Abstract
Objectives
To examine the prevalence of dementia in the absence of a reported dementia diagnosis and whether potentially unsafe activities and living conditions vary as a function of dementia diagnosis status in a nationally representative sample of older adults.
Design
Observational cohort study.
Setting
Community.
Participants
7,609 Medicare beneficiaries age ≥ 65 enrolled in the National Health and Aging Trends Study.
Measurements
Participants were classified into four groups based on self-report of dementia diagnosis, proxy screening interview, and cognitive testing: 1) probable dementia with reported dementia diagnosis (n=457), 2) probable dementia without reported dementia diagnosis (n=581), 3) possible dementia (n=996), or 4) no dementia (n=5,575). We examined potentially unsafe activities (driving, preparing hot meals, managing finances or medications, attending doctor visits alone) and living conditions (falls, living alone, and unmet needs) by dementia status subgroups in stratified analyses and multivariate models, adjusting for sociodemographic factors, medical comorbidities, and physical capacity.
Results
The prevalence of driving (22.9%), preparing hot meals (31%), managing finances (21.9%), managing medications (36.6%), and attending doctor visits alone (20.6%) was lowest in persons with probable dementia. However, among persons with probable dementia, the covariate-adjusted rates of driving, preparing hot meals, managing finances, managing medications, and attending doctor visits alone were significantly higher in those without reported dementia diagnosis than for those with reported diagnosis (all odds ratios ≥ 2.00, p's < 0.01).
Conclusion
Older adults with probable dementia who are not aware of a dementia diagnosis are more likely to report engaging in potentially unsafe behaviors. Understanding the prevalence of potentially unsafe activities and living conditions can help clinicians focus safety screening and counseling in older adults with diagnosed or suspected dementia.
Keywords: safety, dementia, observational study
Introduction
An estimated 5 million people in the United States have dementia, and the prevalence is projected to nearly triple by 2050.1 Dementia can affect any cognitive domain, including executive function, insight, and judgment.2,3 Over time, cognitive decline leads to increasing functional impairment and difficulty with instrumental activities of daily living (IADLs) and basic activities of daily living (ADLs).4,5 The earliest functional impairments occur in higher level IADLs such as driving, cooking, and managing finances or medications.5 In the context of impaired insight and judgment, disabilities in these IADLs may expose persons with dementia (PWD) to potential harm, including risk of physical injury to self or others, property loss or damage, and financial exploitation.6,7 Other conditions such as frequent falls, unmet needs or neglect, and living alone may also pose a risk of harm.6,8-11 Guidelines for dementia management recognize these risks and include a comprehensive assessment of needs and safety evaluation as important aspects of dementia care.12,13 Given that dementia is often unrecognized,14,15 concerns for safety are often insufficiently addressed.16 Even in diagnosed dementia, quality of care, which includes safety assessment and counseling, is often inconsistent and reactive.12,17,18
Dementia-related safety concerns include falls, medication management, financial management, cooking, access to firearms, being left alone, inability to respond to crises, driving, and abuse or neglect.7,12,19,20 Many studies examine these safety concerns in the framework of functional decline,4,5,16 focusing on activities PWD cannot perform independently rather than potentially risky activities PWD continue to perform despite risk of adverse consequences.6,10,21-24 Existing studies on safety in dementia largely focus on a single issue, such as driving, falls, living alone, or unmet needs,6,8,10,21,23,25-28 while activities such as cooking and medication management have been less studied. Most studies have also been conducted in small samples or dementia-specific populations.6-8,10,21,25-27,29 There is currently no data on the prevalence of potentially unsafe activities and living conditions in PWD from a nationally representative sample.
Understanding the prevalence of potentially unsafe activities and living conditions in PWD and characteristics of PWD engaging in these activities is essential to guide and prioritize safety screening and interventions. Understanding whether potentially unsafe activities and living conditions vary according to whether PWD and their families are aware of the diagnosis of dementia may also have implications for the screening and diagnosis of dementia. Our objectives were to (1) quantify the prevalence of dementia without report of dementia diagnosis, (2) determine rates of potentially unsafe activities and living conditions in older adults with cognitive impairment, and (3) examine the association between dementia status and potentially unsafe activities and living conditions.
Methods
Participants and Study Design
The National Health and Aging Trends Study (NHATS) is an ongoing observational study of a nationally representative cohort of Medicare beneficiaries aged 65 and older in the United States.30 In-person interviews were conducted with older adult participants or proxy respondents if the participant was unable to respond. If the participant could respond with help, an assistant could help answer factual questions. A sample of 8,245 participants was enrolled in 2011, with an overall 71% response rate. The present cross-sectional analyses excluded participants who were residents of a nursing home (n=468) or were missing baseline dementia classification data (n=168), resulting in an analytic sample of 7,609 study participants living in the community or other residential care settings (assisted living, continuing care retirement community, or group homes). A proxy responded for 583 participants, and 2,017 self-respondents received help from an assistant during the interview.
Dementia Status
Methods to identify cognitive impairment in NHATS have been developed and validated.31 NHATS dementia classification is based on three types of information: 1) self or proxy report of being told by a doctor that the participant has dementia or Alzheimer's disease, 2) a score indicating probable dementia on the validated AD8 Dementia Screening Interview32,33 administered to proxy respondents, and 3) cognitive test results. Cognitive testing in NHATS consists of evaluating memory (immediate and delayed 10-word recall), orientation (date, month, year, day of the week, President and Vice President), and executive function (clock drawing test). For participants with proxy respondents who did not allow administration of cognitive test items (n=284), report of diagnosis and AD8 scores were used for dementia classification.
Any participant with report of dementia diagnosis was classified as probable dementia. In sample persons with a proxy respondent, persons without reported diagnosis for whom AD8 Dementia Screening Interview responses met criteria for dementia (score ≥ 2 out of 8) were also classified as probable dementia. For remaining participants (self-respondents without reported diagnosis and 79 persons with proxy respondents who had no reported diagnosis, did not meet AD8 criteria, and completed cognitive tests), dementia categorization was based on performance on cognitive tests. Cognitive impairment in each of the three domains tested was defined as score ≤ 1.5 standard deviations below the mean for self-respondents, a cutpoint commonly used to classify cognitive impairment.34 Resulting cutpoints were ≤ 3 for memory (score 0 to 20), ≤ 3 for orientation (score 0 to 8), and ≤ 1 for executive function (score 0 to 5). Participants were classified as probable dementia if they met criteria for impairment in at least two cognitive domains and as possible dementia if they had impairment in one cognitive domain.31 Among participants classified as having probable dementia, individuals were further classified as having probable dementia with or without reported physician diagnosis. Participants not meeting criteria for possible or probable dementia were classified as no dementia.
