Abstract
Setting: A caesarean section (C-section) is a life-saving emergency intervention. Avoiding pregnancies for at least 24 months after a C-section is important to prevent uterine rupture and maternal death.
Objectives: Two years following an emergency C-section, in rural Burundi, we assessed complications and maternal death during the post-natal period, uptake and compliance with family planning, subsequent pregnancies and their maternal and neonatal outcomes.
Methods: A household survey among women who underwent C-sections.
Results: Of 156 women who underwent a C-section, 116 (74%) were traced; 1 had died of cholera, 8 had migrated and 31 were untraceable. Of the 116 traced, there were no post-operative complications and no deaths. At hospital discharge, 83 (72%) women accepted family planning. At 24 months after hospital discharge (n = 116), 23 (20%) had delivered and 17 (15%) were pregnant. Of the remaining 76 women, 48 (63%) were not on family planning. The main reasons for this were religion or husband's non-agreement. Of the 23 women who delivered, there was one uterine rupture, no maternal deaths and three stillbirths.
Conclusions: Despite encouraging maternal outcomes, this study raises concerns around the effectiveness of current approaches to promote and sustain family planning for a minimum of 24 months following a C-section. Innovative ways of promoting family planning in this vulnerable group are urgently needed.
Keywords: emergency obstetrics, family planning, inter-pregnancy interval, sub-Saharan Africa, operational research
Abstract
Contexte : Une césarienne est une intervention d'urgence destinée à sauver une vie. Eviter une nouvelle grossesse pendant au moins 24 mois après une césarienne est important afin de prévenir une rupture utérine et un décès maternel.
Objectifs : Deux ans après une césarienne en urgence, dans le Burundi rural, nous avons évalué : les complications et les décès maternels pendant la période post-natale ; la couverture de la planification familiale et son adhérence ; les grossesses suivantes et leur devenir pour la mère et le nouveau-né.
Méthodes : Enquête à domicile auprès de femmes qui ont bénéficié d'une césarienne.
Résultat : Sur 156 femmes qui ont bénéficié d'une césarienne, 116 (74%) ont pu être retrouvées ; 1 était décédée du choléra, 8 avaient déménagé et 31 n'ont pas pu être localisées. Sur les 116 femmes retrouvées, il n'y a eu aucune complication post-opératoire et aucun décès. Lors de leur sortie de l'hôpital, 83 (72%) femmes ont accepté une contraception. A 24 mois après leur sortie (n = 116), 23 (20%) avaient accouché et 17 (15%) étaient enceintes. Sur les 76 femmes restantes, 48 (63%) n'avaient pas de contraception. Les motifs principaux étaient la religion ou le désaccord du mari. Parmi les 23 qui avaient accouché, il y a eu une rupture utérine, aucun décès maternel, mais il y a eu trois mort-nés.
Conclusion : En dépit de résultats encourageants pour les mères, cette étude pose la question de l'efficacité des approches actuelles de la promotion et de la pérennité de la planification familiale pendant un minimum de 24 mois. Il est urgent de trouver des manières innovantes de promouvoir la planification familiale dans ce groupe vulnérable.
Abstract
Marco de referencia: La cesárea es una intervención de urgencia que salva vidas. Es importante evitar un embarazo por lo menos durante los 24 meses que siguen a la operación, con el fin de evitar la ruptura uterina y la mortalidad materna.
Objetivos: El seguimiento durante 2 años después de una cesárea de urgencia en una zona rural de Burundi tuvo por objeto evaluar las complicaciones y la mortalidad materna durante el período posnatal, la aceptación y el cumplimiento del método de anticoncepción y examinar los siguientes embarazos con su desenlace materno y neonatal.
Método: Se llevó a cabo una encuesta domiciliaria de las mujeres en quienes se había practicado una cesárea.
Resultados: Se evaluaron 116 de las 156 mujeres (74%) que se sometieron a una cesárea; una paciente falleció por cólera, 8 migraron y fue imposible localizar 31 mujeres. Durante el seguimiento de las 116 mujeres no se observaron complicaciones postoperatorias ni defunciones. En el momento del alta hospitalaria, 83 mujeres aceptaron practicar un método anticonceptivo (72%). Veinticuatro meses después del alta hospitalaria, 23 mujeres habían tenido un parto (20%) y 17 estaban embarazadas (15%). De las 76 mujeres restantes, 48 no seguían ningún método de planificación familiar (63%); las principales razones aducidas fueron religiosas o el desacuerdo del cónyuge. En los 23 casos de mujeres que tuvieron un parto, ocurrió una ruptura uterina sin mortalidad materna, pero hubo tres mortinatos.
