Abstract
To find ‘missing’ tuberculosis (TB) cases, in November 2014 we trained private practitioners (PPs) and Ayurvedic practitioners (APs; Indian system of medicine) in Bilaspur district, India, to identify patients with presumptive TB and refer them to sputum microscopy centres. To reinforce this training, we sent weekly text message reminders during January–March 2015. All 50 APs and 23 of 29 PPs participated. The number of patients with presumptive TB referred by the PPs and APs increased from 38 (January–March 2014) to 104 (January–March 2015), and the number of smear-positive TB patients diagnosed increased from 5 to 16, a 220% increase. While the intervention increased the number of referrals, it did not impact case detection at district level, due to the short duration of the intervention and the non-dominant private sector.
Keywords: private practitioners, Indian system of medicine, India, operational research
Abstract
Dans le but de trouver des cas de tuberculose (TB) « manquants », nous avons formé des praticiens privés (PP) et des praticiens ayurvédiques (AP ; médecine indienne) du district de Bilaspur, Inde, en novembre 2014 afin d'identifier des patients avec une TB présumée et de les référer dans des centres de microscopie de crachats. Pour renforcer cette formation, nous avons envoyé des messages sous forme de texto chaque semaine comme aide-mémoire de janvier à mars 2015. Tous les 50 AP et 23 des 29 PP ont participé. Le nombre de patients présumés TB référés par les PP et AP a augmenté de 38 (janvier–mars 2014) à 104 (janvier–mars 2015) et le nombre de patients à frottis de TB positifs diagnostiqués a augmenté de 5 à 16 (augmentation de 220%). Si l'intervention a augmenté la référence de patients au laboratoire, elle n'a pas eu d'impact sur la détection des cas au niveau du district à cause de sa durée brève et du fait que le secteur privé n'est pas dominant dans la région.
Abstract
Con el propósito de detectar los casos de tuberculosis (TB) que ‘se pasan por alto’, se llevó a cabo una capacitación de los médicos del sector privado (PP) y los médicos del sistema Ayurveda (AP) de medicina tradicional de la India; la formación, realizada en el distrito de Bilaspur en noviembre del 2014, buscó mejorar el reconocimiento de los pacientes con presunción clínica de TB y su remisión a los centros de examen microscópico del esputo. Con el objeto de reforzar la capacitación, se enviaron mensajes recordatorios por SMS de enero a marzo del 2015. Participaron en el estudio todos los 50 AP y 23 de los 29 PP del distrito. El cociente del número de pacientes con presunción de TB remitidos por los PP y los AP de 38 (entre enero y marzo del 2014) a 104 (entre enero y marzo del 2015) y el número de casos diagnosticados de TB con baciloscopia positiva aumentó de cinco a 16 (incremento del 220%). Si bien la intervención aumentó el número de remisiones, la detección de casos a escala del distrito no se modificó, debido a la corta duración de la intervención y a que el sector privado no es predominante en este distrito.
Tuberculosis (TB) is a major public health problem with a global incidence of 9 million cases in 2013, of whom approximately 3 million were either not diagnosed, not treated, or not reported to national TB programmes.1 India accounts for about one third of these ‘missing’ millions.1 Identifying and treating these patients as early as possible is crucial to reducing transmission and ending the TB epidemic. A considerable number of existing medical care providers are not yet engaged in TB case detection. Overcoming this challenge will require innovative interventions to engage medical practitioners working outside the government sector, such as private practitioners (PPs) and health care providers in the traditional Indian medical system, known as Ayurvedic practitioners (APs), who are often the first—and preferred—point of contact for a substantial proportion of people with symptoms consistent with TB.2–5 While studies have shown that public-private partnerships can help increase case detection,6 the cost and time required to establish these partnerships can be prohibitive.7
Bilaspur (population ~400 000) is a predominantly rural, hilly district in the northern state of Himachal Pradesh, India. The services under the Revised National Tuberculosis Control Programme (RNTCP) are primarily delivered by the public health sector in the form of allopathic medicine. Eleven public health institutions and one private hospital in Bilaspur have facilities for sputum smear microscopy (Designated Microscopy Centres [DMC]). Health services in the district are also provided by 29 PPs and 50 APs through 69 Ayurvedic health centres. The PPs and APs had not been trained in TB diagnosis or the TB reporting requirements set out in the RNTCP guidelines. In Bilaspur, the annual new TB case notification rate is 74 per 1 million population and the contribution from the private sector is zero.8 While there had been some efforts to formally link PPs and APs with the RNTCP, the number of TB referrals from these doctors was low. This raised the concern that many TB cases cared for by these doctors were never reported.
