Abstract
Background
Prior work has shown that symptoms leading to restrictions in daily activities are common at the end of life. Hospice is a Medicare benefit designed to alleviate distressing symptoms in the last 6 months of life. The effect of hospice on the burden of such symptoms is uncertain.
Methods
From an ongoing cohort study of 754 community-dwelling older persons, aged 70 years or older, we evaluated 241 participants who were admitted to hospice from March 1998 to December 2013. A set of 15 physical and psychological symptoms leading to restricted activity (i.e. cut down on usual activities or spend at least ½ day in bed) were ascertained during monthly telephone interviews in the year before and three months after hospice admission.
Results
The prevalence and mean number of restricting symptoms increased progressively until about 2 months prior to hospice admission, before increasing precipitously to a peak around the time of hospice admission. After the start of hospice, both the prevalence and the mean number of restricting symptoms dropped markedly. For several symptoms deemed most amenable to hospice treatment, including depression and anxiety, the prevalence dropped to levels comparable to or lower than those observed 12 months before the start of hospice. The trends observed in symptom prevalence and mean number of symptoms before and after hospice did not differ appreciably according to hospice admission diagnosis or sex. The median duration of hospice (before death) was only 15 days.
Conclusion
The burden of restricting symptoms increases progressively several months before the start of hospice, peaks around the time of hospice admission, and decreases substantially after the start of hospice. These results, coupled with the short duration of hospice, suggest that earlier referral to hospice may help to alleviate the burden of distressing symptoms at the end-of-life.
Keywords: Aging, Longitudinal study, Hospice, Disability
Towards the end of their lives, many patients point to the alleviation of distressing symptoms as their most pressing need.1,2 A recent Institute of Medicine report, however, found that symptom management at the end of life is often inadequate.3 Despite calls to address this inadequacy,4–6 the problem has gotten worse in the last decade. The prevalence of the most distressing end-of-life symptoms increased between 1998 and 2010 and remains high today.7–9 Furthermore, symptom burden steadily increases during the last year of life.10
One of the most common approaches to ameliorating distressing symptoms is palliative care. Prior studies have shown that palliative care can significantly improve quality of life and even increase survival rates.11–14 At the end of life, hospice, a specific type of palliative care, is often considered. Hospice use has grown substantially in the past decade. However, the median length of stay in hospice has remained very short, at about 2.5 weeks.15 Because a primary objective of hospice is to provide symptom relief in the last 6 months of life,16 this short duration raises concerns about whether hospice is being properly utilized.
While the literature is replete with studies on hospice, relatively little is known about the course of distressing symptoms before and after the start of hospice. Prior studies of distressing symptoms at the end of life have focused on specific subgroups, such as patients with cancer,17 have lacked data on hospice,18 have not had access to detailed longitudinal data prior to hospice,19 or have focused on only a single symptom such as pain.20 In an earlier study,10 we used a longitudinal cohort design to study symptom burden in the last year of life. To our knowledge, comparable longitudinal data do not exist for patients before and after admission to hospice.
In the current study, we set out to evaluate the course of symptoms before and after hospice admission. We were particularly interested in determining whether the occurrence of restricting symptoms (i.e. those that lead to bed rest or cause one to cut down on activities) is reduced after the start of hospice. To address this question, we used data from a unique longitudinal study that includes monthly assessments of restricting symptoms before and after the start of hospice. Given the wide range of symptom severity, we focused on restricting symptoms because they are the most likely to be important for patients and their caregivers. We categorized these symptoms based on clinical judgment into three groups, from most to least amenable to hospice treatment. Given previously reported differences in hospice referral, utilization, and functional decline at the end-of-life,21–24 we also evaluated the monthly occurrence of restricting symptoms according to hospice admission diagnosis and sex as a secondary aim.
METHODS
Study Population
Participants were drawn from an ongoing longitudinal study, previously described in detail,25 involving 754 older persons. Eligible participants were community-dwelling, nondisabled, and 70 years or older at the time of enrollment. Exclusion criteria were substantial cognitive impairment with no available proxy, life expectancy less than 12 months (at the time of eligibility assessment), plans to move out of the area, or inability to speak English. Of the 1002 persons eligible for the study, 754 agreed to participate and were enrolled between March 1998 and October 1999. The research protocol was approved by the Yale Human Investigation Committee.
Analytic Sample
We identified 260 hospice admissions through 2013 using Medicare claims data and review of medical records.26,27 Of these, 12 had previously dropped out of the study and 1 had died prior to their first monthly interview. To permit pre-post comparisons, 6 additional participants were excluded because they did not have at least 6 months of symptom data prior to hospice admission, leaving 241 participants in the analytic sample.
