Summary
Objectives:
To systematically search for scientific evidence concerning the stability of treatment (Tx) results achieved by means of Class II fixed functional appliance therapy and to assess possible differences between appliances.
Search Methods:
An electronic search of databases and orthodontic journals was carried out (until December 2013), with supplemental hand searching. In addition to the names of all identified appliances, the term fixed functional was used in combination with each of the following search terms: long-term, post-Tx, relapse, retention, stability.
Selection Criteria:
To be included in the review, the articles had to contain clear data on: Class II Tx with a fixed functional appliance (>5 patients), post-Tx period ≥ 1 year, assessment of ANB angle, Wits appraisal, molar relationship, soft-tissue profile convexity excluding the nose, overjet and/or overbite.
Data Collection and Analysis:
The literature search revealed 20 scientific investigations which corresponded to only two of the 76 identified appliances (Herbst and Twin Force Bite Corrector). As only one publication was found for the Twin Force Bite Corrector, a meta-analysis could only be performed for Herbst Tx. The data were extracted, pooled and weighted according to the number of patients in each study.
Results:
The mean values for post-Tx relapse (percentages relative to the Tx changes) were: ANB angle 0.2 degrees (12.4 per cent), Wits appraisal 0.5mm (19.5 per cent), sagittal molar relationship 1.2mm/0.1 cusp widths (21.8 per cent /6.5 per cent); soft-tissue profile convexity excluding nose less than 0.1 degrees (1.0 per cent), overjet 1.8mm (26.2 per cent), overbite Class II:1 1.4mm (44.7 per cent), overbite Class II:2 1.0mm (22.2 per cent).
Conclusions:
The scientific evidence concerning the stability of Tx results is inexistent for most fixed functional appliances for Class II correction except for Herbst appliance Tx. Even if the evidence level of most included studies is rather low, good dentoskeletal stability without clinically relevant changes was found for most variables.
Introduction
Class II malocclusion affects 12–32 per cent of the Caucasian population (1–4) and numerous treatment (Tx) approaches involving removable and/or fixed appliances with/without extractions have been described during the last decades. However, since the reintroduction of the Herbst appliance into modern orthodontics by Pancherz in 1977, fixed functional appliances have become the most popular tool for non-surgical Class II Tx (5). Many Herbst appliance derivatives, which all use the bite-jumping-mechanism but differ in appliance and/or anchorage design, have been introduced during the last 30 years (6–8).
Quite a number of papers analysing the dental, skeletal and facial changes taking place during the active Tx period of fixed functional appliance therapy have been published (9–37). However, data beyond the active Tx period seem to be scarce for most appliances and corresponding reviews are lacking.
Therefore, the purposes of the present study were (1) to identify all fixed functional appliances for Class II correction, (2) to systematically review the literature for scientific evidence concerning the stability of Tx results achieved by means of Class II fixed functional appliance therapy, and (3) to perform a meta-analysis (if possible) as well as to assess possible differences between appliances.
Materials and methods
Search strategy—fixed functional appliances
Before conducting the systematic literature review, a non-systematic search was performed in order to identify all fixed functional appliances for Class II correction ever described. For that purpose, orthodontic textbooks (6,8) and review articles (7,9,12,14,15,23,38–40) were screened. Furthermore, the internet pages and catalogues of all major dental/orthodontic manufacturers were consulted as well as the exhibitions of the 2012 annual meetings of the European Orthodontic Society and the German Orthodontic Society. In addition, for all appliances not found in current publications/catalogues, the last known manufacturer was contacted to gain information on whether the appliance was still available on the market.
Search strategy—literature
In the next step, a systematic electronic search strategy was conducted in two main databases (covering a total of 12 databases) as well as 10 international orthodontic journals to systematically search for literature published until (including) December 2013. A full list of all databases and journals is presented in Supplementary Table 1.
In addition to the term fixed functional, the name of each of the identified appliances, was used in combination with each of the following search terms: long-term, post-Tx, relapse, retention, stability. Furthermore, a hand search of the reference lists of the retrieved articles was performed. As an example, the search strategy which was applied onto the database of ‘NCBI-PubMed’ for the term ‘fixed functional’ is given: (fixed functional[All Fields] AND retention[All Fields]) OR (fixed functional [All Fields] AND relapse[All Fields]) OR (fixed functional [All Fields] AND stability[All Fields]) OR ((fixed functional [All Fields]) AND (post[All Fields] AND treatment[All Fields])) OR ((fixed functional [All Fields]) AND (long[All Fields] AND term[All Fields])).