Potentially Unsafe Activities and Living Conditions
The potentially unsafe activities and living conditions examined in this study were informed by previous studies and guidelines7,12,13,20 and are based on self or proxy reported activities and living conditions over the last month. Caregiving was defined as providing assistance for a person who could not care for him/herself. Driving included any driving in the past month. Participants were classified as preparing hot meals, handling finances, and managing medications if they always or sometimes made hot meals, handled bills, banking, or complex money matters, or kept track of medications by themselves. Participants who reported seeing their regular doctor in the last year were asked whether they were accompanied by another person or whether they went alone to physician visits.
Multiple falls were elicited as more than one fall, slip, or trip in which the participant lost balance and landed on the ground in the past year. Living alone indicates there were no other individuals reported as living in the participant's household. Drawing from prior work,35 unmet ADL needs was defined based on participants' reports that they ever went without eating, bathing, dressing, or toileting due to difficulty performing the task or lack of help. Unmet IADL needs represent whether the participant ever went without laundry, grocery, hot meals, paying bills or made a mistake with medications. Unmet in-home mobility needs refer to not going somewhere within the home/building or staying in bed, and unmet outside mobility needs refer to staying in the home/building, due to difficulty or lack of help. Unmet ADL, IADL, and mobility needs were examined separately, as in a prior study,36 and as an aggregated measure of any unmet need.
In addition to assessing engagement in potentially unsafe activities and living conditions, NHATS also assesses difficulty with activities in the past month. Participants who performed the following activities themselves were asked how much difficulty (none, a little, some, or a lot) they experienced: preparing hot meals, handling finances, managing medications, leaving the home to go outside, getting around inside the home, getting out of bed, laundry, shopping, eating, bathing, toileting, and dressing. We classified difficulty for each activity dichotomously (none versus any difficulty). Participants who drive reported whether they avoided driving at night, alone, on busy roads or highways or in bad weather. Participants who avoided at least one driving situation were classified as having difficulty.
Covariates
Comprehensive questions regarding sociodemographic factors, health status and medical conditions, and physical capacity were included in NHATS. Respondents provided information on participant age, gender, race, marital status, number of living children, education, income, and residence type (private residence, retirement community, or assisted living, continuing care retirement community or group home). They were asked to rate overall health status (poor, fair, good, very good, or excellent) and report chronic medical conditions (myocardial infarction, coronary artery disease, hypertension, arthritis, osteoporosis, diabetes, lung disease, stroke, and cancer). Subjective physical impairment was assessed through report of hearing or vision impairment and other physical symptoms that limit activity, such as pain, shortness of breath, fatigue, or dizziness. Objective physical capacity was measured using the Short Physical Performance Battery (SPPB),37 which included balance stand, walking speed, and chair stand with scores ranging from 0 to 12. Participants unable or ineligible to complete the SPPB were given a score of 0. Higher scores indicate better physical capacity.
Statistical Analysis
Analytic sampling weights accounting for the complex sampling strategy of NHATS and potential nonresponse bias are available for NHATS.38 All inferential analyses were carried out using weighted data. Inferences were based on statistical significance tests using an alpha of 0.05. The chi-square statistic was used to compare proportions and simple linear regression to compare means between dementia status groups for baseline characteristics. The adjusted Wald test was used to examine cognitive test performance by dementia status, with weighted group mean scores compared to the mean score for the reference group (probable dementia with reported dementia diagnosis). The prevalence and reported difficulty of each dichotomous potentially unsafe activity and living condition for participants by dementia status was determined by cross tabulation, with statistically significant differences evaluated using the chi-square statistic.
Multinomial logistic regression models were used to examine the prevalence of each potentially unsafe activity and living condition across dementia status. Odds ratios were examined for participants with probable dementia without reported dementia diagnosis, possible dementia, and no dementia compared to the group classified as probable dementia with reported diagnosis (the common reference group). This model provided pairwise comparisons of each group with the diagnosed dementia group. Unadjusted odds ratios were followed by multivariable logistic regression models to evaluate the adjusted odds ratio of each potentially unsafe activity and living condition after controlling for covariates.
To explore potential effects of inaccurate self-report in dementia, we performed sensitivity analyses on the prevalence and logistic regression models. We excluded 1) participants with probable dementia who responded independently (without proxy or assistant) and rated their memory as very good or excellent on a 5-point Likert scale (n=51), as self-report may be particularly unreliable in this subgroup39 and 2) all participants with probable dementia who responded independently (n=217).
Results
Description of Participants
Descriptive, unweighted baseline characteristics of participants by dementia status are displayed in Table 1. Among 1038 participants classified as having probable dementia, 457 participants (44%) reported a dementia diagnosis (58.9% proxy, 41.1% self-report) and 581 (56%) did not report a dementia diagnosis (31.7% proxy, 68.3% self-report). In the probable dementia group, 8.8% with and 30.5% without reported diagnosis responded independently (without proxy or assistant) compared to 60.6% and 73.5% with possible or no dementia, respectively. Inferential analyses based on weighted data indicated statistically significant differences on all baseline sociodemographic and health measures by dementia status (all p's < .01), with the exception of lung disease and cancer. Participants with probable or possible dementia were more likely to be older, non-white, not married (widowed or never married), less educated, lower income, live in residential care settings, and rate their health as fair or poor compared to participants with no dementia. Participants with probable dementia were more commonly female. Subjective physical impairments related to hearing, vision, pain, or other physical symptoms were highest in the group with probable dementia and reported dementia diagnosis. SPPB scores were lowest in participants with probable dementia, both with and without reported dementia diagnosis.
