Abstract
The medial meniscus is crucial for knee homeostasis. Treating patients who have undergone a subtotal or total meniscectomy, or equivalent irreparable tear pattern, can be extremely challenging, especially in young, active patients. The importance of meniscal preservation has been reported by several authors. Meniscal repair is now widely accepted as the first surgical option for treating medial meniscal tears. Moreover, current guidelines recommend preserving as much meniscal tissue as possible. Treating a symptomatic medial meniscectomized knee is challenging because of limited surgical options. In this context, medial meniscal allograft transplantation arises as the preferred procedure. The purpose of this article was to detail the arthroscopic medial meniscal allograft transplantation technique with the use of 2 bone plugs.
Meniscal tears are one of the most commons lesions in orthopaedics.1, 2 It is well established in the literature that the menisci play an important role in load absorption and distribution, knee stability, joint lubrication, and congruity.3, 4 The medial meniscus absorbs 50% of the medial compartment load in an extended knee and it has an important role in stabilizing anteroposterior (AP) knee translation.5 When a medial meniscectomy or equivalent irreparable tear pattern leads to symptoms that could indicate predictable early onset osteoarthritis, medial meniscal allograft transplantation (MMAT) is a viable treatment option.
Several MMAT techniques including open and arthroscopically assisted have been described as an attempt to restore knee biomechanics and potentially decrease the risk of osteoarthritis. Among these, arthroscopic soft tissue and bone plug techniques have been described for root fixation. Bone plug techniques for MMAT have been reported to lead to better results than the soft-tissue fixation,6 and therefore constitutes the preferred option. The purpose of this surgical technique description was to describe our method of MMAT using a 2 bone plug method.
Objective Diagnosis
Imaging studies should include weightbearing AP, lateral, and long-leg standing alignment radiographs, as well as magnetic resonance imaging (MRI). Partial and total medial meniscectomy can be evaluated on axial, coronal, and/or sagittal MRI views. Classic MRI presentation of a medial meniscectomy is seen as the absence of an identifiable meniscus. An arthroscopic evaluation should be performed to determine if the patient is a suitable candidate for MMAT in cases of doubtful indication.7, 8 Uncorrected joint comorbidities are contraindications to MMAT. Concomitant procedures such as joint alignment, ligament stabilization, and cartilage resurfacing will likely improve the survival of the graft, and are encouraged to be performed in the same surgical procedure or previous to the MMAT.9
Indications for Surgery
At present, no clear guidelines exist regarding inclusion criteria and timing for a MMAT. The criteria used by the senior author (R.F.L.) (blinded for review) include isolated medial knee pain with or without postactivity effusions after subtotal, total, or a functionally equivalent meniscectomy in patients with closed physes.7 The physes must be closed to avoid causing a physeal arrest and alignment deformities. Obesity should be considered as a relative contraindication to performing a MMAT; some authors contraindicate this procedure in patients with a body mass index of more than 30, because it increases the load within the knee compartments, resulting in increased risk of allograft failure.10
Patients with Outerbridge classification grade IV chondromalacia11 and bipolar (“kissing lesions”) articular cartilage lesions are not good candidates for MMAT. Patients who are candidates for a concurrent articular cartilage resurfacing procedure can be considered for an exemption.7
Graft Selection
Fresh frozen and nonirradiated or nonantigen matched grafts are preferred for MMAT. Graft sizing is essential to the successful outcome of MMAT. The method used by our group is the one described by Pollard et al.,12 which incorporates radiographic measurements to improve graft sizing. This method was reported to have a size mismatch of less than 5%. According to this method, meniscal width (medial-lateral dimension) is equivalent to the coronal distance from the peak of the medial tibial eminence to a line perpendicular to the joint line, tangent to the periphery of the medial tibial metaphysis on AP films. Meniscal length (AP dimension) is measured from lateral radiographs and can be calculated as 80% of the measured sagittal length of the tibial plateau. MRI has also been used for measurements of the affected and contralateral knee.13
Patient Positioning and Anesthesia
Bilateral knee examination must be performed after positioning the patient supine on the operating table and induction of general anesthesia to evaluate for any concurrent ligamentous instability and to assess for range of motion. A well-padded high-thigh tourniquet is subsequently placed on the operative limb and then it is placed into a leg holder (Mizuho OSI, Union City, CA). The uninjured knee is placed into an abduction stirrup (Birkova Product LLC, Gothenburg, NE) and the hip abducted sufficiently to be able to gain access to the posteromedial corner of the surgical knee. The leg holder should be placed proximal enough to allow sufficient exposure of the posteromedial corner for an inside-out meniscal repair.
