Abstract
Background:
Susceptibility-guided therapies (SGTs) have been proposed as preferable to empirical rescue treatments after two treatment failures. The aim of this study was to perform a systematic review and meta-analysis evaluating the effectiveness and efficacy of SGT as third-line therapy.
Methods:
A systematic search was performed in multiple databases. Studies reporting cure rates of Helicobacter pylori with SGT in third-line therapy were selected. A qualitative analysis describing the current evidence and a pooled mean analysis summarizing the cure rates of SGT in third-line therapy was performed.
Results:
No randomized controlled trials or comparative studies were found. Four observational studies reported cure rates with SGT in third-line treatment, and three studies which mixed patients with second- and third-line treatment also reported cure rates with SGT. The majority of the studies included the patients when culture had been already obtained, and so the effectiveness of SGT and empirical therapy has never been compared. A pooled mean analysis including four observational studies (283 patients) showed intention-to-treat and per-protocol eradication rates with SGT of 72% (95% confidence interval 56–87%; I2: 92%) and 80% (95% confidence interval 71–90%; I2: 80%), respectively.
Conclusions:
SGT may be an acceptable option as rescue treatment. However, cure rates are, at best, moderate and this approach has never been compared with a well-devised empirical therapy. The evidence in favor of SGT as rescue therapy is currently insufficient to recommend its use.
Keywords: Helicobacter pylori, tailored treatment, susceptibility-guided treatment, third-line treatment
Introduction
Helicobacter pylori infection is the major cause of chronic gastritis, peptic ulcers, gastric mucosa-associated lymphoid tissue lymphoma (MALT) and gastric cancer. Its worldwide prevalence approaches 50% [McColl, 2010].
The standard triple therapy combining amoxicillin (1 g b.d.) and clarithromycin (500 mg b.d.) or metronidazole (500 mg b.d.) has long been the recommended first-line therapy for H. pylori infection [Malfertheiner et al. 2012]. However, this combination seems to have lost efficacy over the last decade [Malfertheiner et al. 2012], mostly due to clarithromycin resistance [Neri et al. 2003]. The overall clarithromycin resistance rate in Europe increased from 9% in 1998 to 17.6% in 2008 [Malfertheiner et al. 2012], and primary resistances are above 20% in many European countries [Megraud et al. 2013].
The Maastricht IV/Florence consensus [Malfertheiner et al. 2012] suggests that culture and standard susceptibility testing should be considered in all regions before second-line treatment if endoscopy is carried out for another reason (evidence level: 5; grade of recommendation: D). However, challenging this expert opinion, a recent meta-analysis of randomized controlled trials (RCTs) [Lopez-Gongora et al. 2015] did not observe significant differences between susceptibility-guided therapies (SGT) and empirical therapy as second-line treatment in the few comparative studies performed. Furthermore, the studies included in the meta-analyses did not compare SGT versus the currently recommended quadruple therapies, and allocated patients once the endoscopy and culture was performed. Whether the need for invasive testing reduces the acceptability and the effectiveness of SGT in clinical practice remains uncertain. Finally, the evidence regarding SGT in third-line treatment has not been systematically revised to date.
The aim of this study was to perform a systematic review and meta-analysis evaluating the evidence of the efficacy of SGT in the treatment of H. pylori after two failed attempts.
Material and methods
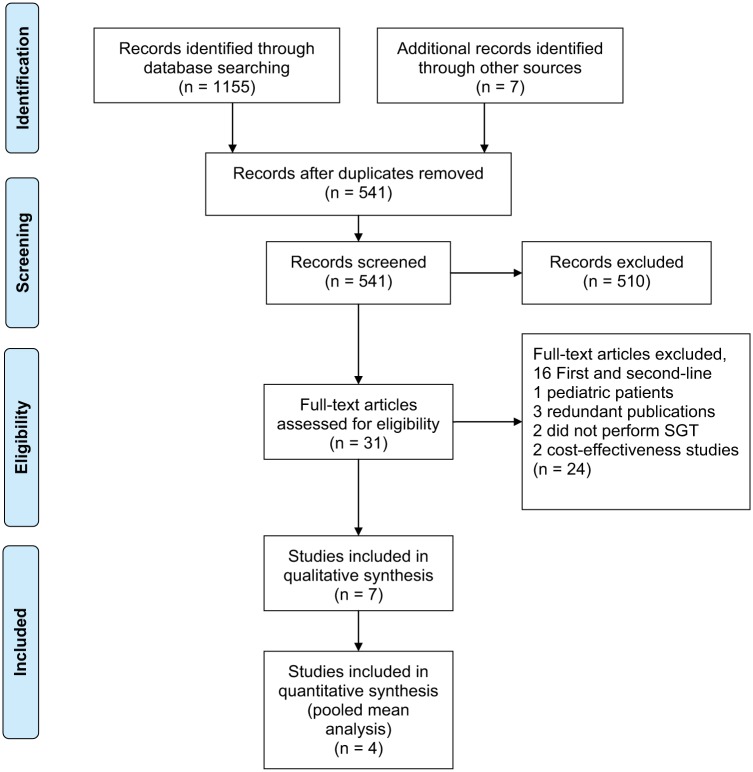
The study was performed in accordance with the MOOSE Statement [Stroup et al. 2000], because the systematic review and meta-analysis included observational studies. The MOOSE checklist is shown in the online Supplementary Table 1. A flow-chart of the studies included in the meta-analyses is shown in Figure 1.
Figure 1.
Flow of information through the various phases of the selection of the studies.
Search strategy
A systematic computerized literature search was conducted in PubMed, Scopus, the Cochrane Library and the ISI Web of Knowledge including full-text published articles and abstracts from the of DDW, UEGW, EHSG and other relevant meetings from 1984 to May 2015. Combinations of different terms combinations are shown in the online Supplementary Table 2. In addition, references of articles retrieved and significant reviews were also examined, searching for articles to include in the present study. Finally, the personal databases of the authors were also reviewed for eligible publications.
