Abstract
Purpose: To evaluate LithoVue, the new single-use digital flexible ureteroscope, in a human cadaveric model and compare it with a nondisposable fiber optic and digital flexible ureteroscopes.
Materials and Methods: LithoVue, a conventional fiber optic, and digital flexible ureteroscopes were each tested in four renal units of recently deceased female cadavers by three surgeons. The following parameters were analyzed: accessibility to the kidney and navigation of the entire collecting system with and without ureteral access sheath (UAS), lower pole access measuring the deflection of the ureteroscope with the working channel empty, and with inside two different baskets and laser fibers. A subjective evaluation of maneuverability and visibility was assessed by each surgeon at the end of every procedure.
Results: Kidney access into the Renal unit 1 was not possible without UAS for all ureteroscopes because of noncompliant ureter at the level of sacroiliac joint. The reusable digital ureteroscope was unable to reach one calix of the lower pole and one calix of the upper pole (Renal units 2 and 3) without UAS placement. Lower pole access with baskets and laser fibers was possible for each ureteroscope after UAS placement. No statistically significant differences were detected in angle deflection between ureteroscopes. The digital ureteroscope was preferred for visibility in all procedures: LithoVue for maneuverability in six procedures, fiber optic in five procedures, and the digital ureteroscope in one procedure.
Conclusions: LithoVue seems to be comparable with conventional ureteroscopes in terms of visibility and manipulation into the collecting system in fresh human cadavers. Further studies in humans are needed to determine the clinical value of this new instrument.
Introduction
With the advancement of technology, flexible ureteroscopy (fURS) has become an attractive option for surgical management of kidney stones. Published by Ordon and coworkers, a population-based case series analysis of kidney stone treatment in Canada showed that from 1994 to 2010, fURS has become the most used surgical treatment modality, exceeding external shock wave lithotripsy by more than 30%.1 Flexible ureteroscopes have been used to access the upper urinary tract by Marshall in 1964,2 and in clinical practice they were promoted by Bagley and Rittenberg who first reported their preliminary outcomes of stones treated by means of these instruments.3 As a matter of fact, by the end of the 20th century, several publications demonstrated the advancement of the technique3,4 and fURS became popular worldwide. Currently, there is a variety of flexible ureteroscopes available, including fiber optic and digital ureteroscopes. Despite the technologic advancement of flexible ureteroscopes, durability remains a major concern.5 Due to the high cost and limited durability, the cost–benefit of these permanent, nondisposable ureteroscopes continues to be the most important factor for initiating and maintaining fURS programs worldwide, especially in developing countries.
LithoVue (Boston Scientific, Marlborough, MA) is the first disposable digital flexible ureteroscope developed to access the upper urinary tract. It claims to be cost-effective but there is sparse data regarding its performance, image quality, and accessibility to the entire collecting system.
The aim of this study was to evaluate LithoVue in a human cadaveric model and compare it with a nondisposable fiber optic and digital flexible ureteroscopes.
Materials and Methods
LithoVue, a conventional fiber optic flexible ureteroscope (URF-P5; Olympus, Tokyo, Japan), and digital (URF-V; Olympus) ureteroscope were each tested in four renal units (two right and two left) of recently deceased female cadavers by three surgeons (one senior, two junior). The cadavers were used according to all legal, public health, and ethical standards. All the characteristics of ureteroscopes used are reported in Table 1. The following parameters were analyzed: accessibility to the kidney and navigation of the entire collecting system with and without ureteral access sheath (UAS), lower pole access measuring the deflection of the ureteroscope with the working channel empty and with inside two different baskets (1.9F Zero-tip; 1.3F Optiflex—Boston Scientific), and laser fibers (AccuTrac 200 micron—Boston Scientific; standard laser fiber 272 micron—Rocamed, Monaco, MC). The ureteroscopes were used in the following sequence:
Table 1.
