Abstract
Setting: Patients with chronic non-communicable diseases attending a primary health care centre, Lilongwe, Malawi.
Objective: Using an electronic medical record monitoring system, to describe the quarterly and cumulative disease burden, management and outcomes of patients registered between March 2014 and June 2015.
Design: A cross-sectional study.
Results: Of 1135 patients, with new registrations increasing each quarter, 66% were female, 21% were aged ⩾65 years, 20% were obese, 53% had hypertension alone, 18% had diabetes alone, 12% had asthma, 10% had epilepsy and 7% had both hypertension and diabetes. In every quarter, about 30% of patients did not attend the clinic and 19% were registered as lost to follow-up (not seen for ⩾1 year) in the last quarter. Of those attending, over 90% were prescribed medication, and 80–90% with hypertension and/or diabetes had blood pressure/blood glucose measured. Over 85% of those with epilepsy had no seizures and 60–75% with asthma had no severe attacks. Control of blood pressure (41–51%) and diabetes (15–38%) was poor.
Conclusion: It is feasible to manage patients with non-communicable diseases in a primary health care setting in Malawi, although more attention is needed to improve clinic attendance and the control of hypertension and diabetes.
Keywords: operational research, SORT IT, non-communicable disease, electronic medical record system, Malawi
Abstract
Contexte : Les patients atteints de maladies chroniques non transmissibles fréquentant un centre de santé primaire et soignés à Lilongwe, Malawi.
Objectif : Se servant d'un système électronique de suivi des dossiers médicaux, décrire le poids trimestriel et cumulé des maladies, la prise en charge et le pronostic des patients enregistrés entre mars 2014 et juin 2015.
Schéma : Une étude transversal.
Résultats : De 1135 patients nouvellement enregistrés avec une augmentation chaque trimestre, 66% étaient des femmes, 21% avaient plus de 65 ans, 20% étaient obèses, 53% avaient une hypertension isolée, 18% avaient un diabète isolé, 12% avaient de l'asthme, 10% avaient une épilepsie et 7% avaient à la fois hypertension et diabète. Chaque trimestre, environ 30% des patients ne se sont pas présentés au centre de santé et 19% ont été enregistrés comme perdus de vue (pas vus depuis au moins 1 an) au cours du dernier trimestre. Parmi ceux qui se sont présentés, plus de 90% ont eu une prescription de médicaments et 80% à 90% des patients atteints d'hypertension et/ou de diabète ont eu une mesure de tension artérielle/de glycémie. Plus de 85% des patients avec épilepsie n'ont pas eu de convulsions et 60–75% des patients atteints d'asthme n'ont pas eu de crise grave. Le contrôle de la tension artérielle (41–51%) et du diabète (15–38%) a été médiocre.
Conclusion : Il est possible de prendre en charge les patients atteints de maladies chroniques non transmissibles dans un contexte de centre de santé primaire au Malawi, mais il faut accorder plus d'attention à l'amélioration de la fréquentation du centre et au contrôle de l'hypertension et du diabète.
Abstract
Marco de referencia: Los pacientes con diagnóstico de enfermedades crónicas no transmisibles que acuden a un centro de atención primaria de salud en Lilongwe, Malawi.
Objetivo: Utilizando un sistema de electrónico seguimiento de las historias clínicas, describir la carga de morbilidad trimestral y acumulada, el tratamiento y el desenlace clínico de los pacientes registrados de marzo del 2014 a junio del 2015.
Método: Fue este un estudio transversal.
Resultados: Se registraron 1135 pacientes y los casos nuevos registrados aumentaron en cada trimestre. De estos pacientes el 66% era de sexo femenino, la 21% de los pacientes tenía 65 años de edad o más, el 20% era obeso, contaba con un diagnóstico exclusivo de hipertensión el 53%, de diabetes el 18%, de asma el 12%, epilepsia el 10% y 7% de los pacientes presentaba hipertensión y diabetes. En cada trimestre, cerca de 30% de los pacientes no acudió al centro y el 19% se registró como perdidos durante el seguimiento (no acudieron en un año o más) en el último trimestre. De los pacientes que acudieron al centro, más del 90% recibió recetas de medicamentos y se midió la tensión arterial y la glucemia en 80% a 90% de los pacientes con diagnóstico de hipertensión, diabetes o ambos. Más del 85% de los pacientes con epilepsia no presentó convulsiones y de 60% a 75% de los pacientes con asma no sufrió crisis graves. Se observó una regulación deficiente de la tensión arterial (de 41% a 51%) y de la diabetes (de 15% a 38%).
