Abstract
Background
Non-operating room (non-OR) airway management has previously been identified as an area of concern because it carries a significant risk for complications. One reason for this could be attributed to the independent practice of residents in these situations. The aim of the present study was to ascertain whether differences in performance exist between residents working alone vs with a resident partner when encountering simulated non-OR airway management scenarios.
Methods
Thirty-six anaesthesia residents were randomized into two groups. Each group experienced three separate scenarios (two scenarios initially and then a third 6 weeks later). The scenarios consisted of one control scenario and two critical event scenarios [i.e. asystole during laryngoscopy and pulseless electrical activity (PEA) upon post-intubation institution of positive pressure ventilation]. One group experienced the simulated non-OR scenarios alone (Solo group). The other group consisted of resident pairs, participating in the same three scenarios (Team group).
Results
Although the time to intubation did not differ between the Solo and Team groups, there were several differences in performance. The Team group received better overall performance ratings for the asystole (8.5 vs 5.5 out of 10; P<0.001) and PEA (8.5 vs 5.8 out of 10; P<0.001) scenarios. The Team group was also able to recognize asystole and PEA conditions faster than the Solo group [10.1 vs 23.5 s (P<0.001) and 13.3 vs 36.0 s (P<0.001), respectively].
Conclusions
Residents who performed a simulated intubation with a second trained provider had better overall performance than those who practised independently. The residents who practised in a group were also faster to diagnose serious complications, including peri-intubation asystole and PEA. Given these data, it is reasonable that training programmes consider performing all non-OR airway management with a team-based method.
Keywords: airway management, high-fidelity simulation, team-based anaesthesia
Editor's key points.
It is not clear whether or not performance of a resident in cardiopulmonary resuscitation outside the operating theatre can be improved by the presence of another person.
Residents were randomized to two groups, and residents performed cardiopulmonary resuscitation, with or without another person.
Performance of cardiopulmonary resuscitation by a team was better than by one person.
Although the majority of airway management performed by anaesthetists occurs in the operating room (OR), there are many instances where it takes place in settings such as medical wards, intensive care units (ICUs), emergency departments (EDs), and other procedural locations. Although OR intubations are performed in a relatively ‘controlled’ environment, non-OR intubations can be emergent in nature and performed in suboptimal conditions (e.g. missing or unfamiliar equipment, difficulties in patient positioning on patient beds, involvement from staff unfamiliar with airway management).1 Not surprisingly, reported complications from non-OR intubations are numerous (e.g. failed intubation, aspiration, mainstem intubation, haemodynamic compromise),2 and complication rates as high as 27% have been described.3
Although the reasons for non-OR airway management-related complications are myriad, the emergent nature, a lack of expected resources, and superimposed patient co-morbidities are likely to be major contributors. It is perhaps not surprising that complications related to out-of-OR intubations make up a significant number of cases in the ASA closed claims database.4 Most studies have determined that patients intubated in the presence of an attending physician were less likely to suffer complications,1,5 although Schwartz and colleagues6 found no such effect. Although it has been suspected that the presence of a second anaesthesia provider can have a positive effect on patient outcomes,7 studying the performance of anaesthetists in non-OR scenarios has proved difficult.
The influence of a second anaesthesia resident on performance of non-OR intubations is not clear. This may be a lost opportunity, because a recent study at a tertiary care centre revealed that residents working alone managed 64% of non-OR intubations (i.e. without a second trained assistant or attending physician).8 Although similar studies are lacking, this percentage is likely to be representative of the practice at other major academic medical centres. As there is an ethical dilemma in allowing trainees to engage in airway management on their own for the sole purpose of research, simulation affords an opportunity to study performance in an analogous environment. The aim of the present study was to ascertain whether differences in performance exist between residents working alone vs with a resident partner when encountering simulated non-OR airway management scenarios.
Methods
A waiver of written consent was granted for this study by the Mount Sinai Hospital Program for the Protection of Human Subjects. Thirty-six resident physicians from the Department of Anesthesiology, encompassing clinical anaesthesia years 1, 2, and 3 (CA-1, CA-2, and CA-3) were voluntarily enrolled (out of 60 available at the time of study offering). Participants were assigned unique identifiers and randomized to groups based on random integer generator data in Microsoft Excel (Microsoft Corp., Redmond, WA, USA; Fig. 1). One group performed all intubations without an assistant (‘Solo’ cohort), whereas the other group worked in pairs and had predefined roles as laryngoscopist or assistant (‘Team’ cohort), with the pre-assigned laryngoscopist maintaining that role throughout the simulation scenarios (Table 1).