Inclusion criteria
We included published full-text articles that fulfilled the following criteria: (a) they reported clinical trials, observational series or comparative cohort studies that evaluated the H. pylori eradication rates in adult patients who received SGT; (b) SGT was used as rescue treatment after two failed attempts; (c) pretreatment diagnostic tests for H. pylori detection comprised one or more of the common validated tests [urea breath test, histology, rapid urease test, stool antigen, polymerase chain reaction (PCR) or culture]; (d) all of these tests (except culture) were considered adequate as control tests; (e) control diagnostic tests were performed at least 4 weeks after the end of the eradication schedule in the absence of proton pump inhibitor (PPI) use. No language limitations were imposed.
Data extraction
Data were extracted independently by four reviewers (SL, VG, MB and IP) and revised by a fifth investigator (AV). Discordances were resolved by consensus with an additional investigator (XC). Data extraction was standardized using a data extraction table. Variables compiled were: (a) number of patients; (b) type of study (RCT, quasi-RCT, comparative non-RCT, noncomparative); (c) method used to determine antibiotic susceptibility; (d) percentage of successful cultures; (e) time of randomization (before or after endoscopy); (f) intention to treat (ITT) and (g) per-protocol (PP) cure rates and their 95% confidence intervals (CIs) for the susceptibility-guided treatment group; and for the control empiric treatment group when available (h) adherence to treatment and (i) number and severity of side effects.
Risk of bias
Risk of bias was assessed independently by three reviewers (IP, SLG and MB). Discrepancies in the interpretation were resolved with a third reviewer (XC). Observational studies were assessed following the suggestions of Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Agency for Healthcare Research and Quality, 2014]. We recorded whether the study was labeled as prospective, the completeness of outcome data, the presence of selective reporting and the validity of pre- and post-treatment eradication tests.
Statistical analysis
The primary endpoint for the different meta-analyses was the ITT efficacy. Secondary endpoints were PP efficacy, adherence and adverse events.
As the number of comparative studies (either randomized or observational) available in third-line treatments was insufficient, the mean eradication rate of SGT was calculated by combining data from observational noncomparative studies and using the generic inverse variance method, which involves a weighted average of the estimated effect from the individual studies. The weight for each study is taken to be the inverse of the variance (one divided by the square of the standard error) of the estimated effect. If studies differed in terms of treatments administered, a random effect model was used. The I2 statistic was used to assess the heterogeneity of the studies following the recommendation of the Cochrane Collaboration’s Handbook for Systematic Reviews of Interventions [Higgins and Green, 2011], as follows: 0–40%, negligible heterogeneity; 40–75%, moderate heterogeneity; 75–100% considerable heterogeneity. Analyses were performed using the freeware program Review Manager (RevMan) version 5.1 [The Cochrane Collaboration, 2012].
Results
The original searches retrieved more than 1000 articles. Following a review of the abstracts, 34 articles were assessed for eligibility. No unpublished abstracts were found. After careful evaluation of the full texts, seven were included in the qualitative analysis and four in the pooled mean analysis (Figure 1).
Studies excluded
A total of 24 studies were finally excluded, for the following reasons: (a) 16 included patients receiving only first- or second-line therapy [Neri et al. 2003; Furuta et al. 2007; Avidan et al. 2001; Biscontri et al. 2001; Cosme et al. 2013; Kawai et al. 2008; Lamouliatte et al. 2003; Lee et al. 2013; Marzio et al. 2006; Miwa et al. 2003; Molina-Infante et al. 2012; Romano et al. 2003; Sugimoto et al. 2014; Toracchio et al. 2000; Wang et al. 2008; Zhou et al. 2010]; (b) one included pediatric patients [Lopes et al. 2005]; (b) three reported data on patients already included in another study [Gomollón et al. 2000; Furuta et al. 2005; Romano et al. 2000]; (c) two did not perform susceptibility-guided treatment [Seppala et al. 2000; Graham et al. 2000]; (d) two were cost-effectiveness studies [Breuer and Graham, 1999; Zullo et al. 2003b].
Studies included reporting cure rates of SGT in third-line treatment
No RCTs or studies comparing SGT versus empirical treatment after two H. pylori eradication attempts were found. Only four observational noncomparative studies including 283 patients reported the mean cure rates of SGT in third-line therapy [Cammarota et al. 2004; Gasbarrini et al. 2000; Liou et al. 2013; Vicente et al. 2002]. In addition, two noncontrolled studies [Fiorini et al. 2013; Tay et al. 2012] and one controlled nonrandomized study [Yahav et al. 2006] reported cure rates of SGT mixing patients with second and third-line treatment. All of the studies except one [Gasbarrini et al. 2000] included patients once endoscopy had been performed; furthermore, in many of them, patients were included only when a positive culture had been obtained. So, the effectiveness and applicability of SGT in clinical practice could not be evaluated.
Table 1 shows the main characteristics of the studies and cure rates of SGT. Previous antibiotic treatment and antibiotic strategy according to susceptibility tests varied widely (Tables 2 and 3). The risk of bias for observational studies is summarized in Figure 2. All of the studies were non-RCTs, but were described as prospective, included consecutive patients, used a valid diagnostic and control test and reported complete data.
Table 1.
Characteristics of the studies reporting cure rates of SGT after two failed attempts.
| Study and country | N | Study design | Method for determining antibiotic susceptibility | Successful culture | Empiric treatment cure rates |
Susceptibility-guided treatment cure rates |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ITT (%) | 95% CI | PP (%) | 95% CI | ITT (%) | 95% CI | PP (%) | 95% CI | |||||
| Second-line treatment | ||||||||||||
| Cammarota et al. [2004], Italy | 94 | NC | E-test | 94/98 | – | – | – | – | 85/94 (90) | 81–94 | 85/93 (91) | 82–95 |
| Gasbarrini et al. [2000], Italy | 58 | NC | E-test | 39/49 | – | – | – | – | 30/58 (52) | 37–64 | 30/39 (77) | 60–88 |
| Liou et al. [2013], Taiwan | 135 | NC | PCR and agar dilution | – | – | – | – | – | 109/135 (81) | 73–87 | 109/132 (83) | 75–88 |
| Vicente et al. [2002], Spain | 40 | NC | E-test | 41/42 | – | – | – | – | 24/40 (60) | 43–75 | 24/38 (63) | 46–78 |
| Mixed second and third-line treatment | ||||||||||||
| Fiorini et al. [2012], Italy | 254 | NC | E-test | 236/254 | – | – | – | – | 211/254 (83) | 77–87 | 212/236 (90) | 84–93 |
| Tay et al. [2012], Australia | 310 | NC | E-test | 306/310 | – | – | – | – | 291/310 (94) | 90–96 | 291/310 (94) | 90–96 |
| Yahav et al. [2006], Israel | 98 | CNR | E-test | 49/49 | 31/49 (63) | 47–75 | 31/49 (63) | 47–75 | 42/49 (86) | 72–93 | 42/49 (86) | 72–93 |
CI, confidence interval; CNR, controlled nonrandomized study; E-test, Epsilometer test; ITT, intention-to-treat; NC, noncontrolled study; PP, per-protocol; SGT, susceptibility-guided therapy.
