Abstract
To better understand the antibacterial activity of S-649266 against carbapenemase producers, its stability against clinically relevant carbapenemases was investigated. The catalytic efficiencies (kcat/Km) of IMP-1, VIM-2, and L1 for S-649266 were 0.0048, 0.0050, and 0.024 μM−1 s−1, respectively, which were more than 260-fold lower than that for meropenem. Only slight hydrolysis of S-649266 against KPC-3 was observed. NDM-1 hydrolyzed meropenem 3-fold faster than S-649266 at 200 μM.
TEXT
In the 2000s, there has been a striking increase of clinically important carbapenemases, including classes A, B, and D, which can hydrolyze both carbapenems and cephalosporins (1). The carbapenemases of the class A β-lactamase KPC and class B metallo-β-lactamases (MBLs) IMP, VIM, and NDM are disseminated interspecies by mobile elements, which has led to the spread of these carbapenemases worldwide (2–4). The carbapenem-hydrolyzing class D β-lactamases (CHDLs) OXA-23, OXA-24, OXA-51, and OXA-58 have been found in Acinetobacter species worldwide (5, 6). These CHDLs show weak hydrolysis activity against carbapenems, while increased expression by the ISAba gene insertion sequence can mediate carbapenem resistance. The frequent occurrence of multidrug-resistant (MDR) phenotypes of these carbapenemase-producing isolates due to other concurrent resistance genes poses global challenges due to the limited number of treatment options (2–4).
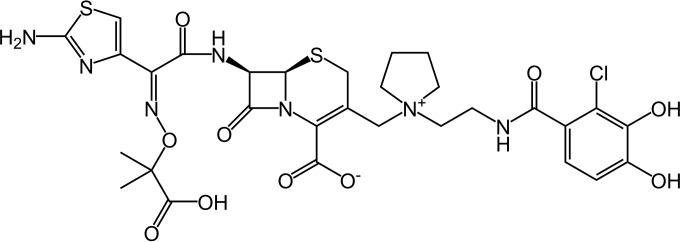
S-649266 is a novel parenteral siderophore cephalosporin (Fig. 1) which employs a “Trojan horse” strategy using the active transport of S-649266 into bacterial cells by exploiting the bacterial iron-siderophore uptake system and has demonstrated potent in vitro and in vivo activity against carbapenemase-producing MDR isolates (7–9). This activity is considered to be due to not only efficient uptake via the active siderophore systems but also the high stability of S-649266 against carbapenemase hydrolysis. To elucidate the contribution of β-lactamase stability of S-649266 to its potent antibacterial activity, the kinetic parameters of clinically relevant carbapenemases for S-649266 were determined in this study.
FIG 1.
Chemical structure of S-649266.
The antibacterial activity of S-649266 against global clinical isolates carrying various β-lactamases is shown in Table 1 (see also Table S1 in the supplemental material). The MICs were determined using cation-adjusted Mueller-Hinton broth (BBL, Franklin Lakes, NJ) according to the CLSI standard (10) except that the medium was supplemented with 20 μM human apotransferrin (BBI Solutions, Cardiff, United Kingdom) for S-649266 to create a ferric iron-deficient condition (7, 8, 11). S-649266 showed strong activity against all the carbapenemase-producing isolates tested, with MIC values of ≤2 μg/ml, whereas meropenem, ceftazidime, and cefepime MICs ranged from 16 to >256 μg/ml. These results suggest that S-649266 is stable against a wide variety of carbapenemases, including KPC types and NDM-1.
TABLE 1.
MICs of S-649266 and other antibacterial agents against clinical strains with various β-lactamases
| Species | β-Lactamase | No. of isolates | MIC range (μg/ml) |
|||
|---|---|---|---|---|---|---|
| S-649266a | Ceftazidime | Cefepime | Meropenem | |||
| Pseudomonas aeruginosa | IMP-1 | 3 | 0.016 to 0.5 | >256 | 256 to >256 | 128 to >256 |
| VIM-2 | 3 | 0.25 to 1 | 128 to 256 | 64 to 128 | 32 to 256 | |
| Klebsiella pneumoniae | NDM-1 | 4 | 0.5 to 2 | >256 | 32 to >256 | 64 to 256 |
| KPC-2 or KPC-3 | 4 | 0.06 to 0.5 | 256 to >256 | 64 to >256 | 16 to 256 | |
| Escherichia coli | NDM-1 | 2 | 0.5 to 1 | >256 | 64 to >256 | 16 to 32 |
| Stenotrophomonas maltophilia | L1 | 3 | 0.125 to 0.5 | 128 to 256 | 64 to 128 | 128 to 256 |
| Acinetobacter baumannii | OXA-23 | 5 | 0.03 to 0.5 | 128 to >256 | 16 to 128 | 16 to 32 |
Supplemented with 20 μM human apotransferrin.
