Abstract
Introduction
Adolescence and emergent adulthood are periods of peak prevalence for substance use that pose risks for short- and long-term health harm, particularly for youth with chronic medical conditions (YCMC) who are transitioning from adolescence to adulthood. As there have been no nationally representative studies of substance use during this period for these medically vulnerable youth, the authors sought to examine onset and intensification of these behaviors for a national sample of youth with and without chronic conditions.
Methods
Longitudinal data are from 2,719 youth between the ages of 12 and 26 years interviewed from 2002 to 2011 for the Panel Study of Income Dynamics, Child Development, and Transition to Adulthood Supplements, a nationally representative, population-based survey. Multivariate generalized linear mixed models were used to estimate patterns of alcohol, tobacco, and marijuana use during adolescence and emergent adulthood for youth with and without chronic conditions, adjusting for potential confounders.
Results
Overall, 68.8%, 44.3%, and 47.8% of youth reported ever trying alcohol, tobacco, and marijuana, respectively. Among users, 42.2%, 73.4%, and 50.3% of youth reported binge drinking, regular cigarette use, and recent marijuana use, respectively. YCMC were more likely to engage in any and heavier substance use; transition years and early adulthood were periods of peak risk for YCMC compared with their healthy peers.
Conclusions
Substance use among YCMC during adolescence and emergent adulthood is a substantial concern. Increased prevention and case detection are in order to address these behaviors and promote optimal health outcomes for medically vulnerable youth.
Introduction
Adolescence and emergent adulthood are periods of peak risk for onset and intensification of substance use behaviors that pose risks for short- and long-term health harm.1–6 Although substance use behaviors comprise health risks for all youth, these behaviors may uniquely undermine health status and disease management of youth with chronic medical conditions (YCMC), such as diabetes, asthma, and heart disease, and directly cause physiologic harm.7–14 For YCMC, alcohol may negatively interact with over-the-counter and prescription medications,15 and alcohol and other substance use may impact treatment adherence: A recent investigation found that the risk for medication non-adherence among YCMC who drink compared with those who do not was nearly double.16 Moreover, substance use carries risks for poor sleep, unhealthy diet, and unprotected sex with attendant risks from sexually transmitted disease and pregnancy,17–19 particularly devastating for youth taking immune-suppressing or teratogenic medications. Both substance use and chronic disease impose heavy morbidity burdens on the unfolding lives of young people, including during periods of added vulnerability when they are transitioning care.20 Hence, intervening early to detect and deter the negative compounding influence of these behaviors on the health and well-being of adolescents and young adults may be especially important.
Although many chronic diseases have roots in substance use,21 to date, there have been no nationally representative, longitudinal studies of substance use conducted among youth who already have a chronic disease. The authors sought to estimate incidence and prevalence of substance use (both lifetime and heavier use) among a national sample of youth with and without chronic conditions as they transition from adolescence to adulthood. Quantification of substance use prevalence among chronically ill and healthy youth and elucidation of differences across groups by behavior and condition have implications for implementation of substance use screening programs, early intervention, and prevention in primary and subspecialty care.8,22–24
Methods
Data Source and Sample
Data are from the Panel Study of Income Dynamics (PSID), a nationally representative, longitudinal household survey.25,26 In 1997, children from birth to age 12 years residing in PSID households were recruited into the Child Development Supplement (CDS); repeat waves of the CDS were administered in 2002–2003 and 2007–2008. CDS participants who graduated or dropped out of high school and were aged ≥18 years were interviewed for the Transition into Adulthood (TA) survey in 2005, 2007, 2009, and 2011.
Respondents were eligible for this study if they were interviewed in the initial 1997 CDS wave and subsequently interviewed in at least one CDS or TA survey between the ages of 12 and 26 years and did not have missing information for any of the primary study measures (N=2,719). As data were already collected and de-identified, this study was exempted from IRB approval.
Measures
Respondents were asked about their experience with alcohol, tobacco, and marijuana; as question content and phrasing varied between the CDS and TA, efforts were made to reconcile responses across questions to construct similar measures for both surveys (Appendix 1). For each substance, measures of lifetime use and heavy/regular/recent use were assessed. Additional details regarding the methods can be found in the technical Appendix.
Lifetime use of alcohol was defined by reports of ever drinking beer/wine/liquor when not with their parents or other adults in their family in the CDS or ever drinking beer/wine/liquor in the TA. “Heavy use” of alcohol was characterized by report of binge drinking, specifically reporting monthly frequency of drinking four (for women)/five (for men) or more drinks in one occasion (CDS or TA), or being “very drunk” in the CDS. Lifetime use of tobacco was defined by the report of ever trying cigarettes in either the CDS or TA. “Regular use” was characterized by report of smoking at least one cigarette every day for 30 days. Lifetime use of marijuana was defined by reports of ever trying marijuana. “Recent use” was characterized by any past-month marijuana use without the consent of a doctor.
Substance use summary variables for incidence and prevalence were constructed separately for each survey administration; respondents completed an average of 3.3 additional assessments after the 1997 CDS administration. Earliest reported age of use or age at survey administration for first report of lifetime use (when reported age of initiation was missing) was used to determine incidence of lifetime use. Period prevalence of heavier use was constructed from point-in-time reports of substance use behavior; estimates for period prevalence were thus conditional on lifetime use.
Chronic conditions were conceptualized as those requiring regular, lifelong medical management with onset in childhood, and identified by report of ever being told by a doctor or other health professional that they had: attention deficit/hyperactivity disorder; asthma; autism; birth defects; breathing problems; cancer; chronic hypertension (reported two or more times); diabetes; digestive problems; emotional or psychological problems; epilepsy; heart conditions; kidney disease; learning disability or developmental delays; migraines; orthopedic conditions; sickle cell anemia; skin disease; hearing, speech, or visual impairments; and other conditions. Youth who did not report any of the aforementioned chronic conditions or reported only acute or episodic conditions (e.g., allergies, jaundice, tonsillitis) were considered to have no chronic conditions. Youth with a reported diagnosis of intellectual disability were excluded.
Age at diagnosis was reported for most conditions but age at first report of each condition was used as a proxy when these data were missing. Youth with onset of a chronic condition after reported initiation of a substance were counted as not having the condition until they were diagnosed. In sensitivity analyses, these youth were excluded and models were re-run; results from the restricted and unrestricted samples were consistent.
Data on child sociodemographic factors included: age in 1997, sex, and race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, non-Hispanic Asian, non-Hispanic other). Several indicators of childhood SES were constructed, including:
whether the mother participated in the Special Supplemental Nutrition Program for Women, Infants, and Children or Aid to Families with Dependent Children programs during pregnancy;
whether or not both parents were present in the household in 1997; and
the highest educational attainment for either parent (less than high school degree/GED, high school degree or GED, some college or vocational school, and college graduate or beyond).