Table 2.
Antimicrobial therapies used in third-line therapy studies.
| Study | First-line treatment | Second-line treatment | Drug resistance after the second treatment failure | Susceptibility-guided third-line treatment | N | Treatment duration |
|---|---|---|---|---|---|---|
| Cammarota et al. [2004] | PPI b.d., A 1 g b.d., M 250 mg q.d. or TI 500 mg b.d. for 7 days (n = 37) | PPI (double dose per day), A 1 g, C 250 or 500 mg b.d. for 7 days (n = 27) PPI (double dose per day), A 1 g, L 500 mg b.d. for 7 days (n = 7) O 20 mg b.d., B 120 mg q.d.s., A 1 g b.d., TE 500 mg q.d.s. for 7 days (n = 3) |
M: 100% C: 95% L: 31% TE: 5% A: 0% |
A and TE sensitive: B 120 mg q.d,s., O 20 mg b.d., A 1 g b.d., D 100 mg b.d. |
89 | 7 days |
| PPI, A 1 g, C 250 or 500 mg b.d. for 7 days (n = 34) | PPI (double dose per day), B 120 mg q.d.s., M 250 mg q.d.s or TI 500 mg b.d., TE 500 mg q.d.s. for 7 days (n = 28) PPI (double dose per day), A 1 g, L 500 mg b.d. for 7 days (n = 6) |
TE, M and C resistant: O 20 mg b.d., A 1 g b.d., L 500 mg b.d. |
4 | 7 days | ||
| PPI b.d., A 1 g, L 500 mg b.d. for 7 days (n = 23) | PPI (double dose per day), A 1 g, C 250 or 500 mg b.d. for 7 days (n = 11) O 20 mg b.d., B 120 mg q.d.s., A 1 g b.d., TE 500 mg q.d.s. for 7 days (n = 2) PPI (double dose per day), B 120 mg q.d.s., M 250 mg q.d.s or TI 500 mg b.d., TE (500 mg q.d.s for 7 days (n = 10) |
TE, M and L resistant: O 20 mg, A 1 g, C 500 mg b.d. |
1 | 7 days | ||
| Gasbarrini et al. [2000] | PPI, TI, C 7 days (n = 58) | RBC, A C 7 days (n = 58) | AZ: 68% ER: 62% C: 56% M and TI 56% TE 12% A 0% |
PPI, B, A, TE | 26 | Not reported |
| PPI, B, A, M | 9 | |||||
| PPI, B, TE, M | 4 | |||||
| Liou et al. [2013] | 100% (131/131) received C and 79.1% (102/129) L in first or in second line | 23S rRNA mutation (tissue) 78.9% (101/128) 23S rRNA mutation (strain) 85.7% (84/98) Gyrase A mutation (tissue) 41.3% (52/126) Gyrase A mutation (strain) 42.9% (42/98) L resistance 46.9% (45/96) A resistance 9.4% (9/96) M resistance 58.3% (56/96) TE resistance 3.2% (3/93) C resistance 86.5% (83/96) |
23S rRNA wild-type: ES 40 mg, A 1 g, M 500 mg, C 500 mg b.d. |
19 | ES, A 7 days followed by M, C 7 days | |
| 23S rRNA mutant-type and gyrA wild-type: ES 40 mg, A 1 g, M 500 mg, L 250 mg b.d. |
51 | ES, A 7 days followed by M, LE 7 days | ||||
| 23S rRNA mutant-type and gyrA mutant-type: ES 40 mg, A 1 g, M 500 mg, TE 500 mg b.d. |
65 | ES, A 7 days followed by M, TE 7 days | ||||
| Vicente et al. [2002] | Not reported | Not reported | M resistance 44% (18/41) C resistance 52% (21/41) Both C and M resistance 19% (5/41) A 0% TE 0% |
Susceptible to C and M: O 20 mg b.d., B 120 mg q.d., TE 500 mg q.d., C 500 mg b.d. |
9 | 14 days |
| Resistant to C: O 20 mg b.d., B 120 mg q.d., TE 500 mg q.d., A 1 g b.d. |
13 | 14 days | ||||
| Resistant to M: O 20 mg b.d., B 120 mg q.d., TE 500 mg q.d., C 500 mg b.d./ A 1 g b.d. |
10 | 14 days | ||||
| M and C resistant and penicillin allergy: O 20 mg b.d., B 120 mg q.d., TE 500 mg q.d., CI 500 mg b.d. |
8 | 14 days | ||||
PPI, proton pump inhibitor; A, amoxicillin; C, clarithromycin; L, levofloxacin; M, metronidazole; TI, tinidazole; b.d., twice a day; q.d.s., four times a day; TE, tetracycline; B, bismuth; O, omeprazole; D, doxycycline; RBC, ranitidine bismuth citrate; AZ, azithromycin; ER, erythromycin; ES, esomeprazole; SGT, susceptibility-guided therapy.
Table 3.
