Abstract
Purpose
The purpose of this case series is to report on changes in pain levels experienced by 69 postsurgical continued pain patients who received Cox Technic Flexion Distraction (CTFD).
Methods
Fifteen doctors of chiropractic collected retrospective data from the records of the postsurgical continued pain patients seen in their clinic from February to July 2012 who were treated with CTFD, which is a type of chiropractic distraction spinal manipulation. Informed consent was obtained from all patients who met the inclusion criteria for this study. Data recorded included subjective patient pain levels at the end of the treatments provided and at 24 months following the last treatment.
Results
Fifty-four (81%) of the patients showed greater than 50% reduction in pain levels at the end of the last treatment, and 13 (19%) showed less than 50% improvement of pain levels at the end of active care (mean, 49 days and 11 treatments). At 24-month follow-up, of 56 patients available, 44 (78.6%) had continued pain relief of greater than 50% and 10 (18%) reported 50% or less relief. The mean percentage of relief at the end of active care was 71.6 (SD, 23.2) and at 24 months was 70 (SD, 25). At 24 months after active care, 24 patients (43%) had not sought further care, and 32 required further treatment consisting of chiropractic manipulation for 17 (53%), physical therapy, exercise, injections, and medication for 9 (28%), and further surgery for 5 (16%).
Conclusion
Greater than 50% pain relief following CTFD chiropractic distraction spinal manipulation was seen in 81% of postsurgical patients receiving a mean of 11 visits over a 49-day period of active care.
Key indexing terms: Low back pain, Radiculopathy, Manipulation, Chiropractic, Sciatica, Pain measurement, Neurosurgical procedures
Introduction
Persistent low back and extremity pain following spine surgery is reported in up to 50% of patients.1, 2, 3 Specific clinical outcome of spine surgery with fusion for degenerative lumbar spine conditions in 208 patients showed 62.5% satisfied, 19.7% partially satisfied, and 17.8% of patients dissatisfied.4 Postsurgical continued pain (PSCP) sends patients to the offices of physicians, surgeons, and pain specialists alike in overwhelming numbers.5 Although surgery for radiculopathy caused by herniated lumbar disk and symptomatic spinal stenosis shows improved short-term benefit compared with nonsurgical care, the benefits diminish long term.
Choi et al6 found that low back and radicular pain returned within 6 months or longer in 70% of 707 postsurgical cases and that 19% experienced no relief or had immediate aggravation of pain after surgery. Complementary alternative care was chosen by 47% of these patients, as opposed to conventional medicine, including herbal medicine, acupuncture, electro- and pharmacupuncture, bee venom, manual therapy, and physical therapy. Blond et al7 report that spine surgery can cause morphological change in neural tissue causing "neuropathic back pain" with increased response of peripheral nervous system receptor input to the central nervous system. Successful clinical pain relief of PSCP patients under chiropractic spinal manipulation is reported in this and other studies. Spinal manipulation is recommended by the American Pain Society and the American College of Physicians for primary care of low back pain.8
The financial burden of lumbar disk disorder care is in excess of 100 billion dollars a year to treat with 5% of the patients absorbing 75% of the cost.9 Spine care annual expenditures increased by 95% between 1999 and 2008. Chiropractic expenditures were stable, whereas physical therapy was the most costly service.10 Readmission rates for spinal stenosis decompression among Medicare patients are approximately 8%-10% per year, and fusion did not protect against subsequent readmission.11 On second opinion for 155 consecutive patients who were suggested to have spine surgery, less than 44% were recommended to have it.12
The frequency and outcomes of chiropractic treatment of PSCP patients are not sufficiently documented. PSCP patients seeking care following spinal fusion are often diagnosed with sacroiliac joint pain, internal disk disruption, and zygapophyseal joint pain.13 A trial of conservative management which includes chiropractic manipulation has been recommended as appropriate prior to surgical intervention.14
At present, there is little literature about the response of postsurgical patients to chiropractic care. Therefore, the purpose of this case series is to report on changes in pain levels experienced by 69 PSCP patients who received Cox Technic Flexion Distraction (CTFD).