Psychological distress was assessed at each interview using the Kessler 6 (range, 0–24; higher scores indicate greater distress).27
Statistical Analysis
Analyses were conducted using survey procedures from SAS, version 9.3. The SEs were corrected for clustering within strata and the primary sampling unit, and CDS sampling weights were used to account for both attrition and the unequal household selection probabilities from the original PSID sampling frame. Statistical significance was considered at p<0.05.
Summary statistics were generated to describe sample characteristics; chi-square and Kruskall–Wallis tests were used to determine significant differences in sociodemographic characteristics between youth with and without any chronic conditions, and to assess differences in substance use behaviors for youth with and without any chronic conditions. Multivariate generalized linear mixed models with a binomial distribution were used to model lifetime and heavier use of substances; sex, race/ethnicity, Special Supplemental Nutrition Program for Women, Infants, and Children or Aid to Families with Dependent Children participation during pregnancy, parent marital status at baseline, and parental educational attainment were treated as time-invariant covariates whereas chronic condition status, psychological distress, and age were treated as time-varying covariates. As the risk of substance use was not assumed to be constant through adolescence and young adulthood, natural cubic splines (with evenly spaced quintile knots) were utilized to model age; models also included an interaction between the spline for age and a time-varying indicator of chronic condition status to allow the effect of chronic condition status to vary non-linearly across age. Likelihood ratio tests suggested that in all cases the trajectory of substance use behaviors across age was significantly different for YCMC compared with their healthy peers. Average marginal predicted probabilities of substance use were calculated by age and chronic condition status. Models for heavier use of substances were conditional on reported lifetime use.
Results
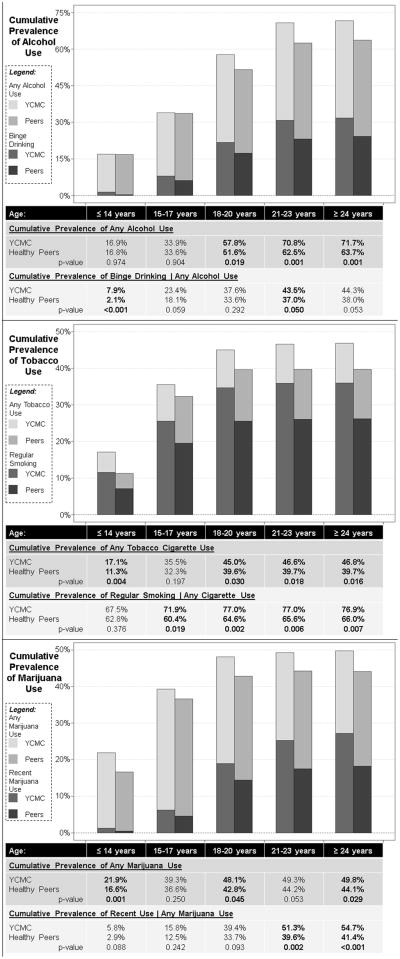
Compared to their healthy peers, YCMC (64.3% of the sample) were older and more likely to be male, have lower SES, and have more psychological distress. Overall, 74.7% of all youth reported some form of substance use, and 47.7% of all youth reported heavier use (Table 1). There was variation in the initiation and prevalence of some substance use behaviors for youth with and without conditions (Figure 1) and across the range of assessed conditions (Table 2, Appendix 2).
Table 1.
Sample Sociodemographic Characteristics by Chronic Condition Status
| Total | Any condition | No condition | p-value | |
|---|---|---|---|---|
| Total N (unweighted) | 2,719 | 1,701 | 1,018 | |
| Total % (weighted) | 64.3% | 35.7% | ||
| Mean age at diagnosis (SD) | - | 9.93 (5.13) | - | - |
| Child’s age in 1997 (SD) | 7.25 (3.30) | 7.39 (3.17) | 6.98 (3.52) | 0.019 |
| Sex | 0.001 | |||
| Male | 49.9% | 52.7% | 44.8% | |
| Female | 50.1% | 47.3% | 55.2% | |
| Race/Ethnicity | 0.121 | |||
| White, non-Hispanic | 57.7% | 58.6% | 56.1% | |
| Black, non-Hispanic | 14.9% | 14.3% | 15.9% | |
| Asian, non-Hispanic | 3.2% | 2.6% | 4.4% | |
| Other, non-Hispanic | 6.9% | 7.7% | 5.4% | |
| Hispanic | 17.3% | 16.8% | 18.2% | |
| Prenatal WIC/AFDC participation | 0.023 | |||
| Yes | 30.6% | 32.5% | 27.1% | |
| No | 69.4% | 67.5% | 72.9% | |
| Parent’s marital status in 1997 | 0.047 | |||
| Two parent household | 76.9% | 75.5% | 79.6% | |
| Single parent household | 23.1% | 24.5% | 20.4% | |
| Parental education | 0.325 | |||
| Less than high school | 12.6% | 11.6% | 14.6% | |
| High school degree | 24.8% | 24.9% | 24.5% | |
| Some college | 22.0% | 22.3% | 21.5% | |
| College grad or more | 40.6% | 41.2% | 39.3% | |
| Psychological distress (SD) | 4.55 (2.73) | 4.88 (2.76) | 3.96 (2.54) | <0.0001 |
| Substance use | ||||
| Lifetime use of any substance | 74.7% | 77.0% | 70.5% | 0.004 |
| Use of one substance | 21.6% | 21.0% | 22.6% | |
| Use of two substances | 20.0% | 20.7% | 18.7% | 0.014 |
| Use of three substances | 33.1% | 35.3% | 29.2% | |
| Heavier use of any substance | 47.7% | 51.7% | 40.4% | <0.001 |
| Heavier use of one substance | 20.4% | 21.2% | 19.1% | |
| Heavier use of two substances | 16.6% | 17.8% | 14.4% | <0.001 |
| Heavier use of three substances | 10.7% | 12.8% | 6.9% | |
| Mean age of initiation (SD) | ||||
| Any alcohol use | 17.49 (3.51) | 17.99 (3.33) | 16.80 (3.65) | <0.001 |
| Any tobacco use | 15.73 (2.69) | 15.88 (2.62) | 15.54 (2.76) | 0.073 |
| Any marijuana use | 15.32 (2.73) | 15.39 (2.67) | 15.24 (2.79) | 0.386 |
Unweighted Ns and weighted percentages and means (SDs) are presented.