Data Collection
Comprehensive home-based assessments were completed at baseline and subsequently at 18-month intervals, while telephone interviews were completed monthly. During the comprehensive assessments, data were collected on demographic characteristics, depressive symptoms (Center for Epidemiological Studies Depression Scale28 score ≥ 16), cognitive impairment (Folstein Mini-Mental State29 examination score < 24), and the presence of 9 self-reported, physician-diagnosed comorbid conditions: hypertension, myocardial infarction, heart failure, stroke, cancer, diabetes mellitus, hip fracture, arthritis, and chronic lung disease. Body mass index (BMI) was calculated using participants’ self-reported height and weight. For descriptive purposes and to fulfill federal regulations regarding the inclusion of minority participants in studies funded by the US National Institutes of Health, participants were asked to identify their race and ethnicity.
Hospice admission diagnosis codes were obtained from the Medicare claims data.26,27 These diagnoses were classified into 7 categories (Table 1) based on the Centers for Medicare & Medicaid Services (CMS) International Classification of Diseases, 9th Revision (ICD-9) diagnosis codes. For 3 participants without CMS Medicare claims data, the hospice admission diagnoses were inferred from information obtained from death certificates, which were coded by a certified nosologist.
Table 1.
Hospice Admission Diagnoses (N=241)
| Category | No. (%) | ICD-9 Description |
|---|---|---|
| Cancer | 75 (31.1%) | Malignant neoplasm |
| Uncertain or unspecified neoplasm | ||
| Neurodegenerative | 55 (22.8%) | Mental disorders |
| Parkinson’s and other cerebral degenerations | ||
| Cardiovascular | 52 (21.6%) | Heart disease |
| Stroke | ||
| Aneurysm or aortic dissection | ||
| Organ Failure | 36 (14.9%) | Pulmonary diseases |
| Respiratory abnormality not elsewhere classified | ||
| Gastrointestinal and liver disease | ||
| Renal disease | ||
| Frailty/debility | 23 (9.5%) | Adult failure to thrive |
| Debility not otherwise specified |
Assessment of Restricting Symptoms
During the monthly interviews, the occurrence of restricting symptoms was ascertained using a standard protocol that has been previously described.25 First, participants were asked 2 questions related to restricted activity: “Since we last talked (i.e. during the last month), have you stayed in bed for at least half a day due to an illness, injury, or other problem?” and “Since we last talked, have you cut down on your usual activities due to an illness, injury, or other problem?” Second, if participants answered “yes” to either of these questions, they were asked whether they had any of 24 pre-specified symptoms and problems since the last interview.30–33 Third, immediately after each “yes” response to a specific symptom or problem, participants were asked, “Did this cause you to stay in bed for at least half a day or to cut down on your usual activities?” During pilot testing among 20 persons, we found that the test-retest reliability (mean time between assessments, 4.1 days) of this protocol was high, with of κ 0.90 for the presence or absence of restricted activity and κ of 0.75 or greater for the presence or absence of all restricting symptoms.10
Given the aims of the current study, we chose to omit the restricting problems (e.g. change in medications, death of a family member, etc.) and focus on the 15 restricting symptoms: fatigue; dizziness or unsteadiness; difficulty with memory or thinking; swelling in feet or ankles; cold or flu symptoms; musculoskeletal pain; dyspnea; depression; anxiety; poor or decreased vision; arm or leg weakness; nausea, vomiting, or diarrhea (determined through a single question); urinary symptoms; difficulty sleeping; and chest pain or tightness. These symptoms were categorized a priori based on clinical judgment into 3 groups according to how amenable they might be to hospice treatment: most, intermediate, and least.
When participants were too ill or otherwise unable to complete the monthly interviews, proxy data were obtained using a standard protocol.34 We required that proxies were cognitively intact and lived with the participant or saw the participant regularly. Of the 2629 monthly interviews in the current study, 41.8% were completed by a proxy respondent. To determine the accuracy of these reports, we had previously conducted interviews with 20 participants and their designated proxies (separately) for 6 months and compared their responses to questions assessing the occurrence of restricted activity. Concordance was substantial, with κ = 0.66 (95% CI, 0.50–0.83).