In the kinetic study, the recombinant β-lactamases of IMP-1, VIM-2, NDM-1, KPC-3, and OXA-23 without any affinity tags and purified L1 from a clinical isolate were used (see Table S2 in the supplemental material). Hydrolysis of β-lactams was detected by monitoring the changes in the absorbance of β-lactam solution using a UV-2550 (Shimadzu, Japan) or U-3010 (Hitachi, Japan) spectrophotometer. The wavelength and molar extinction coefficient (Δε) for S-649266 were 259 nm and −9,430 M−1 cm−1, respectively. The steady-state kinetic parameters (kcat and Km) were determined by using the Hanes linearization of the Michaelis-Menten equation (12). For poorly hydrolyzing substrates, the competitive inhibition constant (Ki) instead of the Km value was determined in the presence of 100 μM reporter substrate (nitrocefin for IMP-1, VIM-2, KPC-3, and OXA-23; imipenem for L1). The detailed protocols are described in “Supplemental Materials and Methods” in the supplemental material.
The kinetic parameters of carbapenemases for S-649266 were determined and compared to those for meropenem, ceftazidime, and cefepime (Table 2). The kcat/Km values of MBLs of IMP-1, VIM-2, and L1 for S-649266 were the lowest among the antibacterial agents tested with low kcat values and high Ki or Km values. These kcat/Km values for S-649266 were more than 260-fold lower than those for meropenem. In the case of NDM-1, due to the increase in initial hydrolysis velocity with increasing concentrations of chromogenic substrates, such as nitrocefin and chromogenic cephalosporin for β-lactamase substrate (CENTA) (13), no competitive hydrolysis inhibition of S-649266 was observed, and the Ki value was unable to be determined (data not shown). The relative hydrolysis velocity of S-649266 by NDM-1 was compared with those of other antibacterial agents (Table 3). The relative hydrolysis velocity of S-649266 was approximately 3 to 10 times lower than that of the other antibacterial agents tested. These data indicate that S-649266 is highly stable against the MBLs of IMP-1, VIM-2, L1, and NDM-1.
TABLE 2.
Kinetic parameters of carbapenemases for S-649266 and other antibacterial agents
| β-Lactamase | Molecular classa | Antibacterial agent | kcat (s−1)b | Km or Ki (μM)b | kcat/Km (μM−1 s−1) |
|---|---|---|---|---|---|
| IMP-1 | B | S-649266c | 0.92 ± 0.0089 | 190 ± 19 | 0.0048 |
| Meropenem | 6.5 ± 0.23 | 3.3 ± 1.2 | 2.0 | ||
| Ceftazidime | 7.2 ± 0.24 | 55 ± 2.6 | 0.13 | ||
| Cefepime | 10 ± 0.50 | 29 ± 2.6 | 0.34 | ||
| Nitrocefin | 220 ± 33 | 2.6 ± 1.3 | 85 | ||
| VIM-2 | B | S-649266c | 1.0 ± 0.019 | 200 ± 12 | 0.0050 |
| Meropenem | 4.4 ± 0.27 | 2.4 ± 0.63 | 1.8 | ||
| Ceftazidime | 3.3 ± 0.13 | 64 ± 1.1 | 0.052 | ||
| Cefepimec | 49 ± 0.74 | 100 ± 9.3 | 0.49 | ||
| Nitrocefin | 890 ± 6.3 | 4.9 ± 0.29 | 182 | ||
| L1 | B | S-649266 | 12 ± 0.57 | 510 ± 64 | 0.024 |
| Meropenem | 45 ± 1.6 | 7.1 ± 0.94 | 6.3 | ||
| Ceftazidime | 71 ± 2.8 | 470 ± 33 | 0.15 | ||
| Cefepimec | NDd | >500 | NCf | ||
| Imipenem | 250 ± 8.5 | 60 ± 1.9 | 4.2 | ||
| KPC-3 | A | S-649266 | NDe | >1,600 | NC |
| Meropenem | 1.3 ± 0.035 | 6.5 ± 0.37 | 0.20 | ||
| Ceftazidimec | NDd | 3,100 ± 520 | NC | ||
| Cefepimec | 19 ± 0.058 | 350 ± 19 | 0.054 | ||
| Nitrocefin | 47 ± 19 | 15 ± 7.6 | 3.1 | ||
| OXA-23 | D | S-649266c | NH | 4,800 ± 1,100 | NC |
| Meropenemc | NDe | 0.028 ± 0.0023 | NC | ||
| Ceftazidimec | NH | 9,800 ± 270 | NC | ||
| Cefepimec | NDd | 1,500 ± 170 | NC | ||
| Nitrocefin | 350 ± 7.7 | 34 ± 4.9 | 10 |
Classification as described by Ambler (14).