Chronic conditions include: attention deficit/hyperactivity disorder; asthma; autism; birth defects; breathing problems; cancer; chronic hypertension; diabetes; digestive problems; emotional or psychological problems; epilepsy; heart conditions; kidney disease; learning disability or developmental delays; migraines; orthopedic conditions; sickle cell anemia; skin disease; hearing, speech, or visual impairments; and other conditions.
WID/AFDC - Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and Aid to Families with Dependent Children (AFDC) programs
Mean Kessler 6 score from administrations during ages 12–26. Higher scores indicate more distress.
Data are from the Panel Study of Income Dynamics, Child Development and Transition to Adulthood Supplements (2002–2011).
Figure 1. Cumulative prevalence of substance use among youth with chronic medical conditions (YCMC) and their healthy peers.
Stacked bar charts show the unadjusted cumulative prevalence of alcohol, tobacco, and marijuana use by age and chronic condition status. Panels depict the unadjusted cumulative prevalence of lifetime use (lighter, taller bars) and heavier/regular/recent use (darker, shorter bars) by age for YCMC and their healthy peers; these estimates and p-values for the comparison between YCMC and their healthy peers are also described in the tables below the charts. (Appendix 3 shows initiation and period prevalence estimates)
Table 2.
Chronic Conditions with the Lowest (≤20th percentile) and Highest (≥80th percentile) Incidence and Prevalence of Substance Use Behaviors
| Pre-adolescence (<14 yrs) | Adolescence (15–17 yrs) | Transition (18–20 yrs) | Early adulthood (21–23 yrs) | Adulthood (24+yrs) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ≤ 20th %ile | ≥ 80th %ile | ≤ 20th %ile | ≥ 80th %ile | ≤ 20th %ile | ≥ 80th %ile | ≤ 20th %ile | ≥ 80th %ile | ≤ 20th %ile | ≥ 80th %ile | |
|
|
||||||||||
|
Lifetime use of alcohol
|
||||||||||
| Initiation of use | Autism Cancer Diabetes Kidney disease | Epilepsy Heart condition Migraines Psychiatric | ADHD/ADD Diabetes Kidney disease Migraines | Autism Cancer Epilepsy Heart condition | Cancer Diabetes Kidney disease Learning disab. | Asthma Autism Epilepsy Migraines | Cancer Heart condition Learning disab. Visual impair. | Autism Hearing Impair. Kidney disease Migraines | Hearing Impair. Heart condition Migraines Visual Impair. | Diabetes Epilepsy Orthopedic Psychiatric |
| Incidence | 1.8% | 22.4% | 17.9% | 40.4% | 33.7% | 48.7% | 54.2% | 91.7% | 6.8% | 53.3% |
|
|
||||||||||
| Cumulative prevalence of use | Autism Cancer Diabetes Kidney disease | Epilepsy Heart condition Migraines Psychiatric | ADHD/ADD Autism Diabetes Kidney disease | Epilepsy Heart condition Hypertension Learning disab. | Autism Diabetes Kidney disease Speech impair. | Epilepsy Heart condition Hypertension Migraines | Autism Learning disab. Speech impair. Visual impair. | Epilepsy Hypertension Kidney disease Migraines | Autism Hearing Impair. Speech impair. Visual impair. | Cancer Hypertension Kidney disease Migraines |
| Prevalence | 1.8% | 22.4% | 28.8% | 40.4% | 50.2% | 65.7% | 67.2% | 81.5% | 65.2% | 84.2% |
|
|
||||||||||
|
Binge drinking alcohol | Ever use of alcohol
|
||||||||||
| Period prevalence of use | Diabetes Heart condition Hypertension Visual impair. | ADHD/ADD Epilepsy Migraines Orthopedic | Cancer Epilepsy Kidney disease Migraines | Autism Diabetes Heart condition Speech impair. | Asthma Autism Kidney disease Visual impair. | Diabetes Hearing Impair. Heart condition Migraines | Cancer Kidney disease Orthopedic Visual impair. | Autism Diabetes Epilepsy Hypertension | Autism Cancer Diabetes Kidney disease | Epilepsy Hearing Impair. Hypertension Speech impair. |
| Prevalence | 0.0% | 15.1% | 15.2% | 46.6% | 26.3% | 47.9% | 23.6% | 47.2% | 7.0% | 37.0% |
|
|
||||||||||
| Cumulative prevalence of use | Diabetes Heart condition Hypertension Visual impair. | ADHD/ADD Epilepsy Migraines Orthopedic | Cancer Kidney disease Migraines Visual impair. | Autism Diabetes Heart condition Speech impair. | Asthma Autism Kidney disease Visual impair. | Diabetes Epilepsy Hearing Impair. Learning disab. | Kidney disease Migraines Orthopedic Visual impair. | Autism Diabetes Hearing Impair. Hypertension | Cancer Kidney disease Migraines Visual impair. | Autism Diabetes Hypertension Psych condition |
| Prevalence | 0.0% | 15.1% | 13.7% | 36.1% | 27.7% | 46.8% | 33.6% | 54.0% | 28.7% | 50.0% |
|
|
||||||||||
|
Lifetime use of tobacco cigarettes
|
||||||||||
| Initiation of use | Autism Cancer Kidney disease Migraines | Epilepsy Learning disab. Other condition Psych condition | Cancer Diabetes Kidney disease Orthopedic | Autism Epilepsy Hypertension Psych condition | Diabetes Epilepsy Heart condition Hypertension | ADHD/ADD Autism Kidney disease Psych condition | Autism Cancer Epilepsy Kidney disease | ADHD/ADD Heart condition Migraines Speech impair. | Learning disab. Orthopedic Psych condition Visual impair. | Asthma Hypertension Other condition Speech impair. |
| Incidence | 3.0% | 23.4% | 16.9% | 37.4% | 10.3% | 30.2% | 0.0% | 9.8% | 0.0% | 0.6% |
|
|
||||||||||
| Cumulative prevalence of use | Autism Cancer Kidney disease Migraines | Epilepsy Learning disab. Other condition Psych condition | Autism Cancer Kidney disease Orthopedic | Epilepsy Hypertension Other condition Psych condition | Autism Diabetes Kidney disease Orthopedic | ADHD/ADD Hypertension Other condition Psych condition | Autism Diabetes Kidney disease Orthopedic | Hypertension Migraines Other condition Psych condition | Autism Diabetes Kidney disease Orthopedic | Hypertension Migraines Other condition Psych condition |
| Prevalence | 3.0% | 23.4% | 27.2% | 45.5% | 37.3% | 55.6% | 38.4% | 57.3% | 38.2% | 57.5% |