Statistical Analysis
Demographic and clinical characteristics of the analytic sample were summarized using information from the comprehensive assessment that immediately preceded the study period (i.e. year prior to hospice). The prevalence of restricting symptoms was calculated by dividing the number of participants with any restricting symptom in a particular month by the total number of participants who completed an interview that month. Similarly, the monthly occurrence of specific restricting symptoms was calculated by dividing the number of participants with that symptom in a specific month by the total number of participants completing the interview. Finally, the mean number of restricting symptoms among participants was calculated. The monthly occurrence of restricting symptoms as well as the mean number of restricting symptoms were plotted in the 12 months prior to hospice admission as well as 3 months after hospice admission. Follow-up beyond 3 months was not included because of the small number of non-decedents. Because restricting symptoms were ascertained “during the past month” and the mean number of days between hospice admission and the first post-admission interview was 14, many of the responses during the first post-admission interview likely refer to symptoms prior to the start of hospice. To evaluate this possibility, we stratified the prevalence and the number of restricting symptoms into three groups based on when the first post-admission interview was completed relative to the start of hospice, i.e. 1–10, 11–20, >20 days.
To account for the high short-term mortality rate after admission to hospice, we also plotted the monthly occurrence of restricting symptoms before and after the start of hospice exclusively for participants who completed at least one post-hospice monthly interview. To address potential selection effects, we repeated these analyses among participants who completed at least three post-hospice monthly interviews. A final set of analyses focused on the monthly occurrence of restricting symptoms according to hospice admission diagnosis and sex.
All analyses were performed using SAS, version 9.4 (SAS Institute).35
RESULTS
As shown in Table 1, the most common admission diagnosis for hospice was cancer. Table 2 provides the characteristics of the analytic sample. The mean age was 88.4 years, with about 30% of the sample being younger than 85. About two-thirds were female and more than a third had less than a high school education. About nine out of ten were non-Hispanic white. Participants had a diverse set of chronic conditions, with an average of 2.6. The median duration of hospice was 15 days (interquartile range, 5–51). Only a minority of participants were admitted to an inpatient hospice facility (n=67 or 27.8%). The others received hospice at home in the community (n=93 or 38.6%) or a nursing home (n=81 or 33.6%).
Table 2.
Characteristics of Participants (N=241)
| Characteristic | Value |
|---|---|
| Age at hospice admission, mean (SD), y | 88.4 (5.7) |
| Age <85 y, No. (%) | 72 (29.9) |
| Non-hispanic White, No.(%) | 216 (89.6) |
| Female sex, No. (%) | 157 (65.2) |
| Education <12y, No. (%) | 90 (37.3) |
| Cognitive impairmenta, No. (%) | 98 (40.7) |
| Body mass index, mean (SD) | 25.3 (5.2) |
| Depressive Symptomsb, No. (%) | 87 (36.1) |
| Individual Chronic Conditions | |
| Diabetes, No. (%) | 59 (24.5) |
| Arthritis, No. (%) | 127 (52.7) |
| Cancer, No. (%) | 71 (29.5) |
| Hypertension, No. (%) | 159 (66.0) |
| Lung Disease, No. (%) | 50 (20.8) |
| Congestive Heart Disease, No. (%) | 36 (14.9) |
| Myocardial Infarction, No. (%) | 59 (24.5) |
| Stroke, No. (%) | 40 (16.6) |
| Hip Fracture, No. (%) | 24 (10.0) |
| No. Chronic conditions, mean (SD) | 2.6 (1.3) |
Notes: Characteristics were assessed at the most proximate comprehensive assessment prior to death.
Folstein Mini-Mental State examination scores less than 24.
Center for Epidemiological Studies Depression Scale scores greater than or equal to 16.
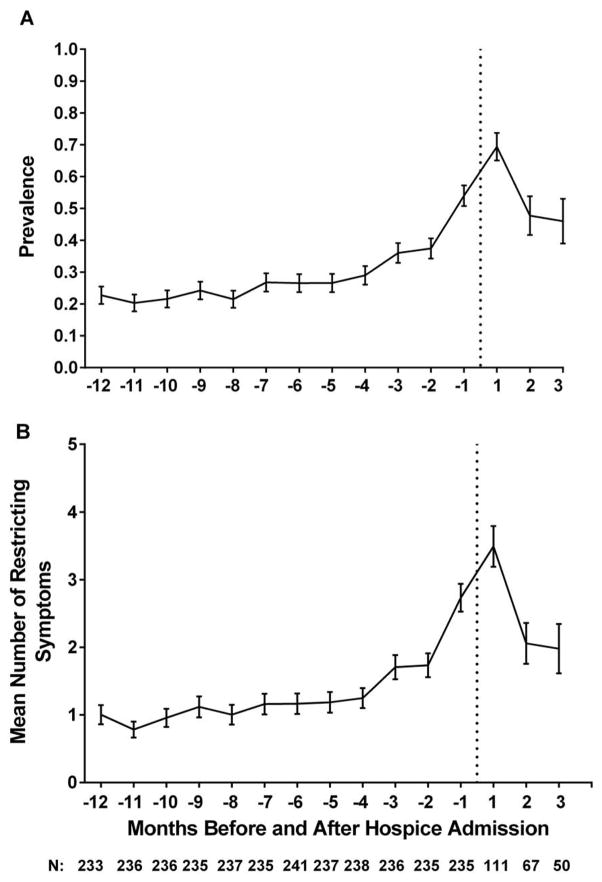
As shown in Figure 1, the prevalence of any restricting symptoms increased slowly until about 2 months prior to hospice admission when it increased precipitously, reaching a peak shortly after the start of hospice. Subsequently, the prevalence of any restricting symptoms dropped markedly from 0.69 to 0.48 before flattening out at 0.46. The pattern for the mean number of restricting symptoms was similar, with a peak of 3.5 restricting symptoms before dropping to 2.1 and flattening out at 2.0. Both the prevalence and number of restricting symptoms decreased as the number of days increased between the time of hospice admission and the time of the first post-hospice interview (Table 3).