Inclusion criteria
The inclusion criteria were defined as papers describing Class II Tx with a fixed functional appliance (with or without subsequent Tx) of at least five subjects and containing numerical data on the changes occurring during a non-active post-Tx period of at least one year (group average) [Comment: Basically there is no doubt that it would be desirable to include only studies with a high evidence level of I or II (41) in a review. However, for the present main parameter post-Tx stability it is unrealistic. Thus, for clinical orientation, there is no alternative than to include studies with lower evidence levels.]. In addition, study models and/or lateral head films had to have been assessed for ANB angle, Wits appraisal, soft-tissue profile convexity excluding the nose, sagittal molar relationship, overjet and/or overbite.
Studies had to be published either in English or one of the following languages: Danish, Finnish, French, German, Greek, Italian, Spanish, Swedish, or Turkish. A three-step selection procedure (title-abstract-full text) was carried out independently by two reviewers according to the PRISMA statement (42). After each step, the cases of disagreement were discussed until a consensus was reached.
Data extraction
For all included studies, the sample’s general data as well as the values given for measurements regarding the eligible variables were extracted. The methodological quality/risk of bias was assessed for each included study using the checklist by Downs and Black (43) consisting of 27 items categorized in 5 subgroups. For each item, one point was scored when the respective question was answered ‘yes’.
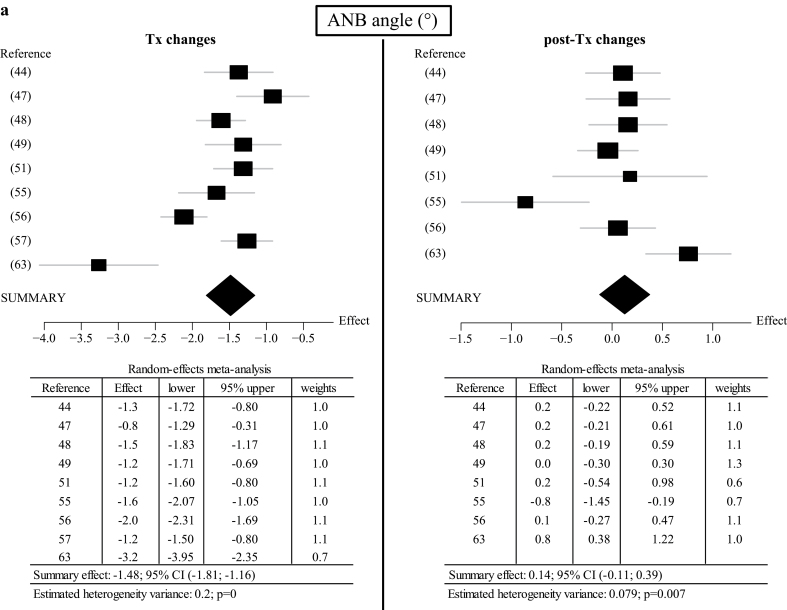
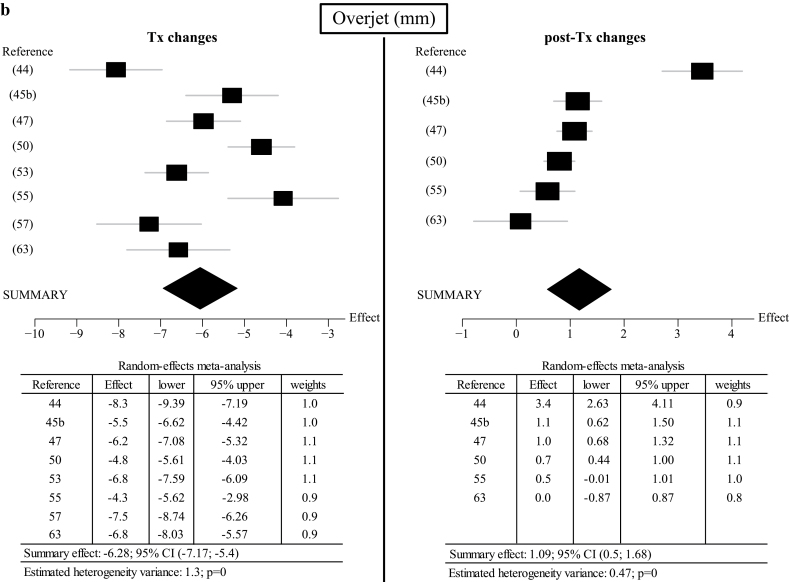
In case of greater than or equal to 3 articles available for the same appliance and malocclusion subtypes, a meta-analysis was performed. The respective mean values were weighted according to the number of patients in each study. For variables where the available data allowed a statistical test for heterogeneity and funnel plots, these were performed in order to identify possible publication bias (Figure 3a and 3b, Supplementary Figures 2a–2e).
