Abstract
Purpose
the present prospective open-label study was designed to gain further insights into a condition thought to constitute a neglected but not uncommon syndrome characterized by anterior shoulder pain and tenderness to palpation over the apex of the coracoid process, not related to rotator cuff or pectoralis minor tendinopathy, long head of the biceps tendon disorders, or instability. The aim was to clarify its prevalence, clinical characteristics, differential diagnosis and response to corticosteroid injections.
Methods
patients with primary anterior shoulder pain precisely reproduced by deep pressure on the apex of the coracoid process were recruited. Patients with clinical or instrumental signs of other shoulder disorders were excluded. Patients were given an injection of triamcinolone acetonide 40 mg/ml 1 ml at the coracoid trigger point. They were evaluated after 15, 30 and 60 days and at 2 years using Equal Visual Analog Scale (EQ-VAS) and the Italian version of the Simple Shoulder Test (SST).
Results
between January 1 and December 31 2010, we treated 15 patients aged 26–66 years. The majority were women (86.67%). At 15 days, 6 (40%) patients reported complete resolution of their symptoms, while 9 (60%) complained of residual symptoms and received another injection. At 30 days, 14 (93.33%) patients were pain-free and very satisfied. At 2 years, the 14 patients who had been asymptomatic at 30 days reported that they had experienced no further pain or impaired shoulder function. The analysis of variance for repeated measures showed a significant effect of time on EQ-VAS and SST scores.
Conclusions
the present study documents the existence, and characteristics, of a “coracoid syndrome” characterized by anterior shoulder pain and tenderness to palpation over the apex of the coracoid process and showed that the pain is usually amenable to steroid treatment. This syndrome should be clearly distinguished from anterior shoulder pain due to other causes, in order to avoid inappropriate conservative or surgical treatment.
Level of evidence
Level IV, therapeutic case series.
Keywords: anterior shoulder pain, coracoid, syndrome, enthesitis
Introduction
Anterior shoulder pain is a very common symptom whose reported annual incidence in primary care settings is 14.7 per 1000 patients per year (1). It is related to a variety of causes that are extrinsic and intrinsic to the shoulder girdle. The major extrinsic causes are cervical brachial pain, shoulder-hand syndrome and neuritis (2). The most common intrinsic causes include rotator cuff and long head of the biceps tendon (LHBT) disorders, adhesive capsulitis, osteoarthritis, acromioclavicular joint disorders, instability syndromes, and “bench-presser’s shoulder”. Shoulder impingement syndrome and rotator cuff disorders usually present with anterolateral shoulder pain that is exacerbated by activities above the shoulder level, along with tenderness to palpation over the rotator cuff tendons with the shoulder in extension (3). Tendonitis of the long head of the biceps brachii is almost always correlated with rotator cuff or labrum pathology. The typical history is the appearance of pain in the anterior aspect of the shoulder that is elicited or worsened by palpation on the bicipital groove and at the level of pectoralis major insertion (4). The pain is also exacerbated by shoulder flexion and lifting activities that involve elbow flexion. In most literature describing the differential diagnosis of anterior shoulder pain, the coracoid process is mentioned, but not as a site causing pain. Gerber et al. described a type of anterior shoulder pain thought to result from impingement of the anterior rotator cuff with the coracoacromial ligament and the deep surface of the coracoid (5), and to be favored by congenital or acquired narrowing of the subcoracoid space. Other researchers consider this a rare condition (6). Symptoms of coracoid impingement syndrome include anterior shoulder pain, occasionally radiating down to the upper arm/forearm. The pain is made worse by passive flexion. On palpation, there is tenderness over the coracoid process (5). Bench-presser’s shoulder is an overuse insertional tendinopathy of the pectoralis minor muscle usually affecting weightlifters and bodybuilders. On examination, medial juxta-coracoid tenderness is present and the active-contraction test and bench-press maneuver are positive (7).