Antimicrobial therapies used in mixed second- and third-line therapy studies.
| Study | Previous treatments | Drug resistances before SGT | Empiric therapy | N | Treatment duration | SGT | N | Treatment duration |
|---|---|---|---|---|---|---|---|---|
| Fiorini et al. [2013] | Not reported | L + C + M 33% (79/236) L + C 3% (8/236) L + M 3% (7/236) C + M 25% (60/236) C 20% (48/236) M 4% (10/10) |
Not administered | – | – | Susceptible to L: ES 40 mg, A 1g, L 250 mg b.d. |
131 | 10 days |
| Resistant to L: ES 40 mg, A 1 g b.d., RFB 150 mg o.d. |
105 | 12 days | ||||||
| Tay et al. [2012] | First line: O, A, C 7-day Second line: O, A, C/M 7-14 days |
C 94% (288/306) M 68% (207/306) C and M 65% (199/306) CIP 5.6% RIF 2% A 0% TE 0% |
Not administered | – | – | Susceptible to RFB and CIP, no penicillin allergy: RA 20 mg t.d.s., A 1 g t.d.s., RFB 150 mg b.d., CIP 500 mg b.d. |
210 | RA and A 10 days. RFB and CIP 5 days |
| Susceptible to RIF and CIP, penicillin allergy: RA 20 mg t.d.s., B 240 q.d, RFB 150 mg b.d., CIP 500 mg b.d. |
69 | 10 days | ||||||
| Resistant to RIF or CIP or failure of RIF and CIP-based therapy: PPI, B, FU, A or RFB PPI, A, M PPI, B, TE, FU or A |
26 | 10 days | ||||||
| Yahav et al. [2006] | First: O, C, A or O, M, A 7-day Second: O,C, M, A or O, B, M, TE 7-day |
M 47% (23/49) C 59% (29/49) Both C and M 29% (14/49) |
O 20 mg, A 1 g, C 500 mg b.d. | 11 | 7 days | Susceptible to C: O 20 mg, A 1 g, C 500 mg b.d. |
34 | 7 days |
| O 20 mg, A 1 g, M 500 mg b.d. | 6 | 7 days | Resistant to C and susceptible to M: O 20 mg, A 1 g, M 500 mg b.d. |
|||||
| O 20 mg b.d., B 120 q.d., M 500 mg b.d., TE 500 mg q.d. | 11 | 7 days | Allergic to penicillin: O 20 mg b.d., B 120 q.d.s., TE 500 mg q.d., M 500 mg b.d. |
15 | 7 days | |||
| Resistant to C and M: O 20 mg b.d., B 120 mg q.d., TE 500 mg q.d., A 1 g b.d. |
A, amoxicillin; b.d., twice a day; B, bismuth; C, clarithromycin; CIP, ciprofloxacin; FU, furazolidone; L, levofloxacin; M, metronidazole; O, omeprazole; o.d., once a day; RA, rabeprazole; RFB, rifabutin; RIF, rifampicin; t.d.s., three times a day; TE, tetracycline; SGT, susceptibility-guided therapy.
Figure 2.
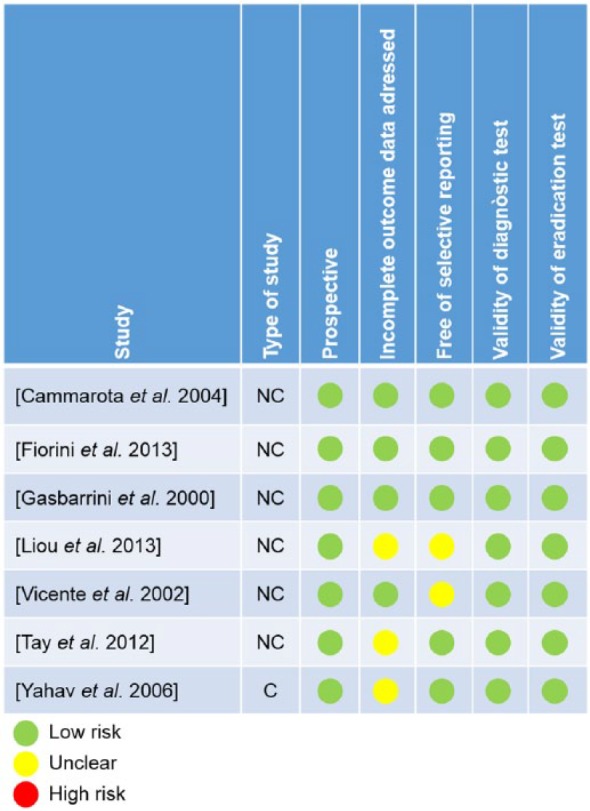
Risk of bias of the studies included in the qualitative analysis.
Cammarota and colleagues conducted a prospective study in Italy including 94 consecutive patients who underwent endoscopy with antral biopsies and in whom successful susceptibility analyses were obtained using the Epsilometer test (E-test) [Cammarota et al. 2004]. In the ITT analysis they did not include 14 patients who had shown poor compliance with the previously prescribed regimens. Four eligible patients were also excluded from the ITT analysis because H. pylori could not be cultured. First-line treatments consisted of a 7-day triple therapy based on a PPI, amoxicillin and clarithromycin, levofloxacin or an imidazole. In second-line treatment, a 7-day bismuth quadruple therapy or a different 7-day triple therapy was administered. In third-line treatment, H. pylori harbored a high prevalence of resistant strains (metronidazole 100%, clarithromycin 95%, levofloxacin 31%, tetracycline 5%, amoxicillin 0%). A 7-day bismuth quadruple therapy containing amoxicillin, tetracycline and omeprazole was used in 89 patients. The five patients harboring tetracycline-resistant strains were treated with a 7-day triple therapy with levofloxacin or clarithromycin. Following this strategy, and taking into account the restrictive inclusion criteria (patients with good previous compliance, positive culture, etc.) and the many exclusions, they obtained cure rates of 90% (ITT) and 91% (PP).
In Italy, Gasbarrini and colleagues evaluated the efficacy of a multistep strategy for H. pylori eradication [Gasbarrini et al. 2000]. A total of 2606 H. pylori-positive patients were administered tinidazole, clarithromycin and a PPI for 1 week. A total of 350 patients with continuing infection were then given a second 1-week course of amoxicillin, clarithromycin and ranitidine bismuth citrate. A total of 58 patients still infected after the second course were invited to undergo an upper gastrointestinal endoscopy with H. pylori culture, but only 49 accepted. Finally, H. pylori culture was obtained in 39 out of these 49 patients. In vitro antibiotic susceptibility analysis by using the E-test showed a high overall prevalence of poly-antibiotic-resistant H. pylori strains (azithromycin 68%, erythromycin 62%, clarithromycin 56%, metronidazole and tinidazole 56%, tetracycline 12% and amoxicillin 0%). They received a 1-week quadruple PPI-bismuth-based scheme established on H. pylori antibiotic sensitivity, and achieved a mean eradication rate of 77% by PP analysis (30 out of 39) or 51.7% by ITT (30 out of 58).