Characteristics of LithoVue, URF-P5, and URF-V
| Characteristics | LithoVue | URF-P5 | URF-V |
|---|---|---|---|
| Use | Single use | Reusable | Reusable |
| Optical system | Digital (CMOS) | Fiber optic | Digital (CCD) |
| Tip diameter | 7.7F | 5.3F | 8.5F |
| Shaft diameter | 9.5F | 8.4F | 9.9F |
| Working channel diameter | 3.6F | 3.6F | 3.6F |
| Deflection (up/down) | 270°/270° | 180°/275° | 180°/275° |
Renal unit 1: LithoVue; URF-V; URF-P5
Renal unit 2: URF-P5; LithoVue; URF-V
Renal unit 3: URF-V; URF-P5; LithoVue
Renal unit 4: LithoVue; URF-P5; URF-V
The purpose of modifying the sequence of the ureteroscopes for each renal unit was to avoid any influence on surgeons' perception by the first image seen with the same instrument. Each surgeon performed one trial per instrument for each renal unit.
A new LithoVue was used for each renal unit; it was connected to its specific monitor for viewing (Figs. 1 and 2). P5 and URF-V were not new ureteroscopes; their performance in terms of visibility and maneuverability was checked before every use in every renal unit.
FIG. 1.
LithoVue: single-use digital flexible ureteroscope.
FIG. 2.

LithoVue's monitor.
The visibility was assessed with a subjective assessment in terms of quality image. Similarly, the maneuverability was evaluated by means of a subjective perception on approachability of all targeted areas of the collecting system, both expressed by each surgeon as a preference at the end of every procedure.
Data are presented as mean and standard deviation. Between-groups comparisons were made using Kruskal–Wallis test. A p value <0.05 was considered significant. Statistical analyses were performed using GraphPad Prism version 6.00 for Mac OS X, GraphPad Software.
Technique
The experiment started with a rigid cystoscopy. The ureteral orifice was identified and a hydrophilic guidewire under fluoroscopy was placed into the kidney as a safety wire to mimic the clinical scenario. Then, a second working wire was placed into the collecting system. Through this wire, the flexible ureteroscope was inserted into the urethra, bladder, then ureter all the way into the renal pelvis. Irrigation was performed with saline, using the gravity system. At this point, the working wire was removed. A retrograde pyelogram was performed using 20 cc of contrast as a guide. Then, the entire collecting system and all calices were navigated through a nephroscopy (Fig. 3). The duration of the nephroscopy was recorded. A wire was placed again into the collecting system through the working channel and left inside the kidney while the flexible ureteroscope was removed. Next, 12–14F by 36 cm UAS (Navigator HD; Boston Scientific) was placed through the wire under fluoroscopy guidance, with its tip located just below the ureteral–pelvic junction. Next, lower pole access was evaluated. A flexible ureteroscope was placed at the lower pole calix and fluoroscopy was recorded and saved for lower pole angle measurements. At the beginning of each procedure, no instruments were inserted into the working channel of the ureteroscopes. Two baskets and two laser fibers were inserted into the working channel of the ureteroscope and the lower pole deflection angle was measured again. The model of the flexible ureteroscope was changed and the procedure was started over again.
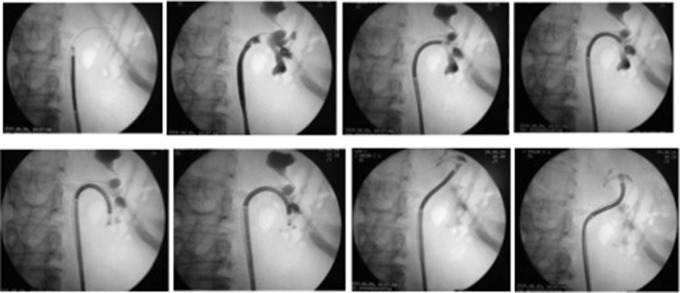
FIG. 3.
Navigation of the entire collecting system by LithoVue.
All fluoroscopic images were recorded and saved for evaluation.
Results
Kidney access into Renal unit 1 was not possible without UAS for all ureteroscopes because of noncompliant ureter at the level of sacroiliac joint. The reusable digital ureteroscope was unable to reach one calix of the lower pole (Renal unit 2) and one calix of the upper pole (Renal unit 3) without UAS placement, probably because of the large diameter of the ureteroscope and the reduced shaft rigidity. Lower pole access with baskets and laser fibers was possible for each ureteroscope after UAS placement (Table 2). No statistically significant differences were detected in angle deflection between ureteroscopes in all circumstances (p > 0.05) (Table 3). The digital ureteroscope was preferred for visibility in all procedures, LithoVue for maneuverability in six procedures, fiber optic in five procedures, and the digital ureteroscope in one procedure.