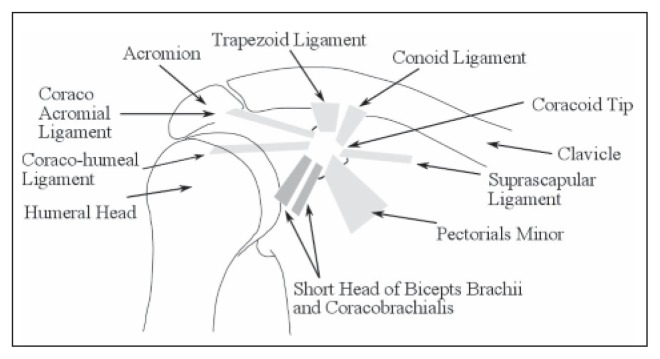
The coracoid is an anterior transverse process of the scapula and it exhibits marked interindividual variability in shape and size (8). Variations in the height and length of the coracoid process are, in most cases, responsible for differences in the size and shape of the space between the coracoacromial arch and the rotator cuff (9). Its medial border is attached to the pectoralis minor, with the result that the function of this muscle is to tilt the scapula anteriorly during activities such as bench-pressing, swimming and push up-exercises (10). The apex of the coracoid process is embraced by the conjoined tendon of the coracobrachialis and short head of the biceps brachii (SHB) muscles (11). The subcoracoid space is occupied by the articular capsule of the glenohumeral joint, the subscapularis tendon and the subacromial bursa. The thickness of these tissues may vary, but variations are small and do not affect the width of the subcoracoid space, unless there is local pathology. The suprascapular ligament is attached by one end to the base of the coracoid process and by the other to the medial end of the scapular notch. It converts the scapular notch into a foramen. The suprascapular nerve runs through this foramen and may be impinged by suprascapular ligament ossification. The coracohumeral ligament arises from the lateral border of the coracoid process, and passes obliquely downward and lateral to the front of the greater tubercle of the humerus. In adhesive capsulitis it is shortened and thickened due to fibroblastic proliferation, thus limiting external rotation (12). The location of the coracoid and its surrounding attachments are schematized in Figure 1.
Fig. 1.
Anterior view of the shoulder joint showing the coracoid process and surrounding structures.
In the course of the senior Author’s long experience with shoulder problems, a large number of patients have presented with anterior shoulder pain but no clinical signs of subacromial or subcoracoid impingement, rotator cuff or pectoralis minor tendinopathy, subscapularis or LHBT disorders, or symptoms and signs of instability. A feature shared by all these patients was tenderness in the anterior part of the shoulder, where deep pressure applied on the apex of the coracoid process elicited the pain symptoms they typically experienced. Treatment of some of these patients with corticosteroid injection at the level of the apex of the coracoid process resulted in rapid, significant and lasting clinical improvement. This intriguing fact prompted the Authors to conduct a PubMed search for reports of “coracoid syndrome”, “coracoid and inflammation”, “tendinopathy and short head of biceps brachii and coracobrachialis”, and “enthesitis and short head of biceps brachii and coracobrachialis” in research papers and the main shoulder surgery books (13–15). The search retrieved a single case series describing local pain that was attributed to enthesitis of the SHB and coracobrachialis at the coracoid process (16).
The present prospective open-label study was designed to gain further insights into this disorder and clarify its prevalence, clinical characteristics, differential diagnosis and response to corticosteroid injections in patients presenting with anterior shoulder pain due to a variety of causes. The starting hypothesis was that these clinical features and response to treatment are distinctive of a neglected but not uncommon syndrome.
Methods
The study was approved by the local institutional review board and complies with the latest version of the Helsinki Declaration, with Good Clinical Practice (GCP), and with relevant national regulations. Before the commencement of any study-related activities, including treatment, each study participant was given exhaustive information and asked to provide a signed informed consent form.
The inclusion criteria were: anterior shoulder pain; pain symptoms elicited exclusively by deep pressure applied on the apex of the coracoid process; and normal coracohumeral distance (CHD) and coracoid index (CI) values (respectively >11.5 mm and >8.2 mm) on MRI (with the arm in adduction) (17, 18).