Surgical Technique
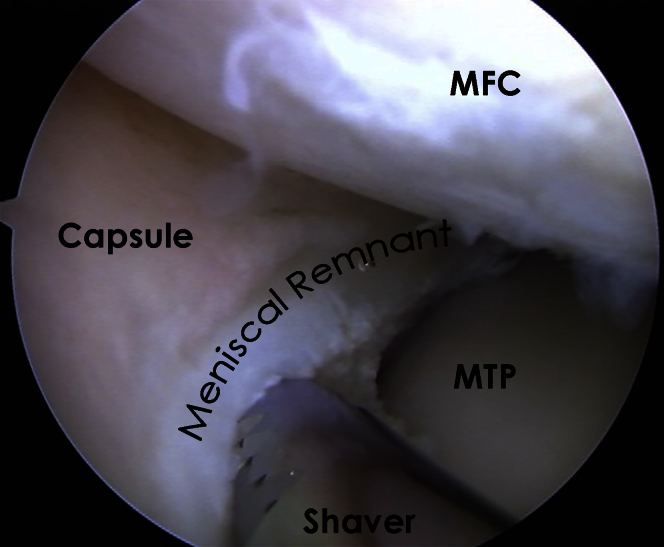
Anterolateral and anteromedial portals are created in a standard fashion adjacent to the patellar tendon and the joint is visualized with a 30° arthroscope (Smith & Nephew, Andover, MA). A diagnostic arthroscopy is performed to confirm the absence of chondral lesions that could contraindicate the procedure. An arthroscope is then used to identify the root attachment sites. An arthroscopic shaver (Smith & Nephew) is used to debride the remnant meniscal tissue, while leaving approximately a 1-mm rim of bleeding meniscal tissue (Fig 1, Video 1). The residual meniscal rim is left in place to prevent radial displacement of the allograft and function as a firm bed for meniscal fixation.14, 15 The medial meniscal allograft (JRF Ortho, Centennial, CO) is then thawed in room temperature saline.
Fig 1.
Arthroscopic image of trimming the meniscal remnant tissue with a mechanical shaver while leaving a small rim of healthy tissue, as viewed through the anteromedial portal. (MFC, medial femoral condyle; MTP, medial tibial plateau.)
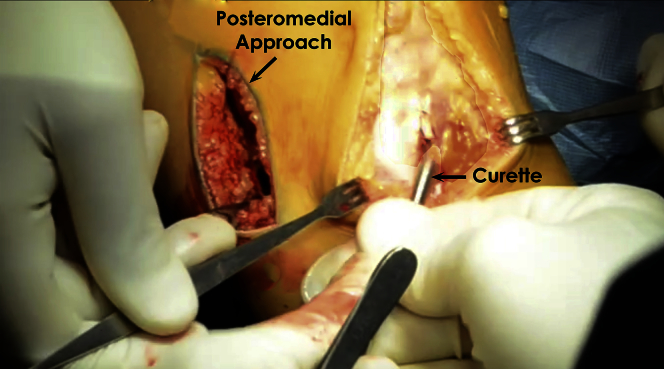
After intra-articular preparation for the meniscal transplant is completed, an arthroscopic probe is placed through the anteromedial portal inside the joint to help locate the planned incision and identify the joint line. An oblique vertical incision is performed from the adductor tubercle to the posterior aspect of the tibial plateau. Subcutaneous sharp dissection is carried out down to the sartorius fascia, which is incised as proximal as possible to preserve the pes anserine tendons. After blunt dissection through the sartorial fascia incision, an anatomic “triangle” delineated by the posteromedial joint capsule anteriorly, the medial gastrocnemius posteriorly, and the semimembranosus inferiorly can be identified. An elevator is then used to release adhesions between the posteromedial capsule and the medial head of the gastrocnemius. Using this same interval, a spoon is inserted and used as a retractor and to prevent injury to the neurovascular structures posteriorly.
Multiple small incisions are made in the proximal portion of the meniscofemoral superficial medial collateral ligament (pie crusting), which allows for increased medial compartment opening, thereby providing improved visualization and workspace during MMAT. In addition, some authors have described a low notchplasty between the fibers of the posterior cruciate ligament and the medial femoral condyle to facilitate visualization of the root attachment and subsequent passage of the posterior horn root bone plug.16, 17 In preparation for tunnel placement, the anteromedial portal is expanded distally and the anterior tibia should be exposed (Fig 2).
Fig 2.
Intraoperative picture of a left knee showing the exposure of the anteromedial aspect of the tibia for tunnel placement.