Methods
Fifteen chiropractic physicians in North America retrospectively collected data from the records of 69 PSCP patients who sought their care for continued or recurrent spine and/or lower extremity pain following spine surgery. The patient treatment period was from February 2012 through July 2012. Informed consent was obtained from all patients who were included in this study. Information regarding subjective patient pain levels at the end of the treatment period and again 24 months later was retrieved from the records.
Two protocols of CTFD were administered depending on the patient symptoms. Both were performed with the patient lying prone on a specially designed manipulation table having a stationary thoracic piece and a moveable caudal section.15 In performing lumbar spine CTFD, the lumbar spine is positioned on the thoracic section of the table and lower extremities on the caudal section. All motions were tested for patient tolerance prior to delivery. This was done by performing CTFD starting at low application force and building to tolerable levels of treatment force but not exceeding tissue tolerance. The doctor’s thenar hand contact is on the spinous process above the spinal segment as CTFD is applied. If no spine fusion was present, each vertebral segment to be distracted and manipulated was tolerance tested and treated. If spinal fusion is present, the unfused levels of the spine adjacent to the spinal fusion were treated. The treated spine levels were from the lower thoracic spine to the lumbosacral spine.15
Protocol I was used in treating patients with lower extremity radicular pain. Protocol II was used on patients exhibiting low back pain and lower extremity pain not extending below the knee or having attained 50% relief of their radicular pain while treated with Protocol I. Protocol I CTFD consists only of manual flexion or automated long y-axis distraction at a fixed flexion of the table’s caudal section and delivered to patient tolerance. This is used in treating patients with radiculopathy and is the only form of CTFD used until the patient exhibits 50% objective and subjective relief of radicular pain. The application of CTFD consists of three 20-second distraction sessions at the selected vertebral segment. Each 20-second distraction session consists of five 4-second cyclic applications of long y-axis or manual CTFD at the contacted spinal segment. Protocol II CTFD is used in treating patients without radiculopathy and/or patients who are at least 50% relieved of their radicular pain under Protocol I spinal manipulation.15 Protocol II application consists of distraction of the spine as in Protocol I with the addition of mobilizing facet joints into the physiological ranges of motion: flexion, lateral flexion, extension, and circumduction.
Patient medical records reflect data collection for typical care which included the following. Before treatment began, patient information was recorded: demographics, time period of pain recurrence following surgery, factors causing postsurgical pain recurrence, presurgical diagnosis, type of spine surgery, and the patient’s pain relief following surgery on a numerical pain scale (NPS) of 0%-100%. At the end of active chiropractic spinal treatment and 24 months following active care, information was collected from patients regarding their NPS pain relief.
During medical record review, the number of treatments and days of care were recorded. Additional care received during the 24-month posttreatment period was documented as well. All data and consents were retrieved and submitted to the lead author of this study. Because this is a descriptive observational study, no statistical tests were used. The data collected on the 69 patients were tabulated and descriptively analyzed.
Results
Fifteen male doctors of chiropractic with 4-49 years of clinical experience (mean, 24 years; SD, 12 years) collected the data from the patient records for this study. The participating doctors of chiropractic graduated from 8 different chiropractic colleges in the United States and had additional training and certification using the specialized CTFD techniques (mean, 13 years; SD, 12 years).
The cases included consisted of 29 men and 40 women. The mean age was 61 years old, with a mean height of 176 cm, a mean weight of 86 kg, and a mean body mass index of 29.6. Table 1 provides the details of the time period between prior spinal surgery and the start of seeking chiropractic care. The majority of the patients had surgery more than 2 years prior to chiropractic consultation, and 12 patients had surgery within the last year. The majority of patients had 1 surgery, and 11 patients had 2 surgical procedures prior to chiropractic consultation.
Table 1.
