Abstract
The optimal treatment and the best rehabilitation protocol after an acute Achilles tendon rupture (ATR) remain a matter of controversy in orthopaedic and sports medicine. The use of validated injury-specific outcome instruments is the only way to clarify these issues, in order to ensure that patients receive the best possible treatment.
This article describes the most commonly reported outcome measures used to assess patients treated for ATR. On the basis of the available evidence, the Achilles tendon Total Rupture Score (ATRS) is the most appropriate outcome measure for evaluating the management of acute ATR.
Keywords: Achilles tendon, surgical treatment, conservative treatment, outcome evaluation
Introduction
Proper evaluation tools are of the utmost importance both in the scientific setting, for the evaluation and comparison of research studies, and in the clinical setting, for guiding therapeutic decisions and assessing the progression of treatments. Recent years have seen an increase in the demand for validated, reliable and responsive outcome measures.
Acute Achilles tendon rupture (ATR) is one of the most common tendon injuries in the adult population, especially in men in their third and fourth decades of life (1).
Despite improved knowledge of Achilles tendon pathology, the optimal treatment and the best rehabilitation protocol after an acute rupture remain a matter of controversy in orthopaedic and sports medicine. The use of validated injury-specific outcome instruments is the only way to clarify these issues, in order to ensure that patients receive the best possible treatment.
This article describes the most commonly reported outcome measures used to assess patients treated for ATR. The aim is to provide clinicians and researchers with an overview of the available evidence on the question of what evaluation tools should be used for this specific injury.
Outcome measures following ATR
The outcome measures used to evaluate functional results following an ATR can be broadly divided into two types: objective measures and patient-reported measures.
The former are parameters directly taken by the clinician, such as ankle range of motion (ROM) or calf muscle strength measurements. These objective data, derived from the patient’s physical examination, have traditionally formed the basis of functional assessment following an ATR.
However, over the past two decades, it has become increasingly recognized that the patient’s own appraisal of outcome is of the utmost importance when judging the results of a treatment (2).
In this regard, none of the traditional objective parameters has been convincingly correlated with patient satisfaction (3, 4).
Therefore, it is now well accepted that traditional outcome measures need to be complemented by measures that focus on the patient’s own feelings regarding a given treatment. This is clearly demonstrated by the explosion, in the literature, of patient-reported outcome measures, i.e. questionnaires completed by patients to measure their perceptions of their own functional status and wellbeing (5–7).
Objective and subjective parameters used to evaluate treatment modalities for ATR are variably reported in the literature – as isolated measures or grouped into different multi-item scoring systems (Tab. 1).
Table 1.
Commonly reported outcome measures used to assess patients treated for Achilles tendon rupture.
| Objective Measures | Multi-item Scoring Scales | |
|---|---|---|
|
| ||
| Clinician-based | Patient-reported | |
|
| ||
| Achilles tendon elongation | AOFAS Ankle-Hindfoot Scale | The Achilles Tendon Rupture Score (ATRS) disease specific |
| Calf muscle size | Leppilahti Score | The Foot and Ankle Outcome Score (FAOS) region specific |
| Calf muscle strength | The Foot and Ankle Ability Measure (FAAM) region specific |
|
| Calf muscle endurance | Short Form-36 (SF-36) generic |
|
| Ankle range of motion | ||
| Achilles tendon mechanical properties | ||
Validity, reliability and responsiveness are the clinimetric properties that define the clinical relevance of each outcome measure (8). In this regard, it is worth remembering that the process of establishing the usefulness of an outcome instrument is never complete, but rather an ongoing process whereby evidence is collected to support the use of the instrument under various conditions (9).
Objective measures
After an ATR patients have been reported to show a lengthening of the healed tendon along with impairments of joint ROM and calf muscle strength, endurance and trophism. Therefore, when evaluating the final outcome of treatment, it is important to include these clinician-generated measurements (10). Each of these parameters is usually compared between the injured and the healthy side, in order to establish the limb symmetry index expressed as a percentage (11).
Achilles tendon lengthening
Some thirty years ago, Nyström and Holmlund reported the occurrence of postoperative separation of the tendon ends after suturing of ruptured Achilles tendons in patients immobilized for three weeks in a position of slight plantarflexion (12). More recently, Schepull et al. confirmed these observations, describing a biphasic lengthening of the tendon in the recovery period after an ATR, regardless of the type of treatment (13).
Although there have been improvements in the therapeutic strategies, Achilles tendon lengthening after ATR remains a frequent complication, assumed to cause functional modifications in the ankle ROM, strength deficits and gait abnormalities (14–16).