Conclusión: Es factible tratar a los pacientes con enfermedades no transmisibles en el marco de la atención primaria de salud en Malawi, pero se precisan esfuerzos encaminados a estimular la asistencia y mejorar el control de la hipertensión y la diabetes.
Chronic non-communicable diseases (NCDs) are now the world's leading cause of mortality, with a significant and rapidly growing impact in low- and middle-income countries (LMICs).1,2 In 2010, there were 34.5 million deaths (two of every three deaths globally) due to NCDs, with cancer, ischaemic heart disease, stroke and diabetes being the predominant causes.3 Despite the increasing burden of disease and associated mortality, access to prevention, care and treatment remains out of reach for most people in LMICs, and as a result there have been calls for action to improve the situation.4,5
In September 2011, the United Nations convened a high-level meeting on NCDs, and agreement was reached on a goal to reduce NCD deaths by 25% by 2025 in people aged 30–70 years.6,7 This was taken forward into the Sustainable Development Goals (SDG), with SDG 3.4 aiming to reduce premature mortality from NCDs by one third by 2030.8 The targets selected to achieve this goal include reducing elevated blood pressure, smoking cessation, reducing salt intake and increasing physical activity. While there is increasing agreement about the upstream policies required to combat NCDs and reduce NCD mortality, far less is known downstream about how to deliver and monitor quality services for the prevention, care and treatment of chronic disease for the millions of people in need.
In LMICs, patients with NCDs are usually managed in tertiary or secondary level hospitals, but there is an urgent and important need to know how to decentralise and integrate the management of NCDs into primary health care and how to monitor the incidence and prevalence of disease, treatment outcomes and associated morbidity and mortality in this setting. A recent study from Kenya reported on the integrated management of patients with hypertension and/or diabetes in a primary health care setting supported by Médecins Sans Frontières (MSF), with encouraging results.9 There is little information, however, about how this could work at the peripheral level in government settings in other LMICs.
In Malawi, a nationwide World Health Organization (WHO) STEPwise approach to Surveillance (STEPS) survey showed that in 2009 respectively 33% and 6% of the population surveyed had hypertension and diabetes mellitus (DM);10 as a result, a Non-Communicable Diseases Management Unit was established within the Ministry of Health. A national strategy and action plan for NCDs has been developed, including the roll-out of the concept of a ‘chronic care clinic’. Currently, most patients with NCDs such as hypertension, DM, asthma and epilepsy are managed in one of the four national tertiary care facilities, or, in some district hospitals, in specialised out-patient clinics treating one disease at a time on separate days of the week. Such specialised clinics are difficult for patients with more than one disease, and may not be cost-effective. A decision was therefore made by the Ministry of Health, in collaboration with partners, to pilot the use of chronic care clinics for key NCDs such as hypertension, DM, asthma and epilepsy at the primary health care level.
To test the concept, a chronic care clinic was set up in the primary health care facility in Area 25, Lilongwe, with patient enrolment starting from March 2014. A decision was made to assess the feasibility, challenges, burden of disease and monitoring system during a 12–15 month period soon after the clinic opened in order to identify gaps, correct mistakes and adjust resources to the disease patterns being observed. The aim of this study was to describe the management and monitoring of patients with NCDs in this primary health care clinic, along with the burden, treatment and programme outcomes of these patients. Specific objectives were to determine, between March 2014 and 30 June 2015: 1) the number of patients registered in each quarter and cumulatively with the different NCDs; 2) the baseline demographic characteristics, risk factors and existing disease-related complications of all patients who had been cumulatively registered by 30 June 2015; 3) the programmatic outcomes in patients cumulatively registered in the five quarters; and 4) the management and treatment outcomes of patients with specific NCDs.
METHODS
Study design
This was a descriptive cross-sectional study involving patients registered with specific NCDs at Area 25 Health Centre, Lilongwe, Malawi.