Conclusión: Pese a la buena perspectiva de los desenlaces maternos favorables, el estudio pone de manifiesto inquietudes con respecto a la eficacia de las estrategias vigentes de promoción y mantenimiento de los métodos anticonceptivos durante un mínimo de 24 meses. Se precisan con urgencia estrategias innovadoras que estimulen la planificación familiar en este grupo vulnerable de mujeres.
Burundi has one of the highest maternal mortality ratios (MMR) in the world, estimated at 740 maternal deaths per 100 000 live births.1 The United Nations Millennium Development Goal 5 (MDG 5) aimed to reduce the MMR by 75% between 1990 and 2015.2 This has now been replaced by Sustainable Development Goal 3 (SDG 3), which aims to reduce the global MMR to less than 70 per 100 000 live births by 2030.3 Most sub-Saharan African countries, including Burundi, are lagging far behind in achieving these desired targets.4
Two previous studies from Burundi showed that offering dedicated emergency obstetric and neonatal care (EmONC), coupled with an efficient ambulance referral network, can rapidly reduce maternal mortality in a rural district setting. This was cited as a possible way forward for achieving and sustaining MDG 5 in sub-Saharan Africa.5,6
Tayler-Smith et al. reported that over 30% of all women transferred from health centres with severe acute maternal morbidity and requiring EmONC underwent a caesarean section (C-section).5 Although a C-section is an immediate and lifesaving surgical intervention, it increases the risk of uterine rupture in future pregnancies.7–9 This risk is accentuated if the inter-pregnancy interval (IPI) is less than 24 months.10
Burundi is known to have high fertility rates of 6.2 per woman compared to 1.8/woman in a country like Belgium.11 Burundi also has very low uptakes of family planning and limited general access to EmONC services.12 These factors further contribute to the risk of uterine rupture and maternal death in a pregnancy that follows a C-section.9
While there are studies from high-income countries on maternal outcomes after a C-section,13 no study from rural Africa has prospectively assessed the status of mothers at household level and as long as 2 years after a C-section. Similarly, no studies have collectively reported on the uptake of family planning, incident pregnancies and the IPI at household-level. Existing knowledge on these issues has been limited to cohorts of women who return to hospital, and is thus subject to selection bias. As these parameters are important determinants of uterine rupture and maternal death in rural Africa, better knowledge of these would help guide maternal health strategies to reduce maternal mortality among vulnerable mothers on the African continent.
We aimed to determine the maternal status of women 2 years following a C-section in a district hospital in rural Burundi. Specific objectives were to determine 1) whether complications and/or death had occurred during the post-natal phase, 2) uptake of and compliance with family planning, 3) subsequent pregnancies, 4) the IPI and 5) maternal and neonatal outcomes of subsequent pregnancies.
METHODS
Study population and period
The study population included all women who underwent a C-section at the EmONC centre and who were discharged between July and September 2012. Only those residing in Bujumbura rural province were included in the study. The study was conducted between July and October 2014.
Design
A prospective household survey using a semi-structured questionnaire.
Study setting
The study was conducted in Bujumbura rural province, one of Burundi's 17 provinces bordering Lake Tanganyika. This rural province is divided into three health districts, Rwibaga, Isale and Kabezi, serving an estimated population of 583 000. In Burundi, an estimated 70% of all deliveries take place in a health structure: 16% in hospitals and 54% in a health centre. Deliveries occurring in health centres and requiring a C-section have to be referred to a hospital. The remaining 30% of deliveries take place at home, without any medical assistance.12
The EmONC centre and C-sections
The EmONC centre, the only one in Bujumbura rural province, is located in Kabezi town and has been described by Tayler-Smith et al. and Zuniga et al.5,6,14 The centre is a dedicated facility located close to the district hospital and 17 km from Burundi's capital, Bujumbura. Roughly 32% of all women who deliver in the EmONC centre undergo a C-section.5 The top five indications for C-sections are obstructed labour, previous C-section, mal-presentation, uterine rupture and foetal distress.15,16 A quarter of all C-sections performed are for mothers who have previously had a C-section.