|
|
||||||||||
|
Regular use of tobacco cigarettes | Ever use of tobacco cigarettes
|
||||||||||
| Period prevalence of use | Cancer Hearing Impair. Migraines Visual impair. | Asthma Diabetes Other condition Psych condition | Autism Hearing Impair. Heart condition Orthopedic disease | Cancer Diabetes Hypertension Kidney | ADHD/ADD Asthma Cancer Speech impair. | Epilepsy Hearing Impair. Kidney disease Migraines | Epilepsy Hearing Impair. Kidney disease Visual impair. | Autism Cancer Diabetes Migraines | ADHD/AD D Diabetes Heart condition Kidney disease | Cancer Learning disab. Migraines Orthopedic |
| Prevalence | 39.3% | 77.4% | 67.5% | 94.1% | 87.2% | 99.1% | 87.2% | 100.0% | 84.3% | 98.1% |
|
|
||||||||||
| Cumulative prevalence of use | Cancer Hearing Impair. Migraines Visual impair. | Asthma Diabetes Other condition Psych condition | Autism Hearing Impair. Heart condition Visual impair. | Cancer Diabetes Hypertension Kidney disease | Autism Heart condition Orthopedic Visual impair. | Diabetes Hypertension Kidney disease Psych condition | Autism Heart condition Orthopedic Visual impair. | Diabetes Hypertension Kidney disease Psych condition | Autism Cancer Heart condition Visual impair. | Diabetes Hypertension Kidney disease Psych condition |
| Prevalence | 39.3% | 77.4% | 59.6% | 91.5% | 69.5% | 88.6% | 70.2% | 87.8% | 68.3% | 86.6% |
|
|
||||||||||
|
Lifetime use of marijuana
|
||||||||||
| Initiation of use | Autism Cancer Kidney disease Orthopedic | Heart condition Hypertension Other condition Psych condition | Diabetes Kidney disease Orthopedic Visual impair. | ADHD/ADD Epilepsy Hypertension Other condition | Autism Hypertension Kidney disease Visual impair. | Epilepsy Hearing Impair. Heart condition Learning disab. | Autism Cancer Diabetes Epilepsy | ADHD/ADD Heart condition Kidney disease Migraines | ADHD/ADD Asthma Orthopedic Visual impair. | Hypertension Migraines Psych condition Speech impair. |
| Incidence | 10.5% | 32.4% | 21.1% | 34.5% | 2.0% | 24.7% | 0.0% | 8.6% | 0.0% | 11.2% |
|
|
||||||||||
| Cumulative prevalence of use | Autism Cancer Kidney disease Orthopedic | Heart condition Hypertension Other condition Psych condition | Autism Kidney disease Orthopedic Visual impair. | Epilepsy Hypertension Other condition Psych condition | Autism Kidney disease Orthopedic Visual impair. | Cancer Epilepsy Hypertension Psych condition | Autism Orthopedic Speech impair. Visual impair. | Cancer Hypertension Other condition Psych condition | Autism Orthopedic Speech impair. Visual impair. | Epilepsy Hypertension Other condition Psych condition |
| Prevalence | 10.5% | 32.4% | 29.4% | 49.8% | 35.5% | 61.8% | 41.1% | 60.5% | 41.4% | 61.3% |
|
|
||||||||||
|
Recent use of marijuana (without doctor recommendation) | Ever use of marijuana
|
||||||||||
| Period prevalence of use | Diabetes Hearing Impair. Heart condition Hypertension | ADHD/ADD Epilepsy Learning disab. Orthopedic | Asthma Cancer Diabetes Visual impair. | Autism Heart condition Kidney disease Learning disab. | Cancer Hypertension Learning disab. Migraines | Heart condition Kidney disease Orthopedic Visual impair. | Cancer Diabetes Heart condition Kidney disease | ADHD/ADD Autism Other condition Visual impair. | Cancer Diabetes Hearing Impair. Heart condition | ADHD/ADD Autism Epilepsy Kidney disease |
| Prevalence | 0.0% | 11.1% | 13.9% | 38.1% | 25.3% | 46.8% | 26.1% | 43.4% | 16.1% | 53.2% |
|
|
||||||||||
| Cumulative prevalence of use | Diabetes Hearing Impair. Heart condition Hypertension | ADHD/ADD Epilepsy Learning disab. Orthopedic | Cancer Diabetes Other condition Visual impair. | Autism Epilepsy Heart condition Kidney disease | Cancer Diabetes Hypertension Migraines | Autism Heart condition Kidney disease Orthopedic | Cancer Diabetes Hypertension Kidney disease | Asthma Autism Orthopedic Psych condition | Cancer Diabetes Hypertension Visual impair. | Autism Heart condition Kidney disease Psych condition |
| Prevalence | 0.0% | 11.1% | 10.4% | 36.1% | 27.5% | 52.3% | 40.9% | 53.9% | 44.7% | 62.0% |
|
|
||||||||||
Incidence was determined by new reporting of substance use behaviors among those who reported no use in the prior period. Values in bold represent statistically significant differences (p<0.05) comparing youth with a diagnosis of any of the listed conditions to those without.
Prevalence refers to the cumulative or period reporting of use behaviors among those followed through each period. Values in bold represent statistically significant differences (p<0.05) comparing youth with a diagnosis of any of the listed conditions to those without.
Chronic conditions include: attention deficit/hyperactivity disorder (ADHD/ADD); asthma; autism; birth defects; breathing problems; cancer; chronic hypertension; diabetes; digestive problems; emotional or psychological problems; epilepsy; heart conditions; kidney disease; learning disability or developmental delays; migraines; orthopedic conditions; sickle cell anemia; skin disease; hearing, speech, or visual impairments; and other conditions. Conditions that were too rare to yield stable estimates (i.e., birth defects, digestive problems, sickle cell anemia, and skin disease) are not shown.
Data are from the Panel Study of Income Dynamics, Child Development and Transition to Adulthood Supplements (2002–2011).
For all youth, alcohol use initiation rose steadily after pre-adolescence (age ≤14 years) and peaked in early adulthood (age 21–23 years), with 68.8% of youth reporting having ever tried alcohol during the study period (71.7% for YCMC vs 63.7% for healthy youth, p<0.001, Figure 1). Among youth who used alcohol, YCMC had higher rates of binge drinking during pre-adolescence (7.9% vs 2.1% for healthy youth, p<0.001).