Table 1. Characteristics of Participants According to Dementia Status (N=7609).
| Characteristic | Probable Dementia | Possible Dementia (N=996) | No Dementia (N=5575) | |
|---|---|---|---|---|
|
| ||||
| Reported Diagnosis (N=457) | No Reported Diagnosis (N=581) | |||
|
|
||||
| Age, n (%) | ||||
| 65-69 | 13 (2.8) | 42 (7.2) | 92 (9.2) | 1262 (22.6) |
| 70-74 | 32 (7) | 52 (9) | 170 (17.1) | 1325 (23.8) |
| 75-79 | 76 (16.6) | 96 (16.5) | 185 (18.6) | 1156 (20.7) |
| 80-84 | 106 (23.2) | 134 (23.1) | 249 (25) | 1016 (18.2) |
| 85-89 | 130 (28.5) | 118 (20.3) | 174 (17.5) | 531 (9.5) |
| 90+ | 100 (21.2) | 139 (23.9) | 126 (12.7) | 285 (5.1) |
| Gender, n (%) | ||||
| Female | 304 (66.5) | 349 (60.1) | 530 (53.2) | 3255 (58.4) |
| Race, n (%) | ||||
| White | 260 (56.9) | 304 (52.3) | 583 (58.5) | 4039 (72.5) |
| Black | 129 (28.2) | 180 (31) | 265 (26.6) | 1088 (19.5) |
| Hispanic | 44 (9.6) | 60 (10.3) | 91 (9.1) | 259 (4.7) |
| Other or >1 | 14 (3.1) | 29 (5) | 44 (4.4) | 138 (2.5) |
| Marital status, n (%) | ||||
| Married | 157 (34.4) | 187 (32.3) | 394 (39.6) | 2909 (52.2) |
| Living with partner | 7 (1.5) | 5 (0.9) | 19 (1.9) | 120 (2.2) |
| Separated/Divorced | 40 (8.8) | 57 (9.8) | 122 (12.3) | 705 (12.7) |
| Widowed | 230 (50.4) | 283 (48.9) | 419 (42.1) | 1646 (29.6) |
| Never Married | 22 (4.8) | 47 (8.1) | 41 (4.1) | 190 (3.4) |
| Number of living children, n (%) | ||||
| 0 | 38 (8.3) | 79 (13.6) | 106 (10.6) | 497 (8.9) |
| 1 | 70 (15.3) | 80 (13.8) | 132 (13.3) | 684 (12.3) |
| 2 | 99 (21.7) | 123 (21.2) | 231 (23.2) | 1412 (25.3) |
| 3 | 78 (17.1) | 112 (19.3) | 194 (19.5) | 1234 (22.1) |
| 4+ | 172 (37.6) | 187 (32.2) | 333 (33.4) | 1748 (31.4) |
| Highest level of education, n (%) | ||||
| < 8th grade | 107 (23.4) | 210 (36.1) | 237 (23.8) | 435 (7.8) |
| 9th-12th grade (no diploma) | 80 (17.5) | 104 (17.9) | 188 (18.9) | 686 (12.3) |
| High school graduate | 126 (27.6) | 130 (22.4) | 244 (24.5) | 1569 (28.1) |
| Some college or trade school | 94 (20.6) | 87 (15) | 183 (18.4) | 1550 (27.8) |
| Bachelor's degree | 29 (6.4) | 34 (5.9) | 83 (8.3) | 717 (12.9) |
| Masters, Professional or Doctoral degree | 21 (4.6) | 16 (2.8) | 61 (6.1) | 618 (11.1) |
| Income, n (%) | ||||
| 0-9,999 | 65 (27) | 87 (31.4) | 133 (25.2) | 358 (11.2) |
| 10,000-24,999 | 105 (43.6) | 131 (47.3) | 207 (39.3) | 926 (28.9) |
| 25,000-49,999 | 48 (19.9) | 44 (15.9) | 113 (21.4) | 879 (27.5) |
| 50,000-99,999 | 15 (6.2) | 13 (4.7) | 51 (9.7) | 714 (22.3) |
| 100,000+ | 8 (3.3) | 2 (0.7) | 23 (4.4) | 325 (10.2) |
| Residence Type, n (%) | ||||
| Private residence | 369 (80.7) | 465 (80) | 842 (84.5) | 4955 (88.8) |
| Retirement community | 29 (6.4) | 50 (8.6) | 81 (8.1) | 410 (7.4) |
| Assisted living, CCRC, or group home | 59 (12.9) | 66 (11.4) | 73 (7.3) | 210 (3.8) |
| Overall health status, n (%) | ||||
| Excellent | 22 (4.8) | 34 (5.9) | 79 (8) | 803 (14.4) |
| Very Good | 72 (15.8) | 95 (16.4) | 222 (22.3) | 1640 (29.4) |
| Good | 129 (28.2) | 172 (29.7) | 312 (31.4) | 1813 (32.5) |
| Fair | 133 (29.1) | 174 (30.1) | 278 (28) | 1022 (18.3) |
| Poor | 101 (22.1) | 104 (18) | 103 (10.4) | 295 (5.3) |
| Chronic diseases, n (%) | ||||
| Myocardial infarction | 101 (22.1) | 112 (19.3) | 200 (20.1) | 751 (13.5) |
| Coronary artery disease | 126 (27.7) | 131 (22.7) | 201 (20.2) | 953 (17.1) |
| Hypertension | 330 (72.4) | 366 (63.3) | 682 (68.5) | 3730 (67) |
| Arthritis | 305 (66.7) | 332 (57.2) | 558 (56.1) | 3053 (54.9) |
| Osteoporosis | 135 (29.6) | 115 (20) | 157 (15.8) | 1152 (20.7) |
| Diabetes | 121 (26.5) | 165 (28.5) | 304 (30.6) | 1335 (24) |
| Lung Disease | 77 (16.9) | 91 (15.7) | 142 (14.3) | 844 (15.2) |
| Stroke | 128 (28) | 111 (19.1) | 144 (14.5) | 509 (9.1) |
| Cancer | 113 (24.7) | 118 (20.3) | 255 (25.6) | 1467 (26.3) |
| Physical Impairment, n (%) | ||||
| Hearing or vision impairment | 187 (40.9) | 195 (33.6) | 171 (17.2) | 521 (9.4) |
| Activity-limiting pain symptoms | 206 (45.4) | 217 (37.5) | 288 (28.9) | 1567 (28.1) |
| Activity-limiting non-pain symptoms | 329 (72) | 354 (60.9) | 470 (47.2) | 2303 (41.3) |
| Short Physical Performance Battery (SPPB)a, mean (SD) | 2.66 (3.49) | 3.41 (3.52) | 6.11 (3.84) | 8.48 (3.36) |
CCRC = continuing care retirement community
SPPB = Short Physical Performance Battery
SD = standard deviation
Score 0 to maximum 12.