Details on Prior Surgery Before Coming to Chiropractic Consultation
| Months | Last Lumbar Spine Surgery |
|---|---|
| Less than 1 mo | 0 |
| 1-3 | 3 |
| 3-6 | 0 |
| 6-9 | 6 |
| 9-12 | 3 |
| 12-18 | 2 |
| 12-24 | 4 |
| More than 2 y | 50 |
| Patient did not answer | 1 |
| Number of Lumbar Spine Surgical Procedures | Number of Patients That Had Lumbar Spine Surgical Procedures |
| 1 | 55 |
| 2 | 11 |
| 3 | 2 |
| 4 | 0 |
| 5 | 1 |
Table 2 provides details on the percentage change (relief and worsening) of pain immediately following spine surgery. The majority of patients reported 50%-100% relief immediately after surgery. Six patients reported no relief after surgery.
Table 2.
The Percentage of Patients Who Reported Relief or Worsening of Immediate Postsurgical Intervention
| Percentage Relief or Worsening | Number of Patients That Had Relief of Back and Lower Extremity Pain | Number of Patients That Had Worsening of Back and Lower Extremity Pain |
|---|---|---|
| 0% | 6 | 43 |
| 10% | 0 | 2 |
| 20% | 2 | 1 |
| 30% | 2 | 1 |
| 40% | 1 | 0 |
| 50% | 10 | 1 |
| 60% | 4 | 1 |
| 70% | 8 | 2 |
| 80% | 7 | 2 |
| 90% | 12 | 0 |
| 100% | 16 | 0 |
| N/A | 0 | 1 |
| Patient did not answer | 1 | 15 |
Table 3 outlines the fusion levels when performed and number of fused segments and the type of fusion surgery reported for 26 of the 29 known fusion patients. The majority of the 26 spinal fusion patients had only 1 or 2 levels fused; 1 had 5 levels fused. The majority of the fusions were at the L4-L5 level. Decompression laminectomy with fusion was the dominant fusion surgery.
Table 3.
Details on the Surgery of the 69 Patients (Lumbar Surgery With Fusion)
| Fusion Lumbar Surgery (26 Patients) | |
|---|---|
| Number of Levels Fused | Number of Patients |
| 1 | 6 |
| 2 | 8 |
| 3 | 2 |
| 4 | 1 |
| 5 | 1 |
| Patient did not answer | 8 |
| Spinal Segment Fused | Number of Patients |
| L2-L3 | 1 |
| L3-L4 | 1 |
| L4-L5 | 10 |
| L5-S1 | 1 |
| L1-S1 | 1 |
| L4-S1 | 3 |
| T10-L3 | 1 |
| Patient did not answer | 8 |
| Type of Surgery Performed | Number of Patients |
| Decompression laminectomy with fusion with screw and rod | 10 |
| Decompression laminectomy with bone fusion | 6 |
| Intertransverse process fusion | 0 |
| Other (cage fusion, spondylolisthesis bolt fusion) | 3 |
| Patient did not answer | 7 |
One patient did not answer. Two patients had fusion surgery as well as nonfusion surgery. (One of them had L3-L4 decompression laminectomy with bolt and rod fusion and 3-level decompression laminectomy without fusion; the second had 2 levels of metal cushions/hardware at L4-L5.)
Table 4 provides information on the details of 40 nonfusion surgical patient procedures. One or 2 levels of surgery and microdiscectomy and decompression laminectomy without fusion were the procedures most patients received.
Table 4.
Details on the Nonfusion Surgery Patients
| Without Fusion Lumbar Surgery (40 Patients) | |
|---|---|
| Number of Levels of Surgery | Number of Patients |
| 1 | 18 |
| 2 | 14 |
| 3 | 3 |
| 4 | 1 |
| 5 | 3 |
| Patient did not answer | 1 |
| Type of Surgery Performed | Number of Patients |
| Microdiscectomy | 15 |
| Decompression laminectomy without fusion | 19 |
| Disk replacement | 0 |
| Microdiscectomy and decompression laminectony without fusion | 1 |
| Other | 5 |
Table 5 provides the information on presurgical diagnosis. Most of the patients had disk herniations followed by spinal stenosis and other conditions.
