| Benefits | Potential Pitfalls |
|---|---|
| Improved cosmesis compared with multiple incisions | Injury risk to the lateral antebrachial cutaneous nerve |
| Single drill hole through radius reducing the amount of bone removed and risk of fracture | Tuberosity exposure can be difficult when chronic injury or scarring is present |
| Preserves radioulnar synostosis | |
| Allows manual tensioning and reduction of tendon |
Footnotes
The authors report the following potential conflict of interest or source of funding: J.S.D receives support from Arthrex, Conmed Linvatec, Ossur, Biomet, and Wolters Kluwer Health.
Supplementary Data
A single-incision technique for distal biceps repair is highlighted. With the patient in the supine position and the arm out on an arm board, an incision is created just distal to the elbow flexion crease over the tuberosity. The tendon stump is identified and a baseball type stitch is placed. Once the radial tuberosity is identified, the bicipital footprint is cleaned and prepared using a scapel. A 3.2-mm unicortical drill hole is placed in the center of the footprint. The sutures attached to the tendon stump are treaded through a Proximal Tenodesis Button (Arthrex), which is passed into the intramedullary canal and flipped. As the sutures are tightened, the tendon is reduced and secured to its anatomic footprint. Step-by-step video and audio guidance is provided for this reliable, efficient, and reproducible method of distal biceps repair.
References
- 1.Miyamoto R.G., Elser F., Millett P.J. Distal biceps tendon injuries. J Bone Joint Surg Am. 2010;92:2128–2138. doi: 10.2106/JBJS.I.01213. [DOI] [PubMed] [Google Scholar]
- 2.Safran M.R., Graham S.M. Distal biceps tendon ruptures: Incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275–283. [PubMed] [Google Scholar]
- 3.Baker B.E., Bierwagen D. Rupture of the distal tendon of the biceps brachii. Operative versus non-operative treatment. J Bone Joint Surg Am. 1985;67:414–417. [PubMed] [Google Scholar]
- 4.Freeman C.R., McCormick K.R., Mahoney D., Baratz M., Lubahn J.D. Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J Bone Joint Surg Am. 2009;91:2329–2334. doi: 10.2106/JBJS.H.01150. [DOI] [PubMed] [Google Scholar]
- 5.Chillemi C., Marinelli M., De Cupis V. Rupture of the distal biceps brachii tendon: Conservative treatment versus anatomic reinsertion—clinical and radiological evaluation after 2 years. Arch Orthop Trauma Surg. 2007;127:705–708. doi: 10.1007/s00402-007-0326-7. [DOI] [PubMed] [Google Scholar]
- 6.Hetsroni I., Pilz-Burstein R., Nyska M., Back Z., Barchilon V., Mann G. Avulsion of the distal biceps brachii tendon in middle-aged population: Is surgical repair advisable? A comparative study of 22 patients treated with either nonoperative management or early anatomical repair. Injury. 2008;39:753–760. doi: 10.1016/j.injury.2007.11.287. [DOI] [PubMed] [Google Scholar]
- 7.Dobbie R. Avulsion of the lower biceps brachii tendon: Analysis of fifty-one previously unreported cases. Am J Surg. 1941;51:662–683. [Google Scholar]
- 8.Boyd H., Anderson L. A method for reinsertion of the distal biceps brachii tendon. J Bone Jt Surg. 1961;43:1041–1043. [Google Scholar]
- 9.Failla J.M., Amadio P.C., Morrey B.F., Beckenbaugh R.D. Proximal radioulnar synostosis after repair of distal biceps brachii rupture by the two-incision technique. Report of four cases. Clin Orthop Relat Res. 1990;253:133–136. [PubMed] [Google Scholar]
- 10.Watson J.N., Moretti V.M., Schwindel L., Hutchinson M.R. Repair techniques for acute distal biceps tendon ruptures: A systematic review. J Bone Joint Surg Am. 2014;96:2086–2090. doi: 10.2106/JBJS.M.00481. [DOI] [PubMed] [Google Scholar]
- 11.Chavan P.R., Duquin T.R., Bisson L.J. Repair of the ruptured distal biceps tendon: A systematic review. Am J Sports Med. 2008;36:1618–1624. doi: 10.1177/0363546508321482. [DOI] [PubMed] [Google Scholar]
- 12.O’Driscoll S.W., Goncalves L.B.J., Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med. 2007;35:1865–1869. doi: 10.1177/0363546507305016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A single-incision technique for distal biceps repair is highlighted. With the patient in the supine position and the arm out on an arm board, an incision is created just distal to the elbow flexion crease over the tuberosity. The tendon stump is identified and a baseball type stitch is placed. Once the radial tuberosity is identified, the bicipital footprint is cleaned and prepared using a scapel. A 3.2-mm unicortical drill hole is placed in the center of the footprint. The sutures attached to the tendon stump are treaded through a Proximal Tenodesis Button (Arthrex), which is passed into the intramedullary canal and flipped. As the sutures are tightened, the tendon is reduced and secured to its anatomic footprint. Step-by-step video and audio guidance is provided for this reliable, efficient, and reproducible method of distal biceps repair.