Abstract
Background
The aim of the study was to determine whether the introduction of a paediatric anaesthesia comic information leaflet reduced preoperative anxiety levels of children undergoing major surgery. Secondary objectives were to determine whether the level of understanding of participants and other risk factors influence STAIC-S (State–Trait Anxiety Inventory for Children—State subscale) score in children.
Methods
We performed a randomized controlled parallel-group trial comparing preoperative anxiety between two groups of children aged >6 and <17 yr. Before surgery, the intervention group received a comic information leaflet at home in addition to routine information given by the anaesthetist at least 1 day before surgery. The control group received the routine information only. The outcome measure was the difference between STAIC-S scores measured before any intervention and after the anaesthetist's visit. A multiple regression analysis was performed to explore the influence of the level of education, the anxiety of parents, and the childrens' intelligence quotient on STAIC-S scores.
Results
One hundred and fifteen children were randomized between April 2009 and April 2013. An intention-to-treat analysis on data from 111 patients showed a significant reduction (P=0.002) in STAIC-S in the intervention group (n=54, mean=−2.2) compared with the control group (n=57, mean=0.90). The multiple regression analysis did not show any influence on STAIC-S scores of the level of education, parental anxiety, or the intelligence quotient of the children.
Conclusions
A paediatric anaesthesia comic information leaflet was a cheap and effective means of reducing preoperative anxiety, measured by STAIC-S, in children.
Clinical trials registration
Keywords: anaesthesia, anxiety, child, randomized controlled trial, surgery
Editor's key points.
Many children about to undergo anaesthesia for major surgery suffer from considerable anxiety.
The prospect of anaesthesia itself is considered to be anxiety provoking.
The authors have developed a cartoon-based anaesthetic information leaflet for children.
The current study investigated the influence of use of this leaflet on preoperative anxiety.
Approximately 50–75% of children undergoing surgery develop preoperative anxiety. The currently accepted pathophysiological model postulates that anxiety attributable to stress increases the concentrations of cortisol and epinephrine and the cytotoxic activity of certain cells.1,2 Stress could also lead to fear, anxiety, cold, and infection. A major component of the preoperative stress response seems to be increased production of corticotrophin-releasing hormone and autonomous nervous system peripheral effectors, particularly of the hypothalamic–pituitary–adrenal axis.2,3 The level of anxiety has been shown to be related to postoperative disorders such as unrest, enuresis, eating disorders, apathy, solitary confinement, and sleep disorders. These complications can persist up to 6 months after intervention.4,5 Furthermore, preoperative anxiety correlates with poor clinical recovery.1,6 As a consequence, the treatment of preoperative anxiety in children is a priority for anaesthetists.7
Many studies have evaluated the anxiety of parents or children before a routine surgery.8–22 Two descriptive studies21,23 have measured the anxiety level of 100 parents before the routine operation of children using the ‘Leeds Anxiety and Depression Scale’,24 a scale used usually in the assessment of psychiatric pathologies. The patients were chosen from a predetermined list depending on the source of their anxiety and the factors that might possibly reduce it. The results of these two studies were similar and have highlighted that 42–47% of parents have a level of anxiety similar to that of adults with anxiety disorders. Anaesthesia has been cited as the anxiety-provoking element. The presence of parents during induction, the accompaniment of their child up to the operating room, and the formulation of a more detailed explanation by the doctor or the nurses of the surgical risk were cited as elements that can reduce their anxiety. However, the limitations of these two studies are that they are descriptive, made only with the parents, and they show only that the anaesthesia care of the child is, in itself, a factor provoking anxiety apart from the surgical procedure.
In France, the preoperative anaesthesia visit is mandatory before surgery. The visit should take place ‘a few days’ before surgery, which is usually interpreted to mean at least 2 days before surgery. No items in the guideline for the preoperative visit address how it should be organized specifically and what should be communicated to children or their parents. It is, however, generally accepted that the presence of parents is mandatory during the interview. Three types of interventions have been described to reduce preoperative anxiety: sedative premedication, presence of parents, and training programmes for participants and their parents. Few studies have explored whether the information provided to participants or the level of understanding of the information delivered is related to the parent's anxiety.19–25 To our knowledge, no study has explored the relationship between the information delivered before anaesthesia, the level of understanding of children, and their level of anxiety.