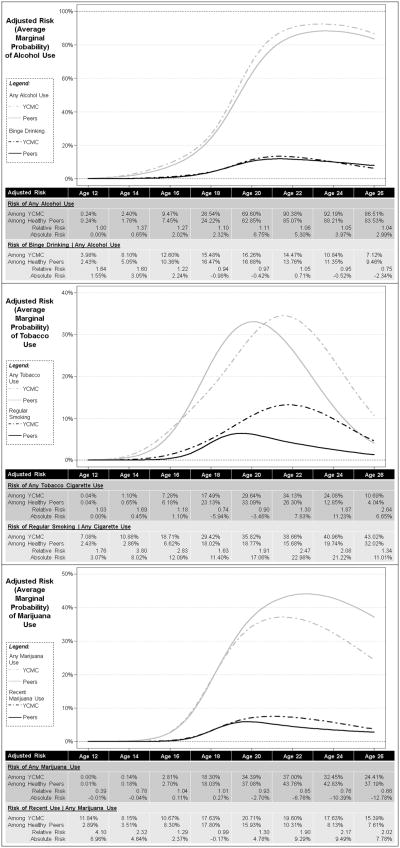
Adjusted generalized linear mixed models identified that the relative risk (RR) of alcohol use for YCMC compared with their peers was greatest at age 14.5 years (3.7% vs 2.7%, RR=1.4) but the greatest difference in absolute risk (AR) occurred at age 20.25 years (74.3% vs 67.3%, AR=6.9%, Figure 2). The RR and AR of binge drinking were greatest for YCMC prior to age 17 years.
Figure 2. Adjusted risk of substance use behaviors by age and chronic conditions.
Figures show the adjusted risk of use of alcohol, tobacco, and marijuana by age and chronic condition status, derived as the average marginal probabilities as predicted by the multivariate generalized linear mixed models. The inset tables shows the adjusted risk at given ages for youth with chronic medical conditions (YCMC) and their healthy peers, as well as the relative risk and absolute risk difference of use for YCMC compared to their peers. Note that for heavier use, risk depicted in the tables has a denominator of lifetime users and thus is larger than risk graphed on the figures, which depicts the overall risk among the entire sample at a given age (derived as [risk of heavier use | any use] * risk of any use).
Tobacco use initiation peaked in adolescence (age 15–17 years) and YCMC exhibited higher rates of tobacco use initiation in pre-adolescence than did their healthy counterparts (17.1% vs 11.3% for healthy youth, p=0.004, Figure 1), with higher rates of any tobacco use among YCMC (46.8% vs 39.7% for healthy youth, p=0.016,). Among smokers, YCMC were consistently more likely to report regular cigarette smoking than their healthy peers.
Adjusted analyses suggested that YCMC experienced a modest elevation in RR around age 14 years (1.1% vs 0.7%, RR=1.7) but that both relative and absolute risk of tobacco use were amplified in early adulthood (Figure 2). Among smokers, YCMC had consistently higher risk for engaging in regular smoking across all ages.
Marijuana use initiation peaked in adolescence and YCMC had higher rates of initiation in pre-adolescence and adulthood but somewhat lower rates in the years between (Figure 1, Appendix 3). Among marijuana users, YCMC were more likely to report past-month marijuana use, especially in early adulthood (51.3% vs 39.6%, p=0.002, Figure 1) and adulthood (54.7% vs 41.4%, p<0.001).
Adjusted models identified that YCMC were approximately as likely as their peers to use marijuana through adolescence (Figure 2), and displayed reduced risk thereafter. Among marijuana users, YCMC displayed the highest RR and AR for recent marijuana use in pre-adolescence (RR=4.1, AR=9.0% at age 12 years) and in early adulthood (RR=2.2, AR=9.5% at age 24 years).
Discussion
Substantial percentages of YCMC reported using alcohol, tobacco, and marijuana during adolescence and emergent adulthood. Both lifetime and heavier use of substances appeared to be similar or elevated for YCMC compared with their healthy counterparts, though some differences were modest. YCMC’s risk of substance use was most consistently elevated during older adolescence and early adulthood, periods when transition from pediatric to adult-focused care is recommended,20 but when youth are most likely to fall out of contact with a healthcare provider.28 Healthcare interactions may help stimulate health-promoting behaviors and improve detection/reduction of risky ones, making it particularly important to develop strategies that support continued healthcare engagement throughout the transition period.
The present estimates are similar to other national surveys of adolescents, including the most recent estimates from the 2013 Youth Risk Behavior Surveillance System, which reports that among 12th graders, 75.6% ever tried alcohol (29.2% binged in the past 30 days), 48.1% ever tried cigarettes (12.2% were ever regular smokers), and 48.6% ever used marijuana (27.7% used marijuana in the past 30 days).29 However, Youth Risk Behavior Surveillance System data suggest that the prevalence of cigarette use has decreased dramatically over the decade in which the present data were collected (from 71.1% in 2001 to 54.5% in 2011) and other nationally representative surveys suggest that alcohol use among U.S. teens may also be declining.30 Some variability in prevalence estimates across existing population based surveys may be expected given that timeframes during which substance use is reported differ (e.g., past 30–day use versus lifetime use, point versus period prevalence) with potential for differential recall associated with these varying time periods. Despite this, substance use behaviors are prevalent among both healthy and medically vulnerable youth in the PSID and comprise a common, concerning, and modifiable behavioral risk.