Table 5.
Description of Diagnosis That Required Surgery
| Primary Presurgical Diagnosis | |
|---|---|
| Diagnosis | Number of Patients |
| Lumbar herniation | 39 |
| Spinal stenosis | 11 |
| Spondylolishthesis | 2 |
| Tumor | 0 |
| Scoliosis | 0 |
| Fracture | 1 |
| Discogenic back and leg pain | 5 |
| Lumbar herniation and spinal stenosis | 1 |
| Spinal stenosis and spondylolishthesis | 1 |
| Spinal stenosis and scoliosis | 1 |
| Scoliosis and DDD | 1 |
| Discogenic back and leg pain and scar tissue | 1 |
| Others (spondylosis w neuroforaminal narrowing and radiculopathy, cauda equina syndrome, right L4 synovial cyst, left L5 synovial cyst) | 4 |
| N/A | 2 |
DDD, degenerative disc disease.
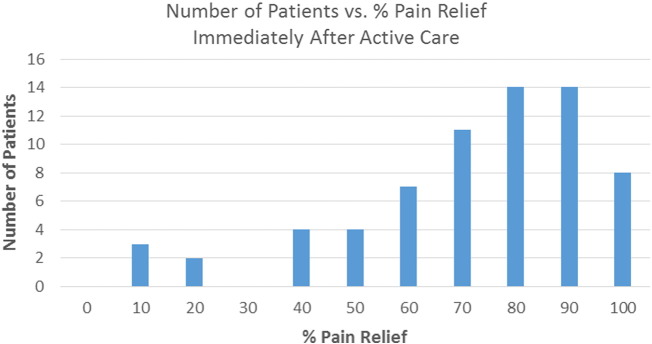
Fifty-four of 67 patients (81%) reported greater than 50% improvement in pain levels at the end of the last treatment provided, 13 (19%) reported less than 50% improvement in pain levels, and 2 patients did not answer (Fig 1). The NPS percentage of relief for the patients varied from 10% for 3 patients, 20% for 2, 40% for 4, 50% for 4, 60% for 7, 70% for 11, 80% for 14, 90% for 14, and 100% for 8 patients following active CTFD. The average number of treatments given was 11, and the average number of days of care was 49. At 24-month follow-up, data were obtainable from only 56 patients. Of these 56 patients, 44 (78.6%) had continued pain relief of greater than 50%, 10 (18%) reported 50% or less pain relief, and 2 patients did not answer (Fig 2). The mean percentage of relief at the end of initial active care was 71.6% (SD, 23.2) and at 24 months was 70% (SD, 25). Twenty-four months after active treatment, 24 patients (43%) had not sought further care, and 32 required further pain management consisting of 17 (53%) having further chiropractic manipulation; 9 (28%) having physical therapy, exercise regimens, injections, and medication; and 5 (16%) having repeat spinal surgery. One patient did not reply.
Fig 1.
Active care clinical outcome of patients receiving CTFD spinal manipulation.
Fig 2.
Twenty-four-month clinical outcome of patients receiving CTFD.