In Taiwan, Liou and colleagues conducted a study in 135 patients who underwent an upper endoscopy and biopsies [Liou et al. 2013]. The study did not state the number of patients who declined endoscopy. Genotypic and phenotypic resistances were determined by PCR with direct sequencing (23S rRNA and gyrA) and agar dilution test, respectively. The authors found an excellent correlation between clarithromycin and levofloxacin phenotypic and genotypic resistance. The patients were re-treated with a sequential therapy containing esomeprazole and amoxicillin for the first 7 days, followed by esomeprazole and metronidazole plus clarithromycin, levofloxacin or tetracycline for another 7 days according to the genotypic resistance determined using gastric biopsy specimens. The overall eradication rate was 80.7% (109/135) in the ITT analysis and 82.6% (109/132) in the PP analysis.
Vicente and colleagues included 42 patients in a Spanish multicenter observational study who failed both a 7-day triple therapy and a second-line empirical attempt [Vicente et al. 2002]. These authors found a prevalence of resistance to clarithromycin and metronidazole around 50% by using the E-test and administered a 14-day bismuth-containing quadruple therapy. Four patients were not included in the PP analyses (one patient with culture failure, one with multidrug allergy, one who did not accept the treatment and one more who did not attend the follow-up visit). H. pylori was cured in only 60% of infected patients despite good compliance (>90% in all the patients included). Surprisingly, cure was not achieved in six out of nine patients infected by a H. pylori strain susceptible to all antibiotics. The authors suggest that, in addition to antibiotic resistances, unknown factors (for instance, host immunogenicity or differences in the adherence of H. pylori to the mucosa) may also influence treatment efficacy.
In Italy, Fiorini and colleagues included 254 patients who failed at least one standard therapy for H. pylori eradication and underwent an upper endoscopy [Fiorini et al. 2013]. A total of 44% had failed at least two treatment attempts. Culture was obtained in 236 patients (93%) and a susceptibility analysis using the E-test identified 131 patients with levofloxacin-susceptible and 105 with levofloxacin-resistant strains. In patients with levofloxacin-susceptible H. pylori strains, 50% were resistant to clarithromycin and metronidazole, 43% to clarithromycin alone and 8% to metronidazole alone. In the levofloxacin-resistant H. pylori strains, 85% were also resistant to clarithromycin and metronidazole and 8% to both clarithromycin and metronidazole alone. Patients received either 10 days of levofloxacin or 12 days of rifabutin (in the case of patients resistant to levofloxacin) in combination with amoxicillin and esomeprazole. All patients took at least 90% of the prescribed drugs. H. pylori infection was cured in 90% of the patients who received levofloxacin triple therapy and 89% of the patients who received rifabutin triple therapy. Unfortunately, the results for second- and third-line treatments were not reported separately.
In Australia, Tay and colleagues successfully cultured 306 H. pylori strains from 310 consecutive patients who had completed and failed at least one course of the standard 7-day triple therapy containing PPI and combinations of amoxicillin, clarithromycin or metronidazole [Tay et al. 2012]. The proportions resistant to clarithromycin and metronidazole using the E-test were 94.1% and 67.6%, respectively, with 65% presenting resistance to both. Resistance to ciprofloxacin and rifampicin was 6% and 2%, respectively. In patients harboring rifampicin-susceptible strains, 10-day treatment with rabeprazole and amoxicillin plus rifabutin and ciprofloxacin from day 6, for 5 days, was prescribed. This schedule obtained a 95% cure rate. Again, the results for second- and third-line treatments were not reported separately.
Finally, in Israel Yahav and colleagues enrolled 49 patients who also failed at least one treatment course and in whom an upper endoscopy and culture had been performed [Yahav et al. 2006]. These authors compared the efficacy of SGT with a cohort of patients who received empirical rescue treatment. Resistance rates to clarithromycin and metronidazole by using the E-test were 59% and 47%, respectively (29% to both antibiotics). The empirical treatment consisted in a 7-day triple therapy containing clarithromycin or metronidazole or a 7-day bismuth-containing quadruple therapy. In the experimental group, the same therapies were administered but depending on the susceptibility of the H. pylori strain. SGT was significantly more efficacious than empirical therapy (86% versus 63%, p = 0.02).
Pooled mean analysis of cure rates of SGT as third-line treatment
As no RCTs or comparative observational studies reporting efficacy of SGT versus empirical therapy were found, a meta-analysis of cure rates of SGT of noncomparative studies was performed. ITT and PP analyses including four studies (283 patients) showed mean eradication rates of 72% (95% CI 56–87%; I2: 92%) and 80% (95% CI 71–90%; I2: 80%), respectively. In view of the lack of comparative trials and the high heterogeneity between the studies, this pooled mean cure rate should be interpreted with caution. The poorest results according to ITT were shown in the only study that reported rates of patients’ acceptance of upper endoscopy and the rates of positive culture. As these two issues were not considered in the ITT analysis of the remaining studies, the effectiveness in clinical practice may be even lower.
Safety and side effects
Percentages of patients with adverse events were generally not reported. Cammarota and colleagues reported poor tolerance of quadruple bismuth therapy, and 1 out of 94 patients abandoned treatment due to severe side effects [Cammarota et al. 2004]; Liou and colleagues reported a dropout rate of 1% due to side effects [Liou et al. 2013]; and Vicente and colleagues reported no severe adverse events or dropouts [Vicente et al. 2002]. Fiorini and colleagues reported mild-to-moderate side effects in 15% and 20% of patients in each treatment arm; however, all patients complied with at least 90% of the treatment [Fiorini et al. 2013]. Gasbarrini and colleagues, Tay and coworkers and Yahav’s group did not mention the number of patients with adverse events, though the latter author reported a treatment compliance of 97% [Gasbarrini et al. 2000; Tay et al. 2012; Yahav et al. 2006].