Table 2.
Kidney Access, Navigation of Collecting System, and Navigation Time by LithoVue, Fiber Optic, and Digital Reusable Ureteroscopes
| Ureteroscopes | |||
|---|---|---|---|
| Parameters | LithoVue | URF-P5 | URF-V |
| Kidney access (without/with UAS) | |||
| Renal unit 1 (L) | No/yes | No/yes | No/yes |
| Renal unit 2 (R) | Yes/yes | Yes/yes | Yes/yes |
| Renal unit 3 (L) | Yes/yes | Yes/yes | Yes/yes |
| Renal unit 4 (R) | Yes/yes | Yes/yes | Yes/yes |
| Navigation (without/with UAS) | |||
| Renal unit 1 (L) | Yes/yes | Yes/yes | Yes/yes |
| Renal unit 2 (R) | Yes/yes | Yes/yes | No (lower pole)/yes |
| Renal unit 3 (L) | Yes/yes | Yes/yes | No (upper pole)/yes |
| Renal unit 4 (R) | Yes/yes | Yes/yes | Yes/yes |
| Navigation time (minutes) (Surgeon 1/2/3) | |||
| Renal unit 1 (L) | 2.30/2.35/2.10 | 1.38/3.11/1.45 | 2.10/4.43/3.42 |
| Renal unit 2 (R) | 1.25/2.10/1.18 | 1.13/2.08/1.55 | 1.17/2.48/2.02 |
| Renal unit 3 (L) | 0.38/1.16/1 | 0.45/0.55/0.54 | 0.51/1.33/1.53 |
| Renal unit 4 (R) | 0.52/1.33/1.08 | 0.49/1.42/1.09 | 0.58/1.03/0.56 |
Bold text underlines every time an instrument was unable to reach a renal unit or a calix.
UAS = ureteral access sheath.
Table 3.
Lower Pole Angle Measurements
| LithoVue | URF-P5 | URF-V | p | |
|---|---|---|---|---|
| No UAS/working channel empty | 179 ± 12.7 | 179.5 ± 9.2 | 168.5 ± 0.7 | 0.33 |
| Yes UAS/working channel empty | 176.7 ± 5.9 | 178 ± 3.5 | 170 ± 4.1 | 0.21 |
| Optiflex | 175.3 ± 2.1 | 176.3 ± 2.1 | 168 ± 7.5 | 0.24 |
| Zero-tip | 173 ± 3.6 | 175 ± 2.6 | 167.3 ± 8.1 | 0.23 |
| Ball tip laser fiber | 174.7 ± 4.9 | 177.3 ± 2.9 | 168.3 ± 4.9 | 0.11 |
| Standard laser fiber | 174.3 ± 5.7 | 176.6 ± 3.2 | 167.3 ± 4.9 | 0.14 |
Discussion
Flexible ureteroscopes were first introduced by Marshall in 19642 and in clinical practice they were promoted by Bagley and Rittenberg, who first reported their preliminary outcomes of stones treated by means of these instruments.3 Since then, several advancements have occurred such as smaller ureteroscopes, greater deflection in both directions (ventral and dorsal), and digital technology. All these improvements have made fURS increasingly appealing for the management of renal stones, even in special and complicated circumstances.6
Several flexible ureteroscopes are available in the market, including fiber optic and digital ureteroscopes. The digital flexible ureteroscope has a “chip at the tip” technology that claims to provide better image quality than the conventional fiber optic flexible ureteroscope.7 Although the digital ureteroscopes have better image quality, both fiber optic and digital ureteroscopes can be used efficiently with comparable results. Somani and coworkers published a study comparing digital vs fiber optic ureteroscopes, and the results were similar in terms of accessibility to the entire collecting system and stone-free rates (SFRs). The only advantage of the digital ureteroscope in cases of stone treatment was the decreased operative time by 20%.8
Despite the technologic advancement that improved surgical performance, durability remains a major concern.