To explain the proposed relationship between tendon elongation and functional impairments, it has been suggested that the lengthening of the tendon reduces the tension of the whole musculotendinous unit. As a consequence the power produced by the calf muscle contraction is reduced because the muscle is potentially acting at a different point in its force-length curve (16). Tension of this unit is also necessary for the healing of muscle fibers. Therefore slackness of the tendon can also affect the potential for strength recovery through physical therapy (17). Schepull et al. could not find any correlation between tendon elongation and other functional outcomes after ATR (13), suggesting that variations in elongation within reasonable limits probably do not influence the end result. Currently there exists no clear definition and no validated outcome measure for tendon elongation. Nyström and Holmlund reported a technique involving the placement of a marker (thin steel wire) at each end of the tendon during the surgical repair and subsequent direct measures of the position of these markers on postoperative standardized X-ray (12). Silbernagel et al. evaluated Achilles tendon length as the distance between the calcaneal osteotendinous junction and musculotendinous junction, by means of non-invasive ultrasound imaging (15). Selvik reported the use of Roentgen stereophotogrammetric analysis (RSA) to measure, with high accuracy, the distance between implanted tantalum beads in three dimensions (18).
In conclusion, given its potential influence on functional recovery, an important treatment goal appears to be to minimize tendon elongation.
Calf muscle strength
Calf muscle strength is significantly reduced following ATR. The majority of the reports on functional outcome after an ATR show a permanent strength deficit of up to 30% compared with the uninjured side (19, 20). Because of the detrimental effects related to persistent calf muscle strength deficit, the treatment of an ATR should not only restore the Achilles tendon length but also the original strength of the whole musculotendinous unit (17). In several studies strength measurements obtained through dynamometry were used to evaluate outcome after surgical and conservative treatment of ATR (21–23).
Currently, there is no consensus regarding the best method to determine strength. Both isokinetic and isometric measurements of ankle dorsiflexion and plantarflexion power are reported, as well as eccentric and concentric surveys. The position used, in the clinical setting, to measure these parameters also varies between studies (17, 21–24).
The reliability of isokinetic and isometric dynamometry is generally high, and the various testing positions for plantarflexion and dorsiflexion have good test-retest reliability (25, 26).
Strength deficits following an acute ATR seem to be related to anatomical and structural changes of the healed tendon, specifically elongation, as the ability of the calf muscle to contract is not reduced after the injury (16).
However, it is important to remember that although strength tests are valid for measuring improvements in strength, they are only moderately correlated to functional performance and they need to be supplemented with other types of functional assessment (17, 27).
Endurance/heel-rise test
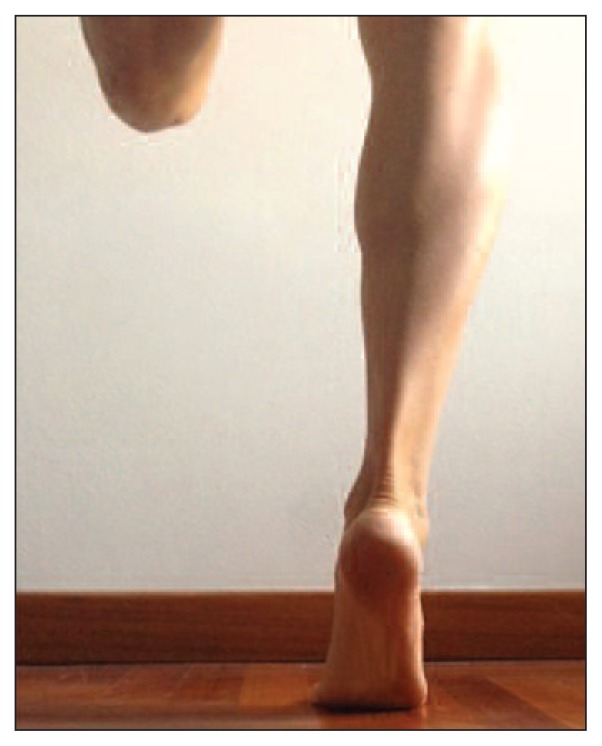
Evaluation of muscular endurance is another type of muscle function measurement. The heel-rise test is the most commonly used test for measuring calf muscle endurance (28) (Fig. 1).
Fig 1.
The Heel Rise Test - The subject is standing on one leg, maintaining a straight knee; support with the fingertips for balance.
The subject being tested stands on one leg, while maintaining a straight knee, using fingertip support for balance, and avoiding body sway forward. It is important to instruct the patient to go as high as possible with every heel rise. Heel rise can be measured both as the number of repetitions and the height of each heel rise (29). This test has been shown to be reliable, valid and responsive in patients with ATR (30, 31).
Following an ATR there is a significant deficit in heel-rise height and repetition between the injured and uninjured side (14, 15, 29). Silbernagel et al. showed a correlation between the degree of tendon elongation and the side-to-side deficit in heel-rise height (15). The test also correlated well with isokinetic measurements in several research studies (4, 19, 30).
Given these observations, and the ease of execution of the test, the heel-rise test is recommended as a measure of functional recovery after ATR.