Table 2 displays group differences in cognitive testing. On average, participants classified as probable dementia without reported dementia diagnosis who completed cognitive tests (n=511) scored slightly worse on tests of memory and executive function than participants with reported diagnosis who completed cognitive tests (n=319). Orientation scores were similar between these two groups.
Table 2. Cognitive Test Performance by Domain According to Dementia Statusa.
| Probable Dementia | Possible Dementia | No Dementia | ||
|---|---|---|---|---|
|
|
||||
| Cognitive Domain | Reported Diagnosis | No Reported Diagnosis | ||
| Memoryb, mean (95%CI) | 2.99 (2.61 - 3.37) |
1.93 (1.69 - 2.18) |
4.80 (4.45 - 5.14) |
9.18 (9.08 - 9.29) |
| Orientationc, mean (95%CI) | 2.67 (2.34 - 2.99) |
2.93 (2.70 - 3.16)e |
5.06 (4.81 - 5.31) |
6.52 (6.47 - 6.57) |
| Executive functiond, mean (95%CI) | 1.80 (1.63 - 1.96) |
1.50 (1.37 - 1.62)f |
2.43 (2.28 - 2.58) |
3.76 (3.73 - 3.79) |
Weighted data shown.
Weighted P<0.001 compared to reference group (probable dementia with reported diagnosis) except where noted. Calculated with adjusted Wald test.
Unweighted sample n=319 for group with probable dementia with reported diagnosis, n=511 for probable dementia with no reported diagnosis, n=996 for possible dementia, and n=5499 for no dementia.
Score 0 to maximum 20
Score 0 to maximum 8
Score 0 to maximum 5
p=0.13
p=0.005
CI = confidence interval
Prevalence of Potentially Unsafe Activities and Living Conditions
The crude weighted prevalence of each potentially unsafe activity and living condition across dementia status groups is reported in Table 3. Participants with probable dementia were less likely to report providing care to another person (5.8%), driving (22.9%), preparing hot meals (31%), handling finances (21.9%), managing medications (36.6%), and attending physician visits alone (20.6%) compared to persons with possible or no dementia. Participants with probable dementia who did not report a dementia diagnosis were more likely to report engagement in all potentially unsafe activities compared with those who reported a diagnosis.
Table 3. Prevalencea of Potentially Unsafe Activities and Living Conditions Within the Context of Dementia.
| Probable Dementia, column % | Possible Dementia, column % | No Dementia, column % | P valued | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Reported Diagnosis | No Reported Diagnosis | ||||||
|
| |||||||
| Entire Sampleb | Subsamplec | Entire Sampleb | Subsamplec | ||||
| Potentially Unsafe Activities | |||||||
| Caregiving | 3.8 | 3.4 | 7.3 | 6.2 | 12.3 | 21 | <.001 |
| Drives | 16.6 | 11.6 | 27.9 | 22.1 | 59.4 | 84.2 | <.001 |
| Prepares hot meals | 16.8 | 10.8 | 42.2 | 34.1 | 56.8 | 72.4 | <.001 |
| Handles finances | 12.4 | 7.3 | 29.4 | 20.1 | 59.8 | 74.8 | <.001 |
| Manages medications | 21.7 | 14.9 | 49.5 | 40.4 | 78.5 | 92.8 | <.001 |
| Alone during MD visits | 10.3 | 6.8 | 29.2 | 18.9 | 51.6 | 69.9 | <.001 |
|
| |||||||
| Potentially Unsafe Living Conditions | |||||||
| Multiple falls in last year | 40 | 39.1 | 25.3 | 29.7 | 15.7 | 11.2 | <.001 |
| Living alone | 32.2 | 27.1 | 33.4 | 21.3 | 35.8 | 29.1 | .001 |
| Unmet IADL need | 14.9 | 14.1 | 10.8 | 11.1 | 9.3 | 5.1 | <.001 |
| Unmet ADL need | 28.8 | 31 | 16.9 | 20.4 | 7.4 | 3.7 | <.001 |
| Unmet in-home mobility need | 22.9 | 23.3 | 16.6 | 19.4 | 8.9 | 3.9 | <.001 |
| Unmet outside mobility need | 15.2 | 16.2 | 10.9 | 14.2 | 5.2 | 2.1 | <.001 |
| Any unmet need | 50.6 | 53.4 | 36 | 41.5 | 21.9 | 10.6 | <.001 |
No dementia group displayed for comparison.
Prevalence calculated using weighted survey data.
Unweighted N=7609 (n=457 with probable dementia and reported diagnosis, n=581 with probable dementia and no reported diagnosis, n=996 with possible dementia, and n=5575 with no dementia).
Subsample excludes self-respondents with probable dementia who did not have a proxy or assistant present during the interview. Unweighted N=7392 (n=417 with probable dementia and reported diagnosis, n=404 with probable dementia and no reported diagnosis, n=996 with possible dementia, and n=5575 with no dementia).
P-values calculated using chi-square statistic. P-values were the same for both the entire sample and the subsample.
MD = physician
IADL = instrumental activity of daily living
ADL = activity of daily living
Participants classified as having probable dementia with reported diagnosis had the highest rates of multiple falls and unmet IADL, ADL, and mobility needs. While rates were lower in persons who had probable dementia without reported diagnosis, this group had higher prevalence of falls and unmet ADL and mobility needs compared to those with possible or no dementia. The prevalence of living alone was similar across groups. As shown in Table 4, despite no report of dementia diagnosis, participants classified as probable dementia without reported diagnosis had higher rates of reported difficulty for all activities in comparison to participants with possible or no dementia.