Methods
Trial design
This was a multicentre, open-label, parallel-group randomized trial conducted in Lyon, France (three sites).
Participants
Patients between 6 and 17 yr of age, who were to undergo surgery and who presented a high, normal, or low level of verbal comprehension (normal academic level or not being held back a year), were eligible. In our study, children were selected after the surgeon had confirmed the surgical indication. The information sheets (one for parents and one for the child suitable for his or her age) were sent by post to the family of the child. The information leaflet contained the study information and clearly specified the right to decline involvement in the study. A week after posting the information leaflet (the time allowed for reflection), the parents were contacted by telephone by the lead psychologist; the study was proposed again and explained. During this interval, the administrative information was also collected. Children were also asked about the school class they attended. If the child was not in the class equivalent to his or her age or if he or she had repeated a school year twice or more, then the pre-inclusion process was stopped. Before any intervention, the general anxiety score of the child was measured using the State–Trait Anxiety Inventory for Children—State subscale (STAIC-S). The time provided for this questionnaire was 10–15 min maximum; thereafter, if no disagreement was expressed by the parents (or holders of parental authority) then the randomization procedure was performed to determine the group allocation of the child. The intervention group received detailed information standardized with the comic illustration, whereas the control group received only routine information. The information sheets were dispatched by post to the study participants before the pre-anaesthetic visit, and a note (detailed information standardized with the comic illustration) was mentioned only for the intervention group.
The level of understanding of children was also evaluated and was verified by their performance on three items of the Wechsler Intelligence Scale for Children-4th edition (WISC-IV: similarity, vocabulary, and understanding) and the anxiety level as a function of level of understanding, the anxiety level adjusted on the State–Trait Anxiety Inventory for Children—Trait subscale (STAIC-T).
Patients whose illness created a major delay in verbal comprehension (score <70) were excluded from the study. As a result of this low score, the children would be expected to have difficulty with group discussions, auditory memory, reasoning aloud, reading, writing and expressing their ideas, and multistep directions; therefore, it was expected that these children would not be able to understand the comic illustration themselves and should be excluded from the study. However, the randomization reduced confounding by equalizing so-called factors (independent variables) that had not been accounted for in the experimental design.
Interventions
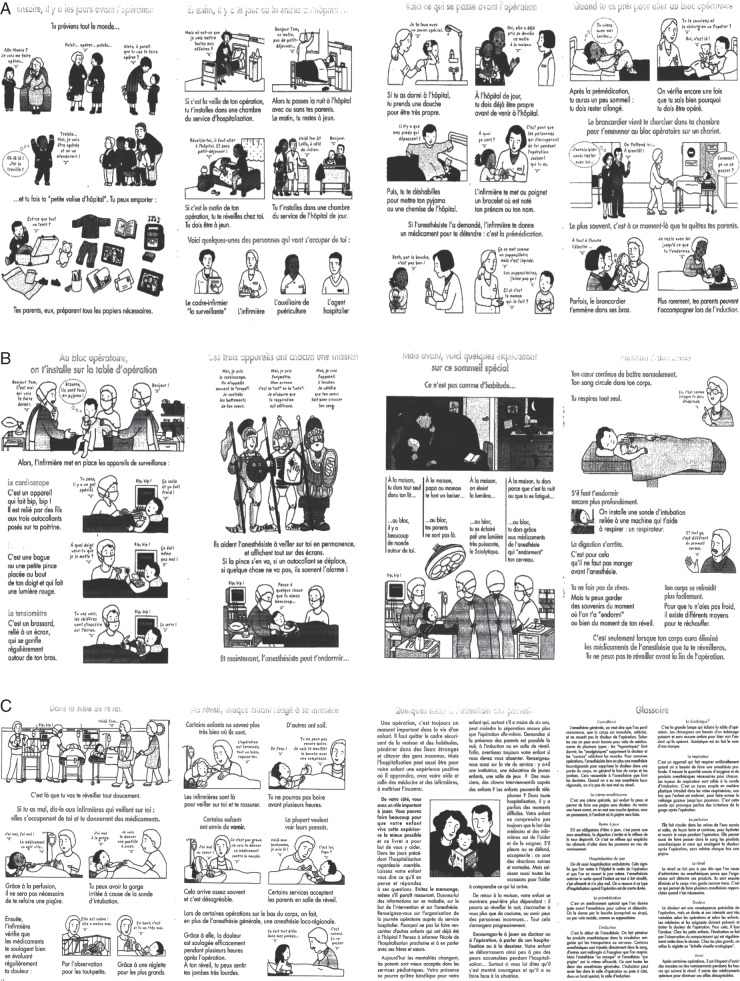
After central randomization, participants were assigned to either the intervention group or the control group. The control group received verbal information, as usually given by the anaesthetist during the pre-anaesthesia consultation, on fasting, hospitalization, surgical procedures, risks of anaesthesia, pain management after surgery, risks of transfusion. The intervention group received similar oral information in addition to the written information provided by the comic information leaflet sent to their home a few days before hospitalization. The comic information leaflet contained 20 pages, and each step was accompanied by a short text and a few illustrations. At the end of the booklet was a page written for the parents and a glossary (Fig. 1 a–c).