Next, the tunnel for the posterior root attachment of the medial meniscal transplant is prepared. With the aid of a cruciate aiming device (Arthrex, Naples, FL), a guide pin is drilled through the anteromedial aspect of the tibia to the posterior insertion of the medial meniscus, at an approximate 45° angle. The proximal tibial tunnel opening should be anterior to the posterior cruciate ligament insertion, along the downslope of the posterolateral aspect of the medial tibial plateau. Once the guide pin position is confirmed, the posterior horn tunnel is reamed (9-mm reamer, Arthrex) to create a tunnel just posterior to the medial eminence and lateral to the plateau cartilage. The socket should be the same size as the donor plug. The proximal tunnel aperture is then cleaned of remnant soft tissue with a series of shavers, curved rasps, and backbiters.
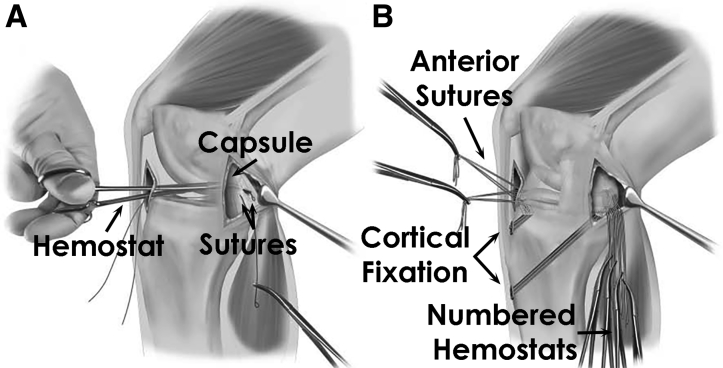
Next, a medial parapatellar arthrotomy incision is made in line with the previous arthroscopic portal. A looped suture is passed up through the posterior tunnel and retrieved through the anteromedial arthrotomy incision. Four passing sutures are then passed through the posteromedial capsule in an inside-out fashion with the aid of the a curved Adson hemostat tip to bluntly pierce the capsule while the surgeon (R.F.L.) controls the exit point using his finger to protect the neurovascular structures of the medial side (Fig 3). These passing sutures will match the location of the graft sutures to be placed in the posterior horn. Numbered hemostats are used at this point to hold the sutures in place and prevent mismatching of sutures later. The anterior root tunnel and socket will be created after insertion of the posterior meniscal root bone plug.
Fig 3.
Illustrations of a medial meniscal allograft transplantation for a right knee. (A) Placing the posterior meniscal horn passing sutures from the anteromedial incisions through the posteromedial capsule and out the posteromedial approach. These will later be matched up with the posterior horn sutures and used to pull the graft into place. (B) Illustration after the 2 tibial tunnels have been drilled and the allograft has been inserted. Both bone tunnels as well as the anterior and posterior horn sutures are in place.
(Reproduced with permission from LaPrade et al.7)
Graft Preparation
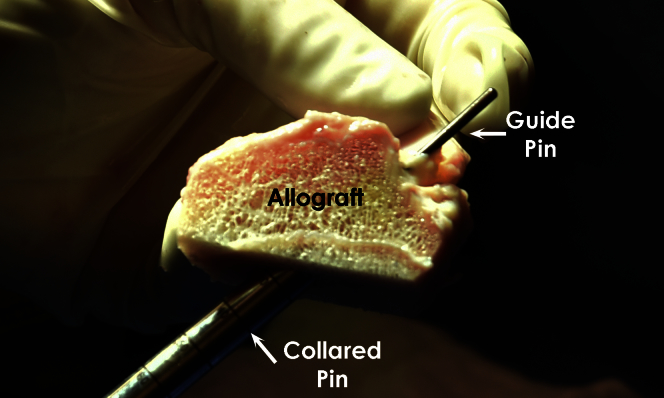
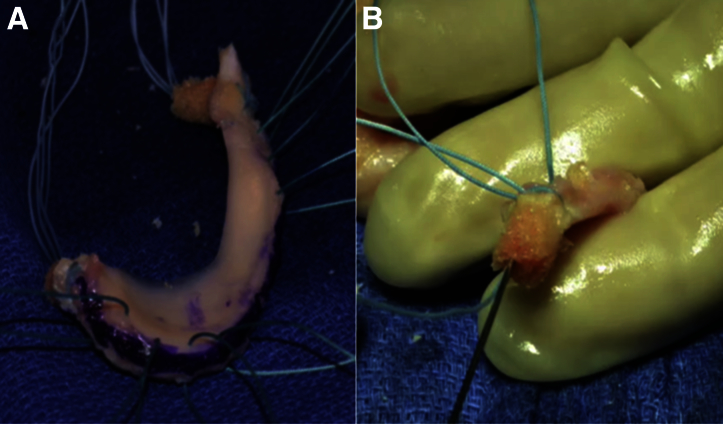
A 2.4-mm guide pin is drilled through the attachments of the anterior and posterior root attachments. It should be drilled at an angle that approximates the tibial tunnel. A collared pin (Arthrex) is inserted into the bottom of the bone allograft in a retrograde fashion so that a coring reamer (Arthrex) can be used to cut a dowel (Fig 4). The borders of the dowel should be removed with a rongeur. To release the bone plug from the donor, a sagittal saw (ConMed, Utica, NY) is used to cut the meniscal bone block to a depth of 10 mm.