The exclusion criteria were: pain symptoms elicited by digital pressure applied on an area of tenderness medial to the coracoid along the inferior-medial orientation of the muscle fibers, the anterolateral subacromial area and the apex of the contralateral coracoid process; symptoms, clinical signs (e.g. painful active-contraction test and bench-press maneuver), X-ray, or MRI findings suggesting other shoulder girdle disorders, including tendon tears, adhesive capsulitis or coracoid impingement; previous or multiple shoulder problems; neck pain symptoms or clinical features indicating neck pathology; ipsilateral upper limb problems; suspected nerve compression; clinical signs or laboratory test findings of rheumatic disease, including fibromyalgia (19); and obesity, as this condition hampers digital palpation of the coracoid process.
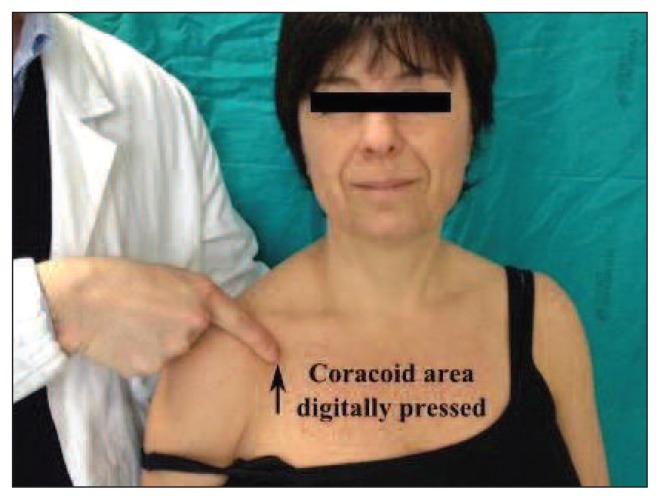
Between 1st January and 31st December 2010, a total of 284 patients with primary anterior shoulder pain unrelated to trauma or surgery were seen at the Shoulder and Elbow Service of our University or at the senior Author’s private practice. Of these, 269 patients were excluded for the following reasons: subacromial impingement syndrome (n=80), rotator cuff tear (n=62), instability (n=51), acromioclavicular joint pathology (n=28), glenohumeral joint arthritis (n=17), calcific tendinitis (n=17), LHBT disorders (n=12), and coracoid impingement (n=2). The remaining 15 patients (13 women and 2 men with a mean age of 49.27±11.44 years, range: 26–66 years), reported an at least six-month history of unilateral shoulder pain (8 right, 7 left shoulders) both during daily activities and at night. None of the patients practised sporting activities involving the upper limb; all reported doing only occasional moderate walking, running or cycling. Although they were unable to describe the site of their pain precisely, identical pain symptoms were elicited, in all the patients, by deep pressure on the apex of the coracoid process. Eleven patients (73.33%) remembered performing abrupt, repetitive flexion and adduction movements of the shoulder against resistance with the elbow in extension (as when lifting a person from a bed) prior to symptom onset; the other 4 reported that their job involved movements of this kind. None of the patients suffered from diabetes or from other metabolic diseases. Two patients had hypertension that was well controlled with medications; one had thyroid disease that was treated with levothyroxine. Another patient had been treated with chemotherapy for breast cancer 5 years earlier. Pain information was obtained by asking patients to rate its severity on a 100 mm visual analogue scale (EQ-VAS), where 0 indicated no pain and 100 the most severe pain imaginable. The test was considered positive if the score difference for pain elicited by pressure on the apex of the coracoid process was ≥30 compared with other three areas around the coracoid (Fig. 2). The Italian version of the Simple Shoulder Test (SST) was also applied (20). Patients were given an injection of triamcinolone acetonide 40 mg/ml 1 ml under ultrasound guidance in sterile conditions at the coracoid trigger point. In normal-weight patients this point is easy to identify since it is found at the inferior pole of the apophysis, at the site of the enthesis of the conjoined tendon, which is located 1 cm inferiorly to the insertion of the coracoacromial ligament and 1.5 cm laterally to the insertion of the conoid and trapezoid ligaments. Patients were asked to forgo sports and avoid overhead movements as much as possible for 15 days. They were prospectively evaluated at 15, 30 and 60 days and at two years after the first infiltration using the same measures. Further injections were performed as necessary. Patients were contacted 2 years after the first infiltration for a telephone interview. We evaluated the prevalence of coracoid syndrome in the orthopaedic patient population reporting shoulder problems by taking the population presenting at our center with anterior shoulder pain as the denominator and the cases found to present with the syndrome as the numerator. Mean and standard deviation (SD) of the mean as well as 95% confidence intervals were calculated for the EQ-VAS and SST. A one-way repeated measures ANOVA was performed to evaluate the effect of treatment on the EQ-VAS and SST scores. Greenhouse-Geisser correction was used, when necessary, to correct for violations of sphericity. The Bonferroni adjustment for multiple comparisons was used for pairwise post-hoc analyses. Partial eta squared (η2), and Cohen’s d were calculated to show effect size.