Discussion
Disability and back pain have biopsychosocial health relationships with the physical, psychological, and social factors of patients.16 Studies support this finding. Surgical decompression of the lumbar spine in older patients had a 24% reoperation rate,17 and a 20-fold increase in lumbar surgical fusion rates among Medicare enrollees is reported.18 Lumbar cage fusion rates increased from 3.6% in 1996 to 58% in 2001, and the result was increased complication risk without improved disability or reoperation rates.19 Adjacent segment degenerative changes and instability at the level immediately above single-segment fusion with clinical deterioration are shown in up to 90% of the cases.20, 21, 22, 23 The incidence of radiographic adjacent segment disease following fusion has been reported to be as high as 50% in the cervical spine and 70% in the lumbar spine at 10 years. However, the incidence of clinically relevant symptomatic adjacent segment disease is quite lower, estimated at 25% in the cervical spine and 36% in the lumbar spine at 10 years.24
Comparing surgery with nonsurgical treatment for back and radicular pain shows that intensive rehabilitation is more effective than fusion surgery,25 and nonsurgical treatment of low back and radicular pain patients is reported to reduce lumbar disk surgery by approximately two-thirds.26 Chronic low back pain in 349 patients aged 18-55 years found no evidence that surgery was any more beneficial than intensive rehabilitation.27 A study of 600 single-operated low back patients showed that 71% did not return to work 4 years after surgery, and 400 multiple-operated backs showed that 95% did not return to work 4 years later.28 Treating lumbar disk herniation and spinal stenosis patients successfully with conservative care is documented.29, 30, 31, 32 Chiropractic manipulation prior to spine surgery is appropriate.14
PSCP Spinal Manipulation Clinical Treatment and Benefit Outcomes
Previous reports of the biomechanical changes in the spine when CTFD spinal manipulation is applied include33 decreased intradiscal pressure; intervertebral disk foraminal area increase; increased intervertebral disk space height; and physiological range of motion of the facet joint.
Aspegren and Burt34 reported that the incidence of PSCP patients seeing a doctor of chiropractic was 68 of 1939 patients (3.75%) in a study of 12 chiropractic practices over a 30-day period. Thirty-two of the 68 cases were male (47%) and 36 were female (53%), with the average age being 52 years. Twelve percent of the 68 patients had undergone more than 1 lumbar spine surgery, and the average time since surgery was 14.5 (0.5-41) years. Thirteen of the 68 PSCP patients (19%) stated being worse following spine surgery.34 It is hypothesized that the PSCP patient is 3 times more likely to visit a doctor of chiropractic than the average citizen, whereas 70% of patients 4-17 years after discectomy still complain of low back pain with more than a third still under active treatment.34 Aspegren and Burt and this study agree on the treatment incidence of PSCP patients by doctors of chiropractic.
O’Shaughnessy et al35 cited positive outcomes following spinal manipulation for 8 patients with PSCP following total disk replacement. Other studies report positive outcomes in treating the PSCP patient with chiropractic spinal manipulation.36, 37, 38, 39, 40 Coulis and Lisi41 reported on 3 cases (1 cervical, 2 lumbar) of PSCP. They reported that 15% to 61% of spine surgery patients report persistent or recurring pain postsurgically, with 2.3% to 12% of them presenting to chiropractic offices. A 31-year-old man who suffered continuing PSCP with bilateral lower extremity pain 2.5 years following surgery was treated with CTFD after high-velocity, low-amplitude spinal manipulation increased the patient’s pain. His pain levels reduced to 4 of 10 from 7 of 10 following 16 treatments in 4 weeks. A 60-year-old man complaining of low back and right anterior lower extremity pain following an L3-5 laminectomy 27 years prior for herniated disks received combined CTFD and side posture adjusting. His pain was rated 7 to 10 of 10. Five visits over a 5-week period reduced his overall pain to a tolerable level that satisfied his quality of life.41
Kruse and Cambron42 reported that mean NPS pretreatment scores of 6.4 decreased to 2.3 in treating 32 PSCP patients (average age was 50.6 years, 50% equal male and female) with CTFD. Time from the first surgery to receiving spinal manipulation was 8.5 years. No adverse events were reported for any of the PSCP patients. Cox et al43 reported the clinical outcomes of treating 1000 low back and radicular pain patients with CTFD. Data for 1000 cases were collected from 30 chiropractic clinics with each treating at least 20 consecutive low back and leg pain patients who sought their care. A 293-variable data collection document was used by all clinics. In that study, L4-L5 and L5-S1 disk herniation patients showed 60.7% and 65.8% good to excellent response.
Limitations of the Study
This study is a retrospective case series report; therefore, it is nonexperimental and lacks a control or placebo group. There was no centralized treatment center with controlled clinical parameters for participating doctors; thus, there was diminished data collection control. Clinical treatment other than CTFD (eg, electrical stimulation, acupuncture, massage, or other nonsurgical care) may have occurred in conjunction with care and therefore may have influenced results. Not all data were able for all patients, and some were lost during the 24-month follow-up, which may have influenced final results. This study requires further basic science and clinical trial investigations to best define the role of chiropractic spinal manipulation in the treatment of postsurgical continued pain patients.