Fig 1.
(a–c) Snapshots of comic leaflet.
Outcomes
The primary outcome was the change in anxiety level, measured by STAIC-S, between the first evaluation carried out before any intervention and the evaluation carried out after the pre-anaesthetic visit. A secondary outcome was the difference between the level of anxiety at the first evaluation and at the evaluation carried out on the day of hospitalization, the night before the surgery, or the same day as the planned surgery. The STAIC-S has been validated in children older than 6 yr and is widely used to measure anxiety in children,26 the Cronbach α for state anxiety was high (i.e. 0.87 and 0.82 for girls and boys, respectively); for trait anxiety, it was 0.81 and 0.78, respectively. The correlation of the test–retest 8 weeks after was moderate 0.46–0.61.26
In the present study, STAIC was used instead of modified Yale preoperative anxiety scale, because its French version has been validated.27 We also assessed the correlation between parental and childrens' anxiety with the same tool. Finally, STAIC allows the measurement of trait anxiety of children apart from the perioperative anxiety. The STAIC questionnaires were administered by two child psychologists who were not blinded to the allocation group. Two questionnaires, including 7 and 16 questions, were used to assess childrens' and parents' evaluation of the leaflet and the information given during the pre-anaesthetic visit.28
Sample size determination
A total of 110 participants, with 55 participants in each group, would be required in order to show a difference of 1 point between groups on the evolution of the STAIC-S scale considering the α risk of 0.05, 90% power, and an sd of the difference of 1.6.
Randomization
Randomization was performed by a computer-generated random number list prepared by the department of biostatistics of the coordination centre, which had no clinical involvement in the trial. The random list was created using R statistical software, with a 1:1 allocation using a block size of 5. After obtaining the patient's consent to participate, a neuropsychologist at the coordination centre allocated participants to the intervention or control group by unmasking one line at each randomization on the list.
Statistical analysis
Statistical analysis was performed using R software. The evolution of the STAIC-S score between the first evaluation and the evaluation carried out after the pre-anaesthetic visit was compared between the two groups using the Mann–Whitney U-test. The proportion of patients with a score <34 after the pre-anaesthetic visit was calculated and compared between the two groups using Fisher's exact test. The threshold of 34 has been shown to have a sensitivity of 0.73 and a specificity of 0.70.26 The differences between the first evaluation and the one carried out on the day of hospitalization were also measured. The α risk of 5% was used as the statistical significance level for all the comparisons.
In order to adjust on the risk factors of anxiety in children, a multiple linear regression was performed on the primary outcome measures. The tested intervention, the Verbal Comprehension Index, the level of parental anxiety, and the educational level of the mother were independent variables. The level of parental anxiety was measured by the mother's STAIC score. If the mother's score was missing, then the father's STAIC score was used.