Findings have important implications for clinical practice. Many providers only sporadically screen young patients for substance use,31 or may not rely on validated screening tools,32 a substantial missed opportunity for detection and intervention of modifiable behavioral risks, which may also contribute to underestimating the scope of and harms associated with substance use.33,34 Increasing provider awareness about substance use among YCMC and advancing use of tailored screening tools that can identify and appropriately triage medically vulnerable youth to services may augment primary and subspecialty care practice and improve outcomes.35,36 However, subspecialty providers who treat YCMC may assume that their patients know about the potential for complications and disease exacerbation resulting from substance use, and may presume that screening is unnecessary or occurring in primary care. The converse may be true for primary care providers interacting with these youth: Fragmentation across providers and absence of coordinated care cloud this picture and may impede effective preventive services.37 Further, as YCMC may be engaging in substance use as a form of self-medication for disease symptoms or comorbid depression or anxiety,12,38–41 integration of mental health services may be critically important for providing comprehensive preventive care. Given that alcohol use among YCMC is associated with medication non-adherence and poor knowledge about interactions between alcohol and medications/laboratory tests,16 implementing screening and preventive action around substance use will likely also be important for improving both preventive and chronic disease care.34,35,42,43
The evolving policy context around adolescent/young adult health is an opportunity to address risk behaviors among chronically ill and healthy youth. Prior to the implementation of the Affordable Care Act, adolescents and young adults had the highest rates of uninsurance and correspondingly low rates in access to care.44 Policy changes, such as dependent coverage expansion and expanded coverage for preventive services such as smoking cessation, together with integration of behavioral health into the medical home, may yield expanded access to care for youth during this time,45–49 and associated spillover effects on health behaviors. Policy reforms hold promise for improving the health of adolescents and young adults and may provide a context for integrating screening and brief intervention into practice, to address the alarmingly high rates of substance use among medically vulnerable youth.34,50 Life course outcomes for chronically ill youth are imperiled without effective disease management,51–53 and substance use may adversely affect self-care and interrupt disease management habits. Early identification and response to ameliorate substance use among YCMC, using a model that appropriately considers this group’s heightened risk for health harm, are critical for protecting health and preventing complications and exacerbations. Efforts to improve screening using standardized and tailored tools are an indispensable part of this picture.54,55
Limitations
This study contributes new information to the extant literature on substance use during adolescence and emerging adulthood, comparing behaviors for youth with and without chronic diseases. Longitudinal data allow examination of trajectories of substance use behaviors and estimation of onset and intensification of three common substances over a decade of follow-up. The nationally representative cohort with high response rates and very low rates of missing items enables generalizable estimates to U.S. adolescents and young adult populations.26 Several important limitations also apply. Parent/self-report of chronic disease diagnosis is not an ideal proxy for clinical report. The high prevalence of conditions among youth in PSID cohorts suggests potential for false positives, albeit misclassification would likely bias findings toward the null. Additionally, prevalence of inheritable chronic conditions in the CDS sample may be inflated, as the CDS allowed the inclusion of up to two children from eligible families. Survey administration began in 2002, prior to the popularization of e-cigarettes or the recent liberalization of marijuana; hence, estimates of these risk behaviors may be conservative. Despite having a relatively large sample, parsimonious models were constructed to preserve power for rare outcomes and these estimates may be subject to residual confounding as a result. Data for this study were collected primarily before health reform. Follow-up work is needed to investigate changes in health behaviors among adolescents and young adults after health reform to determine if expanded access to care translates into quantifiable behavior change.
Conclusions
Although substance use among all U.S. youth remains a major public health problem, findings that YCMC may be more likely than their healthy peers to engage in heavy use of alcohol, tobacco, and marijuana are concerning in light of the potential for disease exacerbation and health harm. Additional work is warranted to understand risk factors for substance use initiation and escalation among this group to guide early intervention and response, including during high-risk periods of healthcare transition. For medically vulnerable youth, expansion of specialty care services to include prevention-oriented education that conveys condition-specific dangers of substance use in combination with screening and case detection may be necessary to optimize physical and mental health outcomes across the life course.
Supplementary Material
Acknowledgments
We wish to acknowledge the helpful comments and suggestions provided by Dr. Sharon Levy, Dr. Elizabeth Harstad, Dr. Scott Hadland, and the anonymous reviewers.
We wish to acknowledge the generous funding support from the Harvard-wide Pediatric Health Services Research Fellowship (Agency for Healthcare Research and Quality 5T32HS00063-21, Principal Investigator [PI]: J. Finkelstein), the Thomas O. Pyle Fellowship (Department of Population Medicine), the National Institute on Alcohol Abuse and Alcoholism (1R01AA021913-01, PIs: E. Weitzman and S. Levy), and the Conrad N. Hilton Foundation (20140273). The collection of data used in this study was partly supported by the NIH (R01 HD069609) and the National Science Foundation (1157698).
Footnotes
LEW contributed to study design and data acquisition, data analysis and interpretation, and writing the article. ERW contributed to study design, interpretation of data, and writing the article.
Earlier versions of this work have been presented at the Pediatric Academic Societies Annual Meeting (San Diego, CA; April 25–28, 2015), National Research Service Award Trainees Research Conference (Minneapolis, MN; June 13, 2015), and American Public Health Association Annual Meeting and Exposition (Chicago, IL; October 31–November 4, 2015).