Conclusion
Sixty-nine PSCP patients received active chiropractic care for an average of 11 treatments over a 49-day period. Pain relief was 71.6%. Twenty-four months later, the sustained pain relief was 70%, with 32 patients needing further care to maintain pain relief. Postsurgical continued pain patients did demonstrate pain relief following specific chiropractic distraction spinal manipulation.
Funding Sources and Conflicts of Interest
James M. Cox, DC, DACBR, is developer of the technique used in treating the postsurgical continued pain patients and developed the spinal manipulation used in performing the manipulation. Dr Cox also is paid a royalty on the sale of the instrument. Drs Olding and Joachim are paid instructors of the Cox Technique seminars.
Acknowledgments
The authors thank the following chiropractic physicians who participated in the clinical data collection of patients presented in this article: Marc Baker, Keith Bartley, Jim Brandt, Walter Burt, Garry Butwell, James Cox, George Joachim, Lee Hazen, Ron Manoni, Stephen Novelli, Kurt Olding, Mike Poulin, Ted Siciliano, Kim Skibsted, and Mark Thompson.
References
- 1.Atlas S, Keller RB, Wu YA, Deyo RA, Singer DE. Long term outcomes of surgical and non-surgical management of sciatica secondary to lumbar disk herniation: 10 year results from the Maine lumbar spine study. Spine. 2005;30:927–935. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 2.Atlas SJ, Keller RB, Su YA, Deyo RA, Singer DE. Long term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the Maine lumbar spine study. Spine. 2005;30:936–941. doi: 10.1097/01.brs.0000158953.57966.c0. [DOI] [PubMed] [Google Scholar]
- 3.Foulongne E, Derrey S, Ould Slimane M. Lumbar spinal stenosis: which predictive factors of favorable functional results after decompressive laminectomy? Neurochirurgie. 2013;59:23–29. doi: 10.1016/j.neuchi.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Juricek M, Rehak L, Horvath J, Tisovsky P. Quality of life after elective lumbar spinal fusions. Bratisl Lek Listy. 2010;111:290–295. [PubMed] [Google Scholar]
- 5.Hussain A, Erdek M. Interventional pain management for failed back surgery syndrome. Pain Pract. 2014;14:64–78. doi: 10.1111/papr.12035. [DOI] [PubMed] [Google Scholar]
- 6.Choi HS, Chi EH, Kim MR. Demographic characteristics and medical service use of failed back surgery syndrome patients at an integrated treatment hospital focusing on complementary and alternative medicine: a retrospective review of electronic medical records. Evid Based Complement Alternat Med. 2014;2014:714389. doi: 10.1155/2014/714389. [Epub 2014 Nov 4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blond S, Mertens P, David R, Roulaud M, Rigoard P. From "mechanical" to "neuropathic" back pain concept in fbss patients. a systematic review based on factors leading to the chronification of pain (part c) Neurochirurgie. 2015 doi: 10.1016/j.neuchi.2014.11.001. [pii: S0028-3770(14)00276-8, Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Chou R, Loeser JD, Owens DK. Interventional therapies, surgery and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine. 2009;34:1066–1077. doi: 10.1097/BRS.0b013e3181a1390d. [DOI] [PubMed] [Google Scholar]
- 9.Katz JN. Lumbar disc disorders and low back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88A:10–14. doi: 10.2106/JBJS.E.01273. [Suppl.] [DOI] [PubMed] [Google Scholar]
- 10.Davis MA, Onega T, Weeks WB, Lurie JD. Where the United States spends its spine dollars: expenditures on different ambulatory services for the management of back and neck conditions. Spine. 2012;37:1693–1701. doi: 10.1097/BRS.0b013e3182541f45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Modhia U, Takemoto S, Braid-Forbes MJ, Weber M, Berven SH. Readmission rates after decompression surgery in patients with lumbar spinal stenosis among medicare beneficiaries. Spine. 2013;38:591–596. doi: 10.1097/BRS.0b013e31828628f5. [DOI] [PubMed] [Google Scholar]