Fig. 2.
Clinical evaluation of coracoid syndrome. Digital pressure on the coracoid area (black arrow) elicits intense pain with respect to other shoulder areas.
No funder was involved in any of the stages of this trial, including the design of the study, the data collection, analysis and interpretation, the writing of the manuscript, or the decision to submit the paper for publication. All the Authors had full access to all the data in the study. The final decision to submit the report for publication was made by the senior Author.
Results
The one-year prevalence of coracoid syndrome among patients with anterior shoulder pain was 5.28% (CI 2.99–8.56). The vast majority of the patients were women (86.67%) and the mean age at symptom onset was 48.23±11.99 years.
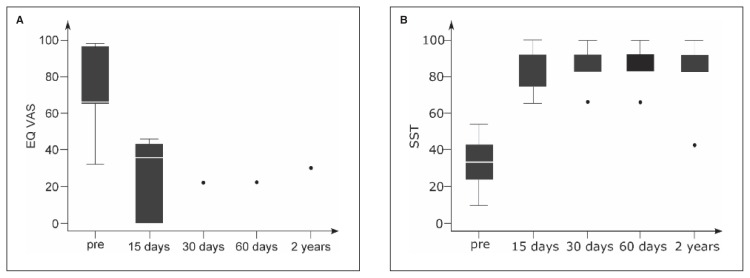
At baseline (prior to treatment), the 15 patients had a mean EQ-VAS score of 75.53±19.63 (CI 64.66–86.40) and their mean SST score was 31.67±10.54 (CI 25.83–37.4). The scores recorded before and after the treatment are summarized in Figure 3.
Fig. 3.
Distribution of mean outcome measurement scores of participants at different follow-up times. A: EQ-VAS scores. B: SST scores (white line, median; box limit, quartiles; extreme values, minimum-maximum; pre, pretreatment).
As regards the effects of the first treatment, 3 (20%) patients reported a transient burning sensation immediately after the injection or mild pain over the first 2–3 days.
At the first follow-up at 15 days, 6 (40%) patients, with a mean baseline EQ-VAS score of 86.00±16.30 (CI 68.89–100) and a mean baseline SST score of 26.39±9.74 (CI 16.17–36.61), reported complete resolution of their pain symptoms (EQ-VAS score 0) and nearly complete recovery of shoulder function (SST score 93.01±6.27; CI 86.43–99.59); in these cases, therefore, the decision on whether or not to perform a further injection was postponed to the subsequent follow-up visit. The other 9 (60%) patients, whose mean baseline scores were EQ-VAS: 68.56±19.28 (53.74–83.38) and SST: 35.19±8.99 (CI 28.28–42.10), reported residual pain (EQ-VAS: 41.33±4.18; CI 38.12–44.54) and unsatisfactory recovery of shoulder function (SST: 71.30±4.39; CI 67.93–74.67), and received another injection.
At 30 days, 14 (93.33%) patients were pain-free (EQ-VAS: 0) and very satisfied with their shoulder function (SST: 89.88±5.83; CI 86.51–93.25); all 14 decided against further treatment. The last patient (6.66%) had residual pain (EQ-VAS: 22) and unsatisfactory shoulder function (SST: 66.67), and received a third infiltration. At 60 days this patient still complained of anterior shoulder pain and his scores were the same as at the previous visit, but he admitted that he had never stopped lifting heavy weights. All the other patients were asymptomatic and their SST scores were unchanged from the previous follow-up visit.