Setting
General setting
Malawi is a small country in central Africa with an estimated population of 16.4 million and a nominal gross domestic product of US$226 per capita.11 It is divided into three regions and has four public tertiary (referral) hospitals and 28 public district hospitals, where health care services are generally free of charge. There are over 700 primary health care centres throughout the country where the majority of the rural population seeks care, although it is unusual for patients with NCDs to be managed in such peripheral settings. The health care worker to patient ratio and physician to patient ratio are amongst the highest in the world, estimated at 1:277 and 1:50 000, respectively. The task-shifting of care to lower cadres of health care workers is common at both primary and secondary health care facilities.12
Study setting
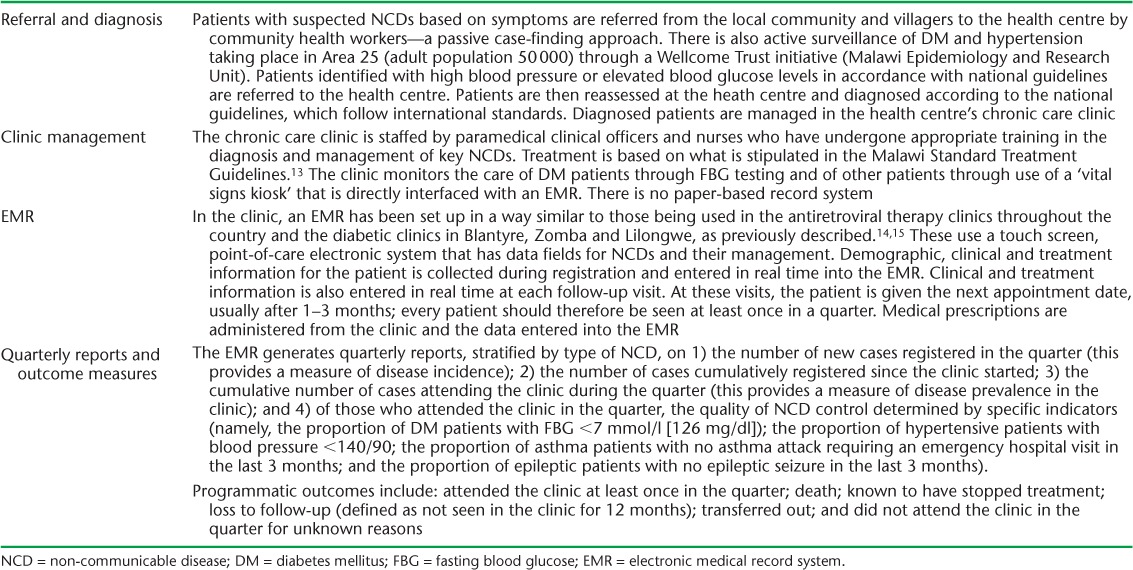
Area 25 Health Centre serves a catchment population of 80 000 adults and children. The chronic care clinic opened formally on 17 March 2014 and started registering patients already under care in the health centre and new patients who were referred or diagnosed with NCDs at the centre. Patients with suspected NCDs are referred to the health centre for diagnosis and care, with a maximum distance between home and the health centre of about 5 km. Once under treatment, patients receive their medications free of charge from the health centre pharmacy. If the health centre has a stock-out of drugs, the patients are advised to go to the public tertiary hospital for their medications. Drugs can be obtained at local pharmacies, but patients have to pay for their medications. The referral, diagnosis, registration, management, monitoring and reporting of NCDs in this centre are briefly described in Table 1.14,15
TABLE 1.
Management and monitoring of NCDs in the chronic care clinic in Area 25 Health Centre, Lilongwe, Malawi
Study population
All patients registered with NCDs in the Area 25 Health Centre chronic care clinic from 17 March 2014 to 30 June 2015 were included in the study.
Data variables and analysis
The data variables collected in this study included the number of patients with hypertension, DM, asthma and epilepsy newly registered in each quarter and cumulatively registered at the end of each quarter; the demographic characteristics such as sex and age; risk factors for NCDs such as current cigarette smoking (⩾1 cigarettes per week), alcohol consumption (drinking any alcohol at any time) and obesity (body mass index ⩾30 kg/m2); existing disease-related complications; cumulative programmatic outcomes (see Table 1) and management and treatment outcomes of each NCD (see Table 1 for the quality of NCD control determined by specific indicators). The data were sourced from integrated cohort quarterly reports generated by the electronic medical record (EMR) system and the paper-based database at the Malawi Epidemiology and Research Unit, Lilongwe. These were exported to an Excel spreadsheet (Microsoft Corp, Redmond, WA, USA) and analysed descriptively using percentages and frequencies.