To engage PPs and APs in TB control activities and improve TB case detection, we designed and implemented an intervention package. In this paper, we report on the change in the number of patients with presumptive TB referred and patients with smear-positive TB diagnosed by the PPs and APs before (January–March 2014) and after (January–March 2015) the intervention.
ASPECT OF INTEREST
All of the PPs and APs registered in Bilaspur were invited to participate in the study. Those who consented underwent a half-day training session in November 2014 to recognise the signs and symptoms of TB and refer patients with presumptive TB (cough ⩾2 weeks) to a DMC. A triplicate referral form was introduced: the first copy of the form was given to the patient, the second was used by RNTCP staff for documentation and for tracing referrals who did not reach the DMC for sputum smear microscopy, and the third was kept at the referring clinic. Each PP and AP was supplied with 20 sputum collection cups. Weekly reminders were sent to participants about the importance of referring cases with presumptive TB to a DMC. All referrals were documented in the laboratory register. Patients diagnosed with TB at the laboratory were referred back to the referring providers for initiation of treatment supplied free of charge by the RNTCP.
We calculated the difference in the number of patients with presumptive TB examined and smear-positive patients diagnosed by the PPs and APs before and after the intervention. For comparison, we did the same for allopathic medical practitioners working in the public sector. Data were extracted from the laboratory registers at the DMCs by RNTCP staff.
Ethics approval for the study was obtained from the Ethics Committees of the National Tuberculosis Institute, Bengaluru, India, and the International Union Against Tuberculosis and Lung Disease, Paris, France.
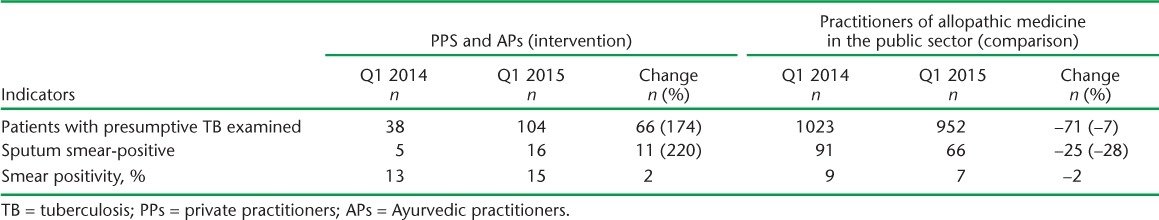
All 50 APs and 23/29 (79%) PPs who participated in the study referred a total of 104 patients with presumptive TB for sputum smear microscopy during January–March 2015. Of these, 16 (15%) were diagnosed as sputum smear-positive and initiated on treatment (Table 1). This represented an increase of 66 (174%) patients examined and 11 (220%) diagnosed with smear-positive TB during January–March 2014. At the same time, there was a 7% decrease in the number of patients with presumptive TB examined and a 28% decrease in the number found to be sputum smear-positive among those referred by public sector practitioners. The overall numbers in the district thus remained the same.
TABLE 1.
Change in numbers of patients with presumptive TB examined and diagnosed with smear-positive TB by PPs and APs and the comparison group before (January–March 2014) and after the intervention (January–March 2015) in Bilaspur, Himachal Pradesh, India
The costs incurred in training the PPs and APs and printing the referral forms were about 65 000 Indian rupees (approximately US$1000), and were drawn from existing programme budgets.
DISCUSSION
Following this brief intervention, we noted a substantial increase in the number of individuals with presumptive TB referred and patients with TB diagnosed by the PPs and APs. All of the APs and most of the PPs consented to participate, indicating the high acceptability of the intervention. Furthermore, the intervention was simple, efficient (requiring only half a day of training) and used existing programme resources, thus providing a feasible model for scale-up.