There were no severe complications related to the infiltrations during either the treatment or the follow-up.
At 2 years all patients were interviewed by telephone and offered an appointment for another visit. All accepted and were examined by the junior Author. The 14 patients who had been asymptomatic at 30 days reported that they had experienced no further pain or impaired shoulder function in either the affected or the contralateral shoulder. The patient who had received three infiltrations reported periodic exacerbations, although the pain was less intense (EQ-VAS: 22) than before treatment; he also told us that he had sometimes seen a physiotherapist. Deep pressure on the coracoid still elicited tenderness, and he showed a positive Neer and Hawkins signs for supraspinatus impingement. MRI in this patient revealed degenerative tendinopathy of the supraspinatus without tendon tears or calcifications, and conservative treatment was prescribed. Analysis of variance (ANOVA) for repeated measures showed a significant effect of time on the scores of both measures: VAS, F(4,14)=74.29, p<0.05, and SST, F(4,14)=25.70, p<0.05; in particular, partial variance of time for VAS accounted for η2=0.85, and Cohen’s f = 2.39; while SST η2 was =0.89, and Cohen’s f = 2.85.
Discussion
This prospective open-label observational study demonstrates the existence and illustrates the characteristics of a “coracoid syndrome” characterized by anterior shoulder pain and tenderness to palpation over the coracoid process at the common tendon origin of the biceps brachii and coracobrachialis muscles. Its prevalence in the 284 patients presenting with anterior shoulder pain in 2010 was 5.28% (CI 2,99–8,56); middle-aged women made up the overwhelming majority of the affected patients. Treatment of the syndrome is straightforward and effective; indeed, a single infiltration of triamcinolone acetonide was found to induce complete and statistically significant pain resolution and restoration of shoulder function to a level comparable to that of the contralateral shoulder in 40% of patients. After the second infiltration achieved these effects were obtained in a further 53.33% of patients. The ANOVA for repeated measures showed a significant effect of time on VAS and SST scores. The only patient still experiencing symptoms at 2 years – who was also the only patient who never stopped lifting heavy weights – nevertheless reported improved shoulder pain and function. A possible explanation for this case is that his coracoid syndrome, combined with an initially undiagnosed supraspinatus tendinitis, worsened with shoulder overuse and finally led to tendon inflammation, which does not respond to steroid treatment.
A clinical syndrome characterized by anterior shoulder pain that increases with flexion and adduction but not with activities above the shoulder has been described only once before, by Karim et al. (16). Their 6 patients experienced tenderness (identical to their typical symptoms) on palpation over the coracoid process at the common tendon origin of the biceps brachii and coracobrachialis muscles, and their impingement X-ray series were reported to be normal. They received diagnostic bupivacaine injection before corticosteroid infiltration at the level of the coracoid process over the common tendon origin of the biceps brachii and coracobrachialis muscles. All 6 patients reported improvement or resolution of symptoms at follow-up and were able to return to their usual activities. The Authors diagnosed these patients’ condition as enthesitis of the SHB and coracobrachialis at the coracoid process caused primarily or secondarily by injury or altered mechanics. In our opinion, the patients described by Karim et al. presented the same characteristics as those reported in the current study, and may therefore be considered to have been affected by the same syndrome. However, that study was not prospective and the syndrome was not further investigated. Moreover, the Authors did not report pain or function scores, nor did they perform MRI investigations for rotator cuff diseases or assessments that could exclude coracoid impingement (CHD, CI).