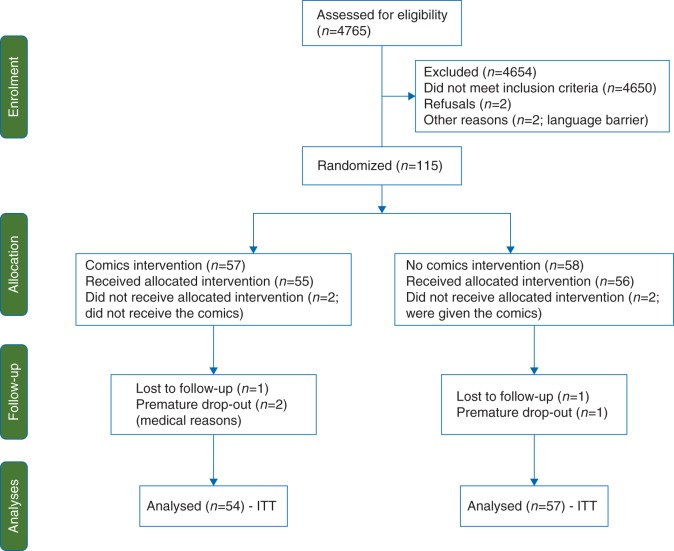
Results
The flow diagram of patients is presented in Fig. 2. Between April 2009 and April 2013, 115 patients, 58 in the control group and 57 in the intervention group, were enrolled through three units. Four patients did not receive the allocated treatment (3.4%). One hundred and eleven participants (93.0%) completed the study, three (2.6%) discontinued the intervention, and one (0.9%) was lost during the follow-up. The primary analysis was an intention-to-treat analysis and involved 111 patients. At inclusion, the mean STAIC-S score was not significantly different between the two groups (30.4 in the control group vs 32.1 in the intervention group, P=0.14; Table 1).
Fig 2.
Flow diagram of patients. ITT, intention to treat.
Table 1.
Participants' characteristics. STAIC-S, The State-Trait Anxiety Inventory for Children State form; STAIC-T, The State-Trait Anxiety Inventory for Children Trait form; STAI Y, The State-Trait Anxiety Inventory form Y (trait anxiety); WISC-IV, Wechsler Intelligence Scale for Children-4th edition
| Characteristic | Control (n=57) | Intervention (n=54) |
|---|---|---|
| Age [yr; mean (sd)] | 12.2 (3.1) | 12.6 (2.6) |
| Age range [yr; (minimum–maximum)] | 6.4–16.8 | 6.4–16.8 |
| Female [n (%)] | 30 (52.6) | 29 (53.7) |
| Male [n (%)] | 27 (47.4) | 25 (46.3) |
| Weight [kg; mean (sd)] | 57.29 (13.46) | 52.71 (12.69) |
| Height [cm; mean (sd)] | 164 (9) | 161 (11) |
| History of surgery, yes [n (%)] | 35 (61.4) | 31 (57.4) |
| STAIC-S [mean (sd)] | 30.4 (5.0) | 32.1 (5.1) |
| Neurosurgery | 32.2 (4.9) | 33.6 (5.2) |
| Orthopedic or visceral surgery | 29.3 (4.8) | 31.0 (4.7) |
| STAIC-T [mean (sd)] | 31.1 (7.5) | 31.4 (6.1) |
| STAI Y, mother [mean (sd, n)] | 42.9 (8.9, n=54) | 41.1 (7.2, n=48) |
| STAI Y, father [mean (sd, n)] | 40.2 (7.1, n=10) | 38.5 (7.1, n=16) |
| Verbal Comprehension Index WISC-IV | 101.4 (14.4, n=56) | 104.5 (12.3) |
| Vocabulary [mean (sd, n)] | 10.0 (2.7, n=56) | 10.6 (2.5) |
| Similarity [mean (sd, n)] | 10.6 (2.5, n=56) | 11.0 (2.3) |
| Comprehension [mean (sd, n)] | 10.3 (2.9, n=56) | 10.8 (2.1) |
| Highest diploma of the mother | ||
| Junior high [n (%)] | 19 (33.3) | 17 (31.5) |
| High school [n (%)] | 19 (33.3) | 13 (24.1) |
| University [n (%)] | 19 (33.3) | 24 (44.4) |
Interestingly, anxiety was higher at inclusion in one site, neurosurgery (median score 33), compared with the two other sites (median score 30). The assessment of the leaflet and the information received during the pre-anaesthetic visits by children and parents are shown in Tables 2 and 3. Of 50 patients, 45 (90%) found the received leaflet useful and 43 (86%) found it comforting. Among parents, 93.5% found it useful and 91.3% comforting. Generally, most of the parents read the leaflet (86.3% positive answers). Eighty-eight per cent of children (95 of 108) and 89% of parents (97 of 109) indicated they had been informed regarding general anaesthesia during the pre-anaesthetic visit. They found this visit useful (88.1% of children and 92.6% of parents) and reassuring (82.6% of children and 90.8% of parents).
Table 2.