The decision for C-section is taken by either a general medical doctor or the obstetrician, both of whom perform C-sections. General medical doctors are trained and supervised by the obstetrician. Anaesthesia is given by trained anaesthesia nurses, and in most cases spinal anaesthesia is preferred to general anaesthesia; general anaesthesia with intubation is rarely performed. After surgery, patients are transferred to a recovery room under the supervision of the anaesthesia nurse, and transferred to the obstetric ward once stable.
Risk counselling and family planning for patients who underwent a C-section
In the EmONC centre, all women who underwent a C-section received special counselling sessions by the treating physician and a social-nurse educator on the increased risk for future deliveries. All women were made aware about the importance of child spacing and that they should avoid pregnancy for a minimum of 24 months, per Médecins Sans Frontières (MSF) and World Health Organization guidelines.17,18 Women who underwent a C-section were also counselled explicitly on the importance of having future deliveries in hospital. Prior to discharge, all women received individual counselling on family planning methods from the social-nurse educator. For the purposes of this study, compliance with family planning recommendations was defined as avoidance of any pregnancy during the 24-month period following a C-section and being on a family planning method at the time of the interview.
Prospective household follow-up of women after undergoing a C-section
Data related to the study objectives were extracted from a dedicated EmONC centre electronic database. Each unique patient identity number in the database was cross-checked with clinical files for data validation. The two data sources were used to identify eligible patients, and to create a line-list of women to be followed up and their geographic addresses.
Two nurses who were knowledgeable in emergency obstetric care and spoke Kirundi (the local language) were selected and trained as interviewers. A semi-structured questionnaire, which was pre-tested, translated into Kirundi and back into French, was used for interviews. Prior to the household interviews, line-listed women were visited at home by community health workers and appointments were made for a detailed interview. A dedicated nurse, experienced in performing household surveys, acted as team supervisor and ensured that the interview procedure was respected. This nurse also liaised with community health workers and local district health authorities.
Data and analysis
All data related to the study objectives were double-entered and validated. Inconsistencies were cross-checked with patient files and questionnaires. Where inconsistencies could not be resolved by cross-checking patient files and questionnaires, a dedicated home visit was made for further validation.
EpiData version 3.1 (EpiData Association, Odense, Denmark) was used for data entry and validation while version 2.2.2.182 was used for analysis. Descriptive statistics were used to report results.
Ethics
Ethical approval was obtained from the MSF Ethical Review Board, Geneva, Switzerland, and the National Ethics Review Committee, Bujumbura, Burundi.
RESULTS
Characteristics of the study population at hospital discharge
There were a total of 512 deliveries, of which 228 (45%) were performed by C-section. Of the latter, 72 were from areas outside the Bujumbura rural province and were thus excluded. Of the remaining 156 women eligible to be included in the study, 116 (74%) were traced and interviewed (Figure); of the 40 women who were not found, 1 had died of cholera, 8 had migrated out of the study catchment area and 31 could not be traced at their indicated residential address. On further inquiry, the 31 women were also not known by the village leaders, and had thus possibly given false addresses.
FIGURE.
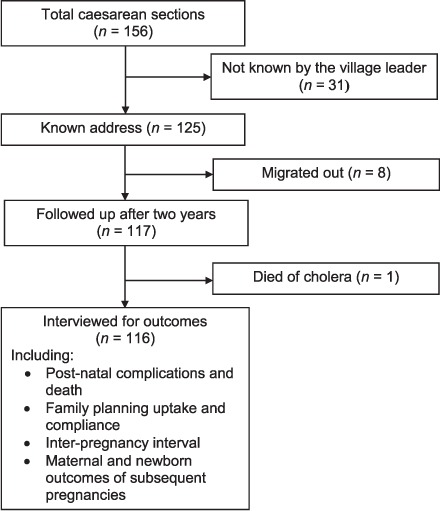
Follow-up status of women residing in Bujumbura rural province 2 years after undergoing a caesarean section, Burundi, 2012.