Ethics
The study was approved by the National Health Sciences Research Committee (Lilongwe, Malawi). The study met the MSF Ethics Review Board (Geneva, Switzerland) approved criteria for studies of routinely collected data, and was also approved by the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease (Paris, France).
RESULTS
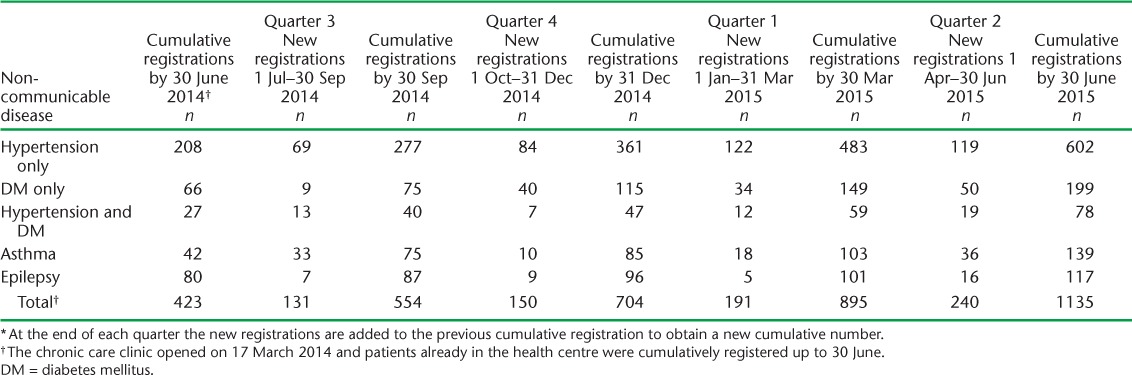
A total of 1135 patients were cumulatively registered in the chronic care clinic between 17 March 2014 and 30 June 2015. The numbers of newly registered patients increased in each quarter, and the cumulative numbers of patients rose by the end of each quarter, as shown in Table 2. Hypertension accounted for 53% of the total cumulative registrations by 30 June, with the remainder of the patients registered with DM (18%), asthma (12%), epilepsy (10%) and hypertension and DM together (7%).
TABLE 2.
Quarterly and cumulative registrations * from March 2014 to June 2015 at Area 25 Health Centre, Lilongwe, Malawi
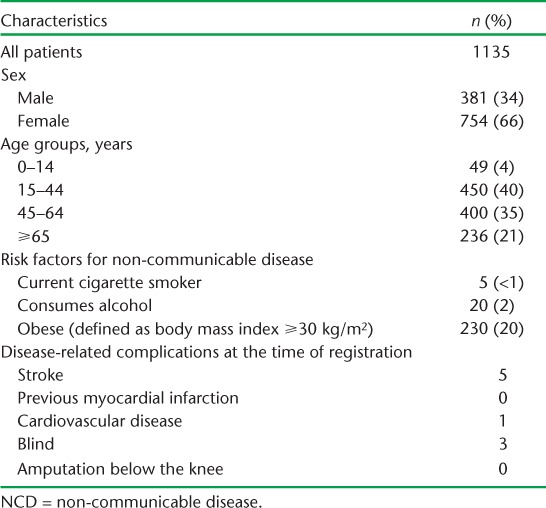
Baseline demographic characteristics, risk factors for NCDs and existing NCD-related complications at the time of registration of all patients are shown in Table 3. There were more females (66%) enrolled into care than males. Of all registered patients, 21% were aged ⩾65 years. Few patients reported cigarette smoking or alcohol consumption. About one fifth of the patients were obese. Only nine patients had disease-related complications (stroke, cardiovascular disease or blindness) at the time of registration.
TABLE 3.