Figure 1.
The Occurrence of any Restricting Symptoms (Panel A) and Mean Number of Restricting Symptoms (Panel B) in the 12 Months before and 3 Months after Hospice Admission. Values for the prevalence of symptoms were calculated by dividing the number of participants who reported any restricting symptoms that month by the total number of participants who completed interviews in the month. Error bars in Panel A represent the asymptotic standard error. Errors in Panel B represent the standard error. The dashed vertical line denotes the time of hospice admission. Months before hospice admission are denoted by negative values, while those afterwards are denoted by positive values. The number of participants varies prior to hospice admission because of missing values and decreases after hospice admission because of deaths.
Table 3.
Restricting Symptoms according to Timing of First Post-Hospice Interview (N=111)
| Days after Hospice Admission | Prevalence of Restricting Symptoms | Mean Number of Restricting Symptoms | N |
|---|---|---|---|
| 1–10 | 0.79 | 4.3 | 48 |
| 11–20 | 0.64 | 3.0 | 33 |
| >20 | 0.60 | 2.7 | 30 |
Note: 130 participants died before their first post-hospice interview.
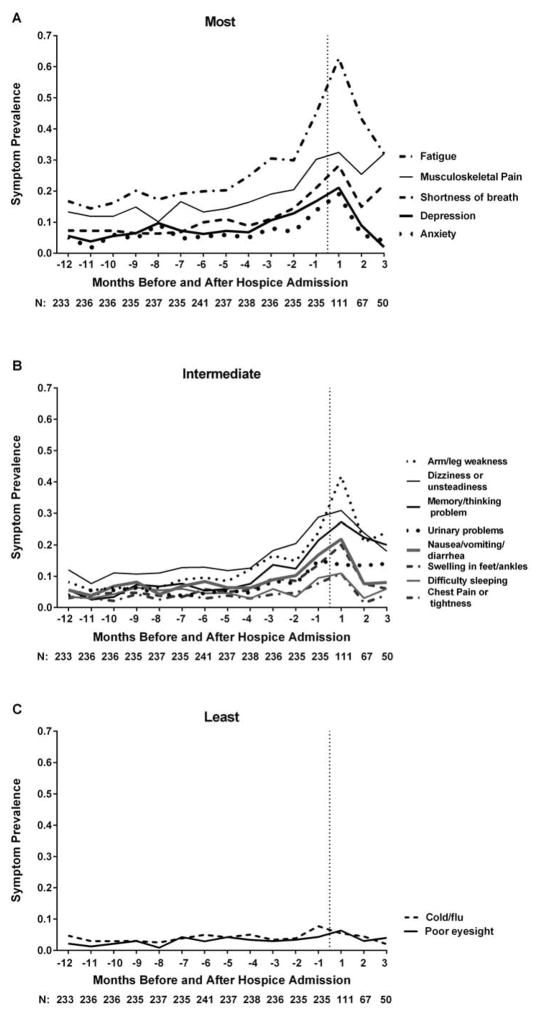
Figure 2 provides the results for each of the restricting symptoms, categorized into three groups, from most to least amenable to hospice treatment. For Panels A and B, the prevalence of most restricting symptoms followed the same general pattern as for any restricting symptoms, with a slow increase, followed by a more pronounced increase shortly before the start of hospice and a subsequent decrease after the start of hospice. These results were most striking for fatigue, depression, anxiety (Figure 2A) and arm/leg weakness (Figure 2B). For several of these symptoms, the prevalence after admission to hospice dropped to levels comparable to those observed 12 months prior to the start of hospice. For some, including depression and anxiety, the prevalence 3 months after hospice admission was lower than 12 months before hospice admission (Figure 2A). In contrast, the prevalence of the two symptoms deemed least amenable to hospice treatment – cold/flu symptoms and poor eyesight – was low throughout the follow-up period, with little change before or after hospice admission (Figure 2C). These results were consistent among participants who had at least one post-hospice follow-up interview (eFigure 1). Additional analyses among participants who had at least three post-hospice follow-up interviews showed similar patterns (results not shown).