Table 4. Reported Difficulty with Ongoing Activities Within the Context of Dementia.
| Probable Dementia, column %a | Possible Dementia, column %a | No Dementia, column %a | ||
|---|---|---|---|---|
|
| ||||
| Reported Diagnosis | No Reported Diagnosis | |||
|
|
||||
| Potentially unsafe activities | ||||
| Driving (n=5090) | 72.7 | 46.9 | 45.1 | 35.7 |
| Preparing meals (n=4916) | 37.8 | 29.3 | 17.8 | 9.7 |
| Handling finances (n=4735) | 35.8 | 23.8 | 11.4 | 6.3 |
| Managing medications (n=5734) | 38.3 | 18.3 | 9.3 | 8.4 |
|
| ||||
| Potentially unsafe living conditions (IADLs, ADLs, and mobility) | ||||
| Laundry (n=4526) | 40.6 | 14.4 | 10.2 | 7.7 |
| Shopping (n=4078) | 53.3 | 25 | 11.9 | 10.4 |
| Eating (n=7540) | 25.6 | 16.2 | 7.7 | 2.3 |
| Bathing (n=7141) | 38.2 | 24.2 | 16.4 | 8.1 |
| Toileting (n=7474) | 32.7 | 20 | 10.4 | 7.1 |
| Dressing (n=7297) | 45.6 | 27.7 | 18.2 | 10.3 |
| In-home mobility (n=7398) | 46.7 | 32.6 | 21.9 | 12 |
| Bed mobility (n=7452) | 45.8 | 32.9 | 23.6 | 15 |
| Outside mobility (n=6896) | 36 | 29.2 | 17.4 | 9.8 |
Reported difficulty defined as a little, some, or a lot of difficulty in performing activity among participants who reported always or sometimes completing activity by him/herself. No dementia group displayed for comparison.
P<.001 for all activities by chi-square statistic
Weighted
IADL = instrumental activity of daily living
ADL = activity of daily living
After adjusting for sociodemographic factors, health status, medical conditions, and physical capacity, the odds of driving, preparing hot meals, managing finances and medications, and attending medical visits alone remained higher in persons who had probable dementia without reported dementia diagnosis in comparison to those with reported diagnosis. These covariate-adjusted effects are depicted in Figure 1A. After adjusting for covariates, the odds of potentially unsafe living conditions, including multiple annual falls, living alone, unmet IADL needs, ADL needs, and mobility needs, was more similar between probable dementia groups (Figure 1B). The odds ratio for unmet IADL needs was no longer statistically significant for any groups.
Figure 1.
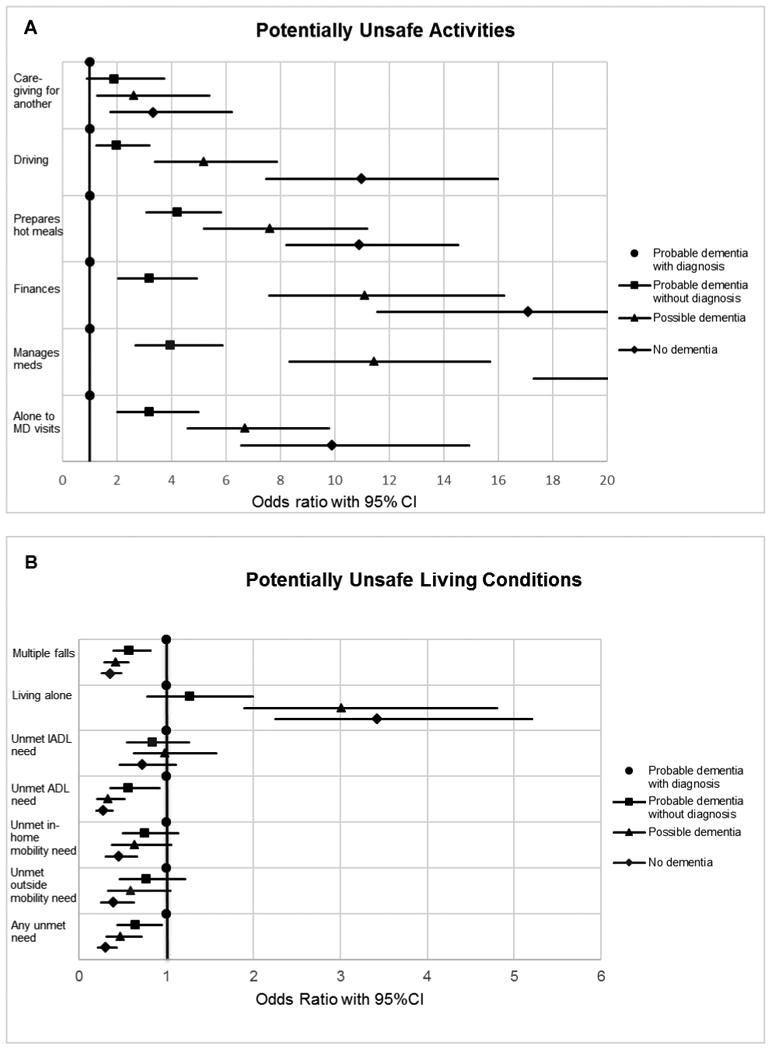
(A & B) Multivariate adjusted odds ratio with 95% CI (confidence interval) for each potentially unsafe activity and living condition according to dementia status. Group with probable dementia with reported diagnosis (circle) was the reference group. Probable dementia without reported diagnosis (square) and possible dementia (triangle) are shown in full for each activity or living condition. The group with no dementia (diamond), shown for comparison, has incomplete data displayed for handling finances (odds ratio 17.1, 95% CI 11.6–25.3) and managing medications (odds ratio 24.1, 95% CI 17.3–33.6) due to large values. Meds = medications, MD = physician, IADL= instrumental activities of daily living, ADL = activities of daily living.
After excluding participants with probable dementia who responded independently and reported very good/excellent memory, prevalence rates and adjusted odds ratios were similar. The proportion in both probable dementia groups reporting potentially unsafe activities and living alone decreased slightly while potentially unsafe living conditions increased. Similar patterns were seen after excluding all participants with probable dementia who responded independently (Table 3). Adjusted odds ratios remained similar but caregiving, unmet ADL needs, and falls became non-significant in participants with probable dementia and no reported diagnosis.