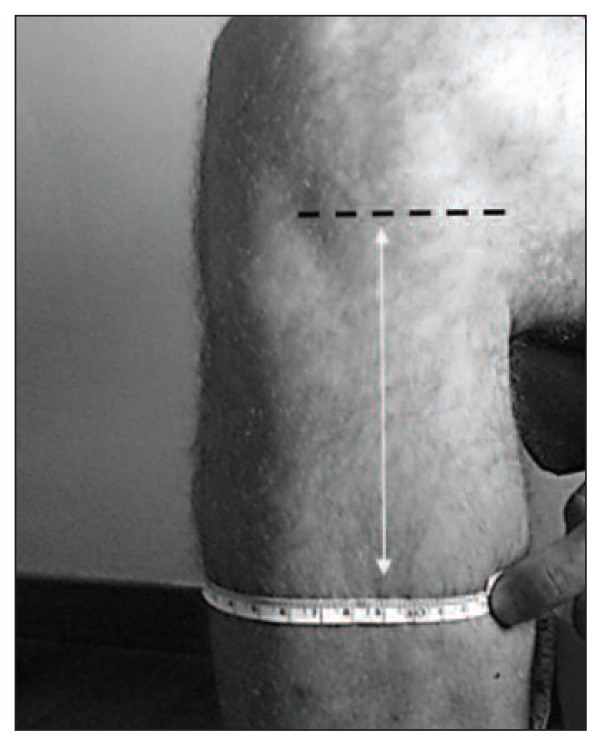
Calf muscle size
Calf muscle circumference is measured to evaluate muscle trophic modifications after rupture and during the recovery phase. It is important to remember that there are aspects, such as swelling and body composition (relative presence of fat tissue versus muscle tissue), that need to be taken into account in order to obtain unambiguous interpretations of circumference values. Different techniques are described to measure this parameter. Some Authors propose CT or MRI measurement techniques (13, 22, 23), while others report circumference values detected manually at predetermined positions related to bony landmarks (33) (Fig. 2). Regardless of the technique used, calf circumference is described as a reliable parameter (30, 32).
Fig 2.
Calf muscle circumference - The maximal calf circumference is measured relative to fixed identifiable bony landmarks, e.g. the medial joint line.
Nevertheless, its correlation with other important outcomes, such as calf muscle endurance and strength, is debated (17, 19, 33).
Leppilahti et al. reported muscle size recovery in only 30% of patients surgically treated for an ATR, in spite of excellent isokinetic strength results in 73% (33).
Conversely, Rosso et al. recently reported that calf muscle circumference is an easy-to-measure parameter that correlates well with the force that can be exerted by the muscle (17). Möller et al. (19) showed that when calf muscle size is evaluated by means of CT-derived cross-sectional area, it correlates well with the muscular ability to perform repeated heel-rise tests. These apparently conflicting data suggest that the assessment technique is probably an important factor influencing the validity of calf muscle size as an outcome for evaluating recovery after ATR.
Ankle range of motion
Measurements of joint ROM are common both in clinical and in research settings.
Ankle ROM is usually used as an indirect measure of tendon elongation: increased dorsiflexion after an ATR is assumed to result from tendon lengthening.
Goniometric measurements, both active and passive, in different positions are described in the literature (34). These measurements have been shown to have higher intra-tester than inter-tester reliability (11).
Other parameters
In an attempt to propose increasingly valid outcome measures, some Authors described specific mechanical parameters for evaluating different treatment regimens for ATR. Selvik was the first to use RSA to describe the mechanical properties of a healing Achilles tendon (18). Using an RSA technique Schepull et al. calculated the early modulus of elasticity of the healing tendon and found a correlation with late functional outcome (13, 35). Interestingly the Authors reported no difference in early mechanical properties between operative and non-operative treatment for ATR.
Rosso et al. (17) recently introduced pedobarographic analysis of plantar pressure distribution as a means of evaluating the results of different surgical techniques for ATR. They found a significant correlation between the push-off force and calf muscle volume measurements. Dynamic pedobarography is easy to measure and seems to be a suitable tool for evaluating functional changes following an ATR (36).
Multi-item scoring scales
These rating systems are important measures of subjective (the patient’s perception of pain and function) and objective (physical examination) data, or both, and they are useful for evaluating and comparing patient functioning and different treatment modalities. Generally, outcome scales are characterized as global, regional or disease-specific. Each type of instrument has an unique purpose and has advantages and disadvantages that affect its potential usefulness. Global scales like the Short Form-36 (SF-36) (37) are designed to be general health status assessment tools; the SF-36 may be used in different patients and in different conditions, but it might not capture important aspects of a specific disease. Conversely, disease-specific measures are designed to assess function, pain and disability in specific conditions, and have the important advantage of showing greater responsiveness in capturing changes in the targeted disease. Region-specific instruments contain items specific to only one body part (e.g. the foot or ankle) and they can be used in several different disease states affecting this specific region (9, 38).