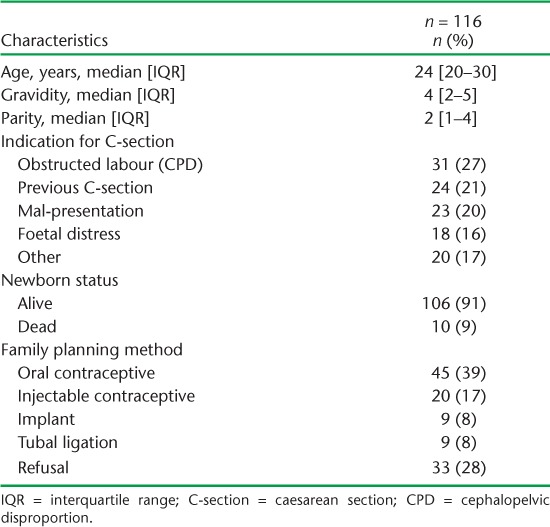
The characteristics of the 116 women included in the interviews are shown in Table 1. The median age was 24 years, median gravidity was 4 (interquartile range [IQR] 2–5), and median parity was 2 (IQR 1–4). The most common reasons for a C-section were obstructed labour (27%) and having had a previous C-section (21%), both of which are recurrent indications for a C-section.
TABLE 1.
Socio-demographic and clinical characteristics of women at discharge and newborn status after a C-section in 2012, district hospital, Bujumbura rural province, Burundi
Complications and death after discharge following a C-section
None of the women suffered from complications following discharge or within the 42-day post-natal period and there were no caesarean-related deaths.
Uptake and compliance with family planning
At discharge, of the 116 women, 83 (72%) accepted a family planning method, of whom only 18 (22%) were using a long-term method (tubal ligation or implants, Table 1). Of the 33 (28%) women who did not accept a family planning method at hospital discharge, the majority (55%; 18/33) wanted to first consult their husbands.
At the time of the interview, 24 months after hospital discharge, 40 women (34%) had already delivered or were pregnant. Of the remaining 76 women, 48 (63%) were not using any family planning method. These 88 individuals were thus considered to be non-compliant with family planning advice (overall family planning compliance at 24 months = 25%). Two women had removed implants inserted at the time of hospital discharge and subsequently became pregnant.
Of the 48 women found not to be using any family planning method at the time of the interview, the main reasons were religious (63%; 30/48); 10/48 (21%) didn't want to, in 5 cases (10%) the husband did not agree, and another 3 (6%) women gave no reason.
Subsequent pregnancies and inter-pregnancy interval
Of the 116 women interviewed, 23 (20%) had already delivered by the time of the interview, and 17 (15%) were pregnant (Table 2). Of the 23 deliveries, 18 (78%) occurred at hospital, 3 in a health centre maternity and 2 at home. The median time between the C-section and the next pregnancy (IPI) for those who had already delivered was 12 months (range 3–16). Three (13%) had become pregnant within 6 months of the C-section. For those who were pregnant at the time of interview, the IPI was 18 months (range 16–24).
TABLE 2.
Subsequent pregnancies following caesarean section and maternal and newborn outcomes, Bujumbura rural province, Burundi
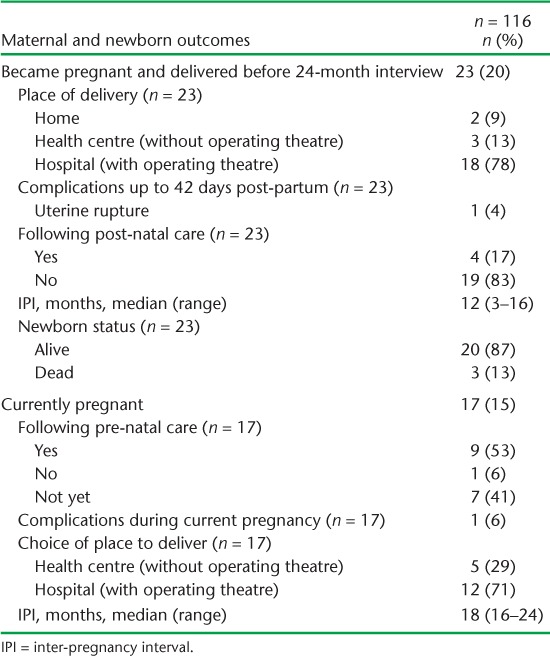
Maternal and neonatal outcomes of subsequent pregnancies
Of the 23 deliveries that occurred before the date of interview, there were no maternal deaths but there were three stillbirths. One woman had had a uterine rupture but survived in hospital.
DISCUSSION
This is the first prospective household study to assess maternal and newborn outcomes at 24 months after an emergency C-section in rural Africa where maternal mortality is high. Encouragingly, there were no reported complications during the post-natal period and no maternal deaths related to C-sections. However, despite intensive counselling efforts to encourage family planning to avoid pregnancies for a 24-month period after the C-section, only three quarters of the women followed this advice at discharge. Disappointingly, compliance with family planning had dropped three-fold, to 25%, at 24 months.