Figure 3.
Funnel plots for (a) ANB angle and (b) overjet (Tx and post-Tx). Reference numbers of the included studies, summary effects, confidence intervals (CI), estimated heterogeneity variances and P-values are given.
Results
This chapter consists of three sections—(1) identification of fixed functional appliances for Class II correction, (2) systematic review concerning the stability of Tx results, and (3) meta-analysis.
Seventy-six fixed functional appliances for Class II correction were identified, of which the majority (n = 59) is still available on the market (Supplementary Tables 2 and 3). A large number of these appliances are—at least in major part—derivatives of the original Herbst appliance, and some of them are even available in several different subtypes, which vary in appliance and/or anchorage design (Supplementary Table 2). Other appliances, however, differ concerning the mode of action (Supplementary Table 3).
Systematic review
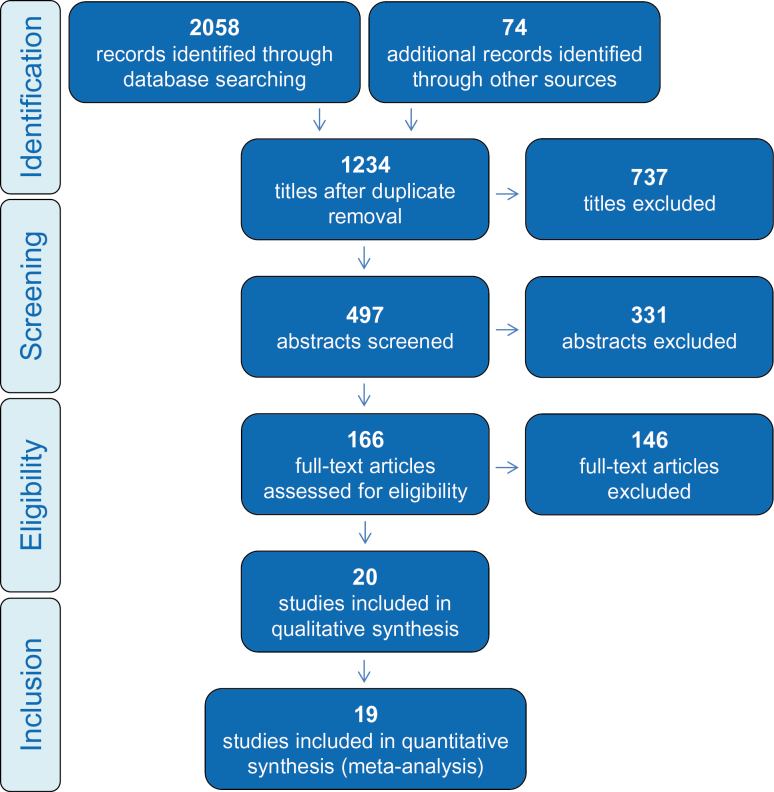
The number of studies identified through the search in the different databases and the selection procedure is detailed in Figure 1. Of the original 2132 hits, 497 abstracts were retrieved and 166 full-text papers were evaluated. The hand search did not deliver any additional material.
Figure 1.
Flow chart outlining the systematic literature search according to the PRISMA guidelines.
Excluded papers
One hundred forty-six of the 166 studies had to be excluded. The main reasons for exclusion were: overview article and/or no scientific study (n = 40), appliance used was not a fixed functional (n = 33), no post-Tx period (n = 27), post-Tx period too short (n = 8), no variable of interest assessed (n = 19), less than 5 patients (n = 16). A full list of the 146 papers and the reasons for exclusion can be obtained from the authors.
Included papers
Finally, 20 publications remained, which were included in the present review (44–63). Most of these papers are case series, and none was on a higher evidence level than of a cohort study. The assessment according to Downs and Black’s checklist (43) revealed moderate methodological quality/risk of bias with the following scoring results—mean: 13.8, median: 14.0, minimum: 8, maximum: 17 (detailed results for each separate paper can be found in Supplementary Table 4). Up to December 2013, no level I or II studies (meta-analysis, randomized clinical trial, or controlled clinical trial) on the stability of Class II fixed functional appliance therapy existed. The 20 scientific investigations (Table 1) correspond to only two of the 76 identified appliances (Herbst and Twin Force Bite Corrector).