Figure 2.
The Occurrence of Specific Restricting Symptoms in the 12 Months before and 3 Months after Hospice Admission. Symptoms were categorized a priori according to how amenable they might be to hospice treatment. Panel A: most; Panel B: intermediate; Panel C: least. Values for the prevalence of symptoms were calculated by dividing the number of participants that reported the particular restricting symptom that month by the total number of participants who completed interviews in the month. Dashed vertical lines denote the time of hospice admission. Months before hospice admission are denoted by negative values, while those afterwards are denoted by positive values. The number of participants varies prior to hospice admission because of missing values and decreases after hospice admission because of deaths.
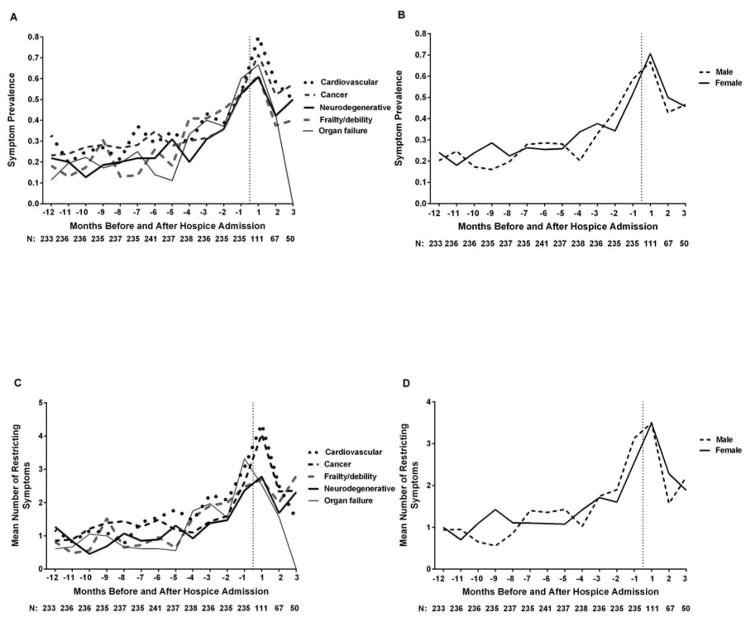
Although there was some month-to-month variability, the trends observed for symptom prevalence and mean number of symptoms before and after hospice did not differ appreciably according to hospice admission diagnosis or sex (Figure 3). For both Figure 2 and Figure 3, the estimates at 3 months post-hospice are less stable than those at earlier time points because they are based on a relatively small proportion of participants surviving through 3 months. For example, the low values at 3 months for organ failure (Figure 3) are likely due to the small number of participants (n=5) who survived to this point from the initial group of 36.
Figure 3.
The Occurrence of any Restricting Symptoms (Panels A and B) and Mean Number of Restricting Symptoms (Panels C and D) in the 12 Months before and 3 Months after Hospice Admission by Hospice Admission Diagnosis and Sex. Values for the prevalence of symptoms were calculated by dividing the number of participants that reported the particular restricting symptom that month by the total number of participants who completed interviews in the month. Dashed vertical line denote the time of hospice admission. Months before hospice admission are denoted by negative values, while those afterwards are denoted by positive values. The number of participants varies prior to hospice admission because of missing values and decreases after hospice admission because of deaths. At 3 months, none of the 5 survivors with organ failure had any restricting symptoms.
DISCUSSION
In this prospective cohort study of older persons, we found that the burden of restricting symptoms increases progressively several months before the start of hospice, peaks around the time of hospice admission, and decreases substantially after the start of hospice. These trends were observed most notably for fatigue, depression, anxiety, arm/leg weakness, and swelling in feet/ankles. As in prior studies,36–38 median survival after hospice admission was only 15 days. When coupled with the short duration of hospice, the high burden of restricting symptoms prior to hospice admission and the reduction of these symptoms after the start of hospice suggest that earlier referral to hospice may help to alleviate the burden of distressing symptoms at the end-of-life.