Baseline demographic characteristics, risk factors and NCD-related complications at the time of registration in all patients registered in Area 25 Health Centre, Lilongwe, Malawi, by 30 June 2015
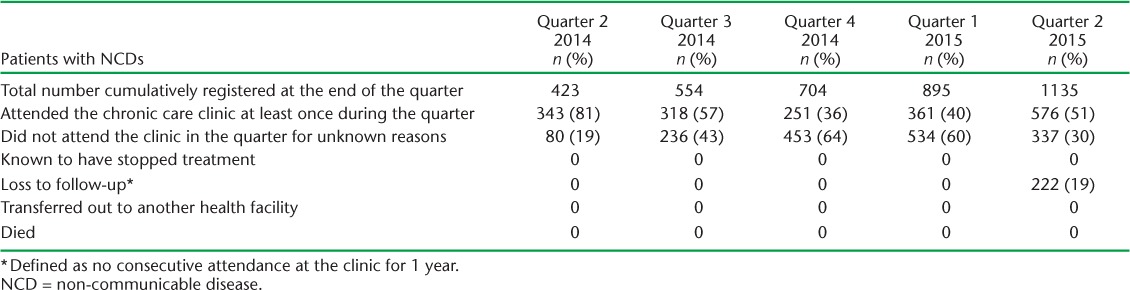
The programmatic outcomes at the end of five quarters for all patients cumulatively registered during these periods are shown in Table 4. No patient was known to have stopped treatment and there were no known deaths or transfers-out (transfer to other health facilities). In every quarter, a substantial proportion of patients did not attend for unknown reasons, and this remained fairly constant, at about 30% during the last four quarters. One year after the clinic had formally opened, the proportion registered as lost to follow-up was 19%.
TABLE 4.
Cumulative programmatic outcomes recorded between Quarter 2 2014 and Quarter 2 2015 in patients registered with NCDs at Area 25 Health Centre, Lilongwe, Malawi
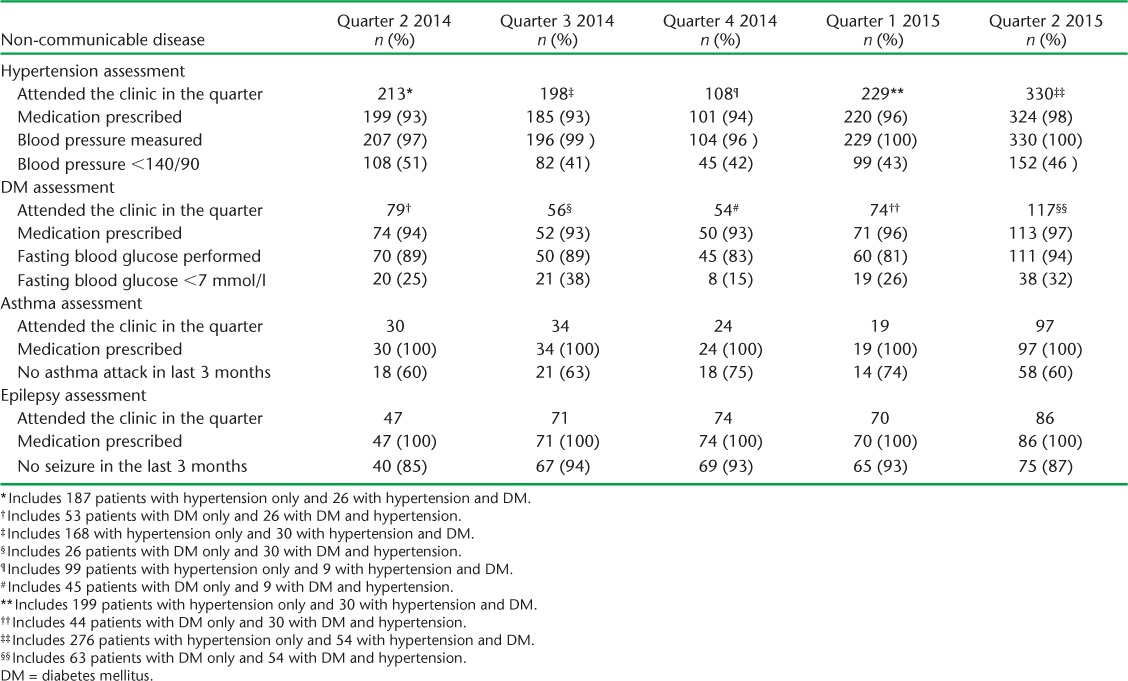
The management and treatment outcomes in patients with hypertension, DM, asthma and epilepsy during each of the five quarters are shown in Table 5. In patients with hypertension (which included those with hypertension alone or in combination with DM), over 90% were prescribed medication and had their blood pressure measured, but during the last four quarters less than 50% had their blood pressure controlled. In patients with DM (which included those with DM alone or in combination with hypertension), over 90% were prescribed medication and over 80% had their fasting blood glucose measured, but only 15–36% had any blood glucose control. All patients with asthma were always given medication, and 60–75% remained without any serious asthma attack between clinic visits. All patients with epilepsy were always given medication, and 85–94% remained seizure-free between visits.