In 2011, Kearney et al. (39) performed a systematic review of the literature in order to identify the most suitable outcome scales for the assessment of patients after an ATR. The Authors reported 21 different multi-item patient outcome measures, of which the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scale was the most frequently used. Of all the cited tools, the Achilles tendon Total Rupture Score (ATRS) was the only one developed using recognized methodology for outcome measure development (5).
We here provide a brief description of some of the outcome scales commonly used in research studies on ATR treatment.
The American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scale
The AOFAS developed its Ankle-Hindfoot Scale in 1994, in order to provide a universally accepted outcome measure for comparing different methods of treatment in patients with hindfoot problems (40) (Tab. 2).
Table 2.
The AOFAS Ankle - Hindfoot Scale.
| Pain (40 points) | |
| None | 40 |
| Mild, occasional | 30 |
| Moderate, daily | 20 |
| Severe, almost always present | 0 |
| Function (50 points) | |
| Activity limitations, support requirement | |
| No limitations, no support | 10 |
| No limitation of daily activities, limitation of recreational activities, no support | 7 |
| Limited daily and recreational activities, cane | 4 |
| Severe limitation of daily and recreational activities, walker, crutches, wheelchair, brace | 0 |
| Maximum walking distance, blocks | |
| Greater than 6 | 5 |
| 4–6 | 4 |
| 1–3 | 2 |
| Less than 1 | 0 |
| Walking surfaces | |
| No difficulty on any surface | 5 |
| Some difficulty on uneven terrain, stairs, inclines, ladders | 3 |
| Severe difficulty on uneven terrain, stairs, inclines, ladders | 0 |
| Gait abnormality | |
| None, slight | 8 |
| Obvious | 4 |
| Marked | 0 |
| Sagittal motion (flexion plus extension) | |
| Normal or mild restriction (30° or more) | 8 |
| Moderate restriction (15°–29°) | 4 |
| Severe restriction (less than 150) | 0 |
| Hindfoot motion (inversion plus eversion) | |
| Normal or mild restriction (75%–100% normal) | 6 |
| Moderate restriction (25%–74% normal) | 3 |
| Marked restriction (less than 25% normal) | 0 |
| Ankle-hindfoot stability (anteroposterior, varus-valgus) | |
| Stable | 8 |
| Definitely unstable | 0 |
| Alignment (10 points) | |
| Good, plantigrade foot, midfoot well aligned | 10 |
| Fair, plantigrade foot, some degree of midfoot malalignment observed, no symptoms | 5 |
| Poor, nonplantigrade foot, severe malalignment, symptoms | 0 |
This clinician-based outcome scale gathers both subjective and objective factors into numerical scales and has a maximum total score of 100 points. The subjective portion has been shown to have satisfactory reliability and responsiveness (41).
As a region-specific system, the AOFAS Ankle-Hindfoot Scale is intended to be used in several hind-foot problems affecting the ankle, subtalar, talonavicular and calcaneocuboid joints (40).
As a result, it is commonly used to evaluate conditions and treatments very different from ATR and ATR treatment, such as ankle arthroplasty, talonavicular arthrodesis and ankle instability (42). Although the Ankle-Hindfoot Scale is routinely reported as an outcome measure in studies in patients with ATR (39, 43), its validity and responsiveness have never been evaluated in this specific population (24, 39). Therefore some Authors question its clinical relevance. On the basis of the available evidence this scale cannot be recommended for use in research studies on ATR (11, 44).
The Achilles tendon Total Rupture Score ATRS
The ATRS (Tab. 3) is a patient-reported, injury-specific instrument developed in 2007 to specifically evaluate outcome after treatment in patients with ATR (45). This questionnaire is a self-administered instrument, filled out by the patient and scored by the clinician. It consists of ten items evaluating aspects of symptoms and function. Each item has scores ranging between 0 and 10 on a Likert scale. The instrument therefore has a maximum score of 100, which corresponds to no symptoms and full function.
Table 3.
The Achilles Tendon Total Rupture Score (ATRS).
| All questions refer to your limitations/difficulties related to your injured Achilles tendon. | |||||||||||
| Mark with an X the number which matches your level of limitation! | |||||||||||
| 1. Are you limited due to decreased strength in the calf/Achilles tendon/foot? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 2. Are you limited due to fatigue in the calf/Achilles tendon/foot? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 3. Are you limited due to stiffness in the calf/Achilles tendon/foot? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 4. Are you limited due to pain in the calf/Achilles tendon/foot? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 5. Are you limited during activities of daily living? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| All questions refer to your limitations/difficulties related to your injured Achilles tendon | |||||||||||
| Mark with an X the number which matches your level of limitation! | |||||||||||
| 6. Are you limited when walking on uneven surfaces? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 7. Are you limited when walking quickly up the stairs or up a hill? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 8. Are you limited during activities that include running? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 9. Arc you limited during activities that include jumping? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10. Are you limited in performing hard physical labor? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
Thanks to its injury-specific nature the ATRS has demonstrated multiple facets of validity for use in the specific ATR patient population (39).