We need to be cautious of the limitations of this study, as the increased referrals by the PPs and APs did not impact the overall case notification in the district. Rather, a negative change was seen in the comparison group. While we are not aware of the exact reasons for this, we speculate that, first, the patient load in the private health sector and the APs may not be sufficient to make a major impact on the district-level case notification; in another district with a more dominant private health sector, the effects might be greater. Second, several of the public sector providers had been recruited recently, had not received any training in RNTCP guidelines and there was no active tracing of their referrals, which might be partially responsible for the negative change. Third, the apparent increase in notification and diagnosis by the PPs and APs may be a result of better documentation and attribution in the laboratory register. Fourth, while the intervention did not increase the overall numbers of cases, it might have affected the patient pathways involved in TB diagnosis. Patients who would eventually have been diagnosed by the public sector (in the no intervention scenario) might now have been detected on first contact with the PPs and APs, thus benefiting from earlier diagnosis and treatment initiation. We plan to monitor these cohorts for their treatment outcomes to examine if this was indeed the case. Furthermore, we need to continue this intervention to see if these short-term effects are sustained over time.
In conclusion, engaging PPs and APs led to an increase in the number of patients examined and patients diagnosed with TB by the PPs and APs. It did not, however, impact overall district-level case notification.
Acknowledgments
The authors would like to thank the staff of the TB Division, Office of Chief Officer, Bilaspur, the District Ayurvedic Officer and all the Ayurvedic medical officers and private practitioners of Bilaspur district, Himachal Pradesh, and the State and Central TB Division, India, for participating in and contributing to this study. They would also like to thank the National Health Mission, Himachal Pradesh, India, for funding this study.
The study was conducted as part of the TB Operations Research Training Programme and aimed to build operational research capacity within the Government of India's Revised National Tuberculosis Control Programme. This training programme was conceived and implemented jointly by the Central TB Division (Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, New Delhi), the National Tuberculosis Institute (Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, Bangalore), the World Health Organization (New Delhi, India Country Office), the International Union Against Tuberculosis and Lung Disease, South-East Asia Regional Office (New Delhi) and the Centers for Disease Control and Prevention Division of TB Elimination (Atlanta, GA, USA). The authors acknowledge the support of all the above. This study was funded by the National Health Mission, Himachal Pradesh, India. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: none declared.
References
- 1.World Health Organization. Global tuberculosis report 2014. Geneva, Switzerland: WHO; 2014. WHO/HTM/TB/2014. [Google Scholar]
- 2.Satyanarayana S, Nair S A, Chadha S S et al. From where are tuberculosis patients accessing treatment in India? Results from a cross-sectional community based survey of 30 districts. PLOS ONE. 2011;6:e24160. doi: 10.1371/journal.pone.0024160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uplekar M, Juvekar S, Morankar S, Rangan S, Nunn P. Tuberculosis patients and practitioners in private clinics in India. Int J Tuberc Lung Dis. 1998;2:324–329. [PubMed] [Google Scholar]
- 4.Suganthi P, Chadha V K, Ahmed J et al. Health seeking and knowledge about tuberculosis among persons with pulmonary symptoms and tuberculosis cases in Bangalore slums. Int J Tuberc Lung Dis. 2008;12:1268–1273. [PubMed] [Google Scholar]
- 5.Gautham M, Binnendijk E, Koren R, Dror D M. ‘First we go to the small doctor’: first contact for curative health care sought by rural communities in Andhra Pradesh & Orissa, India. Indian J Med Res. 2011;134:627–638. doi: 10.4103/0971-5916.90987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar M K, Dewan P K, Nair P K et al. Improved tuberculosis case detection through public-private partnership and laboratory-based surveillance, Kannur District, Kerala, India, 2001–2002. Int J Tuberc Lung Dis. 2005;9:870–876. [PubMed] [Google Scholar]
- 7.Naqvi S A, Naseer M, Kazi A et al. Implementing a public-private mix model for tuberculosis treatment in urban Pakistan: lessons and experiences. Int J Tuberc Lung Dis. 2012;16:817–821. doi: 10.5588/ijtld.11.0440. [DOI] [PubMed] [Google Scholar]
- 8.Government of India, Ministry of Health & Family Welfare, Central TB Division. TB India 2014. Revised National TB Control Programme Annual Status Report: Reach the unreached—find, treat, cure TB, save lives. New Delhi, India: MOHFW; 2014. http://tbcindia.nic.in/index1.php?lang=1&level=1&sublinkid=4160&lid=2807 Accessed March 2016. [Google Scholar]