TABLE 5.
Management and treatment outcomes at the end of each quarter in patients who attended the chronic care clinic at Area 25 Health Centre, Lilongwe, Malawi
DISCUSSION
This is the first report from Malawi to describe how a chronic care clinic set up at the primary health care level performed during the first 15 months of operation. There were increasing numbers of patients newly registered each quarter, and the cumulative burden of patients with NCDs was over 1000 by the end of 12 months. Hypertension was the predominant problem. There was a low prevalence of smoking and alcohol consumption, but obesity was recorded in one fifth of patients at presentation. Our working definitions for cigarette smoking and alcohol consumption were imprecise, however, and it is possible that the prevalence of these lifestyle habits was more common than we have reported.
We were able to track programmatic outcomes through the EMR, although this required help from the Wellcome Trust database in the Malawi Epidemiology and Research Unit, Lilongwe. Worryingly, a large proportion of patients who did not attend either in the quarter or after 1 year were recorded as lost to follow-up, meaning that they had not been seen in the clinic for ⩾1 year. We do not know whether they were truly not seen or whether this was a feature of missing data. Furthermore, we do not know whether these patients who were lost to follow-up or recorded as non-attending had died or transferred out, and this requires further investigation. Of patients who were seen, it was encouraging that most were prescribed medication, that most of those with hypertension and/or DM had their blood pressure and/or blood glucose measured and that a substantial proportion with epilepsy had their seizures controlled according to our pre-set parameters. Interestingly, less than 10% of patients had both hypertension and DM, much lower than has been found elsewhere.16,17 This requires further investigation to determine whether patients with DM have their blood pressure measured regularly and vice versa. About a third of patients with asthma had a severe attack in Quarters 2 and 3, compatible with the season of the year when asthma attacks are more frequent in the country.18 Despite medication, the control of blood pressure and DM was generally poor during all of the quarters of the period studied.
The strength of this study is the reporting of the feasibility of running a chronic care clinic within a routine government setting that uses an EMR, with the lessons learnt being applicable to similar settings in Malawi and possibly elsewhere. Furthermore, this observational study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.19 Limitations relate to the operational nature of the study, which included imprecise definitions of NCD risk factors and a lack of detailed individual information about why patients failed to attend the clinic in the various quarters. It is also possible that some of the patients diagnosed and classified as having asthma had chronic obstructive airways disease.
Several implications result from this study. First, the quarterly and cumulative cohort system that we have set up for chronic disease care generally functioned well, and is similar to systems being implemented for DM and hypertension clinics in central hospitals in Malawi13 and in primary health care centres in other countries such as Jordan.16,17 In these other settings, cohort monitoring relies on an electronic system, as this is probably the only way to follow a cohort of patients with their programmatic and management outcomes that increases cumulatively month by month. Over time, the EMR will also allow a survival analysis of each particular cohort to assess the quality of disease control, the development of co-morbidities and the programmatic outcomes, as has been undertaken in Jordan.20 Such information, updated and produced every quarter, will allow the clinic not only to review and assess the growing case load but also to rationally plan for human resources, drugs and consumables that are needed at the facility level.
We did experience challenges with the EMR in the chronic care clinic in Lilongwe, mainly around ascertaining that each patient visit had been recorded and ensuring that the system is functional at all times; there is a need for a rapid response team linked to government that is consistently available to resolve computer problems when they arise. It has been suggested that clinics run both paper-based and electronic record systems. Anecdotally, this has been done elsewhere in antiretroviral clinics in Malawi, but given the human resource constraints that the country faces, with increased workload errors creeping in, we believe it is better to use one system or the other rather than trying to operate both simultaneously.