The authors have no financial relationships or conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hadland SE, Harris SK. Youth marijuana use: state of the science for the practicing clinician. Curr Opin Pediatr. 2014;26(4):420–427. doi: 10.1097/MOP.0000000000000114. http://dx.doi.org/10.1097/MOP.0000000000000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hallfors DD, Waller MW, Bauer D, Ford CA, Halpern CT. Which comes first in adolescence--sex and drugs or depression? Am J Prev Med. 2005;29(3):163–170. doi: 10.1016/j.amepre.2005.06.002. http://dx.doi.org/10.1016/j.amepre.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. J Stud Alcohol Drugs Suppl. 2009;(Supplement)(16):12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson TF, Xuan Z, Lee H, Weitzman ER, Wechsler H. Persistence of heavy drinking and ensuing consequences at heavy drinking colleges. J Stud Alcohol Drugs. 2009;70(5):726–734. doi: 10.15288/jsad.2009.70.726. http://dx.doi.org/10.15288/jsad.2009.70.726. [DOI] [PubMed] [Google Scholar]
- 5.Rao U. Links between depression and substance abuse in adolescents: neurobiological mechanisms. Am J Prev Med. 2006;31(6 Suppl 1):S161–174. doi: 10.1016/j.amepre.2006.07.002. http://dx.doi.org/10.1016/j.amepre.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. J Nerv Ment Dis. 2004;192(4):269–277. doi: 10.1097/01.nmd.0000120885.17362.94. http://dx.doi.org/10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- 7.Gellad WF, Grenard J, McGlynn EA. A Review of Barriers to Medication Adherence: A Framework for Driving Policy Options. Santa Monica, CA: RAND Corporation; 2009. [Google Scholar]
- 8.Gritz ER, Vidrine DJ, Fingeret MC. Smoking cessation: a critical component of medical management in chronic disease populations. Am J Prev Med. 2007;33(6 Suppl):S414–422. doi: 10.1016/j.amepre.2007.09.013. http://dx.doi.org/10.1016/j.amepre.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: A review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269–286. doi: 10.2147/tcrm.s1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lange RA, Hillis LD. Cardiovascular complications of cocaine use. N Engl J Med. 2001;345(5):351–358. doi: 10.1056/NEJM200108023450507. http://dx.doi.org/10.1056/NEJM200108023450507. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz BG, Rezkalla S, Kloner RA. Cardiovascular effects of cocaine. Circulation. 2010;122(24):2558–2569. doi: 10.1161/CIRCULATIONAHA.110.940569. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.940569. [DOI] [PubMed] [Google Scholar]
- 12.Storr M, Devlin S, Kaplan GG, Panaccione R, Andrews CN. Cannabis use provides symptom relief in patients with inflammatory bowel disease but is associated with worse disease prognosis in patients with Crohn’s disease. Inflamm Bowel Dis. 2014;20(3):472–480. doi: 10.1097/01.MIB.0000440982.79036.d6. http://dx.doi.org/10.1097/01.MIB.0000440982.79036.d6. [DOI] [PubMed] [Google Scholar]
- 13.Tetrault JM, Crothers K, Moore BA, Mehra R, Concato J, Fiellin DA. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch Intern Med. 2007;167(3):221–228. doi: 10.1001/archinte.167.3.221. http://dx.doi.org/10.1001/archinte.167.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turner BC, Jenkins E, Kerr D, Sherwin RS, Cavan DA. The effect of evening alcohol consumption on next-morning glucose control in type 1 diabetes. Diabetes Care. 2001;24(11):1888–1893. doi: 10.2337/diacare.24.11.1888. http://dx.doi.org/10.2337/diacare.24.11.1888. [DOI] [PubMed] [Google Scholar]
- 15.Breslow RA, Dong C, White A. Prevalence of alcohol-interactive prescription medication use among current drinkers: United States, 1999 to 2010. Alcohol Clin Exp Res. 2015;39(2):371–379. doi: 10.1111/acer.12633. http://dx.doi.org/10.1111/acer.12633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weitzman ER, Ziemnik RE, Huang Q, Levy S. Alcohol and Marijuana Use and Treatment Non-Adherence Among Medically Vulnerable Youth. Pediatrics. 2015;136(3):450–457. doi: 10.1542/peds.2015-0722. http://dx.doi.org/10.1542/peds.2015-0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pasch KE, Latimer LA, Cance JD, Moe SG, Lytle LA. Longitudinal bi-directional relationships between sleep and youth substance use. J Youth Adolesc. 2012;41(9):1184–1196. doi: 10.1007/s10964-012-9784-5. http://dx.doi.org/10.1007/s10964-012-9784-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Terry-McElrath YM, O’Malley PM, Johnston LD. Energy drinks, soft drinks, and substance use among United States secondary school students. J Addict Med. 2014;8(1):6–13. doi: 10.1097/01.ADM.0000435322.07020.53. http://dx.doi.org/10.1097/01.ADM.0000435322.07020.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wray TB, Celio MA, Kahler CW, et al. Daily co-occurrence of alcohol use and high-risk sexual behavior among heterosexual, heavy drinking emergency department patients. Drug Alcohol Depend. 2015;152:109–115. doi: 10.1016/j.drugalcdep.2015.04.011. http://dx.doi.org/10.1016/j.drugalcdep.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians, Transitions Clinical Report Authoring Group. Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200. doi: 10.1542/peds.2011-0969. http://dx.doi.org/10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 21.Proimos J, Klein JD. Noncommunicable diseases in children and adolescents. Pediatrics. 2012;130(3):379–381. doi: 10.1542/peds.2012-1475. http://dx.doi.org/10.1542/peds.2012-1475. [DOI] [PubMed] [Google Scholar]
- 22.Lubman DI, Hides L, Yucel M, Toumbourou JW. Intervening early to reduce developmentally harmful substance use among youth populations. Med J Aust. 2007;187(7 Suppl):S22–25. doi: 10.5694/j.1326-5377.2007.tb01331.x. [DOI] [PubMed] [Google Scholar]
- 23.Toumbourou JW, Stockwell T, Neighbors C, Marlatt GA, Sturge J, Rehm J. Interventions to reduce harm associated with adolescent substance use. Lancet. 2007;369(9570):1391–1401. doi: 10.1016/S0140-6736(07)60369-9. http://dx.doi.org/10.1016/S0140-6736(07)60369-9. [DOI] [PubMed] [Google Scholar]
- 24.Weitzman ER, Nelson TF. College student binge drinking and the “prevention paradox”: implications for prevention and harm reduction. J Drug Educ. 2004;34(3):247–265. doi: 10.2190/W6L6-G171-M4FT-TWAP. http://dx.doi.org/10.2190/W6L6-G171-M4FT-TWAP. [DOI] [PubMed] [Google Scholar]
- 25.Thabit H, Lubina-Solomon A, Stadler M, et al. Home use of closed-loop insulin delivery for overnight glucose control in adults with type 1 diabetes: a 4-week, multicentre, randomised crossover study. Lancet Diabetes Endocrinol. 2014;2(9):701–709. doi: 10.1016/S2213-8587(14)70114-7. http://dx.doi.org/10.1016/S2213-8587(14)70114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGonagle KA, Schoeni RF, Sastry N, Freedman VA. The Panel Study of Income Dynamics: Overview, Recent Innovations, and Potential for Life Course Research. Longit Life Course Stud. 2012;3(2) doi: 10.14301/llcs.v3i2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. http://dx.doi.org/10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 28.Wisk LE, Finkelstein JA, Sawicki GS, et al. Predictors of timing of transfer from pediatric- to adult-focused primary care. JAMA Pediatrics. 2015;169(6):e150951. doi: 10.1001/jamapediatrics.2015.0951. http://dx.doi.org/10.1001/jamapediatrics.2015.0951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.CDC. [Accessed June 28, 2015];High School Youth Risk Behavior Survey Data. 1991–2013 http://nccd.cdc.gov/youthonline/