Fig 4.
Picture depicting a guide pin passing through the posterior root of the medial meniscal graft and a collared pin inserted through the bottom of the posterior root.
Medial meniscal grafts are prepared with 3 to 4 nonabsorbable sutures close to the meniscocapsular junction in both the anterior and posterior horns. These sutures will be hereafter used to pass and securely fixate the meniscal graft to the joint capsule.
The bone plugs of the anterior and the posterior horn roots should have 9 mm diameter and the entire meniscal root attachments should be preserved. Two nonabsorbable sutures are passed through 1.5-mm drill holes in each root insertion and whipstitched into the root soft tissue attachments and threaded back down the bone plug again (Fig 5).
Fig 5.
Picture depicting (A) a medial meniscal allograft with 3 anterior and 4 posterior meniscocapsular junction sutures, as well as 2 sutures through each bone plug. The periphery of the graft is marked with methylene blue to help distinguish it from the remnant native meniscal rim during arthroscopy. (B) Two nonabsorbable sutures are passed up through the bone plug, through the soft tissue, and back down the bone plug with a large straight needle.
Allograft Insertion and Fixation
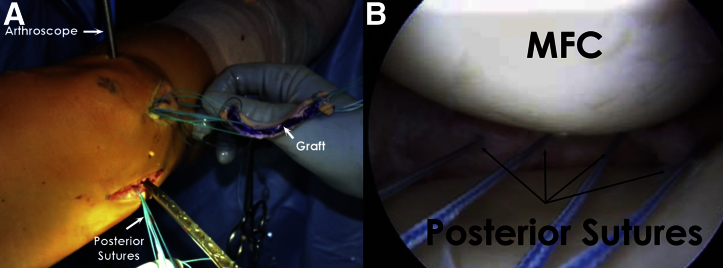
Next, the prepared allograft is inserted through the medial incision by pairing up the 2 sutures in the posterior root bone plug with the 2 looped sutures through the posterior root tunnel. Two sutures are used in case 1 of the sutures breaks. Then, the 4 sutures placed through the meniscal allograft are passed matching the numbered sutures of the posteromedial capsule (Fig 6). The posterior root bone plug is reduced into place with the use of a probe. When the posterior bone plug of the medial meniscus is properly positioned, the sutures are tied over a cortical fixation device (Endobutton, Smith & Nephew) on the anteromedial aspect of the tibia, securing the bone plug in the posterior tunnel.
Fig 6.
Left knee picture showing (A) posterior passing sutures used to help with passage of the meniscal allograft, and (B) an arthroscopic view of the posterior horn sutures being used to properly position the graft. (MFC, medial femoral condyle.)
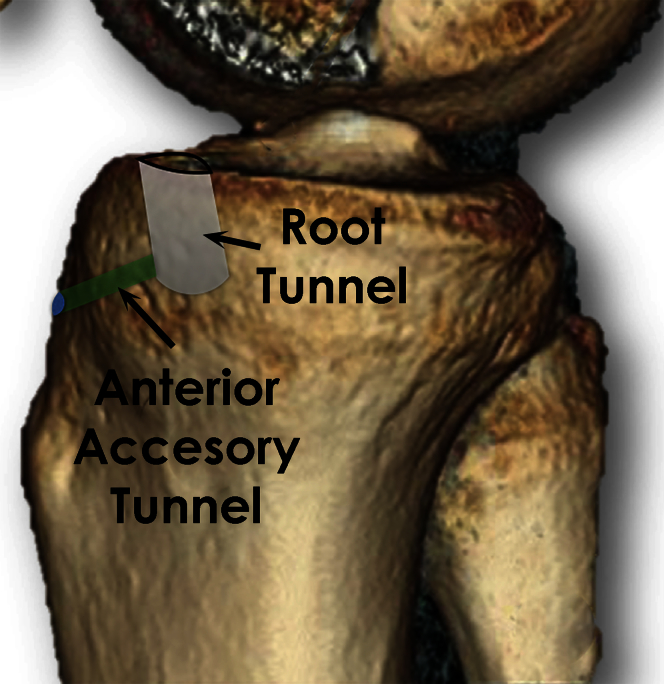
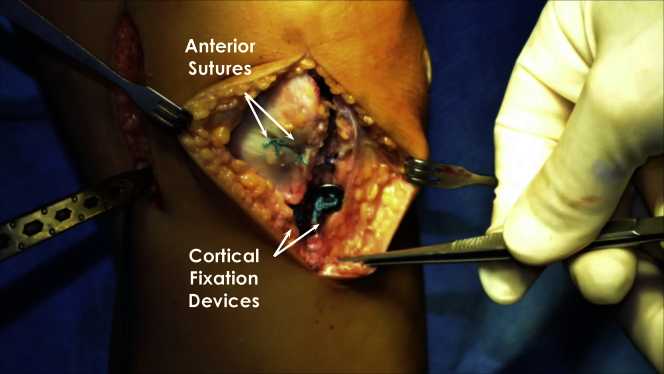
Then, the anterior tibial tunnel is drilled in a retrograde fashion by placing a guide pin over the remnant of the anterior root of the medial meniscus, approximately 3 to 4 mm posterior to the anterior aspect of the tibial plateau. Using a 9-mm reamer inserted through the medial parapatellar arthrotomy, a closed socket for the anterior horn bone plug is drilled to a depth of 15 mm, following the root insertion angle, being cautious to avoid any potential anterior cruciate ligament (ACL) reconstruction tunnel collision. A small drill hole is performed to communicate the distal aspect of the socket with the anterior cortex of the tibia (Fig 7). Passing sutures are then placed through the anterior cortex and up the anterior tunnel to facilitate the anterior horn bone block passage. After the anterior bone plug is positioned, the sutures are tied to a cortical fixation device (Endobutton, Smith & Nephew) in a similar manner as previously mentioned (Fig 8).
Fig 7.