There are other disorders that may be responsible for anterior shoulder pain and these should be considered in the differential diagnosis. The coracoid is an uncommon site of shoulder disease. Gerber et al., in their report on coracoid impingement syndrome, were the first to assign the coracoid a role in shoulder pathology (5). They calculated, on CT scans, that the physiological CHD is about 8.6 mm, and found that this distance was reduced in patients with suspected impingement syndrome. The shape and size of the coracoid process were also held to affect the development of coracoid impingement, as is true of the acromion in rotator cuff impingement. According to these Authors, coracoid impingement syndrome is characterized clinically by dull pain in the anterior region of the shoulder that may (rarely) radiate to the arm and forearm. The pain is induced and worsened by elevation and internal rotation, abduction, or simple internal rotation of the arm; moreover, it is greatest at between 120 and 130° of elevation, rather than at between 60 and 120°, as seen in the more common subacromial impingement syndrome. Infiltration of local anesthetic into the subcoracoid space temporarily relieves the pain.
In an anatomical morphometric study of the coracoid process and the coracoglenoid (CG) space, Gumina et al. described three scapula configurations. Type 1, found in 45% of scapulae, is characterized by the lowest mean values of the CG angle and coracoid overlap, which are associated with a short CHD. The Authors suggested that the type 1 configuration, with concomitant severe narrowing of the CG space, may be a predisposing factor for coracoid impingement (21). Bench-presser’s shoulder is an overuse insertional tendinopathy of the pectoralis minor muscle usually affecting male weightlifters and bodybuilders with an average age of around 30 years. The initiating and aggravating factor is the bench-press exercise. Tenderness is present on medial palpation (not over the apex) of the coracoid along the inferior-medial orientation of the pectoralis minor muscle fibers. The active-contraction test and bench-press maneuver are both positive and evoke the symptoms experienced by the patients when performing bench-press exercise (7). These clinical aspects differentiate bench-presser’s shoulder from the current syndrome. Subacromial impingement syndrome and rotator cuff disorders usually present with an intense pain, mainly in the lateral border of the acromion and the lateral portion of the deltoid muscle. Active and resisted movements are painful and may be partially restricted, whereas passive movements are full, albeit painful. Weakness, positive Hawkins and Neer impingement signs, and positive tendon tear signs on the Jobe and Apley tests are components of the history and physical examination. Radiography may show humeral head sclerosis or cysts, loss of acromial-humeral interval and acromial spur (3). Pain related to pathology of the biceps tendon is located mainly at the anterior part of the shoulder, often at the bicipital groove and is elicited or worsened by palpation. Several provocative tests for isolating pathology of the LHBT have been described, including Yergason’s test, Speed’s test and the biceps instability test. For the diagnosis of SLAP lesions, the most common clinical tests are the O’Brien active compression test and the abduction external rotation supination test. In dislocations of the LHBT the tenderness is more medial on the lesser tuberosity, and the tendon can sometimes be rolled under the fingers (22). Adhesive capsulitis is characterized by deep joint pain and impaired external rotation. On examination, global pain is present along with restriction of all movements, both active and passive. Adhesive capsulitis is more common in people with diabetes or thyroid disease and may occur following a single traumatic event or also after prolonged immobilization (23). Glenohumeral instability is more likely under the age of 40 and often presents as an ongoing impingement following dislocation due to structural instability or poor proprioceptive muscle control. Apprehension sign, with the arm in abduction and external rotation, is usually present and laxity tests such as the sulcus sign are positive (24). Glenohumeral osteoarthritis usually presents as global pain in patients older than 50 years. Crepitus and decreased motion, especially external rotation, is consistent with the diagnosis. Radiographs are diagnostic (25). Acromioclavicular joint pathology is usually well localized and is secondary to trauma or osteoarthritis. Tenderness to palpation and occasionally swelling at the acromioclavicular joint, and pain on cross-body adduction testing, extreme internal rotation, and forward flexion are consistent with the diagnosis (26).
In our study none of the 15 patients had symptoms, clinical signs or X-ray/MRI findings that suggested other disorders of the shoulder girdle, including coracoid impingement syndrome. In particular, the mean CHD and CI in the adducted arm were in the normal range. Furthermore, none had type 1 scapula.
The distinctive characteristics of our patients compared with other patients with anterior shoulder pain are tenderness at the level of the apex of the coracoid process, where deep pressure elicited the symptom, and rapid, significant and lasting clinical improvement after corticosteroid injection at the same site. Karim et al. attributed the syndrome to enthesitis, albeit of unknown cause (16).