Fig 1.
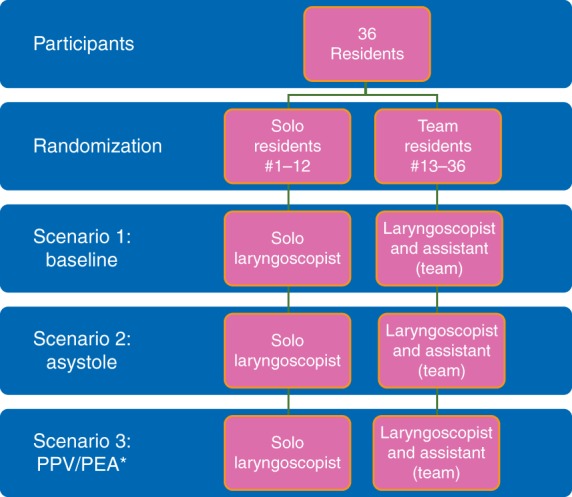
Randomization scheme and study time line. PEA, pulseless electrical activity; PPV, positive pressure ventilation; *Scenario 3 occurred 6 weeks after Scenarios 1 and 2.
Table 1.
Simulation scenarios
| Scenarios |
|---|
| Scenario 1: standard, uncomplicated floor intubation proceeding uneventfully |
| Scenario 2: floor intubation complicated by asystole during laryngoscopy because of intense vagal stimulus of laryngoscopy (simulated airway made ‘difficult’ via tongue swelling feature) |
| Scenario 3: intensive care unit intubation complicated by pulseless electrical activity cardiac arrest with initiation of positive pressure ventilation |
Baseline participant characteristics were obtained from a survey given at the beginning of the experiment. For our purposes, a resident was defined as a senior resident if they had completed 1 yr of anaesthesia training [e.g. CA-2/postgraduate year (PGY)3 or CA-3/PGY4]. All junior residents (i.e. CA-1/PGY2) enrolled in the study had completed at least 6 months of anaesthesia training and were credentialled by the department to respond independently to airway management consultations outside of the OR at the time of the study. Blinding was not feasible for this study, because both participants and observers would easily be able to distinguish who was working solo vs those working as a member of a team. However, participants did not know what sort of scenarios they would be encountering or what sort of performance ratings would be collected.
Once assigned to their respective groups, residents participated in three simulated scenarios. We used a high-fidelity human patient simulator (CAE HPS; CAE, Gainesville, FL, USA) with predetermined clinical scenarios to test residents in simulated ‘floor intubations’. In each scenario, the anaesthesia resident (or team) was called to intubate a patient located on an inpatient ward or ICU.
Although all residents at Mount Sinai are familiar with the simulator and the simulated environment, each underwent a 30 min group orientation on the equipment and the simulator's capabilities before the study, for purposes of standardization. The simulation laboratory was designed to resemble a standard inpatient hospital ward or unit bed. A five-lead ECG, automatic non-invasive blood pressure cuff, and pulse oximeter were available in each instance, although not yet attached to the patient at the start of the scenario. Although continuous carbon dioxide monitoring (waveform capnography) is standard of care in the operating room and in many critical care units, it was not routinely available for ‘floor’ intubations at our institution at the time of study, and therefore, was not made available to participants in the study.
All roles of the actors in the simulated environment were scripted and standardized. These included a nurse, who was instructed to assist the residents only when given specific tasks but not to take initiative to set up any equipment beyond what was asked for by the participants. Also present was a technician, who operated the simulator but did not participate in the scenarios. There was no communication between the technician and study subjects.
Each participant experienced three distinct scenarios lasting ∼5–10 min in duration. During the scenario, they were scored by a real-time rater. Confirmation of successful intubation was also made by the technician at the conclusion of each scenario by laryngoscopic examination. Other performance data included time to successful intubation (the time from introduction of the laryngoscope blade into the mannequin's mouth until the attachment of a manual self-inflating resuscitation device to the tracheal tube), time to recognition of asystole during laryngoscopy (for Scenario 2), and time to recognition of pulseless electrical activity (PEA) on initiation of positive pressure ventilation (PPV; for Scenario 3). Subjects were graded by the rater through a pre-established grading scheme examining preparation for airway management, induction of anaesthesia, intubation, and overall performance (Appendix 1).