Of particular concern is that about one third of all women had already delivered or become pregnant before the end of the 24-month high-risk threshold for uterine rupture. This raises serious concerns about the effectiveness of current approaches to promote family planning in this high-risk group and context. Family planning is a vital determinant for averting uterine rupture and maternal death post C-section in rural Africa, and ways to improve this situation are urgently needed.
The strengths of this study are that mothers were traced in a systematic manner and determined maternal and newborn outcomes beyond the hospital doors. This is unique in that all other reported studies have assessed one or other parameters and were restricted to the limits of the health facility. Furthermore, the household interviews were conducted in a standardised manner, with well trained and supervised staff. Data were also double-encoded and validated, including repeat visits to mothers' homes, and we thus believe they are robust.
The main study limitation is that we could not trace 39 of the line-listed women. Although eight of these women were known to have migrated for various reasons, we believe that the remaining 31 gave false addresses. This may be because they did not want to be traced for whatever reason or because they originated from neighbouring provinces, where access to emergency obstetric services was poor. In any case, we cannot exclude unascertained complications or deaths in this subgroup, which may negate our reported outcomes.
This limitation aside, the study findings raise a number of operational issues that merit discussion. First, the fact that 40 women became pregnant and/or delivered even when they were at risk of uterine rupture is a possible reflection of socio-cultural pressures to have children. The fact that religion and husbands' opinions were influential determinants of whether women were compliant with family planning advice highlights the need to actively engage with both parties. The way forward is unclear and merits specific operational research. One possible method of engaging husbands is to try to establish contact with them within the community through community health workers. Another method would be to provide the means for transport, which could encourage their presence at the hospital during the mothers' recovery period. The imperative to approach husbands early is highlighted by the fact that five (10%) women in our study expressed the need to consult their husbands before taking up family planning. On the other hand, how to engage with religious leaders on family planning issues remains an unanswered question in contexts such as Burundi.19 This issue needs guidance from specific qualitative research.
Second, despite intensive counselling on the need for family planning for a 24-month period, 28% of the women openly refused to use any allopathic method of family planning. Although this was surprising, it may be related to the very young median age of the cohort and the fact that many mothers had previously lost a newborn. The desire to become pregnant and have a baby might thus have been overwhelming, thereby obliging mothers to refuse family planning despite the associated risks.
Third, about 20% of the women became pregnant and had actually delivered within a much shorter IPI than the recommended 24 months. Five (22%) of these women did not comply with the recommendation to deliver in hospital. This notwithstanding, there was only one case of uterine rupture and no reported maternal deaths. The highly efficient ambulance referral network and high quality emergency obstetric services of the Bujumbura rural province5,6 may explain this encouraging finding. Put simply, even if a woman ran into trouble, she was likely to be managed well. Our findings could thus paint a good case scenario while the real situation in rural contexts where such services do not exist may be much worse.
Finally, there were three stillbirths during subsequent pregnancies. It may well be that the women sought medical help too late, despite the presence of foetal distress, or that other factors may be to blame. The risk for the newborn of a short IPI is thus real.
In conclusion, this first study from rural Burundi highlights important gaps in uptake of and compliance with family planning related to C-sections, and these need to be addressed at both the patient and community level. Perhaps what we need is not more of the same, but to do things differently!
Acknowledgments
The authors thank the research team and community health workers, without whom they would not have been able to locate the participants. They are grateful to the women who were willing to participate and who thanked them for showing interest even two years after.
This study was funded by Médecins Sans Frontières, Brussels Operational Centre, Luxembourg, and the Ministry of Foreign Affairs, Luxembourg.
Footnotes
Conflicts of interest: none declared.