Table 1.
Scientific investigations fulfilling the inclusion criteria of the systematic review. The reference details, the appliance used, the malocclusion, the number of patients and the mean pre-Tx age are given.
| Reference | Appliance | Malocclusion | Number of patients | Pre-Tx age (mean) |
|---|---|---|---|---|
| Bock and Pancherz (44) | Herbst | II:1 | 26 | 13.8 |
| Bock et al. (45) | Herbst | (a) II subdivision | 22 | 15 |
| (b) II:1 | 22 | |||
| Bock and Ruf (46) | Herbst | II:2 | 37 | 16.1 |
| Bock and Ruf (47) | Herbst | II:1 | 15 | 25.6 |
| Bock and Ruf (48) | Herbst | II:2 | 37 | 16.2 |
| Bock et al. (49) | Herbst | II:2 | 16 | 18.8 |
| Bock et al. (50) | Herbst | II:1 | 26 | 21.1 |
| Chaiyongsirisern et al. (51) | Herbst | II | 16 | 22 |
| Chhibber et al. (52) | Twin Force Bite Corrector | II:1 | 5 | 11 |
| Hansen et al. (53) | Herbst | II:1 | 53 | 12.5 |
| Hansen et al. (54) | Herbst | II:1 | 24 | 13.0 |
| Nelson et al. (55) | Herbst | II:1 | 15 | 13.5 |
| Pancherz (56) | Herbst | II:1 | 10 | 12.1 |
| Pancherz (57) | Herbst | II:1 | 29 | 12.4 |
| Pancherz and Anehus-Pancherz (58) | Herbst | II:1 | 69 | 12.6 |
| Pancherz et al. (59) | Herbst | II:1 | 14 | 13.4 |
| Pancherz and Hansen (60) | Herbst | II:1 | 40 | 12.5 |
| Phan et al. (61) | Herbst | II:1 | 16 | 12.6 |
| Schweitzer and Pancherz (62) | Herbst | II:2 | 19 | 13 |
| Soytarhan and Isiksal (63) | Herbst | II:1 | 10 | 11.3 |
The included studies report on Tx results and their stability in Class II division 1 and Class II division 2 malocclusions as well as other Class II subgroups. In all investigations, Tx had started with a fixed functional appliance which was—in some cases—accompanied or followed by multibracket appliance Tx conditionally in conjunction with Class II elastics for settling and/or Tx result stabilization. The number of patients included in the studies varied considerably between 5 and 69 individuals (mean = 25, median = 22). The same was true for the patients’ mean age at start of Tx, which varied between 11 and 26 years (mean = 15, median = 14) and the average post-Tx period, which ranged from 12 to 382 months (mean = 58, median = 36). There was a large intra- and inter-study-variation concerning the retention protocol. This varied from removable retention devices to fixed bonded retainers or a combination of both, while some patients did not receive retainers at all.
The retrieved results are presented in detail in Table 2. Negative percentages of post-Tx changes correspond to a favourable development regarding Class II correction (=improvement).
Table 2.
Individual stability data of all 20 fixed functional appliance studies included in the systematic review for ANB angle, Wits appraisal, sagittal molar relationship, soft-tissue profile convexity excluding nose, overjet, and overbite. The appliance used and the reference number are given as well as the means for duration of post-Tx period, changes during Tx and post-Tx [shown in mm, degree or cw, and %, respectively; standard deviations (SD) given if available]. −indicates a favourable post-Tx change concerning Class II correction (=no relapse). For values in italic no meta-analysis could be performed (<3 articles).