Scenarios
Participants were brought in for two separate sessions. During the first session, subjects completed Scenarios 1 and 2. After the first session, residents were brought back 6 weeks later to experience Scenario 3. The simulator was set up in order to facilitate the easiest possible intubating conditions in Scenario 1, with a slight increase in difficulty in Scenario 2. The subjects were allowed to ask for any and all necessary medications or equipment that would typically be available on the hospital ‘floor’. Available equipment and specific scenario details can be found in Appendix 2.
Statistical analysis
Descriptive data were presented as the median [range] for continuous variables and n (%) for categorical variables. For comparisons between solo and team groups, we used Cochran–Mantel–Haenszel tests for repeated measures to evaluate the global rating scores because the scores were in ordinal scale and evaluated by two reviewers. We used Wilcoxon rank sum tests to compare the time required for successful diagnosis.
Results
Study group characteristics were as follows: Solo group participants were a median age of 29 yr and Team group participants 30 yr of age; half of each cohort was from the CA-1 class and half from the CA-2 and CA-3 classes; 67% of the Solo and 75% of the Team group participants were male. Intubation was ultimately successful by each participant, for each scenario, irrespective of group assignment. The time taken for laryngoscopy also did not differ by group for each scenario (17.5 vs 18.0 s for Solo and Team cohorts, respectively).
Ratings of preparation for airway management, induction of anaesthesia, and intubation, and overall global ratings of performance are presented in Table 2. In Scenarios 2 and 3, the Team participants performed better than Solo laryngoscopists on the overall performance category, with significant differences noted for the categorical ratings of preparation. The technical performance of tracheal intubation was not rated as different across groups for any of the scenarios.
Table 2.
Global rating scores by scenario (median [25th–75th percentile]). Each category had a maximal score of 10, where 10 was the best performance and 1 the worst. PEA, pulseless electrical activity; PPV, positive pressure ventilation. *P<0.05 and **P<0.001
| Scenario 1 |
Scenario 2 (asystole) |
Scenario 3 (PPV/PEA) |
||||
|---|---|---|---|---|---|---|
| Category | Solo | Team | Solo | Team | Solo | Team |
| Preparation | 8.5 [7.3–9.0] | 8.5 [8.5–9.0] | 8.0 [6.5–8.8]* | 8.5 [8.5–9.0]* | 8.0 [7.5–9.0]* | 8.5 [8.5–9.0]* |
| Induction/intubation | 8.5 [7.5–9.0] | 8.5 [8.5–9.0] | 8.5 [7.0–8.8] | 8.5 [8.5–9.0] | 8.5 [7.5–9.0] | 8.5 [8.5–9.0] |
| Post-induction management | 9.0 [7.8–9.0] | 8.5 [8.5–9.0] | 8.0 [5.8–8.5] | 8.5 [7.5–9.0] | 8.0 [6.0–8.5] | 8.5 [7.0–9.0] |
| Overall performance | 9.0 [7.5–9.0] | 9.0 [9.0–9.5] | 5.5 [5.0–7.4]** | 8.5 [7.5–9.0]** | 5.8 [5.0–7.0]** | 8.5 [7.5–9.0]** |
As part of Scenarios 2 and 3, participants were timed as to how long it took for them to recognize and treat either asystole during laryngoscopy or PEA upon institution of PPV, respectively (Table 3). These differed by group assignment, with the Team participants performing faster than Solo participants.
Table 3.
Time intervals for successful diagnosis and treatment of adverse events. *P<0.01
| Scenario 2 (asystole) |
Scenario 3 (PPV/PEA) |
|||
|---|---|---|---|---|
| Solo | Team | Solo | Team | |
| Time [s; mean (sd)] | 23.5 (17.7)* | 10.1 (19.3)* | 36.0 (17.4)* | 13.3 (23.6)* |
Discussion
Team-based models of care are largely promoted in health care, especially for high-acuity patient care areas.9 Anaesthesia providers often perform airway management in non-operative settings, and these areas have been identified as hazard prone.2,3 After appropriate training, our institution, like others,8 permits residents to manage patients' airways independently in out-of-OR locales without the presence of a trained assistant. The present study demonstrates that (at least in a simulated environment) the presence of another anaesthesia resident significantly increased the odds of prompt recognition and treatment of severe complications during airway management, namely asystole or PEA. Additionally, the presence of a second trained provider increased subjective scores of performance in these scenarios as measured by their preparation for airway management and overall performance during the entire procedure.