Discussion
The present study highlights the lack of strong evidence regarding SGT in third-line therapy, as no RCTs or comparative studies with empirical treatment were found. The pooled mean analysis of cure rates including four observational noncomparative studies showed ITT and PP mean cure rates of 72% and 80%, respectively. However, the heterogeneity of the studies was high and this pooled mean cure rate should be interpreted carefully. Although the PP cure rate after two failed attempts was acceptable, ITT cure rates were not as good as desired. Furthermore, as three out of the four studies included patients once the endoscopy and the culture was obtained, the acceptance of an invasive procedure and feasibility of a successful culture was not considered. So, the effectiveness in clinical practice may be even lower than 70%. However, if the patient accepts an invasive test and a culture is feasible, SGT may be an acceptable strategy in third-line treatment.
This study agrees with the Maastricht consensus which suggested that treatment could be guided by antimicrobial susceptibility testing, whenever possible, after failure of second-line therapy (evidence level: 4; grade of recommendation: A). On the other hand, empirical treatment after two failed attempts has shown heterogeneous results: 65–85% with bismuth-containing quadruple therapies [Hsu et al. 2008; Gisbert et al. 2014], 60–90% with levofloxacin-based therapy [Sereni et al. 2012; Tursi et al. 2012; Gisbert et al. 2006; Zullo et al. 2003a] and 62–95% with a rifabutin-based therapy associated with PPIs and amoxicillin [Lim et al. 2014; González et al. 2007]. The studies differ in terms of previously administered therapies, study populations and drug schedules. So, until comparative studies are available, SGT also seems to be an acceptable treatment option in third-line treatment.
The major strong points of the study are the updated systematic review, the qualitative analysis and the pooled mean analyses of cure rates for summarizing the current evidence. The quality of the observational studies was acceptable. However, major limitations are the lack of comparative analyses, the high heterogeneity between the studies and the evaluation of acceptance of an invasive test and the feasibility of H. pylori culture. All of the studies tend to use four drugs or long therapies after antibiotic sensitivity testing. Therefore, it is difficult to ascertain whether the improved cure rates are due to the determination of antibiotic resistances or to the use of far more effective therapies. This aspect requires future investigation.
In conclusion, SGT may be an acceptable option as rescue treatment. However, cure rates are, at best, moderate and this approach has never been compared with a well-devised empirical therapy, particularly with the highly effective quadruple therapies. The evidence in favor of SGT as rescue therapy is currently insufficient to recommend its use in clinical practice.
Supplementary Material
Supplementary Material
Acknowledgments
We thank Michael Maudsley for his help with the English.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: Xavier Calvet has served on advisory boards or received research grants or fees for educational activities from Pfizer, MSD and Abbvie; research grants from Janssen-Cilag; and served as an advisor and received fees for educational activities from Shire. There are no conflicts of interest related to the content of the present article. Albert Villoria has received fees for educational activities from MSD and Abbvie. There are no conflicts of interest related to the content of the present article. Sheila López-Góngora, Ignasi Puig, Mireia Baylina, David Suarez, Victor García-Hernando and Javier P. Gisbert have no relevant conflicts of interest to report. Writing support was provided by Michael Maudsley and funded by CIBERehd.
Contributor Information
Ignasi Puig, Digestive Diseases Unit, Althaia Xarxa Assistencial Universitaria de Manresa. Barcelona, Spain; Departament de Medicina, Universitat Autònoma de Barcelona, Barcelona, Spain; Universitat Internacional de Catalunya, Barcelona, Spain.
Sheila López-Góngora, Internal Medicine Department, Corporació Sanitària Universitària Parc Taulí, Sabadell, Spain.
Xavier Calvet, Servei d’Aparell Digestiu, Hospital de Sabadell, Departament de Medicina, Universitat Autònoma de Barcelona, Centro de Investigación Biomédica en Red de enfermedades hepáticas y digestivas (CIBERehd), Instituto de Salud Carlos III, Parc Taulí, 1 08208 Sabadell (Barcelona), Spain.
Albert Villoria, Departament de Medicina, Universitat Autònoma de Barcelona, Barcelona, Spain; Digestive Diseases Unit, Corporació Sanitaria Universitària Parc Taulí, Sabadell, Spain; Centro de Investigación Biomédica en Red de enfermedades hepáticas y digestivas (CIBERehd), Madrid, Spain.
Mireia Baylina, Internal Medicine Department, Corporació Sanitària Universitària Parc Taulí, Sabadell, Spain.
Jordi Sanchez-Delgado, Departament de Medicina, Universitat Autònoma de Barcelona, Barcelona, Spain; Digestive Diseases Unit, Corporació Sanitaria Universitària Parc Taulí, Sabadell, Spain; Centro de Investigación Biomédica en Red de enfermedades hepáticas y digestivas (CIBERehd), Madrid, Spain.
David Suarez, Unitat d’Epidemiologia i Avaluació, Hospital de Sabadell, Sabadell, Spain.
Victor García-Hernando, Departament de Medicina, Universitat Autònoma de Barcelona, Barcelona, Spain.
Javier P. Gisbert, Centro de Investigación Biomédica en Red de enfermedades hepáticas y digestivas (CIBERehd), Madrid, Spain Servicio de Aparato Digestivo, Hospital Universitario de la Princesa, Instituto de Investigación Sanitaria Princesa (IP), Madrid, Spain.