- 12.Gamache FW. The value of "another" opinion for spinal surgery: a prospective 14-month study of one surgeon's experience. Surg Neurol Int. 2012;3(Suppl. 5):S350–S354. doi: 10.4103/2152-7806.103867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DePalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med. 2011;12:732–739. doi: 10.1111/j.1526-4637.2011.01098.x. [DOI] [PubMed] [Google Scholar]
- 14.Daffner SD, Hymanson HJ, Wang JC. Cost and use of conservative management of lumbar disc herniation before surgical discectomy. Spine J. 2010;10:463–468. doi: 10.1016/j.spinee.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Cox JM. 7th rev. ed. Lippincott, Williams & Wilkins; Philadelphia: 2011. Low back pain: mechanism, diagnosis, treatment; p. 362. [Google Scholar]
- 16.Foster NE, Delitto A. Embedding psychosocial perspectives within clinical management of low back pain: integration of psychosocially informed management principles into physical therapist practice—challenges and opportunities. Phys Ther. 2011;91:790–803. doi: 10.2522/ptj.20100326. [DOI] [PubMed] [Google Scholar]
- 17.Mannion AF, Denzler R, Dvorak J, Grob D. Five-year outcome of surgical decompression of the lumbar spine without fusion. Eur Spine J. 2010;19:1883–1891. doi: 10.1007/s00586-010-1535-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinstein J, Lurie JD, Olson PR, Bronner K, Fisher ES. United States' trends and regional variations in lumbar spine surgery: 1992-2003. Spine. 2006;31:2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Juratli S, Maghout MD, Franklin GM, Mirza S, Wickizer TM, Fulton-Kehoe D. Lumbar fusion outcomes in Washington state workers' compensation. Spine. 2006;31:2715–2723. doi: 10.1097/01.brs.0000244589.13674.11. [DOI] [PubMed] [Google Scholar]
- 20.Zencica P, Chaloupka R, Hladíková J, Krbec M. Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis] Acta Chir Orthop Traumatol Cech. 2010;77:124–130. [PubMed] [Google Scholar]
- 21.Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine. 2004;29:1535–1540. doi: 10.1097/01.brs.0000131417.93637.9d. [DOI] [PubMed] [Google Scholar]
- 22.Röllinghoff M, Schlüter-Brust K, Groos D. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia) 2010;20(2(1)):e3. doi: 10.4081/or.2010.e3. [doi:] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Celestre PC, Montgomery SR, Kupperman AI, Aghdasi B, Inoue H, Wang JC. Lumbar clinical adjacent segment pathology: predilection for proximal levels. Spine. 2014;39:172–176. doi: 10.1097/BRS.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 24.Levin DA, Hale JJ, Bendo JA. Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bull NYU Hosp Jt Dis. 2007;65(1):29–36. [PubMed] [Google Scholar]
- 25.Chou R, Qaseem A, Snow V. Clinical efficacy assessment subcommittee of the American College Of Physicians; American College Of Physicians; American Pain Society low back pain guidelines panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 26.Rasmussen RA, Nielsen C, Hansen VK, Jensen OK, Schioettz-Christensen B. Rates of lumbar disc surgery before and after implementation of multidisciplinary nonsurgical spine clinics. Spine. 2005;30:2469–2473. doi: 10.1097/01.brs.0000184686.70838.96. [DOI] [PubMed] [Google Scholar]
- 27.Fairbank J. Randomized controlled trial to compare surgical stabilization of the lumbar spine with an intensive rehabilitation program for patients with chronic low back pain. The MRC Stabilization Trial. British Med J. 2005;330:1233–1239. doi: 10.1136/bmj.38441.620417.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berger E. Late postoperative results in 1000 work related lumbar spine conditions. Surgical Neurolog. 2000;54:101–106. doi: 10.1016/s0090-3019(00)00283-4. [DOI] [PubMed] [Google Scholar]