Evaluation of the leaflet by children and parents in the intervention group. n, number of children or parents who answered yes to the question; N, total number of children or parents for whom the answer to the question was not missing
| Question | Children (N=54) | Parents (N=54) |
|---|---|---|
| Did you read the leaflet? [% (n/N)] | 96.0 (48/50) | 86.3 (44/51) |
| Did the leaflet comfort you? [% (n/N)] | 86.0 (43/50) | 91.3 (42/46) |
| Did the leaflet stress you out? [% (n/N)] | 8.0 (4/50) | 2.1 (1/47) |
| Did you find the leaflet too complicated? [% (n/N)] | 4.0 (2/50) | 2.2 (1/45) |
| Did you find the leaflet useful? [% (n/N)] | 90.0 (45/50) | 93.5 (43/46) |
| Did the leaflet give you information that you ignored? [% (n/N)] | 70.0 (35/50) | 34.8 (16/46) |
Table 3.
Evaluation of the pre-anaesthetic visit by children and parents. n, number of children or parents who answered yes to the question; N, total number of children or parents for whom the answer to the question was not missing
| Evaluation | Children | Parents |
|---|---|---|
| Duration of the pre-anaesthetic visit [min; mean (sd)] | 20.31 (9.44, N=108) | 21.15 (9.17, N=107) |
| Information received | ||
| Have you been informed on the risk of anaesthesia? [% (n/N)] | 56.5 (61/108) | 68.8 (75 /109) |
| Have you been informed on the pain and the means for pain management? [% (n/N)] | 85.2 (92/108) | 85.3 (93/109) |
| Have you been informed on the general anaesthesia? [% (n/N)] | 88.0 (95/108) | 89.0 (97/109) |
| Have you been informed on the risks of potential transfusion? [% (n/N)] | 16.0 (17/106) | 24.0 (24/100) |
| Comprehension of the information | ||
| Is there a risk with anaesthesia? [% (n/N)] | 35.2 (38 /108) | 77.4 (82/106) |
| Did you understand how your pain (of your children) will be handled? [% (n/N)] | 86.2 (94/109) | 86.4 (95/110) |
| Did you understand how you (your children) will be anaesthetized? [% (n/N)] | 99.1 (105/109) | 95.5 (105/110) |
| Have you been reassured by the consultation? [% (n/N)] | 82.6 (90/109) | 90.8 (99/109) |
| Quality of the visit | ||
| Was the consultation long enough? [% (n/N)] | 88.8 (95/107) | 94.5 (104/110) |
| Did you get an answer to your questions? [% (n/N)] | 85.2 (92/108) | 92.5 (99/107) |
| Did you find the consultation useful? [% (n/N)] | 88.1 (96/109) | 92.6 (100/108) |
| General questions on anaesthesia | ||
| Did you know that this visit is mandatory? [% (n/N)] | 43.1 (47 /109) | 93.6 (103/110) |
| Do you know who was the consultant? [% (n/N)] | 22.9 (25/109) | 65.1 (71/109) |
| Do you know that the doctor that you have seen is not always the same who is going to anaesthetize you? [% (n/N)] | 78.9 (86/109) | 94.5 (104/110) |
| Is it important to you to have the same doctor for anaesthesia? [% (n/N)] | 46.8 (51/109) | 50.0 (55/110) |
In the intervention group, mean STAIC-S score was decreased from 32.09 to 30.07 (−2.02, sd=4.23) between the first evaluation and the evaluation carried out after the pre-anaesthetic visit. On the contrary, in the control group the mean STAIC-S score increased from 30.40 to 31.30 between the two evaluations (0.90 points, sd=4.97). The difference of evolution of the STAIC-S score between the two groups was statistically significant (P=0.002). This difference persisted on the day of hospitalization, when the mean STAIC-S score increased by 0.39 (sd=4) in comparison to the first evaluation in the intervention group and by 5.14 (sd=6) in the control group (P<0.001). When the STAIC-S score threshold of 34 was considered, the proportion of children below 34 was significantly higher in the intervention group (48 of 54=88.9%) compared with the control group (39 of 57=68.4%, P=0.011). In the multiple linear regression analysis of the STAIC-T score between the first and the second evaluation, 110 patients were included. After adjustment of the potential confusion factors, the difference in the evolution of the STAIC-T score between the two groups persisted. The adjusted difference of the mean evolution was estimated at −2.9 in favour of the intervention group (P=0.002; Table 4).