The reliability, validity and responsiveness of the ATRS have been evaluated and confirmed outside the developing center and for languages other than that of the original version (24, 46, 47).
At present, the best available evidence suggests that the ATRS is the most appropriate outcome measure for evaluating the management of acute ATR (11, 39).
The Leppilahti Score
Described by Leppilahti et al. in 1998, the Leppilahti Score (Tab. 4) is the first reported disease-specific standardized protocol for evaluation of outcome after ATR (48). This scoring system combines both subjective assessments of symptoms and objective measures, such as ankle ROM and isokinetic calf strength. It has a total of seven items giving a sum of 100 points as the best possible score.
Table 4.
The Leppilahti Score.
| Pair | |
| None | 15 |
| Mild, no limitations on recreational activities | 10 |
| Moderate, limitations on recreational, but not daily activities | 5 |
| Severe, limitations on recreational and daily activities | 0 |
| Stiffness | |
| None | 15 |
| Mild, occasional, no limitations on recreational activities | 10 |
| Moderate, limitations on recreational, but not daily activities | 5 |
| Severe, limitations on recreational and daily activities | 0 |
| Calf muscle weakness (subjective) | |
| None | 15 |
| Mild, no limitations on recreational activities | 10 |
| Moderate, limitations on recreational, but not daily activities | 5 |
| Severe, limitations on recreational and daily activities | 0 |
| Footwear restrictions | |
| None | 10 |
| Mild, most shoes tolerated | 5 |
| Moderate, unable to tolerate fashionable shoes, modified shoes tolerated | 0 |
| Active range of motion (ROM) difference between ankles | |
| Normal (<6°) | 15 |
| Mild (6°–10°) | 0 |
| Moderate (11°–15°) | 5 |
| Severe (>15°) | 0 |
| Subjective result | |
| Very satisfied | 15 |
| Satisfied with minor reservations | 10 |
| Satisfied with major reservations | 5 |
| dissatisfied | 0 |
| Isokinetic muscle strength (score) | |
| Excellent | 15 |
| Good | 10 |
| Fair | 5 |
| Poor | 0 |
The Leppilahti score is currently reported in several research studies on ATR treatment (21, 49, 50). However, a potential limitation for comparison between different studies is the presence, in the final score, of parameters for the detection of which no consensus has been established, such as muscle strength (24).
The Foot and Ankle Ability Measure (FAAM)
Described by Martin et al. in 2005 (51), the FAAM is a self-reported outcome instrument that takes the form of questionnaire filled out by the patient. It is region specific, being divided into two separate subscales, namely activities of daily living and sports activities, comprising 21 and 8 items respectively. The two subscales are scored separately, then summed: a higher score represents a higher level of physical function (51) (Tabs. 5, 6).
Table 5.
The Foot and Ankle Ability Measure (FAAM). Activities of Daily Living Subscale.
| Please answer every question with one response that most closely describes to your condition within the past week. | ||||||
| If the activity in question is limited by something other than your foot or ankle mark not applicable (N/A). | ||||||
| Activities | ||||||
| Standing | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking on even ground | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking on even group without shoes | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking up hills | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking down hills | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Going up stairs | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Going down stairs | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking on uneven ground | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Stepping up and down curbs | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Squatting | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Coming up on your toes | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking initially | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking 5 minutes or less | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking approximately 10 minutes | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Walking 15 minutes or greater | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Because of your foot and ankle, how much difficulty do you have with: | ||||||
| If the activity in question is limited by something other than your foot or ankle mark not applicable (N/A). | ||||||
| Activities | ||||||
| Home responsibilities | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Activities of daily life | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Personal care | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Light to moderate work (standing, walking) | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Heavy work (pushing/pulling, climbing, carrying) | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Recreational activities | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| How would you rate your current level of function during your usual activities of daily living from 0 to 100 with 100 being your level of function prior to your foot or ankle problem and 0 being the inability to perform any of your usual daily activities? | ||||||
Table 6.