In an anatomical study, Crichton and Funk recently showed that the origin of the SHB “consisted of muscle fibers attaching directly to the tip of the coracoid process, with a thin, tendinous aponeurosis covering its anterior surface, rather than a true tendon as previously described” (27). In the light of this, the syndrome here described should be regarded as a fasciitis of the SHB and coracobrachialis at the coracoid process.
Most of our patients reported having performed abrupt and repetitive shoulder flexion and adduction against resistance with the elbow in extension before symptom onset, or having done work involving these movements over a long period of time. It is thus reasonable to surmise that the type, mode and duration of these movements may be involved in the development of coracoid syndrome. Lack of response to steroids at the coracoid trigger point should lead the clinician to search for non-coracoid causes.
Limitations of our study are the lack of randomization and placebo control groups, the low number of patients treated, and the fact that this was a single-center experience.
In conclusion, the present study documents a “coracoid syndrome” characterized by anterior shoulder pain and tenderness to palpation over the apex of the coracoid process at the common tendon origin of the SHB and coracobrachialis muscles; the pain in this syndrome is usually amenable to steroid treatment. Middle-aged women seem to be predominantly affected. The syndrome should be clearly distinguished from other several causes of anterior shoulder pain and in particular from bench-presser’s shoulder, coracoid impingement and shoulder capsulitis. Rheumatic diseases might be investigated, but they usually involve multiple joints and have different clinical characteristics. Coracoid syndrome should be included in the differential diagnosis of anterior shoulder pain, and palpation of the apex of the coracoid should be included in routine physical examination of the shoulder, to avoid inappropriate conservative or surgical treatments.
References
- 1.van der Windt DA, Koes BW, de Jong BA, et al. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54:959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lollino N, Brunocilla PR, Poglio F, et al. Non-orthopaedic causes of shoulder pain: what the shoulder expert must remember. Musculoskelet Surg. 2012;96( Suppl 1):S63–S68. doi: 10.1007/s12306-012-0192-5. [DOI] [PubMed] [Google Scholar]
- 3.Diercks R, Bron C, Dorrestijn O, et al. Dutch Orthopaedic Association. Guideline for diagnosis and treatment of subacromial pain syndrome: a multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop. 2014;85:314–322. doi: 10.3109/17453674.2014.920991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarmento M. Long head of biceps: from anatomy to treatment. Acta Reumatol Port. 2015;40:26–33. [PubMed] [Google Scholar]
- 5.Gerber C, Terrier F, Ganz R. The role of the coracoid process in the chronic impingement syndrome. J Bone Joint Surg Br. 1985;67:703–708. doi: 10.1302/0301-620X.67B5.4055864. [DOI] [PubMed] [Google Scholar]
- 6.Neer CS, 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983;65:1232–1244. [PubMed] [Google Scholar]
- 7.Bhatia DN, de Beer JF, van Rooyen KS, et al. The “bench-presser’s shoulder”: an overuse insertional tendinopathy of the pectoralis minor muscle. Br J Sports Med. 2007;41:e11. doi: 10.1136/bjsm.2006.032383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Terra BB, Ejnisman B, de Figueiredo EA, et al. Anatomic study of the coracoid process: safety margin and practical implications. Arthroscopy. 2013;29:25–30. doi: 10.1016/j.arthro.2012.06.022. [DOI] [PubMed] [Google Scholar]