Our results build on those of prior studies that have shown beneficial effects of palliative care on symptom burden.39–42 Less is generally known about symptom relief after the start of hospice. Three studies have suggested possible alleviation of symptoms by hospice care,17,43,44 although two of these were restricted to patients with cancer,17,44 including one that did not focus solely on hospice.17 In contrast, our study included older persons with a diverse array of hospice admission diagnoses and demonstrated that the observed pattern of restricting symptoms before and after the start of hospice did not differ according to these diagnoses. The availability of detailed information on symptom burden prior to hospice admission is a unique feature of our study.19
While many prior studies of hospice have focused on only a single symptom such as pain,20 we evaluated a wide range of symptoms, allowing us to identify a subset of symptoms, including fatigue, depression, anxiety, arm/leg weakness, and foot/ankle swelling, that appear to respond particularly well to hospice care. Our focus on symptoms leading to restricted activity enhances the clinical relevance of our findings because proper management of these symptoms may substantially improve quality of life while reducing caregiver burden. Although prior studies have demonstrated sex-specific differences in hospice referral and utilization,21,22,24 we found no differences between men and women in the prevalence or mean number of restricting symptoms before and after the start of hospice.
The 1-month assessment intervals did not permit us to precisely identify when the burden of restricting symptoms peaked and subsequently declined. However, we found that both the prevalence and number of restricting symptoms decreased as the number of days increased between the time of hospice admission and the time of the first post-hospice interview, supporting the beneficial effects of hospice on the reduction of restricting symptoms, and suggesting that symptom burden likely peaked near the time of hospice admission.
Our results should be interpreted carefully since only 111 individuals, a large minority of participants, survived to complete a post-hospice interview. However, the results were unchanged when the analyses were limited to participants who completed the first post-hospice interview. Similarly, the patterns of restricting symptoms were comparable among the small proportion of participants who completed at least three post-hospice interviews, thereby diminishing the possibility of a selective survival effect. Although causality can be suggested but not proven by a cohort study, prior research has shown a marked and unperturbed increase in symptom burden in the last year of life in the absence of hospice.10
A limitation of the current study is that information was not available on the use of palliative care before the start of hospice. Based on its demonstrated benefits,39–42 palliative care should have reduced the prevalence and number of restricting symptoms prior to the start of hospice, suggesting that our results might be conservative. Because our study participants were members of a single health plan in a small urban area in the US, our results may not be generalizable to older persons in other settings. However, the demographic characteristics of our cohort at the time of enrollment reflected those of older persons in New Haven County, Connecticut, which were similar to the characteristics of the US population as a whole, with the exception of race or ethnic group.45 The generalizability of our results is further enhanced by our high participation, which was greater than 75%. Although a substantial minority of our interviews were completed by proxies, we have previously demonstrated a high concordance between our proxy and participant reports for restricted activity.10
In summary, we found that the burden of restricting symptoms at the end of life decreases significantly after the start of hospice for older men and women, irrespective of hospice admission diagnosis. These results, coupled with the short duration of hospice, suggest that earlier referral to hospice may help to alleviate the burden of distressing symptoms at the end-of-life.
Supplementary Material
The burden of restricting symptoms at the end of life decreases significantly after the start of hospice, irrespective of hospice admission diagnosis.
Median survival after hospice admission is very short.
Earlier referral to hospice may help to alleviate the burden of distressing symptoms at the end-of-life.
Acknowledgments
The work for this report was funded by a grant from the National Institute on Aging (R37AG17560). The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342). Dr. Gill is the recipient of an Academic Leadership Award (K07AG043587) from the National Institute on Aging.
We thank Denise Shepard, BSN, MBA, Andrea Benjamin, BSN, Barbara Foster, and Amy Shelton, MPH, for assistance with data collection; Wanda Carr and Geraldine Hawthorne, BS, for assistance with data entry and management; Peter Charpentier, MPH, for design and development of the study database and participant tracking system; and Joanne McGloin, MDiv, MBA, for leadership and advice as the Project Director.