Each kcat, Km, and Ki value is the mean ± standard deviation (SD) of three different measurements. ND, not determined; NH, no hydrolysis detected.
Ki values were obtained using 100 μM nitrocefin for IMP-1, VIM-2, KPC-3, and OXA-23 or 100 μM imipenem for L1 as a reporter substrate.
Hydrolysis was observed, but the Km or Ki value was too high to determine the kcat value.
Hydrolysis was too weak to determine the kcat value.
NC, not calculated.
TABLE 3.
Hydrolysis velocity of S-649266 and other antibacterial agents by NDM-1
| Antibacterial agent | Velocity at substrate concn ofa: |
|||
|---|---|---|---|---|
| 100 μM |
200 μM |
|||
| Hydrolysis velocity (μM/s) | Relative velocity | Hydrolysis velocity (μM/s) | Relative velocity | |
| S-649266 | 0.092 ± 0.0059 | 18 | 0.23 ± 0.018 | 32 |
| Meropenem | 0.50 ± 0.014 | 100 | 0.72 ± 0.012 | 100 |
| Ceftazidime | 1.0 ± 0.015 | 210 | 1.5 ± 0.024 | 210 |
| Cefepime | 0.46 ± 0.028 | 91 | 0.68 ± 0.0092 | 94 |
Each hydrolysis velocity is the mean ± SD of three different measurements. Relative velocity was calculated by assuming the hydrolysis velocity of meropenem to be 100.
Slight hydrolysis of S-649266 by KPC-3 was observed, where all the other tested antibacterial agents except for ceftazidime were efficiently hydrolyzed. The Km value for S-649266 was extremely high (>1,600 μM), with the initial hydrolysis velocity of 0.078 μM/s at 1,600 μM in the presence of 0.89 μM enzyme, indicating the low affinity of S-649266 with KPC-3. The Ki value for ceftazidime was also extremely high (3,100 μM), and the kcat value could not be determined due to the high concentration of ceftazidime required for the evaluation of the kcat value, although hydrolysis of ceftazidime was observed. The Ki values for S-649266 and ceftazidime with OXA-23 were extremely high (4,800 and 9,800 μM, respectively), and no detectable hydrolysis was observed; the change in absorbance was too small to calculate the initial hydrolysis velocity, that is, the change in absorbance was ≤0.001 after a 90-s measurement with 100 μM substrate in the presence of 0.2 μM enzyme, which corresponded to ≤0.006 μM/s. The Ki value for meropenem with OXA-23 was very low, as reported previously (6), and hydrolysis was too weak to determine the kcat value. These results suggest that the higher Km or Ki value for S-649266 with KPC-3 and OXA-23 than for meropenem may contribute to the antibacterial activity against these carbapenemase-producing isolates. In contrast, significant differences in kinetics against OXA-23 were not observed between S-649266 and ceftazidime, although the antibacterial activities of S-649266 and ceftazidime against OXA-23-producing Acinetobacter baumannii isolates were quite different. The penetration efficiency across the outer membrane between S-649266 and ceftazidime may be different due to the unique feature using the iron-siderophore uptake system with S-649266. Currently, dissemination of the OXA-48 group CHDL among Enterobacteriaceae isolates in the Middle East, North Africa, and some European countries is of great concern (4–6). We did not assess the stability against OXA-48 in this report, but there is a need to conduct further study on this clinically important carbapenemase.
A novel antimicrobial that is active against a broad range of Gram-negative bacteria and is stable against a broad range of β-lactamases, including MBLs, would represent a significant advance in treatment options. S-649266 shows potent antibacterial activity against bacteria that produce a wide variety of β-lactamases, including class B as well as class A and D carbapenemases, without adding a β-lactamase inhibitor. The stability of S-649266 against a broad range of carbapenemases shown in this study illustrates a dual advantage of this siderophore molecule that has greater outer membrane penetration coupled with intrinsic β-lactamase stability. This dual approach to treating MDR Gram-negative pathogens may provide a new therapeutic option.