Discussion
This study is the first to examine the prevalence of a range of potentially unsafe activities and living conditions among older adults with dementia, with and without reported physician diagnosis, in a large nationally representative sample. More than half of community-dwelling older adults suspected of having dementia do not report a physician diagnosis of dementia, consistent with prior reports.14-16 Older adults with probable dementia but no reported diagnosis are more likely to report engagement in potentially unsafe activities, including driving, preparing hot meals, managing finances, managing medications, and attending medical visits alone compared to older adults with probable dementia who report a dementia diagnosis. However, older adults with probable dementia but no reported diagnosis are just as likely to live alone and report unmet IADL and mobility needs as their counterparts with reported diagnosis, indicating their needs may be similar. As a group, older adults with probable dementia have lower prevalence of potentially unsafe activities than older adults with possible or no dementia, though the absolute rates of potentially unsafe activities and higher rates of unmet needs are notable from a clinical and public health standpoint.
Previous data on prevalence of driving in dementia is limited though our findings are similar to a previous study in which 20% of drivers over age 80 failed cognitive screening for dementia.40 The prevalence of PWD independently managing medications, finances, or cooking is not known. However, dementia is a predictor of preventable medication-related hospital admission.41 Managing finances is recognized as one of the first IADLs affected in dementia with potential financial mismanagement and exploitation.5,42,43 Potentially unsafe living conditions have been examined more extensively. The prevalence of at least one fall in the past year was 48% in older adults with probable dementia in our study; several studies have found the incidence and prevalence of annual falls to be over 40% among persons with dementia.10,21 Other studies have found similar rates of about one third of PWD living alone.9,44 Those living alone have more unmet needs, but living alone was not associated with hospitalization in PWD belonging to an integrated healthcare system.9 A prospective study of 139 PWD living alone, however, found that about 22% experienced harm requiring emergency services over 1.5 years of follow up.6
As expected with functional decline in dementia, the prevalence of engaging in potentially unsafe activities is lower in older adults with probable dementia and prevalence of potentially unsafe living conditions is higher compared to older adults without cognitive impairment, as adaptation to new and perhaps unrecognized disabilities may be slow. An important finding among older adults with probable dementia is the higher likelihood of engagement in potentially unsafe activities in persons without reported dementia diagnosis even after multivariate adjustment given similar to slightly worse performance on cognitive testing compared to those with reported diagnosis. Rates of unmet needs are similar between these groups.
Our findings highlight the importance of understanding older adults with potentially undiagnosed dementia, who comprise over 50% of older adults with probable dementia. These individuals may be less functionally impaired, creating more diagnostic difficulty and perhaps less safety risk. However, our findings show that this group has potentially significant cognitive impairment and difficulty with activities. Active assessment of difficulty with activities may help identify older adults for whom dementia screening and informant report of symptoms and activities is warranted. It is possible that these individuals have a dementia diagnosis of which they are unaware or lack of acceptance of their condition contributing to higher rates of potentially unsafe behaviors. These undiagnosed individuals may also be able to safely engage in activities and manage living conditions more effectively than older adults who report dementia diagnosis. Further investigation of the consequences of continuing to undertake potentially unsafe activities and living conditions in older adults with both diagnosed and undiagnosed dementia could help motivate greater attention to screening and diagnosis of dementia, as well as efforts to address potential safety hazards in older adults with dementia, including assisting patients and families to accept, understand, and adapt to a dementia diagnosis.
This study has a number of limitations. First, identifying dementia in large population-based studies will involve misclassification in the absence of clinical evaluation and documentation of cognitive decline. Though dementia classification in NHATS was rigorously developed and evaluated, it is limited compared to a comprehensive neurologic examination. Compared to classification by extensive cognitive testing in The Aging, Demographics, and Memory Study,45 the sensitivity of NHATS dementia classification ranges from 65.7% to 85.7% and specificity from 83.7% to 87.2%. There was high concordance of cognitive test criteria with reported diagnosis and AD8 criteria within NHATS, however. Moreover, the estimated prevalence of dementia in NHATS is more conservative than other studies.31 Among participants with probable dementia, 86% received help with an IADL, and 98.7% performing IADLs reported difficulty with an IADL, suggesting that functional impairment, required for dementia diagnosis, may be present. Self-report, particularly in older adults with cognitive impairment, is another limitation.46,47 Among participants with probable dementia, however, 79.1% had a proxy or assistant during the interview. Sensitivity analyses suggest that self-respondents with dementia over-report potentially unsafe activities and under-report unsafe living conditions. However, results were similar when we excluded the most unreliable self-respondents. Excluding all independent respondents with probable dementia likely underestimates prevalence, as responding independently likely signifies independence in other activities. Dementia diagnosis itself may be underreported though undiagnosed dementia rates in our study are similar to other studies.14-16 Categorization of activities in NHATS also does not capture supervision and frequency of activities. Lastly, while these data provide a population-based understanding of exposure to potential safety hazards, dementia diagnosis does not automatically mean an individual is no longer competent to safely engage in these activities.
Given the high prevalence of dementia,1,48 understanding the activities and living conditions of PWD residing in the community is essential to providing care to this group of older adults as well as public health and policy planning. Over 20% of older adults in this sample who meet criteria for probable dementia reported driving, handling finances, managing medications, or attending physician visits alone. Clinicians may be able to better address safety in PWD and underdiagnosis of dementia by inquiring about patient engagement in potentially unsafe activities and difficulties in carrying out activities. Among older adults with probable dementia, persons who do not report a dementia diagnosis have similar odds of unmet needs and more frequently report engaging in potentially unsafe activities despite difficulty with activities and similar to slightly worse performance on cognitive testing. Understanding the activities and needs of older adults with potentially undiagnosed dementia and associated health outcomes may have further implications for dementia screening, diagnosis, and safety.
Acknowledgments
Grant Support: Dr. Amjad was supported by HRSA grant D01HP08789 and the Pearl M. Stetler Research Fund. The National Health and Aging Trends Study is supported by the National Institute on Aging grant U01AG032947.