- 30.Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE. Use of alcohol, cigarettes, and number of illicit drugs declines among US teens. Ann Arbor, MI: University of Michigan; Dec 16, 2014. [Google Scholar]
- 31.McPherson TL, Hersch RK. Brief substance use screening instruments for primary care settings: a review. J Subst Abuse Treat. 2000;18(2):193–202. doi: 10.1016/s0740-5472(99)00028-8. http://dx.doi.org/10.1016/S0740-5472(99)00028-8. [DOI] [PubMed] [Google Scholar]
- 32.Harris SK, Herr-Zaya K, Weinstein Z, et al. Results of a statewide survey of adolescent substance use screening rates and practices in primary care. Subst Abus. 2012;33(4):321–326. doi: 10.1080/08897077.2011.645950. http://dx.doi.org/10.1080/08897077.2011.645950. [DOI] [PubMed] [Google Scholar]
- 33.Fournier ME, Levy S. Recent trends in adolescent substance use, primary care screening, and updates in treatment options. Curr Opin Pediatr. 2006;18(4):352–358. doi: 10.1097/01.mop.0000236381.33907.9d. http://dx.doi.org/10.1097/01.mop.0000236381.33907.9d. [DOI] [PubMed] [Google Scholar]
- 34.Harris SK, Louis-Jacques J, Knight JR. Screening and brief intervention for alcohol and other abuse. Adolesc Med State Art Rev. 2014;25(1):126–156. [PubMed] [Google Scholar]
- 35.Committee on Substance A. Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128(5):e1330–1340. doi: 10.1542/peds.2011-1754. http://dx.doi.org/10.1542/peds.2011-1754. [DOI] [PubMed] [Google Scholar]
- 36.Sterling S, Valkanoff T, Hinman A, Weisner C. Integrating substance use treatment into adolescent health care. Curr Psychiatry Rep. 2012;14(5):453–461. doi: 10.1007/s11920-012-0304-9. http://dx.doi.org/10.1007/s11920-012-0304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McAllister JW, Presler E, Cooley WC. Practice-based care coordination: a medical home essential. Pediatrics. 2007;120(3):e723–733. doi: 10.1542/peds.2006-1684. http://dx.doi.org/10.1542/peds.2006-1684. [DOI] [PubMed] [Google Scholar]
- 38.Lahat A, Lang A, Ben-Horin S. Impact of cannabis treatment on the quality of life, weight and clinical disease activity in inflammatory bowel disease patients: a pilot prospective study. Digestion. 2012;85(1):1–8. doi: 10.1159/000332079. http://dx.doi.org/10.1159/000332079. [DOI] [PubMed] [Google Scholar]
- 39.Naftali T, Mechulam R, Lev LB, Konikoff FM. Cannabis for inflammatory bowel disease. Digestive Diseases. 2014;32(4):468–474. doi: 10.1159/000358155. http://dx.doi.org/10.1159/000358155. [DOI] [PubMed] [Google Scholar]
- 40.Tashkin DP. Effects of marijuana smoking on the lung. Ann Am Thorac Soc. 2013;10(3):239–247. doi: 10.1513/AnnalsATS.201212-127FR. http://dx.doi.org/10.1513/AnnalsATS.201212-127FR. [DOI] [PubMed] [Google Scholar]
- 41.Wilens TE, Adamson J, Sgambati S, et al. Do individuals with ADHD self-medicate with cigarettes and substances of abuse? Results from a controlled family study of ADHD. Am J Addict. 2007;16(sup1):14–23. doi: 10.1080/10550490601082742. [DOI] [PubMed] [Google Scholar]
- 42.De Micheli D, Fisberg M, Formigoni ML. Study on the effectiveness of brief intervention for alcohol and other drug use directed to adolescents in a primary health care unit. Rev Assoc Med Bras. 2004;50(3):305–313. doi: 10.1590/s0104-42302004000300040. http://dx.doi.org/10.1590/S0104-42302004000300040. [DOI] [PubMed] [Google Scholar]
- 43.Tait RJ, Hulse GK, Robertson SI. Effectiveness of a brief-intervention and continuity of care in enhancing attendance for treatment by adolescent substance users. Drug Alcohol Depend. 2004;74(3):289–296. doi: 10.1016/j.drugalcdep.2004.01.003. http://dx.doi.org/10.1016/j.drugalcdep.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 44.Callahan ST, Cooper WO. Uninsurance and health care access among young adults in the United States. Pediatrics. 2005;116(1):88–95. doi: 10.1542/peds.2004-1449. http://dx.doi.org/10.1542/peds.2004-1449. [DOI] [PubMed] [Google Scholar]
- 45.Akosa Antwi Y, Moriya AS, Simon KI. Access to health insurance and the use of inpatient medical care: evidence from the Affordable Care Act young adult mandate. J Health Econ. 2015;39:171–187. doi: 10.1016/j.jhealeco.2014.11.007. http://dx.doi.org/10.1016/j.jhealeco.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 46.Fox JB, Shaw FE Office of Health System Collaboration OotADfPCDC. Relationship of income and health care coverage to receipt of recommended clinical preventive services by adults - United States, 2011–2012. MMWR Morb Mortal Wkly Rep. 2014;63(31):666–670. [PMC free article] [PubMed] [Google Scholar]
- 47.Lau JS, Adams SH, Park MJ, Boscardin WJ, Irwin CE., Jr Improvement in preventive care of young adults after the affordable care act: the affordable care act is helping. JAMA Pediatrics. 2014;168(12):1101–1106. doi: 10.1001/jamapediatrics.2014.1691. http://dx.doi.org/10.1001/jamapediatrics.2014.1691. [DOI] [PubMed] [Google Scholar]
- 48.Monaghan M. The Affordable Care Act and implications for young adult health. Transl Behav Med. 2014;4(2):170–174. doi: 10.1007/s13142-013-0245-9. http://dx.doi.org/10.1007/s13142-013-0245-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saloner B, Le Cook B. An ACA provision increased treatment for young adults with possible mental illnesses relative to comparison group. Health Aff (Millwood) 2014;33(8):1425–1434. doi: 10.1377/hlthaff.2014.0214. http://dx.doi.org/10.1377/hlthaff.2014.0214. [DOI] [PubMed] [Google Scholar]
- 50.Ridenour TA, Willis D, Bogen DL, et al. Detecting initiation or risk for initiation of substance use before high school during pediatric well-child check-ups. Drug Alcohol Depend. 2015;150:54–62. doi: 10.1016/j.drugalcdep.2015.02.013. http://dx.doi.org/10.1016/j.drugalcdep.2015.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Holmes CS, Chen R, Streisand R, et al. Predictors of youth diabetes care behaviors and metabolic control: a structural equation modeling approach. J Pediatr Psychol. 2006;31(8):770–784. doi: 10.1093/jpepsy/jsj083. http://dx.doi.org/10.1093/jpepsy/jsj083. [DOI] [PubMed] [Google Scholar]
- 52.Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annu Rev Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. http://dx.doi.org/10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- 53.Stinson J, Wilson R, Gill N, Yamada J, Holt J. A systematic review of internet-based self-management interventions for youth with health conditions. J Pediatr Psychol. 2009;34(5):495–510. doi: 10.1093/jpepsy/jsn115. http://dx.doi.org/10.1093/jpepsy/jsn115. [DOI] [PubMed] [Google Scholar]
- 54.Babor TF, Sciamanna CN, Pronk NP. Assessing multiple risk behaviors in primary care. Screening issues and related concepts. Am J Prev Med. 2004;27(2 Suppl):42–53. doi: 10.1016/j.amepre.2004.04.018. http://dx.doi.org/10.1016/j.amepre.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 55.Levy S, Dedeoglu F, Gaffin J, et al. Alcohol Use Risk Among Medically Vulnerable Youth – Validity of the NIAAA Brief Screening Tool. 2015 Under review. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.