Airway management outside the OR is an endeavour fraught with potential complications and even poor outcomes.10 These complications have been well documented, and some institutions have developed difficult airway response teams consisting of a senior anaesthestist and an otolaryngologist, with specific equipment not traditionally available in these settings, to address these concerns.11,12 The implementation of a team approach to management of critical events has found success in a number of arenas in medicine (e.g. rapid response teams, ‘code’ teams).13 Early data on these teams reveals a significant decrease in in-hospital mortality, and the team-based model of care appears to be a successful one.14,15 Unfortunately, many institutions may not have the resources required to form airway response teams, and thus will continue to rely on trainees working independently to perform the majority of out-of-OR airway management.
In this study, the presence of trained assistance aided in the recognition of significant complications of induction of anaesthesia, direct laryngoscopy, and initiation of PPV in out-of-OR scenarios. Additionally, the presence of trained assistance increases subjective measures of preparation and recognition of complications in this high-risk setting. As a result of these data, our department internally adopted policies requiring two providers to be present at floor intubations and recommending that residents continue to bring a fellow resident or attending physician for assistance irrespective of seniority. This is in addition to our existing protocol requiring two providers (including an attending physician) to be present at intubations in the ED, ICU, or for paediatric patients.
There are several potential weaknesses of this study that we acknowledge, some of which may potentially limit broader applicability. Although the simulated environment can be an excellent place for training clinical personnel, there is controversy regarding the extension of outcomes in the simulation centre to the clinical environment.16,17 Additionally, significant controversy exists regarding the durability of skills learned in the simulated environment.18–22 Given the nature of performance grading (e.g. rater watching the scenario unfold), the rater was not blinded to which subjects worked solo vs as a team. Additionally, we studied a cohort of anaesthesia residents in one specific programme acclimated to a given patient population and ancillary staffing and resources; this is potentially not generalizable to a wider variety of institutions and practice settings. Another potential weakness is based around the clinical applicability of our data. Although the clinical complications studied were identified faster by the team cohort, the significance of 10–20 s faster diagnosis and treatment may not be clinically relevant. While the stroke23 and myocardial infarction24 literature highlight that time is of the essence (i.e. ‘time is tissue’) when responding to critical events, the implication of these several seconds on patient outcome (even in a patient cohort so heterogeneous and often with extensive cardiopulmonary disease and requiring emergency intubation) is uncertain. For example, administration of anaesthetic agents and initiation of PPV in haemodynamically unstable patients may result in haemodynamic decompensation within seconds.25 We also do not know why teams performed better than solo anaesthesia residents, although one might surmise that division of workload improved performance here, as it has been shown to do in many other tasks.9
Airway management outside of the OR is challenging and often the purview of trainees who are functioning independently. Although the present study was simulation based, it suggests the utility of having residents work in pairs when managing airways in off-site locations. We saw an improved ability rapidly to detect and treat cardiovascular derangements occurring simultaneously or contemporaneously with airway management, and an improvement in the overall performance of airway management. Further work is necessary to elucidate the level of training and supervision needed to optimize such teams, but this study suggests that added assistance can improve the overall performance of airway management in non-OR settings.
Authors' contributions
Study design: S.D., A.L.
Data collection: S.D., D.B., A.L.
Data analysis: S.D., D.B., A.G., H.-M.L., Y.K., A.L.
Manuscript writing: S.D., D.B., A.G., H.-M.L., Y.K., A.L.
Declaration of interest
None declared.
Funding
Department of Anesthesiology of the Icahn School of Medicine at Mount Sinai.
Appendix 1
Grading scale used by raters
The rater scored subjects in real time. These scores were broken down into three broad categories (preparation, induction process, and post-induction management). Within each category, a number of specific questions were asked, and an overall global rating was given for each category. Finally, a global overall rating was obtained from the rater.