- 9.Cay N, Tosun O, IŞık C, et al. Is coracoacromial arch angle a predisposing factor for rotator cuff tears? Diagn Interv Radiol. 2014;20:498–502. doi: 10.5152/dir.2014.14102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kendall FP, McCreary EK. Muscles: Testing and Function. 3rd edn. Williams & Wilkins; Baltimore/London: 1983. p. 106. [Google Scholar]
- 11.Standring S. The Anatomical Basis of Clinical Practice. Churchill Livingstone Elsevier; London: 2008. Gray’s Anatomy. [Google Scholar]
- 12.Li JQ, Tang KL, Wang J, et al. MRI findings for frozen shoulder evaluation: is the thickness of the coracohumeral ligament a valuable diagnostic tool? PLoS One. 2011;6:e28704. doi: 10.1371/journal.pone.0028704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rockwood CA, Jr, Matsen FA, 3rd, Wirth MA, et al. The Shoulder. 4th ed. Saunders Elsevier; Philadelphia: 2009. [Google Scholar]
- 14.Iannotti JP, Williams JR. Disorders of the Shoulder: Diagnosis & Management. Lippincott Williams & Wilkins; Philadelphia: 2007. [Google Scholar]
- 15.Rockwood CA, Bucholz RW, Court-Brown CM, et al. Rockwood and Green’s Fractures in Adults. Lippincott Williams & Wilkins; Philadelphia: 2010. [Google Scholar]
- 16.Karim MR, Fann AV, Gray RP, et al. Enthesitis of biceps brachii short head and coracobrachialis at the coracoid process: a generator of shoulder and neck pain. Am J Phys Med Rehabil. 2005;84:376–380. doi: 10.1097/01.phm.0000159973.97391.c9. [DOI] [PubMed] [Google Scholar]
- 17.Giaroli EL, Major NM, Lemley DE, et al. Coracohumeral interval imaging in subcoracoid impingement syndrome on MRI. AJR Am J Roentgenol. 2006;186:242–246. doi: 10.2214/AJR.04.0830. [DOI] [PubMed] [Google Scholar]
- 18.Dines DM, Warren RF, Inglis AE, et al. The coracoid impingement syndrome. J Bone Joint Surg Br. 1990;72:314–316. doi: 10.1302/0301-620X.72B2.2312576. [DOI] [PubMed] [Google Scholar]
- 19.Kavanaugh AF, Solomon DH American College of Rheumatology Ad Hoc Committee on Immunologic Testing Guidelines. Guidelines for immunologic laboratory testing in the rheumatic diseases: anti-DNA antibody tests. Arthritis Rheum. 2002;47:546–555. doi: 10.1002/art.10558. [DOI] [PubMed] [Google Scholar]
- 20.Marchese C, Cristalli G, Pichi B, et al. Italian cross-cultural adaptation and validation of three different scales for the evaluation of shoulder pain and dysfunction after neck dissection: University of California - Los Angeles (UCLA) Shoulder Scale, Shoulder Pain and Disability Index (SPADI) and Simple Shoulder Test (SST) Acta Otorhinolaryngol Ital. 2012;32:12–17. [PMC free article] [PubMed] [Google Scholar]
- 21.Gumina S, Postacchini F, Orsina L, et al. The morphometry of the coracoid process - its aetiologic role in subcoracoid impingement syndrome. Int Orthop. 1999;23:198–201. doi: 10.1007/s002640050349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahrens PM, Boileau P. The long head of biceps and associated tendinopathy. J Bone Joint Surg Br. 2007;89:1001–1009. doi: 10.1302/0301-620X.89B8.19278. [DOI] [PubMed] [Google Scholar]
- 23.Uppal HS, Evans JP, Smith C. Frozen shoulder: a systematic review of therapeutic options. World J Orthop. 2015;6:263–268. doi: 10.5312/wjo.v6.i2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rossy WH, Cieslak K, Uquillas CA, et al. Current trends in the management of recurrent anterior shoulder instability. Bull Hosp Jt Dis. 2014;72:210–216. [PubMed] [Google Scholar]
- 25.Menge TJ, Boykin RE, Byram IR, et al. A comprehensive approach to glenohumeral arthritis. South Med J. 2014;107:567–573. doi: 10.14423/SMJ.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell C, Adebajo A, Hay E, et al. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331:1124–1128. doi: 10.1136/bmj.331.7525.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crichton JC, Funk L. The anatomy of the short head of biceps – not a tendon. Int J Shoulder Surg. 2009;3:75–79. doi: 10.4103/0973-6042.63209. [DOI] [PMC free article] [PubMed] [Google Scholar]