Right knee illustration showing the location of the anterior medial meniscal root tunnel and the anterior accessory tunnel. The anterior root tunnel is drilled in an anterograde fashion and the sutures will be passed through the accessory tunnel and tied down to a cortical fixation device over the anteromedial tibia.
Fig 8.
Intraoperative image of a left knee after insertion of the medial meniscal allograft. The cortical fixation devices that secure the anterior and posterior bone plugs through the tibial tunnels can be seen. In addition, anterior horn sutures can be seen.
The meniscocapsular posterior sutures are tied in a cross-matched fashion (i.e., 1 arm of the first suture with 1 arm of the second suture) to make a stronger construct. Three anteriorly placed sutures are tied to the anteromedial capsule with a large free needle.
Lastly, the meniscal allograft is secured to the remnant meniscus and the capsule with 6 to 10 nonabsorbable vertical mattress sutures on both its superior and inferior surfaces with an arthroscopically assisted inside-out technique (Fig 9). The sutures are placed into the remnant rim of the native medial meniscus. The pearls and pitfalls of this technique are summarized in Table 1.
Fig 9.
Arthroscopic image of a left knee showing placement of inside-out sutures to the middle portion of the allograft after the anterior and posterior roots and horns have been secured. (MFC, medial femoral condyle.)
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
|
|
MMAT, medial meniscal allograft transplantation.
Postoperative Rehabilitation
Postoperatively, weightbearing is not allowed until week 6. For the first 2 weeks, assisted range of motion is limited from 0° to 90°. Full range of motion is allowed from week 3 on. At week 6, patients are allowed to bear weight as tolerated and to wean off crutches progressively. At this time, stationary bike activity and progressive low-impact rehabilitation are encouraged as tolerated. Deep squatting should be avoided until at least 4 months postoperatively. Return to full low-impact activities such as walking, swimming, and elliptical machines is allowed at 6 to 9 months. High-impact activities are always discouraged, especially in patients with more than grade I chondromalacia in the medial compartment.
Discussion
Medial meniscal allograft transplants are a safe and successful procedure for properly indicated patients. MMAT results in reduced patient pain, less activity-related effusions, and improved functional activities.7, 17, 18, 19, 20 After MMAT, LaPrade et al.7 reported a significant improvement in symptoms as measured with International Knee Documentation Committee subjective scores (preop 51.2, postop 68.2) and Cincinnati scores (preop 52.3, postop 73.2) after a minimum 2-year follow-up. Verdonk et al.18 reported a survival rate of isolated MMAT to be 72.4% at 10 years.
Several authors have outlined the importance of MMAT in ACL reconstructions.21, 22 When the posterior horn of the medial meniscus is absent, there is a higher ACL graft strain due to the stabilizing role of this structure.21, 22
Sekiya et al.23 reported an increased range of motion with the use of bone fixation compared with soft-tissue fixation. Rodeo6 reported a success rate of 88% in patients who underwent MAT with bone fixation compared with a 44% success rate of patients who had only a soft-tissue fixation. As a result, the bone plug technique is becoming more popular than the soft-tissue fixation alone.