Table 4.
Results of the multiple linear regression analysis on the influence of aggravating factors on the benefit of the leaflet on anxiety. Pr (>|t|), Probability that the mean score of anxiety state of children (STAIC-S) has been influenced by the factors
| Estimate | se | t value | Pr (>|t|) | |
|---|---|---|---|---|
| Intercept | 0.58 | 1.28 | 0.45 | 0.65 |
| Intervention group (intervention vs control) | −2.90 | 0.90 | −3.21 | 0.002 |
| Verbal Comprehension Index WISC-IV |
−0.03 | 0.04 | −0.85 | 0.40 |
| Parental anxiety (STAIC) | −0.03 | 0.06 | −0.48 | 0.63 |
| Children trait anxiety (STAIC-T) | 0.08 | 0.07 | 1.16 | 0.25 |
| Highest diploma of the mother (for an increase of one unit of the diploma) | 0.15 | 0.55 | 0.27 | 0.79 |
Discussion
To our knowledge, this is the first randomized controlled trial evaluating the influence of prehospital-based information, given by means of a comic leaflet to children, on the level of understanding of children and their level of anxiety.
The study aimed to evaluate the reduction in preoperative anxiety through a simple leaflet developed by paediatricians and paediatric anaesthetists, delivered at home before the pre-anaesthetic visit. Our results show that children aged >6 and <17 yr, who had received an educational comic leaflet at home up to 1 week before surgery, had a lower mean STAIC-S score after pre-anaesthetic visits. This benefit seemed to persist until the day of hospitalization. The multiple linear regression analysis did not specify any modification in this benefit in relation to the Verbal Comprehension Index, or the level of parents' and children's trait anxiety.
Randomized controlled trials published so far on the preoperative preparation of children have mainly focused on parental anxiety.9,10,19 Family-centred and psychological preoperative interventions have been shown to be effective in reducing preoperative anxiety measured by mYPAS in children.12
In the study by Kain and colleagues,12 children aged 2–10 yr and their parents were randomly assigned to one of four groups: (i) control, who received standard care; (ii) parental presence, who received standard parental presence during induction of anaesthesia; (iii) ADVANCE, who received family-centred behavioural preparation; and (iv) oral midazolam. The authors assessed the effect of group assignment on preoperative anxiety levels and postoperative outcomes such as analgesic consumption and emergence delirium.12 The primary objective was the anxiety of the children according to the mYPAS scale, and the secondary objective was the parental anxiety assessed using the State–Trait Anxiety Inventory (STAI). The group ADVANCE had scores of mYPAS and STAI that were significantly lower than in the other three groups. However, because the ADVANCE programme consists of a number of components, it is unclear which of the components are essential. Also this type of programme is difficult to implement widely.29,30
Cohort studies suggest that the anxiety of children <3 yr old could be increased by preparation (visual analog scale=46±17 vs 25±14, P=0.001),4 whereas in children >6 yr old the preparation is more effective when delivered 1 week before surgery.4 This corroborates the result of a recent inconclusive randomized controlled trial on the preoperative education delivered on the day of surgery for reducing the anxiety in children during i.v. induction of anaesthesia.
In a recent publication in the Cochrane Database of Systematic Reviews, it was stated that the presence of parents during induction of general anaesthesia does not diminish their child's anxiety.31 The authors also proposed that potentially promising non-pharmacological interventions, such as parental acupuncture, clowns or clown doctors, playing videos of the child's choice during induction, low sensory stimulation, and hand-held video games need further investigation in larger studies.31
The blinding of participants and investigators was not possible in our study because of the type of intervention. We were also not able to organize blinding of outcome assessment by two different assessors because of lack of funds. As a result, our study could suffer from differential measurement errors. However, the multiple linear regression analysis suggests that children enrolled at the neurosurgery centre, who had a higher STAIC score at baseline, benefited more (STAIC score reduction of −4.65) than those at other centres (−1.5; P-value for interaction between group of randomization and centres=0.08). Subgroup analyses did not show an influence of age, a history of surgery, or chronic disease on the STAIC score.
Conclusion
We believe that information on anaesthesia and surgery procedures given in a comic leaflet to children is worth implementation before surgery because it is cheap and seems effective in reducing preoperative anxiety measured by STAIC.
Authors' contributions
All the authors contributed to the conception of this project and to the analysis and interpretation of the results. They were all involved in critically revising the manuscript for important intellectual content and they have all approved this final version.