Footnotes
The authors have no conflicts of interest, and all authors had access to the data and a role in writing the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients’ perspectives. Jama. 1999 Jan 13;281(2):163–168. doi: 10.1001/jama.281.2.163. [DOI] [PubMed] [Google Scholar]
- 2.Stewart AL, Teno J, Patrick DL, Lynn J. The concept of quality of life of dying persons in the context of health care. Journal of pain and symptom management. 1999 Feb;17(2):93–108. doi: 10.1016/s0885-3924(98)00131-6. [DOI] [PubMed] [Google Scholar]
- 3.Committee on Approaching Death: Addressing Key End of Life I, Institute of M. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington (DC): National Academies Press (US); 2015. Copyright 2015 by the National Academy of Sciences. All rights reserved. [PubMed] [Google Scholar]
- 4.Patrick DL, Ferketich SL, Frame PS, et al. National Institutes of Health State-of-the-Science Conference Statement: Symptom management in cancer: pain, depression, and fatigue, July 15–17, 2002. Journal of the National Cancer Institute. Monographs. 2004;(32):9–16. doi: 10.1093/jncimonographs/djg014. [DOI] [PubMed] [Google Scholar]
- 5.Coyle N, Adelhardt J, Foley KM, Portenoy RK. Character of terminal illness in the advanced cancer patient: pain and other symptoms during the last four weeks of life. Journal of pain and symptom management. 1990 Apr;5(2):83–93. doi: 10.1016/s0885-3924(05)80021-1. [DOI] [PubMed] [Google Scholar]
- 6.Bennett SJ, Cordes DK, Westmoreland G, Castro R, Donnelly E. Self-care strategies for symptom management in patients with chronic heart failure. Nursing research. 2000 May-Jun;49(3):139–145. doi: 10.1097/00006199-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Teno JM, Freedman VA, Kasper JD, Gozalo P, Mor V. Is Care for the Dying Improving in the United States? Journal of palliative medicine. 2015 Apr 29; doi: 10.1089/jpm.2015.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walling AM, Asch SM, Lorenz KA, et al. The quality of care provided to hospitalized patients at the end of life. Archives of internal medicine. 2010 Jun 28;170(12):1057–1063. doi: 10.1001/archinternmed.2010.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Annals of internal medicine. 2015 Feb 3;162(3):175–183. doi: 10.7326/M13-1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaudhry SI, Murphy TE, Gahbauer E, Sussman LS, Allore HG, Gill TM. Restricting symptoms in the last year of life: a prospective cohort study. JAMA internal medicine. 2013 Sep 9;173(16):1534–1540. doi: 10.1001/jamainternmed.2013.8732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rabow M, Kvale E, Barbour L, et al. Moving upstream: a review of the evidence of the impact of outpatient palliative care. Journal of palliative medicine. 2013 Dec;16(12):1540–1549. doi: 10.1089/jpm.2013.0153. [DOI] [PubMed] [Google Scholar]
- 12.Casarett D, Pickard A, Bailey FA, et al. Do palliative consultations improve patient outcomes? Journal of the American Geriatrics Society. 2008 Apr;56(4):593–599. doi: 10.1111/j.1532-5415.2007.01610.x. [DOI] [PubMed] [Google Scholar]
- 13.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. The New England journal of medicine. 2010 Aug 19;363(8):733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 14.Connor SR, Pyenson B, Fitch K, Spence C, Iwasaki K. Comparing hospice and nonhospice patient survival among patients who die within a three-year window. Journal of pain and symptom management. 2007 Mar;33(3):238–246. doi: 10.1016/j.jpainsymman.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 15.Report to the Congress: Medicare payment policy. Washington, DC: Medicare Payment Advisory Commission; Mar, 2014. [Google Scholar]
- 16.Gazelle G. Understanding hospice--an underutilized option for life’s final chapter. The New England journal of medicine. 2007 Jul 26;357(4):321–324. doi: 10.1056/NEJMp078067. [DOI] [PubMed] [Google Scholar]
- 17.Mercadante S, Casuccio A, Fulfaro F. The course of symptom frequency and intensity in advanced cancer patients followed at home. Journal of pain and symptom management. 2000 Aug;20(2):104–112. doi: 10.1016/s0885-3924(00)00160-3. [DOI] [PubMed] [Google Scholar]
- 18.Desbiens NA, Mueller-Rizner N, Connors AF, Jr, Wenger NS, Lynn J. The symptom burden of seriously ill hospitalized patients. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcome and Risks of Treatment. Journal of pain and symptom management. 1999 Apr;17(4):248–255. doi: 10.1016/s0885-3924(98)00149-3. [DOI] [PubMed] [Google Scholar]
- 19.Kane RL, Wales J, Bernstein L, Leibowitz A, Kaplan S. A randomised controlled trial of hospice care. Lancet (London, England) 1984 Apr 21;1(8382):890–894. doi: 10.1016/s0140-6736(84)91349-7. [DOI] [PubMed] [Google Scholar]
- 20.Owens MR, Simmons B, Gibson PS, Weeks D. A longitudinal study of pain in hospice and pre-hospice patients. The American journal of hospice & palliative care. 2001 Mar-Apr;18(2):124–128. doi: 10.1177/104990910101800211. [DOI] [PubMed] [Google Scholar]