- 29.Froholdt A, Reikeraas O, Holm I, Keller A, Brox JI. No difference in 9-year outcome in clbp patients randomized to lumbar fusion versus cognitive intervention and exercises. European Spine Journal. 2012;21:2531–2536. doi: 10.1007/s00586-012-2382-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hagen KB, Dagfinrud H, Moe RH. Exercise therapy for bone and muscle health: an overview of systematic reviews. BMC Med. 2012;10:167–175. doi: 10.1186/1741-7015-10-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beattie PF, Nelson RM, Michener LA, Cammarata J, Donley J. Outcomes after a prone lumbar traction protocol for patients with activity-limiting low back pain: a prospective case series study. Arch Phys Med Rehabil. 2008;89:269–274. doi: 10.1016/j.apmr.2007.06.778. [DOI] [PubMed] [Google Scholar]
- 32.Apfel CC, Cakmakkaya OS, Martin W. Restoration of disk height through non-surgical spinal decompression is associated with decreased discogenic low back pain: a retrospective cohort study. BMC Musculoskelet Disord. 2010;11:155. doi: 10.1186/1471-2474-11-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gudavalli MR, Cambron JA, McGregor M. A randomized clinical trial and subgroup analysis to compare flexion-distraction with active exercise for chronic low back pain. Eur Spine J. 2006;15:1070–1082. doi: 10.1007/s00586-005-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aspegren DD, Burt AL. A study of postspinal surgery cases in chiropractic offices. Journal of Manipulative and Physiological Therapeutics. 1994;17:88–92. [PubMed] [Google Scholar]
- 35.O'Shaughnessy J, Drolet M, Roy JF, Descarreaux M. Chiropractic management of patient’s post-disc arthroplasty: eight case reports. Chiropractic & Osteopathy. 2010;18:7. doi: 10.1186/1746-1340-18-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morningstar MW, Strauchman MN. Manipulation under anesthesia for patients with failed back surgery: retrospective report of 3 cases with 1-year follow-up. Journal Chiropractic Medicine. 2012;11:30–35. doi: 10.1016/j.jcm.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMorland G, Suter E, Casha S, du Plessis SJ, Hurlbert RJ. Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. J Manipulative Physiol Ther. 2010;33:576–584. doi: 10.1016/j.jmpt.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 38.Estadt GM. Chiropractic/rehabilitative management of post-surgical disc herniation: a retrospective case report. J Chiropr Med. 2004;3:108–115. doi: 10.1016/S0899-3467(07)60095-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murphy DR, Hurwitz EL, Gregory AA, Clary R. A non-surgical approach to the management of lumbar spinal stenosis: a prospective observational cohort study. BMC Musculoskeletal Disorder. 2006;23(7):16–22. doi: 10.1186/1471-2474-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cox JM. Chiropractic Orthopedics Conference Proceedings. Annual symposium on Investigation of Failed Low Back Surgery; 2009 May 8-May 10; San Antonio, Texas. Published by the American College of Chiropractic Orthopedists and Southern California University of Health Sciences and Texas Council of Chiropractic Orthopedists. American College of Chiropractic Orthopedists. 2009. Spinal adjusting of failed low back surgery; pp. 43–112. [Google Scholar]
- 41.Coulis CM, Lisi AJ. Chiropractic management of postoperative spine pain: a report of 3 cases. Journal of Chiropractic Medicine. 2013;12:168–175. doi: 10.1016/j.jcm.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kruse RA, Cambron J. Chiropractic management of postsurgical lumbar spine pain: a retrospective study of 32 cases. Journal of Manipulative and Physiological Therapeutics. 2011;34:408–412. doi: 10.1016/j.jmpt.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 43.Cox JM, Feller J, Cox-Cid J. Distraction chiropractic adjusting: clinical application and outcomes of 1000 cases. Top Clin Chiropr. 1996;3(3):45–59. [Google Scholar]