| Fixed functional appliance used (reference) | Type of malocclusion (Class) | Post-Tx period (months) | ANB angle | Wits appraisal | Sagittal molar relationship | Soft-tissue profile convexity excluding nose | Overjet | Overbite | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tx changes | post-Tx changes | Tx changes | post-Tx changes | Tx changes | post-Tx changes | Tx changes | post-Tx changes | Tx changes | post-Tx changes | Tx changes | post-Tx changes | |||||||||||||||||||||
| (°)* | SD | (°)* | %* | SD | (mm)* | SD | (mm)* | % | SD | (mm/cw)* | SD | (mm/cw)* | % | SD | (°)* | SD | (°)* | % | SD | (mm)* | SD | (mm)* | % | SD | (mm)* | SD | (mm)* | % | SD | |||
| Herbst (44) | II division 1 | 39 | −1.3 | 1.20 | 0.2 | −11.5 | 0.96 | −5.8 mm | 1.99 | 2.4 mm | −41.4 | 1.79 | −2.8 | 2.28 | 0.6 | −22.6 | 2.80 | −8.3 | 2.86 | 3.4 | −40.7 | 1.93 | ||||||||||
| Herbst (45) | II division 1 | 36 | −1.0 cw | 0.16 | 0.0 cw | −3.0 | 0.11 | −5.5 | 2.63 | 1.1 | −19.2 | 1.06 | ||||||||||||||||||||
| Herbst (47) | II division 1 | 36 | −0.8 | 0.96 | 0.2 | −25.0 | 0.82 | −1.1 | 1.38 | 0.7 | −63.6 | 1.35 | −3.5 mm | 2.11 | 0.3 mm | −8.6 | 0.84 | −1.5 | 1.60 | 0.2 | −13.3 | 1.11 | −6.2 | 1.74 | 1.0 | −16.1 | 0.64 | −2.1 | 1.90 | 1.0 | −47.6 | 0.91 |
| Herbst (50) | II division 1 | 32 | −0.8 cw | 0.26 | 0.1 cw | −9.2 | 0.17 | −4.8 | 2.06 | 0.7 | −14.9 | 0.74 | −2.3 | 1.42 | 0.9 | −38.6 | 0.67 | |||||||||||||||
| Herbst (53) | II division 1 | 74 | −6.8 | 2.80 | 2.0 | −29.2 | −3.3 | 1.69 | 2.3 | −68.9 | ||||||||||||||||||||||
| Herbst (54) | II division 1 | 72 | −1.8 | −0.4 | 22.2 | |||||||||||||||||||||||||||
| Herbst (55) | II division 1 | 72 | −1.6 | 1.01 | −0.8 | 52.6 | 1.25 | −4.3 | 2.60 | 0.5 | −11.6 | 1.00 | −2.3 | 1.80 | 0.5 | −21.7 | 1.30 | |||||||||||||||
| Herbst (56) | II division 1 | 12 | −2.0 | 0.50 | 0.1 | −5.0 | 0.60 | |||||||||||||||||||||||||
| Herbst (57) | II division 1 | 78 | −1.2 | 0.95 | 0.8 | −66.1 | −6.3 mm | 1.50 | 2.0 mm | −32.5 | −7.5 | 3.42 | 3.1 | −41.2 | −4.2 | 1.77 | 2.1 | −50.0 | ||||||||||||||
| Herbst (58) | II division 1 | 74 | −3.3 | 3.62 | −0.3 | 7.6 | ||||||||||||||||||||||||||
| Herbst (59) | II division 1 | 382 | −0.9 cw | 0.2 cw | −22.2 | −4.2 | 0.3 | −7.1 | −1.5 | 0.3 | −20.0 | |||||||||||||||||||||
| Herbst (60) | II division 1 | 12 | −1.5 | 0.1 | −6.7 | −2.4 | 0.1 | −4.2 | −6.4 mm | 1.8 mm | −28.1 | −6.9 | 2.2 | −31.9 | ||||||||||||||||||
| Herbst (61) | II division 1 | 24 | −1.9 | 0.5 | −26.3 | −4.8 | 1.8 | −37.5 | −6.2 mm | 0.9 mm | −14.5 | 7.7 | 2.7 | 35.1 | −3.4 | 1.8 | −52.9 | |||||||||||||||
| Herbst (63) | II division 1 | 12 | −3.2 | 1.29 | 0.8 | −25.4 | 0.68 | −3.6 mm | 1.78 | 0.9 mm | −25.0 | 4.44 | −5.6 | 4.67 | −0.8 | 14.3 | 3.06 | −6.8 | 1.98 | 0.0 | 0.0 | 1.40 | −2.1 | 2.06 | −0.7 | 33.3 | 1.25 | |||||
| Herbst (46) | II division 2 | 27 | −0.8 cw | 0.29 | 0.0 cw | −3.6 | 0.15 | −4.3 | 1.87 | 1.0 | −22.0 | 1.29 | ||||||||||||||||||||
| Herbst (48) | II division 2 | 34 | −1.5 | 1.02 | 0.2 | −13.3 | 1.20 | −1.9 | 1.71 | 0.4 | −21.1 | 1.00 | −3.5 mm | 1.05 | 0.1 mm | −2.9 | 0.87 | −1.4 | −0.4 | 28.6 | −2.2 | 0.5 | −22.7 | −4.1 | 1.78 | 0.9 | −22.2 | 0.94 | ||||
| Herbst (49) | II division 2 | 24 | −1.2 | 1.04 | 0.0 | 0.0 | 0.61 | −2.6 | 2.62 | 1.6 | −61.5 | 2.02 | −1.6 | 1.25 | 0.5 | −31.3 | 0.38 | −4.7 | 1.33 | 1.1 | −23.4 | 0.88 | ||||||||||