References
- 1.World Health Organization, UNICEF, UNFPA, The World Bank, and the United Nations Population Division. Trends in maternal mortality: 1990 to 2015. Geneva, Switzerland: WHO; 2015. http://data.worldbank.org/indicator/SH.STA.MMRT2015 Accessed February 2016. [Google Scholar]
- 2.United Nations. We can end poverty. NY, New York, USA: UN; 2015. http://www.un.org/millenniumgoals/maternal.shtml Accessed February 2016. [Google Scholar]
- 3.United Nations. Goal 3: Ensure healthy lives and promote well-being for all at all ages. NY, New York, USA: UN; 2015. http://www.un.org/sustainabledevelopment/health/ Accessed February 2016. [Google Scholar]
- 4.Word Health Organization. Atlas of African Health Statistics 2014: health situation analysis of the African region. Brazzaville, Republic of Congo: WHO, Regional Office for Africa; 2014. [Google Scholar]
- 5.Tayler-Smith K, Zachariah R, Manzi M et al. Achieving the Millennium Development Goal of reducing maternal mortality in rural Africa: an experience from Burundi. Trop Med Int Health. 2013;18:166–174. doi: 10.1111/tmi.12022. [DOI] [PubMed] [Google Scholar]
- 6.Tayler-Smith K, Zachariah R, Manzi M et al. An ambulance referral network improves access to emergency obstetric and neonatal care in a district of rural Burundi with high maternal mortality. Trop Med Int Health. 2013;18:993–1001. doi: 10.1111/tmi.12121. [DOI] [PubMed] [Google Scholar]
- 7.Al-Zirqi I, Stray-Pedersen B, Forsen L, Vangen S. Uterine rupture after previous caesarean section. BJOG. 2010;117:809–820. doi: 10.1111/j.1471-0528.2010.02533.x. [DOI] [PubMed] [Google Scholar]
- 8.Hofmeyr G J, Say L, Gulmezoglu A M. WHO systematic review of maternal mortality and morbidity: the prevalence of uterine rupture. BJOG. 2005;112:1221–1228. doi: 10.1111/j.1471-0528.2005.00725.x. [DOI] [PubMed] [Google Scholar]
- 9.Mukasa P K, Kabakyenga J, Senkungu J K, Ngonzi J, Kyalimpa M, Roosmalen V J. Uterine rupture in a teaching hospital in Mbarara, western Uganda, unmatched case-control study. Reprod Health. 2013;10:29. doi: 10.1186/1742-4755-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stamilio D M, DeFranco E, Pare E et al. Short interpregnancy interval: risk of uterine rupture and complications of vaginal birth after cesarean delivery. Obstet Gynecol. 2007;110:1075–1082. doi: 10.1097/01.AOG.0000286759.49895.46. [DOI] [PubMed] [Google Scholar]
- 11.Institut de Statistiques et d'Études Économiques du Burundi et Institut National de Santé Publique. Enquête Démographique et de Santé Burundi 2010. Bujumbura, Burundi: ISTEEBU et INSP; 2011. [French] [Google Scholar]
- 12.Ministère de la Santé Publique et de la Lutte Contre le SIDA. Annuaire statistique des données des centres de santé et des hôpitaux pour l'année 2010. Bujumbura, Burundi: MSPLS; 2011. [French] [Google Scholar]
- 13.Guise J M, McDonagh M S, Osterweil P, Nygren P, Chan B K, Helfand M. Systematic review of the incidence and consequences of uterine rupture in women with previous caesarean section. BMJ. 2004;329:19–25. doi: 10.1136/bmj.329.7456.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zuniga I, Van den Bergh R, Ndelema B et al. Characteristics and mortality of neonates in an emergency obstetric and neonatal care facility, rural Burundi. Public Health Action. 2013;3:276–281. doi: 10.5588/pha.13.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chu K, Cortier H, Maldonado F, Mashant T, Ford N, Trelles M. Cesarean section rates and indications in sub-Saharan Africa: a multi-country study from Medecins Sans Frontières. PLOS ONE. 2012;7:e44484. doi: 10.1371/journal.pone.0044484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dumont A, de Bernis L, Bouvier-Colle M H, Breart G. Caesarean section rate for maternal indication in sub-Saharan Africa: a systematic review. Lancet. 2001;358:1328–1333. doi: 10.1016/s0140-6736(01)06414-5. [DOI] [PubMed] [Google Scholar]
- 17.Coutin A S. Essential obstetric and newborn care. In: Médecins Sans Frontières, editor. 2015 ed. Paris, France: Médecins Sans Frontières; 2015. [Google Scholar]
- 18.World Health Organization. Report of a WHO technical consultation on birth spacing, Geneva, Switzerland, 13–15 June, 2005. Geneva, Switzerland: WHO; 2006. http://www.who.int/maternal_child_adolescent/documents/birth_spacing.pdf Accessed February 2016. [Google Scholar]
- 19.Yeatman S E, Trinitapoli J. Beyond denomination: the relationship between religion and family planning in rural Malawi. Demographic research. 2008;19:1851–1882. doi: 10.4054/DemRes.2008.19.55. [DOI] [PMC free article] [PubMed] [Google Scholar]