The distance between the footprints of the medial meniscus is wider than that of the lateral meniscus. Therefore, it is not necessary to use the bone trough method, which creates a long bone slot in the tibial plateau. Although the bone plug method is most commonly used for MMAT, it remains technically challenging.
The degree of cartilage wear at the time of MMAT is the most important variable predicting outcome.19, 24 Von Lewinski et al.25 published a 20-year follow-up study showing no significant difference between the radiographic joint space of the affected knee compared with the noninvolved knee.
In conclusion, MMAT is a safe procedure that has shown good mid-term outcomes.7, 18 All patients should be informed that MMAT is likely not a curative procedure, but should function to delay cartilage wear and preserve the knee joint. Few long-term studies have reported the chondroprotective effects of the MMAT. However, as pain and swelling are decreased it is reasonable to infer that progression rate of arthritis is slowed. We encourage other groups to perform this MMAT technique with the use of bone plugs and report on long-term outcomes.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.F.L. receives support from Arthrex; Ossur; Siemans; Smith & Nephew; Health East, Norway; and a National Institutes of Health R13 grant for biologics.
Supplementary Data
Medial meniscal allograft transplantation using a 2 bone plug method. The patient is positioned supine on the operating table with a high-thigh tourniquet placed on the operating limb (in this case, left), which is held by a leg holder. With the arthroscope placed in the anteromedial portal and a shaver placed in the anterolateral portal, a debridement of the remnant meniscus is performed, leaving a 1-mm rim of tissue. With the aid of a probe placed through the medial portal, the joint line is identified to create the posteromedial repair incision. Blunt dissection is performed to the sartorial fascia and a Cobb elevator is used to release adhesions between the medial gastrocnemius and the posteromedial capsule. A spoon is inserted in this interval to facilitate retraction and to protect the neurovascular bundle. Little stab incisions (pie crusting) are made in the meniscofemoral portion of the superficial medial collateral ligament to increase the medial gapping and create the necessary room for the procedure. The anteromedial portal is vertically expanded down to the capsule, but the capsule is preserved at this point to prevent excessive fluid loss. The knee is extended, and with the arthroscope placed in the lateral portal, an aiming guide is inserted through the expanded medial portal to reach the correct location for the posterior bone plug fixation (back of the medial tibial plateau, and anterior to the more medial aspect of the posterior cruciate ligament). A guide pin is inserted and then over-reamed with a 9-mm reamer and the proximal aperture of the tibial tunnel is cleaned from soft tissues. The anteromedial arthrotomy incision is now completed. Two sutures (1 backup suture) are passed from the posterior tibial tunnel and retrieved through the anteromedial portal. Four looped passing sutures are then passed with the aid of a hemostat through the posteromedial capsule. These sutures will further be used to transport the definitive sutures placed on the posterior aspect of the graft. Graft preparation is performed on the back table. A 2.4-mm drill is drilled through the anterior and posterior root attachments of the allograft at angles that approximate the tunnels to be drilled in the tibia and the bone plugs are shaped. The length and width of the bone plugs are measured to match the width of the tibial tunnels (9-mm diameter and 10-mm depth for the posterior bone plug and 15-mm depth for the anterior bone plug). Two sutures are then placed through each plug, using needles up through the bone plug, the soft tissues and back down the bone plug. Four #2 FiberWire sutures (Arthrex, Naples, FL) are placed in the posterior horn and three #0 sutures are placed in the anterior aspect of the meniscus. The posterior bone plug is the first to be pulled into its position, followed by the 4 posterior sutures using the sutures previously passed through the posteromedial capsule. After the bone plug is anatomically reduced into place with the aid of a small flat elevator, its sutures are fixed to the anterior tibia using a cortical fixation device. Next, the bed of the anterior root is cleaned through the anteromedial portal and a guide pin is placed over its native insertion. With a 9-mm reamer, a closed socket tunnel is over-reamed to a depth of 15 mm and a second small hole is drilled through the anterior cortex to communicate with the bottom of the socket and allow for the retrieval of the anterior bone plug sutures and later fixation with a cortical fixation device. The anterior horn sutures are tied in place with a free needle. The posterior horn sutures are tied in a cross-matched fashion to each other. Once both roots and horns are fixed, 6 to 10 vertical mattress sutures are placed in the superior and inferior surfaces of the meniscus, in an inside-out fashion to complete the fixation of the allograft. Finally, the graft stability is tested with the aid of a probe.