High cost of the ureteroscopes, maintenance, repair, and short life spans remain critical components for expanding the technique worldwide.5,9
Several authors have studied the durability of different instruments, reporting a wide range in the number of procedures performed before there was a need for repair, procedures varying from 5 to 113.5,10–12
Regardless of the manufacturer, the durability of the ureteroscope depends on the overall time of usage, location, size of the stone or tumor, use of other devices (UAS, laser fiber, and basket), surgeons' experience, and the sterilization method used. Furthermore, it has been demonstrated that brand-new flexible ureteroscopes are more resistant to damage than devices refurbished by original manufacturer and by outsourced vendors (mean of 44 usages vs 11.1 vs 6.9, respectively).13 Therefore, the cost of maintaining an older ureteroscope should be considered in addition to the overall cost of the equipment maintenance.
The sterilization process is an important factor when considering ureteroscope damage.
Abraham and coworkers studied two identical fiber optic ureteroscopes that underwent two different sterilization processes (Steris 1™ and Cidex OPA). They demonstrated that after 100 cycles, the first ureteroscope, which was sterilized in the Steris system, had a 12-mm tear on its shaft, 297 damaged fibers, and a 37% drop in resolution. The second ureteroscope, sterilized with Cidex, had no visible external damage and had only 10 damaged fibers.14 Finally, prevention of contamination and infection is pivotal and an efficient sterilization method is mandatory.
Therefore, a single-use flexible ureteroscope may be a cost-effective alternative to prevent problems related to transmission of pathogens.
The concept of disposable flexible ureteroscope is not new. In fact, some models have reached the market in the past, including Maxiflex and Polyscope. Maxiflex has a 180° bidirectional deflection and a working channel of 3.3F; no data were encountered in the literature regarding its performance. Polyscope is a semi-disposable flexible ureteroscope; it has a reusable fiber optical core and a disposable 8F outer sheath, featuring a 265° unidirectional active deflection with a 3.6F working channel. Even though the fiber optic core does not need to be sterilized between procedures, sterilization becomes necessary in cases of inadvertent contamination during surgery. Gu and coworkers reported a primary SFR of 89.5% in 86 patients with renal stones treated by Polyscope and holmium laser lithotripsy.15 In our experience (unpublished data), maneuverability and vision of the Polyscope were not good enough to perform a satisfactory procedure. LithoVue is the first digital single-use flexible ureteroscope in the market, with a 9.5F outer diameter and 7.9F on the tip; the working channel is 3.6F and the tip deflection in both directions is 270°. When comparing LithoVue with the other disposable flexible ureteroscopes available in the market, it embodies an important step forward.
In addition, all reusable ureteroscopes, once used after the first time, should be considered already “used” and potentially not at their top in terms of performance, but this is just one of the major advantages of a disposable flexible ureteroscope. Moreover, of course, to use every time a new reusable ureteroscope is not economically sustainable.
This study describes the initial experience in using LithoVue in a cadaveric model. Our results showed that LithoVue is comparable with the other ureteroscopes in terms of maneuverability, navigation of the entire collecting system, and angle of deflection in the lower pole with or without devices inside the working channel.
A good ureteroscope should have the following properties: good image quality, optimal maneuverability with full torque stability for easy access to the entire collecting system, adequate maximal deflection and irrigation flow when inserting a device into the working channel, and long durability.16
Based on our experiment, LithoVue seems to meet all the criteria for being a good ureteroscope with an additional advantage of disposability, eliminating the durability concerns. Further investigation regarding financial analysis and cost is necessary as LithoVue needs to also be financially viable when competing against reusable flexible ureteroscopes.
The concept of disposable ureteroscopes represents a breakthrough in the endourologic community. In fact, single-use instruments may provide a worldwide dissemination of fURS, including areas with limited possibilities for the acquisition and maintenance of endourologic armamentarium. In addition, in centers where fURS is already a standard procedure, disposable ureteroscopes may decrease overall cost. In conclusion, LithoVue has proved its efficacy in this study regarding maneuverability and visibility in cadaveric models. Clinical trials are needed to confirm the characteristics of this innovative disposable ureteroscope and to validate its cost-effectiveness.