Sponsors' role: The sponsors had no role in the design, methods, subject recruitment, data collection, or analysis and preparation of the paper.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Study concept and design: Halima Amjad, David L. Roth, Jennifer L. Wolff
Acquisition of subjects and data: n/a
Analysis and interpretation of data: Halima Amjad, David L. Roth, Jennifer L. Wolff
Preparation of manuscript: Halima Amjad
Editing of manuscript: David L. Roth, Sevil Yasar, Quincy M. Samus, Jennifer L. Wolff
References
- 1.Hebert LE, Weuve J, Scherr PA, et al. Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology. 2013;80:1778–1783. doi: 10.1212/WNL.0b013e31828726f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onor ML, Trevisiol M, Negro C, et al. Different perception of cognitive impairment, behavioral disturbances, and functional disabilities between persons with mild cognitive impairment and mild Alzheimer's disease and their caregivers. Am J Alzheimers Dis Other Demen. 2006;21:333–338. doi: 10.1177/1533317506292454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rymer S, Salloway S, Norton L, et al. Impaired awareness, behavior disturbance, and caregiver burden in Alzheimer disease. Alzheimer Dis Assoc Disord. 2002;16:248–253. doi: 10.1097/00002093-200210000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Brown PJ, Devanand DP, Liu X, et al. Alzheimer's Disease Neuroimaging Initiative. Functional impairment in elderly patients with mild cognitive impairment and mild alzheimer disease. Arch Gen Psychiatry. 2011;68:617–626. doi: 10.1001/archgenpsychiatry.2011.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arrighi HM, Gelinas I, McLaughlin TP, et al. Longitudinal changes in functional disability in Alzheimer's disease patients. Int Psychogeriatr. 2013;25:929–937. doi: 10.1017/S1041610212002360. [DOI] [PubMed] [Google Scholar]
- 6.Tierney MC, Charles J, Naglie G, et al. Risk factors for harm in cognitively impaired seniors who live alone: A prospective study. J Am Geriatr Soc. 2004;52:1435–1441. doi: 10.1111/j.0002-8614.2004.52404.x. [DOI] [PubMed] [Google Scholar]
- 7.Walker AE, Livingston G, Cooper CA, et al. Caregivers' experience of risk in dementia: The LASER-AD study. Aging Ment Health. 2006;10:532–538. doi: 10.1080/13607860600637828. [DOI] [PubMed] [Google Scholar]
- 8.Miranda-Castillo C, Woods B, Orrell M. People with dementia living alone: What are their needs and what kind of support are they receiving? Int Psychogeriatr. 2010;22:607–617. doi: 10.1017/S104161021000013X. [DOI] [PubMed] [Google Scholar]
- 9.Ennis SK, Larson EB, Grothaus L, et al. Association of living alone and hospitalization among community-dwelling elders with and without dementia. J Gen Intern Med. 2014;29:1451–1459. doi: 10.1007/s11606-014-2904-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allan LM, Ballard CG, Rowan EN, et al. Incidence and prediction of falls in dementia: A prospective study in older people. PLoS One. 2009;4(5):e5521. doi: 10.1371/journal.pone.0005521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rudolph JL, Zanin NM, Jones RN, et al. Hospitalization in community-dwelling persons with Alzheimer's disease: Frequency and causes. J Am Geriatr Soc. 2010;58:1542–1548. doi: 10.1111/j.1532-5415.2010.02924.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Odenheimer G, Borson S, Sanders AE, et al. Quality improvement in neurology: Dementia management quality measures. J Am Geriatr Soc. 2014;62:558–561. doi: 10.1111/jgs.12630. [DOI] [PubMed] [Google Scholar]
- 13.Feil DG, MacLean C, Sultzer D. Quality indicators for the care of dementia in vulnerable elders. J Am Geriatr Soc. 2007;55(Suppl 2):S293–301. doi: 10.1111/j.1532-5415.2007.01335.x. [DOI] [PubMed] [Google Scholar]
- 14.Bradford A, Kunik ME, Schulz P, et al. Missed and delayed diagnosis of dementia in primary care: Prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009;23:306–314. doi: 10.1097/WAD.0b013e3181a6bebc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Connolly A, Gaehl E, Martin H, et al. Underdiagnosis of dementia in primary care: Variations in the observed prevalence and comparisons to the expected prevalence. Aging Ment Health. 2011;15:978–984. doi: 10.1080/13607863.2011.596805. [DOI] [PubMed] [Google Scholar]
- 16.Wilkins CH, Wilkins KL, Meisel M, et al. Dementia undiagnosed in poor older adults with functional impairment. J Am Geriatr Soc. 2007;55:1771–1776. doi: 10.1111/j.1532-5415.2007.01417.x. [DOI] [PubMed] [Google Scholar]
- 17.Chodosh J, Mittman BS, Connor KI, et al. Caring for patients with dementia: How good is the quality of care? Results from three health systems. J Am Geriatr Soc. 2007;55:1260–1268. doi: 10.1111/j.1532-5415.2007.01249.x. [DOI] [PubMed] [Google Scholar]
- 18.Hinton L, Franz CE, Reddy G, et al. Practice constraints, behavioral problems, and dementia care: Primary care physicians' perspectives. J Gen Intern Med. 2007;22:1487–1492. doi: 10.1007/s11606-007-0317-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Home safety and Alzheimer's. [November 15, 2014];Alzheimer's Association (online) 2014 Available at: http://www.alz.org/care/alzheimers-dementia-home-safety.asp#howdementiaaffects.