On a scale of 1–5 (1=completely inappropriate and 5=completely appropriate), our rater was asked to grade the following:
Preparation
Presence of self-inflating manual ventilator bag
Adequacy of oxygen source via wall or tank
Presence of working laryngoscope
Presence of appropriately sized and prepared tracheal tube
Presence of suction
Application of appropriate monitors
Ascertainment of appropriately focused history and physical examination
Induction
Choice of induction agents
Appropriate sequence of induction and delegation of relevant tasks
Post-induction
Appropriateness of intubation technique
Confirmation of tracheal intubation with capnography and auscultation
Timely recognition of relevant complication
Appropriateness of corrective measures taken
On a scale of 1–10 (1=worst performance, 5=average performance, 10=exemplary performance), the rater was asked to evaluate a global assessment of preparation, induction, and post-induction performance. Additionally, the rater was asked to grade overall performance on the same scale.
Additionally, where appropriate the rater was asked to determine in their estimation whether the subject recognized the intended complication. If they indicated recognition, they were asked to review footage and measure the time from laryngoscopy to recognition of the complication.
Appendix II
Description of standardized scenarios
Residents were faced with three scenarios at prespecified intervals in order to assess their ability to perform the necessary tasks safely. Available equipment included a standard group of induction agents, neuromuscular blocking drugs, vasoactive agents, laryngoscopes and handles of various sizes, non-rebreather masks and nasal cannulae, suction tubing and various suction catheters, various sizes of tracheal tubes and stylets, self-inflating manual resuscitating devices, an intubating bougie, and end-tidal CO2 detectors (Easy-Cap CO2 Detector; Covidien, Dublin, Ireland) for confirming tracheal intubation. Video laryngoscopy, fibreoptic bronchoscopy, or surgical airway equipment were not made available to participants.
In Scenario 1, they encountered a patient in a standard hospital ward setting. Participants were called to intubate a 74-yr-old male with a longstanding smoking history who presented with an exacerbation of chronic obstructive pulmonary disease and subsequently required intubation after failing a trial of non-invasive PPV. The scenario ended with confirmation of end-tidal CO2 with PPV by a confirmatory device attached to the end of the tracheal tube. This scenario was intended as a control in order to assess baseline performance.
In Scenario 2, subjects encountered a 58-yr-old female who suffered a stroke and required intubation because of an aspiration event from pharyngeal dysfunction. This intubation was made more difficult by activating the tongue swelling feature of our human patient simulator (HPS; CAE, Gainesville, FL, USA). Upon insertion of the laryngoscope blade into the mouth, the patient became asystolic until withdrawal of the blade from the mouth, mimicking an intense vagal response from laryngoscopy. The scenario ended either after physician recognition of cardiac arrest or the fifth positive pressure breath, whichever came first.
Scenario 3, encountered 6–12 weeks after Scenarios 1 and 2, was a 47-yr-old male with end-stage liver disease who was admitted to the ICU with an upper gastrointestinal bleed and was haemodynamically unstable upon arrival of the anaesthesia team. The scenario was designed to go smoothly throughout the laryngoscopy, but the patient would become pulseless at initiation of PPV. The simulation ended after either physician recognition of cardiac arrest or the fifth positive pressure breath, whichever came first.