The Foot and Ankle Ability Measure (FAAM). Sports Subscale.
| Because of your foot and ankle, how much difficulty do you have with: | ||||||
| If the activity in question is limited by something other than your foot or ankle mark not applicable (N/A). | ||||||
| Activities | ||||||
| Running | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Jumping | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Landing | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Starting and slopping quickly | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Cutting/lateral movements | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Low impact activities | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Ability to perform activity with your normal technique | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| Ability to participate in you desired sport as long as you would like | No difficulty | Slight difficulty | Moderate difficulty | Extreme difficulty | Unable to do | N/A |
| How would you rate your current level of function during your sports related activities from 0 to 100 with 100 being your level of function prior to your foot or ankle problem and 0 being the inability to perform any of your usual daily activities? | ||||||
| Overall, how would you rate your current level of function? | Normal | Nearly normal | Abnormal | Severely abnormal | ||
This scale has been validated for individuals with a broad range of musculoskeletal disorders of the lower leg, foot and ankle, with reported evidence of validity, reliability and responsiveness (28). In a recent systematic review on clinimetric properties of the outcome scales used to measure lower leg conditions, Shultz et al. reported the FAAM to be one of the most frequently assessed in terms of evidence of responsiveness (38). Nevertheless, to date the FAAM has not been evaluated for use in the specific ATR patient population.
Conclusions
A proper outcome evaluation following an ATR is essential in order to properly ascertain the effectiveness of available treatment modalities. At present, the use of validated, responsive and reliable rating systems is the only way to allow comparisons of outcomes across clinical practice, which, in turn, may help us to draw conclusions about the optimal treatment.
The best choice of outcome tools for reporting the results of treatment in patients with foot and ankle disorders remains uncertain. Nevertheless, on the basis of the available evidence, a patient treated for an ATR should be assessed with a disease-specific measure, such as the ATRS, in combination with a generic measure, such as the SF-36. These patient-reported outcome scales focus on the patient’s perception of his/her health status, which has to be considered the most important indicator of the success of a treatment. Patient-reported outcome scales should be complemented by objective indicators of function, such as muscle strength, endurance and return to previous activity level, in order to obtain a complete picture of the effect of the treatment.
References
- 1.Hattrup SJ, Johnson KA. A review of ruptures of the Achilles tendon. Foot Ankle. 1985;6:34–38. doi: 10.1177/107110078500600107. [DOI] [PubMed] [Google Scholar]
- 2.Deshpande PR, Rajan S, Sudeepthi BL, et al. Patient-reported outcomes: A new era in clinical research. Perspect Clin Res. 2011;2:137–144. doi: 10.4103/2229-3485.86879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cetti R, Christensen SE, Ejsted R, et al. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791–799. doi: 10.1177/036354659302100606. [DOI] [PubMed] [Google Scholar]
- 4.Haggmark T, Liedberg H, Eriksson E, et al. Calf muscle atrophy and muscle function after non-operative versus operative treatment of Achilles tendon ruptures. Orthopedics. 1986;9:160–164. doi: 10.3928/0147-7447-19860201-06. [DOI] [PubMed] [Google Scholar]
- 5.Fitzpatrick R, Davey C, Buxton MJ, et al. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess. 1998;2:1–74. [PubMed] [Google Scholar]
- 6.Hale SA, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40:35–40. [PMC free article] [PubMed] [Google Scholar]
- 7.Saltzman CL, Domsic RT, Baumhauer JF, et al. Foot and ankle research priority: report from the Research Council of the American Orthopaedic Foot and Ankle Society. Foot Ankle Int. 1997;18:447–448. doi: 10.1177/107110079701800714. [DOI] [PubMed] [Google Scholar]
- 8.Roach KE. Measurement of health outcomes: reliability, validity and responsiveness. Journal of Prosthetics and Orthotics. 2006;18:8. [Google Scholar]
- 9.Martin RL, Irrgang JJ. A survey of self-reported outcome instruments for the foot and ankle. J Orthop Sports Phys Ther. 2007;37:72–84. doi: 10.2519/jospt.2007.2403. [DOI] [PubMed] [Google Scholar]