References
- Agency for Healthcare Research and Quality (2014) Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville, MD: Agency for Healthcare Research and Quality (US). [PubMed] [Google Scholar]
- Avidan B., Melzer E., Keller N., Bar-Meir S. (2001) The effect of culture results for Helicobacter pylori on the choice of treatment following failure of initial eradication. Isr Med Assoc J 3: 163–165. [PubMed] [Google Scholar]
- Biscontri M., Lisi L., Pellegrini M., Bayeli P. (2001) Helicobacter pylori infection: Culture and antibiotic essay. Argomenti Gastroenterol Clin 14: 81–88. [Google Scholar]
- Breuer T., Graham D. (1999) Costs of diagnosis and treatment of Helicobacter pylori infection: When does choosing the treatment regimen based on susceptibility testing become cost effective? Am J Gastroenterol 94: 725–729. [DOI] [PubMed] [Google Scholar]
- Cammarota G., Martino A., Pirozzi G., Cianci R., Branca G., Nista E., et al. (2004) High efficacy of 1-week doxycycline- and amoxicillin-based quadruple regimen in a culture-guided, third-line treatment approach for Helicobacter pylori infection. Aliment Pharmacol Ther 19: 789–795. [DOI] [PubMed] [Google Scholar]
- Cosme A., Montes M., Martos M., Gil I., Mendarte U., Salicio Y., et al. (2013) Usefulness of antimicrobial susceptibility in the eradication of Helicobacter pylori. Clin Microbiol Infect 19: 379–383. [DOI] [PubMed] [Google Scholar]
- Fiorini G., Vakil N., Zullo A., Saracino I., Castelli V., Ricci C., et al. (2013) Culture-based selection therapy for patients who did not respond to previous treatment for Helicobacter pylori infection. Clin Gastroenterol Hepatol 11: 507–510. [DOI] [PubMed] [Google Scholar]
- Furuta T., Shirai N., Kodaira M., Sugimoto M., Nogaki A., Kuriyama S., et al. (2007) Pharmacogenomics-based tailored versus standard therapeutic regimen for eradication of H. pylori. Clin Pharmacol Ther 81: 521–528. [DOI] [PubMed] [Google Scholar]
- Furuta T., Sugimoto M., Nakamura A., Shirai N. (2005) Susceptibility to antibiotics and drug metabolism in patients with H. pylori infection refractory to the initial treatment - therapeutic strategy based on susceptibility to CAM and CYP2C19 polymorphism. Nippon Rinsho 63(Suppl. 11): 426–433. [PubMed] [Google Scholar]
- Gasbarrini A., Ojetti V., Armuzzi A., Branca G., Canducci F., Torre E., et al. (2000) Efficacy of a multistep strategy for Helicobacter pylori eradication. Aliment Pharmacol Ther 14: 79–83. [DOI] [PubMed] [Google Scholar]
- Gisbert J., Castro-Fernandez M., Bermejo F., Perez-Aisa A., Ducons J., Fernandez-Bermejo M., et al. (2006) Third-line rescue therapy with levofloxacin after two H-Pylori treatment failures. Am J Gastroenterol 101: 243–247. [DOI] [PubMed] [Google Scholar]
- Gisbert J., Perez-Aisa A., Rodrigo L., Molina-Infante J., Modolell I., Bermejo F., et al. (2014) Third-line rescue therapy with bismuth-containing quadruple regimen after failure of two treatments (with clarithromycin and levofloxacin) for H. pylori infection. Dig Dis Sci 59: 383–389. [DOI] [PubMed] [Google Scholar]
- Gomollón F., Sicilia B., Ducóns J., Sierra E., Revillo M., Ferrero M. (2000) Third line treatment for Helicobacter pylori: A prospective, culture-guided study in peptic ulcer patients. Aliment Pharmacol Ther 14: 1335–1338. [DOI] [PubMed] [Google Scholar]
- González Carro P., Pérez Roldán F., De Pedro Esteban A., Legaz Huidobro M., Soto Fernández S., Roncero Garcia Escribano O., et al. (2007) Efficacy of rifabutin-based triple therapy in Helicobacter pylori infected patients after two standard treatments. J Gastroenterol Hepatol 22: 60–63. [DOI] [PubMed] [Google Scholar]
- Graham D., Osato M., Hoffman J., Opekun A., Anderson S., El-Zimaity H. (2000) Furazolidone combination therapies for Helicobacter pylori infection in the United States. Aliment Pharmacol Ther 14: 211–215. [DOI] [PubMed] [Google Scholar]
- Higgins J., Green S. (2011) Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. [Google Scholar]
- Hsu P., Wu D., Chen A., Peng N., Tseng H., Tsay F., et al. (2008) Quadruple rescue therapy for Helicobacter pylori infection after two treatment failures. Eur J Clin Invest 38: 404–409. [DOI] [PubMed] [Google Scholar]
- Kawai T., Yamagishi T., Yagi K., Kataoka M., Kawakami K., Sofuni A., et al. (2008) Tailored eradication therapy based on fecal Helicobacter pylori clarithromycin sensitivities. J Gastroenterol Hepatol 23: S171-S174. [DOI] [PubMed] [Google Scholar]
- Lamouliatte H., Mégraud F., Delchier J., Bretagne J., Courillon-Mallet A., De Korwin J., et al. (2003) Second-line treatment for failure to eradicate Helicobacter pylori: A randomized trial comparing four treatment strategies. Aliment Pharmacol Ther 18: 791–797. [DOI] [PubMed] [Google Scholar]
- Lee H., Kim J., Cheung D., Kim T., Jun E., Oh J., et al. (2013) Eradication of Helicobacter pylori according to 23S ribosomal RNA point mutations associated with clarithromycin resistance. J Infect Dis 208:1123–1130. [DOI] [PubMed] [Google Scholar]
- Lim H., Lee Y., An B., Lee S., Lee Y., Moon B. (2014) Rifabutin-based high-dose proton-pump inhibitor and amoxicillin triple regimen as the rescue treatment for Helicobacter pylori. Helicobacter 19: 455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liou J., Chen C., Chang C., Chen M., Fang Y., Lee J., et al. (2013) Efficacy of genotypic resistance-guided sequential therapy in the third-line treatment of refractory Helicobacter pylori infection: a multicentre clinical trial. J Antimicrob Chemother 68: 450–456. [DOI] [PubMed] [Google Scholar]
- Lopes A., Oleastro M., Palha A., Fernandes A., Monteiro L. (2005) Antibiotic-resistant Helicobacter pylori strains in Portuguese children. Pediatr Infect Dis J 24: 404–409. [DOI] [PubMed] [Google Scholar]