Supplementary Material
ACKNOWLEDGMENTS
We express our appreciation to Takumi Nakamura, Takaomi Ito, Satoshi Hata, Kiyoshi Sugihara, Ayumi Yoshizumi, and Yuichi Kouyama for purification of β-lactamases and Yutaka Jinushi and Toshihiko Hori for antibiotic susceptibility testing. Bacterial strains used for MIC study were kindly provided by Patrice Nordmann (University of Fribourg, Fribourg, Switzerland), Yoshichika Arakawa (Nagoya University, Japan), Tse Hsien Koh (Singapore General Hospital, Singapore), and JMI Laboratories (North Liberty, IA).
Construction of five β-lactamase expression plasmids and enzyme purifications for IMP-1, VIM-2, L1, and KPC-3 were performed at Toho University. Enzyme purifications for NDM-1 and OXA-23 were performed at Shionogi & Co., Ltd. Determination of kinetic parameters for IMP-1, VIM-2, and L1 was conducted at Toho University under contract research for Shionogi. Determination of kinetic parameters for KPC-3 and OXA-23 and relative hydrolysis velocity for NDM-1 was conducted at Shionogi.
We have no other conflicts of interest to declare.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/AAC.03098-15.
REFERENCES
- 1.Queenan AM, Bush K. 2007. Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev 20:440–458. doi: 10.1128/CMR.00001-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walsh TR. 2010. Emerging carbapenemases: a global perspective. Int J Antimicrob Agents 36(Suppl 3):S8–S14. doi: 10.1016/S0924-8579(10)70004-2. [DOI] [PubMed] [Google Scholar]
- 3.Nordmann P. 2014. Carbapenemase-producing Enterobacteriaceae: overview of a major public health challenge. Med Mal Infect 44:51–56. doi: 10.1016/j.medmal.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Tängdén T, Giske CG. 2015. Global dissemination of extensively drug-resistant carbapenemase-producing Enterobacteriaceae: clinical perspectives on detection, treatment and infection control. J Intern Med 277:501–512. doi: 10.1111/joim.12342. [DOI] [PubMed] [Google Scholar]
- 5.Peleg AY, Seifert H, Paterson DL. 2008. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev 21:538–582. doi: 10.1128/CMR.00058-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evansa BA, Amyes SGB. 2014. OXA β-lactamases. Clin Microbiol Rev 27:241–263. doi: 10.1128/CMR.00117-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ito A, Kohira N, Bouchillon SK, West J, Rittenhouse S, Sader HS, Rhomberg PR, Jones RN, Yoshizawa H, Nakamura R, Tsuji M, Yamano Y. 2016. In vitro antimicrobial activity of S-649266, a catechol substituted siderophore cephalosporin, when tested against non-fermenting Gram-negative bacteria. J Antimicrob Chemother 71:670–677. doi: 10.1093/jac/dkv402. [DOI] [PubMed] [Google Scholar]
- 8.Kohira N, West J, Ito A, Ito-Horiyama T, Nakamura R, Sato T, Rittenhouse S, Tsuji M, Yamano Y. 2015. In vitro antimicrobial activity of siderophore cephalosporin S-649266 against Enterobacteriaceae clinical isolates including carbapenem-resistant strains. Antimicrob Agents Chemother 60:729–734. doi: 10.1128/AAC.01695-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakamura R, Toba S, Tsuji M, Yamano Y, Shimada J. 2014. A novel siderophore cephalosporin: IV. In vivo efficacy in various murine infection models, abstr F-1558 54th Intersci Conf Antimicrob Agents Chemother. ASM Press, Washington, DC. [Google Scholar]
- 10.Clinical and Laboratory Standards Institute. 2012. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically—9th ed. CLSI M07-A9. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 11.Otto BR, Verweij-van Vught AM, MacLaren DM. 1992. Transferrins and heme-compounds as iron sources for pathogenic bacteria. Crit Rev Microbiol 18:217–233. doi: 10.3109/10408419209114559. [DOI] [PubMed] [Google Scholar]
- 12.Docquier JD, Lamotte-Brasseur J, Galleni M, Amicosante G, Frère JM, Rossolini GM. 2003. On functional and structural heterogeneity of VIM-type metallo-β-lactamases. J Antimicrob Chemother 51:257–266. doi: 10.1093/jac/dkg067. [DOI] [PubMed] [Google Scholar]
- 13.Bebrone C, Moali C, Mahy F, Rival S, Docquier JD, Rossolini GM, Fastrez J, Pratt RF, Frère JM, Galleni M. 2001. CENTA as a chromogenic substrate for studying β-lactamases. Antimicrob Agents Chemother 45:1868–1871. doi: 10.1128/AAC.45.6.1868-1871.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ambler RP. 1980. The structure of β-lactamases. Philos Trans R Soc Lond B Biol Sci 289:321–331. doi: 10.1098/rstb.1980.0049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.