Writing the protocol, supervision of the methods, performance of the trial analyses, and editing the article: B.K., E.P.S.N., M.R., E.D., S.M., T.G.
Enrolment of participants: E.P.S.N., S.G., D.C., N.T.
Psychological evaluation (anxiety scale and comprehension evaluation): O.R.
Declaration of interest
None declared.
Funding
French Ministry of Health, Programme Hospitalier de Recherche Clinique Régional, and Programme de Recherche en Qualité Hospitalière in 2008 (no. 27-39).
Acknowledgements
We are grateful to Mathilde Vernet, Carla Giugno, Carmine Mottolese, Rémi Kohler, and Pierre Mouriquand for their assistance in recruiting participants. The comic leaflets were developed and graciously offered by SPARADRAP, an association that guides children regarding their health issues.
References
- 1.Kain ZN, Sevarino F, Alexander GM, Pincus S, Mayes LC.. Preoperative anxiety and postoperative pain in women undergoing hysterectomy. A repeated-measures design. J Psychosom Res 2000; 49: 417–22 [DOI] [PubMed] [Google Scholar]
- 2.Chrousos GP, Gold PW. The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA 1992; 267: 1244–52 [PubMed] [Google Scholar]
- 3.Ader R, Cohen N, Felten D. Psychoneuroimmunology: interactions between the nervous system and the immune system. Lancet 1995; 345: 99–103 [DOI] [PubMed] [Google Scholar]
- 4.Kain ZN, Mayes LC, O'Connor TZ, Cicchetti DV.. Preoperative anxiety in children. Predictors and outcomes. Arch Pediatr Adolesc Med 1996; 150: 1238–45 [DOI] [PubMed] [Google Scholar]
- 5.Kain ZN, Caldwell-Andrews AA, Maranets I et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg 2004; 99: 1648–54 [DOI] [PubMed] [Google Scholar]
- 6.Kiecolt-Glaser JK, Page GG, Marucha PT, MacCallum RC, Glaser R.. Psychological influences on surgical recovery. Perspectives from psychoneuroimmunology. Am Psychol 1998; 53: 1209–18 [DOI] [PubMed] [Google Scholar]
- 7.Macario A, Weinger M, Truong P, Lee M.. Which clinical anesthesia outcomes are both common and important to avoid? The perspective of a panel of expert anesthesiologists. Anesth Analg 1999; 88: 1085–91 [DOI] [PubMed] [Google Scholar]
- 8.Bellew M, Atkinson KR, Dixon G, Yates A.. The introduction of a paediatric anaesthesia information leaflet: an audit of its impact on parental anxiety and satisfaction. Paediatr Anaesth 2002; 12: 124–30 [DOI] [PubMed] [Google Scholar]
- 9.Cassady JF Jr, Wysocki TT, Miller KM, Cancel DD, Izenberg N.. Use of a preanesthetic video for facilitation of parental education and anxiolysis before pediatric ambulatory surgery. Anesth Analg 1999; 88: 246–50 [DOI] [PubMed] [Google Scholar]
- 10.Felder-Puig R, Maksys A, Noestlinger C et al. Using a children's book to prepare children and parents for elective ENT surgery: results of a randomized clinical trial. Int J Pediatr Otorhinolaryngol 2003; 67: 35–41 [DOI] [PubMed] [Google Scholar]
- 11.Hatava P, Olsson GL, Lagerkranser M. Preoperative psychological preparation for children undergoing ENT operations: a comparison of two methods. Paediatr Anaesth 2000; 10: 477–86 [DOI] [PubMed] [Google Scholar]
- 12.Kain ZN, Caldwell-Andrews AA, Mayes LC et al. Family-centered preparation for surgery improves perioperative outcomes in children: a randomized controlled trial. Anesthesiology 2007; 106: 65–74 [DOI] [PubMed] [Google Scholar]
- 13.Kain ZN, Caramico LA, Mayes LC, Genevro JL, Bornstein MH, Hofstadter MB.. Preoperative preparation programs in children: a comparative examination. Anesth Analg 1998; 87: 1249–55 [DOI] [PubMed] [Google Scholar]