Conclusion
LithoVue seems to be comparable with conventional ureteroscopes in terms of visibility and manipulation into the collecting system in fresh human cadavers. Further studies in humans are needed to determine the clinical value of this new instrument.
Abbreviations Used
- fURS
flexible ureteroscopy
- SFR
stone-free rate
- UAS
ureteral access sheath
Author Disclosure Statement
O. Traxer, G. Giusti, and W. Molina are consultants for Boston Scientific. For all other authors no competing financial interests exist.
References
- 1.Ordon M, Urbach D, Mamdani M, et al. A population based study of the changing demographics of patients undergoing definitive treatment for kidney stone disease. J Urol 2015;193:869–874 [DOI] [PubMed] [Google Scholar]
- 2.Marshall VF. Fiber optics in urology. J Urol 1964;91:110–114 [DOI] [PubMed] [Google Scholar]
- 3.Bagley DH, Rittenberg MH. Percutaneous antegrade flexible ureteroscopy. Urology 1986;27:331–334 [DOI] [PubMed] [Google Scholar]
- 4.Bagley DH. Ureteroscopic stone retrieval: Rigid versus flexible endoscopes. Semin Urol 1994;12:32–38 [PubMed] [Google Scholar]
- 5.Monga M, Best S, Venkatesh R, et al. Durability of flexible ureteroscopes: A randomized prospective study. J Urol 2006;176:137–141 [DOI] [PubMed] [Google Scholar]
- 6.Giusti G, Proietti S, Peschechera R, et al. Sky is no limit for ureteroscopy: Extending the indications and special circumstances. World J Urol 2015;33:257–273 [DOI] [PubMed] [Google Scholar]
- 7.Lusch A, Abdelshehid C, Hidas G, et al. In vitro and in vivo comparison of optics and performance of a distal sensor ureteroscope versus a standard fiberoptic ureteroscope. J Endourol 2013;27:896–902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Somani BK, Al-Qahtani SM, de Medina SD, et al. Outcomes of flexible ureterorenoscopy and laser fragmentation for renal stones: Comparison between digital and conventional ureteroscope. Urology 2013;82:1017–1019 [DOI] [PubMed] [Google Scholar]
- 9.Carey RI, Gomez CS, Maurici G, et al. Frequency of ureteroscope damage seen at a tertiary care center. J Urol 2006;176:607–610 [DOI] [PubMed] [Google Scholar]
- 10.Traxer O, Dusboq F, Jamali K, et al. New-generation flexible ureterorenoscopes are more durable than previous ones. Urology 2006;68:276–279 [DOI] [PubMed] [Google Scholar]
- 11.Defidio L, De Dominicis M, Di Gianfrancesco L, et al. Improving flexible ureteroscope durability up to 100 procedures. J Endourol 2012;26:1329–1334 [DOI] [PubMed] [Google Scholar]
- 12.Knudsen B, Miyaoka R, Shah K, et al. Durability of the next-generation flexible fiberoptic ureteroscopes: A randomized prospective multi-institutional clinical trial. Urology 2010;75:534–538 [DOI] [PubMed] [Google Scholar]
- 13.Carey RI, Martin CJ, Knego JR. Prospective evaluation of refurbished flexible ureteroscope durability seen in a large public tertiary care center with multiple surgeons. Urology 2014;84:42–45 [DOI] [PubMed] [Google Scholar]
- 14.Abraham JB, Abdelshehid CS, Lee HJ, et al. Effects of Steris 1 sterilization and Cidex high level disinfection on durability of new-generation flexible ureteroscopes. J Endourol 2007;21:985–992 [DOI] [PubMed] [Google Scholar]
- 15.Gu SP, Huang YT, You ZY, et al. Clinical effectiveness of the PolyScope™ endoscope system combined with holmium laser lithotripsy in the treatment of upper urinary calculi with a diameter of less than 2 cm. Exp Ther Med 2013;6:591–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Traxer O. Flexible ureterorenoscopic management of lower-pole stone: Does the scope make the difference? J Endourol 2008;22:1847–1850 [DOI] [PubMed] [Google Scholar]