- Lopez-Gongora S., Puig I., Calvet X., Villoria A., Baylina M., Munoz N., et al. (2015) Systematic review and meta-analysis: susceptibility-guided versus empirical antibiotic treatment for Helicobacter pylori infection. J Antimicrob Chemother 70: 2447–2455. [DOI] [PubMed] [Google Scholar]
- Malfertheiner P., Megraud F., O’Morain C., Atherton J., Axon A., Bazzoli F., et al. (2012) Management of Helicobacter pylori infection - the Maastricht IV/ Florence Consensus Report. Gut 61: 646–664. [DOI] [PubMed] [Google Scholar]
- Marzio L., Coraggio D., Capodicasa S., Grossi L., Cappello G. (2006) Role of the preliminary susceptibility testing for initial and after failed therapy of Helicobacter pylori infection with levofloxacin, amoxicillin, and esomeprazole. Helicobacter 11: 237–242. [DOI] [PubMed] [Google Scholar]
- McColl K. (2010) Clinical practice. Helicobacter pylori infection. N Engl J Med 362: 1597–1604. [DOI] [PubMed] [Google Scholar]
- Megraud F., Coenen S., Versporten A., Kist M., Lopez-Brea M., Hirschl A., et al. (2013) Helicobacter pylori resistance to antibiotics in Europe and its relationship to antibiotic consumption. Gut 62: 34–42. [DOI] [PubMed] [Google Scholar]
- Miwa H., Nacahara A., Kurosawa A., Ohkusa T., Ohkura R., Hojo M., et al. (2003) Is antimicrobial susceptibility testing necessary before second-line treatment for Helicobacter pylori infection? Aliment Pharmacol Ther 17: 1545–1551. [DOI] [PubMed] [Google Scholar]
- Molina-Infante J., Pazos-Pacheco C., Vinagre-Rodriguez G., Perez-Gallardo B., Dueñas-Sadornil C., Hernandez-Alonso M., et al. (2012) Nonbismuth quadruple (concomitant) therapy: empirical and tailored efficacy versus standard triple therapy for clarithromycin-susceptible Helicobacter pylori and versus sequential therapy for clarithromycin-resistant strains. Helicobacter 17: 269–276. [DOI] [PubMed] [Google Scholar]
- Neri M., Milano A., Laterza F., Di Bonaventura G., Piccolomini R., Caldarella M., et al. (2003) Role of antibiotic sensitivity testing before first-line Helicobacter pylori eradication treatments. Aliment Pharmacol Ther 18: 821–827. [DOI] [PubMed] [Google Scholar]
- Romano M., Iovene M., Montella F., Vitale L., De Simone T., Del Vecchio Blanco C. (2000) Pretreatment antimicrobial-susceptibility testing in the eradication of H. pylori infection. Am J Gastroenterol 95: 3317–3318. [DOI] [PubMed] [Google Scholar]
- Romano M., Marmo R., Cuomo A., De Simone T., Mucherino C., Iovene M., et al. (2003) Pretreatment antimicrobial susceptibility testing is cost saving in the eradication of Helicobacter pylori. Clin Gastroenterol Hepatol 1: 273–278. [PubMed] [Google Scholar]
- Seppala K., Kosunen T., Nuutinen H., Sipponen P., Rautelin H., Sarna S., et al. (2000) Cure of Helicobacter pylori infection after failed primary treatment: One-center results from 120 patients. Scand J Gastroenterol 35: 929–934. [DOI] [PubMed] [Google Scholar]
- Sereni G., Azzolini F., Camellini L., Formisano D., Decembrino F., Iori V., et al. (2012) Efficacy of a therapeutic strategy for eradication of Helicobacter pylori infection. World J Gastroenterol 18: 4542–4548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup D., Berlin J., Morton S., Olkin I., Williamson G., Rennie D., et al. (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- Sugimoto M., Uotani T., Sahara S., Ichikawa H., Yamade M., Sugimoto K., et al. (2014) Efficacy of tailored Helicobacter pylori eradication treatment based on clarithromycin susceptibility and maintenance of acid secretion. Helicobacter 19: 312–318. [DOI] [PubMed] [Google Scholar]
- Tay C., Windsor H., Thirriot F., Lu W., Conway C., Perkins T., et al. (2012) Helicobacter pylori eradication in Western Australia using novel quadruple therapy combinations. Aliment Pharmacol Ther 36: 1076–1083. [DOI] [PubMed] [Google Scholar]
- The Cochrane Collaboration (2012) Review Manager (RevMan), Version 5.2. Copenhagen: The Nordic Cochrane Centre. [Google Scholar]
- Toracchio S., Cellini L., Di Campli E., Cappello G., Malatesta M., Ferri A., et al. (2000) Role of antimicrobial susceptibility testing on efficacy of triple therapy in Helicobacter pylori eradication. Aliment Pharmacol Ther 14: 1639–1643. [DOI] [PubMed] [Google Scholar]
- Tursi A., Picchio M., Elisei W. (2012) Efficacy and tolerability of a third-line, levofloxacin-based, 10-day sequential therapy in curing resistant Helicobacter pylori infection. J Gastrointest Liver Dis 21: 133–138. [PubMed] [Google Scholar]
- Vicente R., Sicilia B., Gallego S., Revillo M., Ducóns J., Gomollón F. (2002) Helicobacter pylori eradication in patients with peptic ulcer after two treatments failure: A prospective culture-guided study. Gastroenterol Hepatol 25: 438–442. [DOI] [PubMed] [Google Scholar]
- Wang G., Zhao Q., Li S. (2008) Study of drug sensitivity test in Helicobacter pylori eradication therapy. J Clin Intern Med 25: 474–477. [Google Scholar]
- Yahav J., Samra Z., Niv Y., Evans C., Passaro D., Dinari G., et al. (2006) Susceptibility-guided vs. empiric retreatment of Helicobacter pylori infection after treatment failure. Dig Dis Sci 51: 2316–2321. [DOI] [PubMed] [Google Scholar]
- Zhou J., Huo H., Wu M., Jiang X. (2010) Role of drug sensitivity test in the triple therapy for eradication of Helicobacter pylori. Chin J Gastroenterol 15: 358–360. [Google Scholar]
- Zullo A., Hassan C., Lorenzetti R., Winn S., Morini S. (2003a) A clinical practice viewpoint: to culture or not to culture Helicobacter pylori? Dig Liver Dis 35: 357–361. [DOI] [PubMed] [Google Scholar]
- Zullo A., Hassan C., De Francesco V., Lorenzetti R., Marignani M., Angeletti S., et al. (2003b) A third-line levofloxacin-based rescue therapy for Helicobacter pylori eradication. Dig Liver Dis 35: 232–236. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.