Second, we need to be more precise about classifying patients as smokers and alcohol consumers, with practical definitions available for health care staff in the clinic. The clinic needs to encourage those who smoke to quit.21 As the system matures, we should also consider capturing information about other risk factors such as salt intake and physical inactivity.22 Obesity increases the risk of cardiovascular disease and stroke,23 and there is growing evidence that in DM or pre-DM patients an increase in daily ambulatory activity leads to a reduction in cardiovascular morbidity.24 Interventions to change lifestyle behaviour need to be introduced at chronic care clinics for patients with hypertension and/or DM, and they need to be accompanied by regular and appropriate monitoring.
Third, we need to become better at controlling hypertension and DM to reduce the morbidity and mortality that accompany these conditions. This is not a problem unique to Malawi. DM is generally poorly controlled throughout most of Africa,25 and globally it is estimated that only about 13% of patients with hypertension have their blood pressure controlled.26
Finally, it would be important to be able to quickly identify patients who failed to attend their scheduled appointments so that they can be brought back to the clinic for a visit through either the aid of outreach workers or the use of mobile phone technology, as has been used in antiretroviral clinics in Kenya.27 Prioritising patients with severe hypertension or badly controlled DM is one way of moving forward on this issue and ensuring that these patients do not miss clinic appointments.
In conclusion, we have shown that it is possible to run and monitor registrations and outcomes for patients with NCDs in an integrated chronic care clinic at the primary health care level in Malawi. The evaluation of the clinic at 12 months has been useful in identifying some shortcomings such as EMR functionality, non-attendance and loss to follow-up, and the clinic needs to improve in controlling blood pressure and blood glucose levels in those with hypertension and DM.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR), Geneva, Switzerland. The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union), Paris, France, and Medécins Sans Frontières (MSF), Brussels Operational Centre, Luxembourg. The specific SORT IT programme that resulted in this publication was jointly developed and implemented by the Operational Research Unit (LUXOR), MSF; the Centre for Operational Research, The Union; the Centre for International Health, University of Bergen, Bergen, Norway; the Institute of Tropical Medicine, Antwerp, Belgium; the University of Nairobi, Nairobi, Kenya; and the University of Chester, Chester, UK.
The authors thank the Malawi Epidemiology and Research Unit, Lilongwe, for their help and assistance in finding data missing in the electronic medical record system, and the World Diabetes Foundation, Gentofte, Denmark, for financial support to help set up the chronic care clinic in Lilongwe.
The operational research programme was funded by The Union, MSF, the Department for International Development, London, UK, and the WHO. The clinic also received financial support from the World Diabetes Foundation, Gentofte, Denmark. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: none declared.
In accordance with WHO's open-access publication policy for all work funded by WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution IGO licence (http://creativecommons.org/licenses/by/3.0/igo/legalcode) which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
References
- 1.Mathers C D, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLOS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lozano R, Naghavi M, Foreman K et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Global status report on non-communicable diseases 2010. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 4.Beaglehole R, Epping-Jordan J, Patel V et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008;372:940–949. doi: 10.1016/S0140-6736(08)61404-X. [DOI] [PubMed] [Google Scholar]
- 5.Maher D, Harries A D, Zachariah R, Enarson D. A global framework for action to improve the primary care response to chronic non-communicable diseases: a solution to a neglected problem. BMC Public Health. 2009;9:355. doi: 10.1186/1471-2458-9-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. A comprehensive global monitoring framework, including indicators, and a set of voluntary global targets for the prevention and control of noncommunicable diseases. WHO; Geneva, Switzerland: Revised WHO discussion paper 25 July, 2012. http://www.who.int/nmh/events/2012/discussion_paper3.pdf. Accessed April 2016. [Google Scholar]