- 10.Gartland JJ. Orthopaedic clinical research. Deficiencies in experimental design and determinations of outcome. J Bone Joint Surg Am. 1988;70:1357–1364. [PubMed] [Google Scholar]
- 11.Silbernagel KG, Brorsson A, Karlsson J. Assessment and outcome measures. In: Karlsson J, Calder J, van Dijk CN, Maffulli N, Thermann H, editors. Achilles tendon disorders, a comprehensive overview of diagnosis and treatment. DJO Publications; Guildford: 2014. [Google Scholar]
- 12.Nyström B, Holmlund D. Separation of tendon ends after suture of Achilles tendon. Acta Orthop Scand. 1983;54:620–621. doi: 10.3109/17453678308992899. [DOI] [PubMed] [Google Scholar]
- 13.Schepull T, Kvist J, Aspenberg P. Early E-modulus of healing Achilles tendons correlates with late function: Similar results with or without surgery. Scand J Med Sci Sports. 2012;22:18–23. doi: 10.1111/j.1600-0838.2010.01154.x. [DOI] [PubMed] [Google Scholar]
- 14.Olsson N, Karlsson J, Eriksson BI, et al. Ability to perform a single heel-rise is significantly related to patient-reported outcome after Achilles tendon rupture. Scand J Med Sci Sports. 2014;24:152–158. doi: 10.1111/j.1600-0838.2012.01497.x. [DOI] [PubMed] [Google Scholar]
- 15.Silbernagel KG, Steele R, Manal K. Deficits in heel-rise height and Achilles tendon elongation occur in patients recovering from an Achilles tendon rupture. Am J Sports Med. 2012;40:1564–1571. doi: 10.1177/0363546512447926. [DOI] [PubMed] [Google Scholar]
- 16.Suydam SM, Buchanan TS, Manal K, et al. Compensatory muscle activation caused by tendon lengthening post-Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23:868–874. doi: 10.1007/s00167-013-2512-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosso C, Buckland DM, Polzer C, et al. Long-term biomechanical outcomes after Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc. 2015;23:890–898. doi: 10.1007/s00167-013-2726-2. [DOI] [PubMed] [Google Scholar]
- 18.Selvik G. Roentgen stereophotogrammetric analysis. Acta Radiol. 1990;31:113–126. [PubMed] [Google Scholar]
- 19.Möller M, Lind K, Movin T, et al. Calf muscle function after Achilles tendon rupture. A prospective, randomised study comparing surgical and non-surgical treatment. Scand J Med Sci Sports. 2002;12:9–16. doi: 10.1034/j.1600-0838.2002.120103.x. [DOI] [PubMed] [Google Scholar]
- 20.Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute Achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186–2193. doi: 10.1177/0363546510376052. [DOI] [PubMed] [Google Scholar]
- 21.Willis K, Amendola A, Bryant D, et al. Operative versus non-operative treatment of acute Achilles tendon ruptures. A multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92:2767–2775. doi: 10.2106/JBJS.I.01401. [DOI] [PubMed] [Google Scholar]
- 22.Huttunen TT, Kannus P, Rolf C, et al. Acute Achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419–2423. doi: 10.1177/0363546514540599. [DOI] [PubMed] [Google Scholar]
- 23.Suchak AA, Bostick GP, Beaupré LA, et al. The influence of early weight-bearing compared with non-weight-bearing after surgical repair of the Achilles tendon. J Bone Joint Surg Am. 2008;90:1876–1883. doi: 10.2106/JBJS.G.01242. [DOI] [PubMed] [Google Scholar]
- 24.Carmont MR, Silbernagel KG, Nilsson-Helander K, et al. Cross cultural adaptation of the Achilles tendon Total Rupture Score with reliability, validity and responsiveness evaluation. Knee Surg Sports Traumatol Arthrosc. 2013;21:1356–1360. doi: 10.1007/s00167-012-2146-8. [DOI] [PubMed] [Google Scholar]
- 25.Alfredson H, Pietilä T, Jonsson P, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26:360–366. doi: 10.1177/03635465980260030301. [DOI] [PubMed] [Google Scholar]
- 26.Alfredson H, Pietilä T, Ohberg L, et al. Achilles tendinosis and calf muscle strength. The effect of short-term immobilization after surgical treatment. Am J Sports Med. 1998;26:166–171. doi: 10.1177/03635465980260020301. [DOI] [PubMed] [Google Scholar]
- 27.Augustsson J, Thomeé R. Ability of closed and open kinetic chain tests of muscular strength to assess functional performance. Scand J Med Sci Sports. 2000;10:164–168. doi: 10.1034/j.1600-0838.2000.010003164.x. [DOI] [PubMed] [Google Scholar]
- 28.Lunsford BR, Perry J. The standing heel-rise test for ankle plantar flexion: criterion for normal. Phys Ther. 1995;75:694–698. doi: 10.1093/ptj/75.8.694. [DOI] [PubMed] [Google Scholar]
- 29.Silbernagel KG, Nilsson-Helander K, Thomeé R, et al. A new measurement of heel-rise endurance with the ability to detect functional deficits in patients with Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2010;18:258–264. doi: 10.1007/s00167-009-0889-7. [DOI] [PubMed] [Google Scholar]
- 30.Möller M, Lind K, Styf J, et al. The reliability of isokinetic testing of the ankle joint and a heel-raise test for endurance. Knee Surg Sports Traumatol Arthrosc. 2005;13:60–71. doi: 10.1007/s00167-003-0441-0. [DOI] [PubMed] [Google Scholar]