- 21.Diamond EL, Russell D, Kryza-Lacombe M, et al. Rates and risks for late referral to hospice in patients with primary malignant brain tumors. Neuro-oncology. 2015 Aug 9; doi: 10.1093/neuonc/nov156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Obermeyer Z, Powers BW, Makar M, Keating NL, Cutler DM. Physician Characteristics Strongly Predict Patient Enrollment In Hospice. Health affairs. 2015 Jun;34(6):993–1000. doi: 10.1377/hlthaff.2014.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris P, Wong E, Farrington S, et al. Patterns of functional decline in hospice: what can individuals and their families expect? Journal of the American Geriatrics Society. 2013 Mar;61(3):413–417. doi: 10.1111/jgs.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saito AM, Landrum MB, Neville BA, Ayanian JZ, Weeks JC, Earle CC. Hospice Care and Survival among Elderly Patients with Lung Cancer. Journal of palliative medicine. 2011 Aug;14(8):929–939. doi: 10.1089/jpm.2010.0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Annals of internal medicine. 2001 Sep 4;135(5):313–321. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 26.Gill TM, Murphy TE, Gahbauer EA, Allore HG. The course of disability before and after a serious fall injury. JAMA internal medicine. 2013 Oct 28;173(19):1780–1786. doi: 10.1001/jamainternmed.2013.9063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolinsky FD, Miller TR, An H, et al. Hospital episodes and physician visits: the concordance between self-reports and medicare claims. Medical care. 2007 Apr;45(4):300–307. doi: 10.1097/01.mlr.0000254576.26353.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. Journal of aging and health. 1993 May;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 29.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research. 1975 Nov;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 30.Rakowski W, Julius M, Hickey T, Verbrugge LM, Halter JB. Daily symptoms and behavioral responses. Results of a health diary with older adults. Medical care. 1988 Mar;26(3):278–297. doi: 10.1097/00005650-198803000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Verbrugge LM, Ascione FJ. Exploring the iceberg. Common symptoms and how people care for them. Medical care. 1987 Jun;25(6):539–569. [PubMed] [Google Scholar]
- 32.Brody EM, Kleban MH. Day-to-day mental and physical health symptoms of older people: a report on health logs. The Gerontologist. 1983 Feb;23(1):75–85. doi: 10.1093/geront/23.1.75. [DOI] [PubMed] [Google Scholar]
- 33.Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. Journal of gerontology. 1994 May;49(3):M140–147. doi: 10.1093/geronj/49.3.m140. [DOI] [PubMed] [Google Scholar]
- 34.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. Jama. 2004 Apr 7;291(13):1596–1602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 35.SAS Version 9.3 User’s Manual. Cary, NC: SAS Institute; 2011. [Google Scholar]
- 36.Christakis NA, Iwashyna TJ. Impact of individual and market factors on the timing of initiation of hospice terminal care. Medical care. 2000 May;38(5):528–541. doi: 10.1097/00005650-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Han B, Remsburg RE, McAuley WJ, Keay TJ, Travis SS. National trends in adult hospice use: 1991–1992 to 1999–2000. Health affairs. 2006 May-Jun;25(3):792–799. doi: 10.1377/hlthaff.25.3.792. [DOI] [PubMed] [Google Scholar]
- 38.Haupt BJ. Characteristics of hospice care discharges and their length of service: United States, 2000. Vital and health statistics. Series 13, Data from the National Health Survey. 2003;(154):1–36. [PubMed] [Google Scholar]
- 39.von Gunten CF. Evolution and effectiveness of palliative care. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2012 Apr;20(4):291–297. doi: 10.1097/JGP.0b013e3182436219. [DOI] [PubMed] [Google Scholar]
- 40.Gomes B, Calanzani N, Higginson IJ. Benefits and Costs of Home Palliative Care Compared With Usual Care for Patients With Advanced Illness and Their Family Caregivers. Jama-J Am Med Assoc. 2014 Mar 12;311(10):1060–1061. doi: 10.1001/jama.2014.553. [DOI] [PubMed] [Google Scholar]
- 41.Vollenbroich R, Duroux A, Grasser M, Brandstatter M, Borasio GD, Fuhrer M. Effectiveness of a Pediatric Palliative Home Care Team as Experienced by Parents and Health Care Professionals. Journal of palliative medicine. 2012 Mar;15(3):294–300. doi: 10.1089/jpm.2011.0196. [DOI] [PubMed] [Google Scholar]
- 42.Kelley AS, Morrison RS. Palliative Care for the Seriously Ill. The New England journal of medicine. 2015 Aug 20;373(8):747–755. doi: 10.1056/NEJMra1404684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tierney RM, Horton SM, Hannan TJ, Tierney WM. Relationships between symptom relief, quality of life, and satisfaction with hospice care. Palliative Med. 1998 Sep;12(5):333–344. doi: 10.1191/026921698670933919. [DOI] [PubMed] [Google Scholar]
- 44.MB, Mclllmurray MRW. Evaluation of a new hospice: the relief of symptoms in cancer patients in the first year. Palliative Med. 1989;3(2):135–140. [Google Scholar]
- 45.US Census Bureau. [Accessed July 9, 2013];American FactFinder. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.