- 7.Beaglehole R, Bonita R, Horton R et al. Measuring progress on NCDs: one goal and five targets. Lancet. 2012;380:1283–1285. doi: 10.1016/S0140-6736(12)61692-4. [DOI] [PubMed] [Google Scholar]
- 8.United Nations. Transforming our world: the 2030 agenda for sustainable development. New York, NY, USA: United Nations; 2015. http://sustainabledevelopment.un.org/post2015/transformingourworld. Accessed April 2016. [Google Scholar]
- 9.Sobry A, Kizito W, Van den Bergh R et al. Caseload, management and treatment outcomes of patients with hypertension and/or diabetes mellitus in a primary health care programme, in an informal setting. Trop Med Int Health. 2013;19:47–57. doi: 10.1111/tmi.12210. [DOI] [PubMed] [Google Scholar]
- 10.Msyamboza K P, Ngwira B, Dzowela T et al. The burden of selected non-communicable diseases and their risk factors in Malawi: nationwide STEPS survey. PLOS ONE. 2011;6:e20316. doi: 10.1371/journal.pone.0020316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Bank. World development indicators 2014. Washington, DC, USA: World Bank; 2014. http://data.worldbank.org/sites/default/files/wdi-2014-book.pdf. Accessed April 2016. [Google Scholar]
- 12.Zachariah R, Ford N, Phillips M et al. Task shifting in HIV/AIDS: opportunities, challenges and proposed actions for sub-Saharan Africa. Trop Med Int Health. 2009;103:549–558. doi: 10.1016/j.trstmh.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 13.Malawi Ministry of Health. Malawi standard treatment guidelines. 5th ed. Lilongwe, Malawi: MOH; 2015. [Google Scholar]
- 14.Allain T J, van Oosterhout JJ, Douglas G P et al. Applying lessons learnt from the ‘DOTS’ Tuberculosis Model to monitoring and evaluating persons with diabetes mellitus in Blantyre, Malawi. Trop Med Int Health. 2011;16:1077–1084. doi: 10.1111/j.1365-3156.2011.02808.x. [DOI] [PubMed] [Google Scholar]
- 15.Douglas G P, Gadabu O J, Joukes S et al. Using touchscreen electronic medical record systems to support and monitor national scale-up of antiretroviral therapy in Malawi. PLOS Med. 2010;7:e1000319. doi: 10.1371/journal.pmed.1000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khader A, Farajallah L, Shahin Y et al. Cohort monitoring of persons with diabetes mellitus in a primary health care clinic for Palestine refugees in Jordan. Trop Med Int Health. 2012;17:1108–1116. doi: 10.1111/j.1365-3156.2012.03097.x. [DOI] [PubMed] [Google Scholar]
- 17.Khader A, Farajallah L, Shahin Y et al. Cohort monitoring of persons with hypertension: an illustrated example from a primary health care clinic for Palestine refugees in Jordan. Trop Med Int Health. 2012;17:1163–1170. doi: 10.1111/j.1365-3156.2012.03048.x. [DOI] [PubMed] [Google Scholar]
- 18.Harries A D, Speare R, Wirima J J. A profile of respiratory disease in an African medical ward. J Roy Coll Physicians Lond. 1988;22:109–113. [PMC free article] [PubMed] [Google Scholar]
- 19.von Elm E, Altman D G, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;147:573–578. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 20.Khader A, Ballout G, Shahin Y et al. Treatment outcomes in a cohort of Palestine refugees with diabetes mellitus followed through use of E-Health over 3 years in Jordan. Trop Med Int Health. 2014;19:219–223. doi: 10.1111/tmi.12241. [DOI] [PubMed] [Google Scholar]
- 21.Lancaster T, Stead L F. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2005;2:CD001292. doi: 10.1002/14651858.CD001292.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Villareal D T, Chose S, Parimi N et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–1229. doi: 10.1056/NEJMoa1008234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects) Lu Y, Hajifathalian K et al. Metabolic mediators of the effects of body-mass index, overweight, hypertension, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383:970–983. doi: 10.1016/S0140-6736(13)61836-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yates T, Haffner S M, Schulte P J et al. Association between change in daily ambulatory activity and cardiovascular events in people with impaired glucose tolerance (NAVIGATOR trial): a cohort analysis. Lancet. 2014;383:1059–1066. doi: 10.1016/S0140-6736(13)62061-9. [DOI] [PubMed] [Google Scholar]
- 25.Mbanya J C N, Motala A A, Sobngwi E, Assah F K, Enoru S T. Diabetes in sub-Saharan Africa. Lancet. 2010;375:2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- 26.Angell S Y, De Cock K M, Frieden T R. A public health approach to global management of hypertension. Lancet. 2015;385:825–827. doi: 10.1016/S0140-6736(14)62256-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lester R T, Ritvo P, Mills E J et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376:1838–845. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]