- 31.Silbernagel KG, Gustavsson A, Thomeé R, et al. Evaluation of lower leg function in patients with Achilles tendinopathy. Knee Surg Sports Traumatol Arthrosc. 2006;14:1207–1217. doi: 10.1007/s00167-006-0150-6. [DOI] [PubMed] [Google Scholar]
- 32.Carmont MR, Silbernagel KG, Mathy A, et al. Reliability of Achilles tendon resting angle and calf circumference measurement techniques. Foot Ankle Surg. 2013;19:245–249. doi: 10.1016/j.fas.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Leppilahti J, Lähde S, Forsman K, et al. Relationship between calf muscle size and strength after Achilles rupture repair. Foot Ankle Int. 2000;21:330–335. doi: 10.1177/107110070002100410. [DOI] [PubMed] [Google Scholar]
- 34.Norkin CC, White DJ. Measurement of Joint Motion: a Guide to Goniometry. F.A. Davis; Philadelphia: 2009. [Google Scholar]
- 35.Schepull T, Kvist J, Andersson C, et al. Mechanical properties during healing of Achilles tendon ruptures to predict final outcome: a pilot Roentgen stereophotogrammetric analysis in 10 patients. BMC Musculoskelet Disord. 2007;8:116. doi: 10.1186/1471-2474-8-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Atik OS, BölükbaŞ S, Kanatl U. Does surgical repair of acute Achilles tendon rupture cause structural changes on 15-year follow-up? Eklem Hastalik Cerrahisi. 2011;22:54–55. [PubMed] [Google Scholar]
- 37.Ware JE, Snow KK, Kosinski M, et al. SF-36 Health Survey Manual and Interpretation Guide. The Health Institute; Boston: 1993. [Google Scholar]
- 38.Shultz S, Olszewski A, Ramsey O, et al. A systematic review of outcome tools used to measure lower leg conditions. Int J Sports Phys Ther. 2013;8:838–848. [PMC free article] [PubMed] [Google Scholar]
- 39.Kearney RS, Achten J, Lamb SE, et al. A systematic review of patient-reported outcome measures used to assess Achilles tendon rupture management: what’s being used and should we be using it? Br J Sports Med. 2012;46:1102–1109. doi: 10.1136/bjsports-2011-090497. [DOI] [PubMed] [Google Scholar]
- 40.Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux and lesser toes. Foot and Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 41.Ibrahim T, Beiri A, Azzabi M, et al. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surgery. 2007;46:65–74. doi: 10.1053/j.jfas.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 42.Haddad SL, Coetzee JC, Estok R, et al. Intermediate and long–term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89:1899–1905. doi: 10.2106/JBJS.F.01149. [DOI] [PubMed] [Google Scholar]
- 43.Button G, Pinney S. A meta-analysis of outcome rating scales in foot and ankle surgery: is there a valid, reliable, and responsive system? Foot Ankle Int. 2004;25:521–525. doi: 10.1177/107110070402500802. [DOI] [PubMed] [Google Scholar]
- 44.SooHoo NF, Vyas R, Samimi D. Responsiveness of the Foot Function Index, AOFAS clinical rating systems, and SF-36 after foot and ankle surgery. Foot Ankle Int. 2006;27:930–934. doi: 10.1177/107110070602701111. [DOI] [PubMed] [Google Scholar]
- 45.Nilsson-Helander K, Thomeé R, Silbernagel KG, et al. The Achilles tendon Total Rupture Score (ATRS): development and validation. Am J Sports Med. 2007;35:421–426. doi: 10.1177/0363546506294856. [DOI] [PubMed] [Google Scholar]
- 46.Kearney RS, Achten J, Lamb SE, et al. The Achilles tendon total rupture score: a study of responsiveness, internal consistency and convergent validity on patients with acute Achilles tendon ruptures. Health Qual Life Outcomes. 2012;10:24. doi: 10.1186/1477-7525-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaya Mutlu E, Celik D, Kiliçoglu Ö, et al. The Turkish version of the Achilles tendon Total Rupture Score: cross-cultural adaptation, reliability and validity. Knee Surg Sports Traumatol Arthrosc. 2015;23:2427–2432. doi: 10.1007/s00167-014-3042-1. [DOI] [PubMed] [Google Scholar]
- 48.Leppilahti J, Forsman K, Puranen J, et al. Outcome and prognostic factors of Achilles Rupture repair using a new scoring method. Clin Orthop Relat Res. 1998;(346):152–161. [PubMed] [Google Scholar]
- 49.Kaniki N, Willits K, Mohtadi NG, et al. A retrospective comparative study with historical control to determine the effectiveness of platelet-rich plasma as part of nonoperative treatment of acute Achilles tendon rupture. Arthroscopy. 2014;30:1139–1145. doi: 10.1016/j.arthro.2014.04.086. [DOI] [PubMed] [Google Scholar]
- 50.Bevoni R, Angelini A, D’Apote G, et al. Long term results of acute Achilles repair with triple-bundle technique and early rehabilitation protocol. Injury. 2014;45:1268–1274. doi: 10.1016/j.injury.2014.04.028. [DOI] [PubMed] [Google Scholar]
- 51.Martin RL, Irrgang JJ, Burdett RG, et al. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26:968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]