- 14.Kain ZN, Mayes LC, Caramico LA. Preoperative preparation in children: a cross-sectional study. J Clin Anesth 1996; 8: 508–14 [DOI] [PubMed] [Google Scholar]
- 15.Kain ZN, Mayes LC, Caramico LA et al. Parental presence during induction of anesthesia. A randomized controlled trial. Anesthesiology 1996; 84: 1060–7 [DOI] [PubMed] [Google Scholar]
- 16.Kain ZN, Mayes LC, Cicchetti DV, Bagnall AL, Finley JD, Hofstadter MB. The Yale Preoperative Anxiety Scale: how does it compare with a “gold standard”? Anesth Analg 1997; 85: 783–8 [DOI] [PubMed] [Google Scholar]
- 17.Kain ZN, Mayes LC, Wang SM, Caramico LA, Hofstadter MB.. Parental presence during induction of anesthesia versus sedative premedication: which intervention is more effective? Anesthesiology 1998; 89: 1147–56; discussion 9A–10A [DOI] [PubMed] [Google Scholar]
- 18.Kain ZN, Wang SM, Caramico LA, Hofstadter M, Mayes LC.. Parental desire for perioperative information and informed consent: a two-phase study. Anesth Analg 1997; 84: 299–306 [DOI] [PubMed] [Google Scholar]
- 19.Karl HW, Pauza KJ, Heyneman N, Tinker DE.. Preanesthetic preparation of pediatric outpatients: the role of a videotape for parents. J Clin Anesth 1990; 2: 172–7 [DOI] [PubMed] [Google Scholar]
- 20.Margolis JO, Ginsberg B, Dear GL, Ross AK, Goral JE, Bailey AG.. Paediatric preoperative teaching: effects at induction and postoperatively. Paediatr Anaesth 1998; 8: 17–23 [DOI] [PubMed] [Google Scholar]
- 21.Thompson N, Irwin MG, Gunawardene WM, Chan L. Pre-operative parental anxiety. Anaesthesia 1996; 51: 1008–12 [DOI] [PubMed] [Google Scholar]
- 22.Waisel DB, Truog RD. The benefits of the explanation of the risks of anesthesia in the day surgery patient. J Clin Anesth 1995; 7: 200–4 [DOI] [PubMed] [Google Scholar]
- 23.Shirley PJ, Thompson N, Kenward M, Johnston G. Parental anxiety before elective surgery in children. A British perspective. Anaesthesia 1998; 53: 956–9 [DOI] [PubMed] [Google Scholar]
- 24.Snaith RP, Bridge GW, Hamilton M. The Leeds scales for the self-assessment of anxiety and depression. Br J Psychiatry 1976; 128: 156–65 [DOI] [PubMed] [Google Scholar]
- 25.Orliaguet G. [Preoperative information for paediatric patients. The anaesthesiologist's point of view]. Ann Fr Anesth Reanim 2006; 25: 451–7 [DOI] [PubMed] [Google Scholar]
- 26.Vila G, Nollet-Cleménçon C, de Blic J, Falissard B, Mouren-Simeoni MC, Scheinmann P. Assessment of anxiety disorders in asthmatic children. Psychosomatics 1999; 40: 404–13 [DOI] [PubMed] [Google Scholar]
- 27.Turgeon L, Chartrand E. Reliability and validity of the Revised Children's Manifest Anxiety Scale in a French-Canadian sample. Psychol Assess 2003; 15: 378–83 [DOI] [PubMed] [Google Scholar]
- 28.Galeano A, Ferrandiere M, Blond MH et al. [Evaluation of the information given to parents during the planned preanaesthetic consultation in a paediatric hospital]. Ann Fr Anesth Reanim 2005; 24: 1334–42 [DOI] [PubMed] [Google Scholar]
- 29.Cuzzocrea F, Costa S, Gugliandolo MC, Larcan R. Psychologists in preoperative programmes for children undergoing surgery. J Child Health Care 2016; 20: 164–73 [DOI] [PubMed] [Google Scholar]
- 30.Fortier MA, Blount RL, Wang SM, Mayes LC, Kain ZN. Analysing a family-centred preoperative intervention programme: a dismantling approach. Br J Anaesth 2011; 106: 713–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manyande A, Cyna AM, Yip P, Chooi C, Middleton P. Non-pharmacological interventions for assisting the induction of anaesthesia in children. Cochrane Database Syst Rev 2015; 7: CD006447. [DOI] [PMC free article] [PubMed] [Google Scholar]