References
- 1.Baker B.E., Peckham A.C., Pupparo F., Sanborn J.C. Review of meniscal injury and associated sports. Am J Sports Med. 1985;13:1–4. doi: 10.1177/036354658501300101. [DOI] [PubMed] [Google Scholar]
- 2.Englund M., Guermazi A., Gale D. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–1115. doi: 10.1056/NEJMoa0800777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allen P.R., Denham R.A., Swan A.V. Late degenerative changes after meniscectomy. Factors affecting the knee after operation. J Bone Joint Surg Br. 1984;66:666–671. doi: 10.1302/0301-620X.66B5.6548755. [DOI] [PubMed] [Google Scholar]
- 4.Fairbank T.J. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664–670. [PubMed] [Google Scholar]
- 5.Levy I.M., Torzilli P.A., Warren R.F. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64:883–888. [PubMed] [Google Scholar]
- 6.Rodeo S.A. Meniscal allografts—where do we stand? Am J Sports Med. 2001;29:246–261. doi: 10.1177/03635465010290022401. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade R.F., Wills N.J., Spiridonov S.I., Perkinson S. A prospective outcomes study of meniscal allograft transplantation. Am J Sports Med. 2010;38:1804–1812. doi: 10.1177/0363546510368133. [DOI] [PubMed] [Google Scholar]
- 8.Brophy R.H., Matava M.J. Surgical options for meniscal replacement. J Am Acad Orthop Surg. 2012;20:265–272. doi: 10.5435/JAAOS-20-05-265. [DOI] [PubMed] [Google Scholar]
- 9.Stone K.R., Adelson W.S., Pelsis J.R., Walgenbach A.W., Turek T.J. Long-term survival of concurrent meniscus allograft transplantation and repair of the articular cartilage: A prospective two- to 12-year follow-up report. J Bone Joint Surg Br. 2010;92:941–948. doi: 10.1302/0301-620X.92B7.23182. [DOI] [PubMed] [Google Scholar]
- 10.Abat F., Gelber P.E., Erquicia J.I., Pelfort X., Gonzalez-Lucena G., Monllau J.C. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40:1591–1596. doi: 10.1177/0363546512446674. [DOI] [PubMed] [Google Scholar]
- 11.Outerbridge R.E. The etiology of chondromalacia patellae. Clin Orthop Relat Res. 1961;2001:5–8. doi: 10.1097/00003086-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Pollard M.E., Kang Q., Berg E.E. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11:684–687. doi: 10.1016/0749-8063(95)90110-8. [DOI] [PubMed] [Google Scholar]
- 13.Yoon K.H., Lee S.H., Park S.Y., Kim H.J., Chung K.Y. Meniscus allograft transplantation: A comparison of medial and lateral procedures. Am J Sports Med. 2014;42:200–207. doi: 10.1177/0363546513509057. [DOI] [PubMed] [Google Scholar]
- 14.Verdonk P.C., Verstraete K.L., Almqvist K.F. Meniscal allograft transplantation: Long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14:694–706. doi: 10.1007/s00167-005-0033-2. [DOI] [PubMed] [Google Scholar]
- 15.Verdonk P., Depaepe Y., Desmyter S. Normal and transplanted lateral knee menisci: Evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc. 2004;12:411–419. doi: 10.1007/s00167-004-0500-1. [DOI] [PubMed] [Google Scholar]
- 16.Alford W., Cole B.J. The indications and technique for meniscal transplant. Orthop Clin North Am. 2005;36:469–484. doi: 10.1016/j.ocl.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Cole B.J., Carter T.R., Rodeo S.A. Allograft meniscal transplantation: Background, techniques, and results. Instr Course Lect. 2003;52:383–396. [PubMed] [Google Scholar]
- 18.Verdonk P.C., Demurie A., Almqvist K.F., Veys E.M., Verbruggen G., Verdonk R. Transplantation of viable meniscal allograft. Survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87:715–724. doi: 10.2106/JBJS.C.01344. [DOI] [PubMed] [Google Scholar]
- 19.Matava M.J. Meniscal allograft transplantation: A systematic review. Clin Orthop Relat Res. 2007;455:142–157. doi: 10.1097/BLO.0b013e318030c24e. [DOI] [PubMed] [Google Scholar]
- 20.van Arkel E.R., de Boer H.H. Human meniscal transplantation. Preliminary results at 2 to 5-year follow-up. J Bone Joint Surg Br. 1995;77:589–595. [PubMed] [Google Scholar]
- 21.Graf K.W., Jr., Sekiya J.K., Wojtys E.M. Long-term results after combined medial meniscal allograft transplantation and anterior cruciate ligament reconstruction: Minimum 8.5-year follow-up study. Arthroscopy. 2004;20:129–140. doi: 10.1016/j.arthro.2003.11.032. [DOI] [PubMed] [Google Scholar]
- 22.Sekiya J.K., Giffin J.R., Irrgang J.J., Fu F.H., Harner C.D. Clinical outcomes after combined meniscal allograft transplantation and anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:896–906. doi: 10.1177/03635465030310062701. [DOI] [PubMed] [Google Scholar]