- 20.Lach HW, Chang YP. Caregiver perspectives on safety in home dementia care. West J Nurs Res. 2007;29:993–1014. doi: 10.1177/0193945907303098. [DOI] [PubMed] [Google Scholar]
- 21.Horikawa E, Matsui T, Arai H, et al. Risk of falls in Alzheimer's disease: A prospective study. Intern Med. 2005;44:717–721. doi: 10.2169/internalmedicine.44.717. [DOI] [PubMed] [Google Scholar]
- 22.Duchek JM, Carr DB, Hunt L, et al. Longitudinal driving performance in early-stage dementia of the Alzheimer type. J Am Geriatr Soc. 2003;51:1342–1347. doi: 10.1046/j.1532-5415.2003.51481.x. [DOI] [PubMed] [Google Scholar]
- 23.Ott BR, Heindel WC, Papandonatos GD, et al. A longitudinal study of drivers with Alzheimer disease. Neurology. 2008;70:1171–1178. doi: 10.1212/01.wnl.0000294469.27156.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Black BS, Johnston D, Rabins PV, et al. Unmet needs of community-residing persons with dementia and their informal caregivers: Findings from the maximizing independence at home study. J Am Geriatr Soc. 2013;61:2087–2095. doi: 10.1111/jgs.12549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Imamura T, Hirono N, Hashimoto M, et al. Fall-related injuries in dementia with Lewy bodies (DLB) and alzheimer's disease. Eur J Neurol. 2000;7:77–79. doi: 10.1046/j.1468-1331.2000.00021.x. [DOI] [PubMed] [Google Scholar]
- 26.Charles J, Naglie G, Lee J, et al. Self-report measures of well-being predict incident harm due to self-neglect in cognitively impaired seniors who live alone. J Alzheimers Dis. 2014;44:425–430. doi: 10.3233/JAD-141671. [DOI] [PubMed] [Google Scholar]
- 27.Drachman DA, Swearer JM. Driving and Alzheimer's disease: The risk of crashes. Neurology. 1993;43:2448–2456. doi: 10.1212/wnl.43.12.2448. [DOI] [PubMed] [Google Scholar]
- 28.Abrams RC, Lachs M, McAvay G, et al. Predictors of self-neglect in community-dwelling elders. Am J Psychiatry. 2002;159:1724–1730. doi: 10.1176/appi.ajp.159.10.1724. [DOI] [PubMed] [Google Scholar]
- 29.Alden NE, Rabbitts A, Yurt RW. Burn injury in patients with dementia: An impetus for prevention. J Burn Care Rehabil. 2005;26:267–271. [PubMed] [Google Scholar]
- 30.Montaquila J, Freedman V, Edwards B, et al. National Health and Aging Trends Study round 1 sample design and selection. Baltimore: Johns Hopkins University School of Public Health; 2012. NHATS Technical Paper #1. Available at www.nhats.org. [Google Scholar]
- 31.Kasper J, Freedman V, Spillman B. Classification of persons by dementia status in the National Health and Aging Trends Study. Baltimore: Johns Hopkins University School of Public Health; 2013. Technical Paper #5. Available at www.nhats.org. [Google Scholar]
- 32.Galvin JE, Roe CM, Powlishta KK, et al. The AD8: A brief informant interview to detect dementia. Neurology. 2005;65:559–564. doi: 10.1212/01.wnl.0000172958.95282.2a. [DOI] [PubMed] [Google Scholar]
- 33.Galvin JE, Roe CM, Xiong C, et al. Validity and reliability of the AD8 informant interview in dementia. Neurology. 2006;67:1942–1948. doi: 10.1212/01.wnl.0000247042.15547.eb. [DOI] [PubMed] [Google Scholar]
- 34.Morris JC. Revised criteria for mild cognitive impairment may compromise the diagnosis of Alzheimer disease dementia. Arch Neurol. 2012;69:700–708. doi: 10.1001/archneurol.2011.3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allen SM, Mor V. The prevalence and consequences of unmet need. Contrasts between older and younger adults with disability Med Care. 1997;35:1132–1148. doi: 10.1097/00005650-199711000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Allen SM, Piette ER, Mor V. The adverse consequences of unmet need among older persons living in the community: Dual-eligible versus medicare-only beneficiaries. J Gerontol B Psychol Sci Soc Sci. 2014;69(Suppl 1):S51–58. doi: 10.1093/geronb/gbu124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 38.Montaquila J, Freedman V, Spillman B, et al. National Health and Aging Trends Study development of round 1 survey weights. Baltimore: Johns Hopkins University School of Public Health; 2012. Technical Paper #2. Available at www.nhats.org. [Google Scholar]
- 39.Monahan PO, Alder CA, Khan BA, et al. The healthy aging brain care (HABC) monitor: Validation of the patient self-report version of the clinical tool designed to measure and monitor cognitive, functional, and psychological health. Clin Interv Aging. 2014;9:2123–2132. doi: 10.2147/CIA.S64140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stutts JC, Stewart JR, Martell C. Cognitive test performance and crash risk in an older driver population. Accid Anal Prev. 1998;30:337–346. doi: 10.1016/s0001-4575(97)00108-5. [DOI] [PubMed] [Google Scholar]
- 41.Leendertse AJ, Egberts AC, Stoker LJ, et al. HARM Study Group Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med. 2008;168:1890–1896. doi: 10.1001/archinternmed.2008.3. [DOI] [PubMed] [Google Scholar]
- 42.Marson DC. Clinical and ethical aspects of financial capacity in dementia: A commentary. Am J Geriatr Psychiatry. 2013;21:392–390. doi: 10.1097/JGP.0b013e31826682f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martin R, Triebel K, Falola M, et al. A-75 Financial decline in patients with mild cognitive impairment: A six-year longitudinal study. Arch Clin Neuropsychol. 2014;29:530–531. doi: 10.1093/arclin/acy030. [DOI] [PubMed] [Google Scholar]
- 44.Sibley A, MacKnight C, Rockwood K, et al. The effect of the living situation on the severity of dementia at diagnosis. Dement Geriatr Cogn Disord. 2002;13:40–45. doi: 10.1159/000048632. [DOI] [PubMed] [Google Scholar]
- 45.Langa KM, Plassman BL, Wallace RB, et al. The Aging, Demographics, and Memory Study: Study design and methods. Neuroepidemiology. 2005;25:181–191. doi: 10.1159/000087448. [DOI] [PubMed] [Google Scholar]
- 46.Wadley VG, Harrell LE, Marson DC. Self- and informant report of financial abilities in patients with Alzheimer's disease: Reliable and valid? J Am Geriatr Soc. 2003;51:1621–1626. doi: 10.1046/j.1532-5415.2003.51514.x. [DOI] [PubMed] [Google Scholar]
- 47.Graham DP, Kunik ME, Doody R, et al. Self-reported awareness of performance in dementia. Brain Res Cogn Brain Res. 2005;25:144–152. doi: 10.1016/j.cogbrainres.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 48.Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: The Aging, Demographics, and Memory Study. Neuroepidemiology. 2007;29:125–132. doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]