References
- 1.Jaber S, Amraoui J, Lefrant JY et al. . Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med 2006; 34: 2355–61 [DOI] [PubMed] [Google Scholar]
- 2.Benedetto WJ, Hess DR, Gettings E et al. . Urgent tracheal intubation in general hospital units: an observational study. J Clin Anesth 2007; 19: 20–4 [DOI] [PubMed] [Google Scholar]
- 3.Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology 2011; 114: 42–8 [DOI] [PubMed] [Google Scholar]
- 4.Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the difficult airway: a closed claims analysis. Anesthesiology 2005; 103: 33–9 [DOI] [PubMed] [Google Scholar]
- 5.Schmidt UH, Kumwilaisak K, Bittner E, George E, Hess D. Effects of supervision by attending anesthesiologists on complications of emergency tracheal intubation. Anesthesiology 2008; 109: 973–7 [DOI] [PubMed] [Google Scholar]
- 6.Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology 1995; 82: 367–76 [DOI] [PubMed] [Google Scholar]
- 7.Weller JM, Merry AF, Robinson BJ, Warman GR, Janssen A. The impact of trained assistance on error rates in anaesthesia: a simulation-based randomised controlled trial. Anaesthesia 2009; 64: 126–30 [DOI] [PubMed] [Google Scholar]
- 8.Mhyre J, Martin LD, Ramachandran SK, Kheterpal S. Is faculty presence during emergent tracheal intubations justified? Anesthesiology 2009; 111: 217–8 [DOI] [PubMed] [Google Scholar]
- 9.Lemieux-Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature. Med Care Res Rev 2006; 63: 263–300 [DOI] [PubMed] [Google Scholar]
- 10.Griesdale DE, Bosma TL, Kurth T, Isac G, Chittock DR. Complications of endotracheal intubation in the critically ill. Intensive Care Med 2008; 34: 1835–42 [DOI] [PubMed] [Google Scholar]
- 11.Mark LJ, Herzer KR, Cover R et al. . Difficult airway response team: a novel quality improvement program for managing hospital-wide airway emergencies. Anesth Analg 2015; 121: 127–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Long L, Vanderhoff B, Smyke N, Shaffer LE, Solomon J, Steuer JD. Management of difficult airways using a hospital-wide ‘Alpha Team’ approach. Am J Med Qual 2010; 25: 297–304 [DOI] [PubMed] [Google Scholar]
- 13.Bhanji F, Mancini ME, Sinz E et al. . Part 16: education, implementation, and teams: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S920–33 [DOI] [PubMed] [Google Scholar]
- 14.Winters BD, Weaver SJ, Pfoh ER, Yang T, Pham JC, Dy SM. Rapid-response systems as a patient safety strategy: a systematic review. Ann Intern Med 2013; 158: 417–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis DP, Aguilar SA, Graham PG et al. . A novel configuration of a traditional rapid response team decreases non-intensive care unit arrests and overall hospital mortality. J Hosp Med 2015; 10: 3–52 [DOI] [PubMed] [Google Scholar]
- 16.Reznick RK, MacRae H. Teaching surgical skills—changes in the wind. N Engl J Med 2006; 355: 2664–9 [DOI] [PubMed] [Google Scholar]
- 17.Tamblyn R, Abrahamowicz M, Dauphinee D et al. . Physician scores on a national clinical skills examination as predictors of complaints to medical regulatory authorities. JAMA 2007; 298: 993–1001 [DOI] [PubMed] [Google Scholar]
- 18.Stefanidis D, Korndorffer JR, Markley S, Sierra R, Scott DJ. Proficiency maintenance: impact of ongoing simulator training on laparoscopic skill retention. J Am Coll Surg 2006; 202: 599–603 [DOI] [PubMed] [Google Scholar]
- 19.Wayne DB, Siddall VJ, Butter J et al. . A longitudinal study of internal medicine residents' retention of advanced cardiac life support skills. Acad Med 2006; 81: S9–S12 [DOI] [PubMed] [Google Scholar]
- 20.Berden HJJM, Willems FF, Hendrick JMA, Pijls NHJ, Knape JTA. How frequently should basic cardiopulmonary resuscitation training be repeated to maintain adequate skills? Br Med J 1993; 306: 1576–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kovacs G, Bullock G, Ackroyd-Stolarz S, Cain E, Petrie D. A randomized controlled trial on the effect of educational interventions in promoting airway management skill maintenance. Ann Emerg Med 2000; 36: 301–9 [DOI] [PubMed] [Google Scholar]
- 22.Kuduvalli PM, Jervis A, Tighe SQM, Robin NM. Unanticipated difficult airway management in anaesthetized patients: a prospective study of the effect of mannequin training on management strategies and skill retention. Anaesthesia 2008; 63: 364–9 [DOI] [PubMed] [Google Scholar]
- 23.Gomez CR. Editorial: time is brain! J Stroke Cerebrovasc Dis 1993; 3: 1–2 [DOI] [PubMed] [Google Scholar]
- 24.Lee TH. Effective reperfusion for acute myocardial infarction begins with effective health policy. Ann Intern Med 1997; 126: 652–3 [DOI] [PubMed] [Google Scholar]
- 25.Zwillich CW, Pierson DJ, Creagh CE, Sutton FD, Schatz E, Petty TL. Complications of assisted ventilation. A prospective study of 354 consecutive episodes. Am J Med 1974; 57: 161–70 [DOI] [PubMed] [Google Scholar]