- 23.Sekiya J.K., West R.V., Groff Y.J., Irrgang J.J., Fu F.H., Harner C.D. Clinical outcomes following isolated lateral meniscal allograft transplantation. Arthroscopy. 2006;22:771–780. doi: 10.1016/j.arthro.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 24.Garrett J.C., Steensen R.N. Meniscal transplantation in the human knee: A preliminary report. Arthroscopy. 1991;7:57–62. doi: 10.1016/0749-8063(91)90079-d. [DOI] [PubMed] [Google Scholar]
- 25.von Lewinski G., Milachowski K.A., Weismeier K., Kohn D., Wirth C.J. Twenty-year results of combined meniscal allograft transplantation, anterior cruciate ligament reconstruction and advancement of the medial collateral ligament. Knee Surg Sports Traumatol Arthrosc. 2007;15:1072–1082. doi: 10.1007/s00167-007-0362-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Medial meniscal allograft transplantation using a 2 bone plug method. The patient is positioned supine on the operating table with a high-thigh tourniquet placed on the operating limb (in this case, left), which is held by a leg holder. With the arthroscope placed in the anteromedial portal and a shaver placed in the anterolateral portal, a debridement of the remnant meniscus is performed, leaving a 1-mm rim of tissue. With the aid of a probe placed through the medial portal, the joint line is identified to create the posteromedial repair incision. Blunt dissection is performed to the sartorial fascia and a Cobb elevator is used to release adhesions between the medial gastrocnemius and the posteromedial capsule. A spoon is inserted in this interval to facilitate retraction and to protect the neurovascular bundle. Little stab incisions (pie crusting) are made in the meniscofemoral portion of the superficial medial collateral ligament to increase the medial gapping and create the necessary room for the procedure. The anteromedial portal is vertically expanded down to the capsule, but the capsule is preserved at this point to prevent excessive fluid loss. The knee is extended, and with the arthroscope placed in the lateral portal, an aiming guide is inserted through the expanded medial portal to reach the correct location for the posterior bone plug fixation (back of the medial tibial plateau, and anterior to the more medial aspect of the posterior cruciate ligament). A guide pin is inserted and then over-reamed with a 9-mm reamer and the proximal aperture of the tibial tunnel is cleaned from soft tissues. The anteromedial arthrotomy incision is now completed. Two sutures (1 backup suture) are passed from the posterior tibial tunnel and retrieved through the anteromedial portal. Four looped passing sutures are then passed with the aid of a hemostat through the posteromedial capsule. These sutures will further be used to transport the definitive sutures placed on the posterior aspect of the graft. Graft preparation is performed on the back table. A 2.4-mm drill is drilled through the anterior and posterior root attachments of the allograft at angles that approximate the tunnels to be drilled in the tibia and the bone plugs are shaped. The length and width of the bone plugs are measured to match the width of the tibial tunnels (9-mm diameter and 10-mm depth for the posterior bone plug and 15-mm depth for the anterior bone plug). Two sutures are then placed through each plug, using needles up through the bone plug, the soft tissues and back down the bone plug. Four #2 FiberWire sutures (Arthrex, Naples, FL) are placed in the posterior horn and three #0 sutures are placed in the anterior aspect of the meniscus. The posterior bone plug is the first to be pulled into its position, followed by the 4 posterior sutures using the sutures previously passed through the posteromedial capsule. After the bone plug is anatomically reduced into place with the aid of a small flat elevator, its sutures are fixed to the anterior tibia using a cortical fixation device. Next, the bed of the anterior root is cleaned through the anteromedial portal and a guide pin is placed over its native insertion. With a 9-mm reamer, a closed socket tunnel is over-reamed to a depth of 15 mm and a second small hole is drilled through the anterior cortex to communicate with the bottom of the socket and allow for the retrieval of the anterior bone plug sutures and later fixation with a cortical fixation device. The anterior horn sutures are tied in place with a free needle. The posterior horn sutures are tied in a cross-matched fashion to each other. Once both roots and horns are fixed, 6 to 10 vertical mattress sutures are placed in the superior and inferior surfaces of the meniscus, in an inside-out fashion to complete the fixation of the allograft. Finally, the graft stability is tested with the aid of a probe.