| Herbst (62) | II division 2 | 12 | −3.0 | 2.40 | 0.1 | −3.3 | 0.40 | −5.6 | 3.30 | 1.2 | −21.4 | 0.60 | ||||||||||||||||||||
| Herbst (45) | II subdivision | 36 | −1.0 cw | 0.17 | 0.0 cw | −2.0 | 0.13 | 3.6 | 2.05 | 0.4 | 9.7 | 0.92 | ||||||||||||||||||||
| Herbst (51) | II | 36 | −1.2 | 0.81 | 0.2 | −18.3 | 1.56 | −3.4 | 2.14 | 0.5 | −14.4 | 1.26 | −3.7 mm | 2.71 | 0.6 mm | −16.2 | 1.96 | −2.4 | 1.53 | 0.3 | −10.4 | 1.48 | −5.3 | 2.02 | 0.7 | −13.2 | 1.41 | −2.9 | 0.70 | 0.2 | −6.7 | 0.47 |
| Twin (52) Force Bite Corrector | II division 1 | 72 | −2.4 | 1.71 | −1.1 | −45.8 | 0.55 | −2.8 | 1.48 | −2.4 | −85,7 | 3.71 | ||||||||||||||||||||
Negative Tx and post-Tx changes mean favourable development regarding Class II correction (=no relapse).
Twin force bite corrector—single study results
One article describing a total of 5 patients with an average pre-Tx age of 11 years was found. The mean post-Tx observation period was 72 months. During Tx, a decrease of both the ANB-angle (2.4 degrees) and the soft-tissue profile convexity angle excluding the nose (2.8 degrees) was seen. Both variables showed further improvement during the post-Tx period; the ANB angle decreased by an additional 46 per cent and the soft tissue profile convexity excluding the nose straightened by another 86 per cent of the amount achieved during Tx.
Herbst appliance—meta-analysis
Nineteen studies on Herbst Tx were found. The meta-analysis for the post-Tx changes of the variables ‘ANB angle’, ‘Wits appraisal’ and ‘sagittal molar relationship’ was performed irrespective of the type of Class II malocclusion. Due to the differences in dentofacial morphology between Class II division 1 and Class II division 2 malocclusions, the post-Tx changes of the remaining variables ‘soft-tissue profile convexity angle excluding the nose’, ‘overjet’ and ‘overbite’ were performed separately for each malocclusion type. For sagittal molar relationship, separate calculations were performed for studies using millimetres [from assessing lateral cephalograms (LH)] and cusp widths [cw; from assessing study models (SM)]. In detail, the following data (averages—weighted according to the number of patients in each study) were extracted (Table 3, Figure 2a and 2b, Supplementary Figures 1a–1e). However, due to the heterogeneity of both the patient samples and the length of the post-Tx period, large variations were seen for all changes.
Table 3.
Meta-analysis data for the stability of Herbst appliance Tx derived from 19 studies. The weighted data (weighted according to the number of patients of each individual study) for ANB angle, Wits appraisal, sagittal molar relationship [data from studies using millimetres and cusp widths (cw) shown separately], soft-tissue profile convexity excluding nose, overjet, and overbite are shown. The references, total number of patients, weighted mean pre-Tx age, Tx changes, duration of post-Tx observation period (months), post-Tx changes as well as final values are shown.
| Variable | References | Number of patients | Pre-Tx age (weighted) | Tx changes* (weighted) | Duration of post-Tx observation period in months (weighted) | Post-Tx relapse* (weighted) | Final value (weighted) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | mean (years) | mean | mean | min | max | mean | min | max | mean | ||
| ANB angle (n = 12) | (44,47,48,49,51,54,55,56, 57,60,61,63) | 254 | 15.0 | −1.5° | 34.0 | 12 | 78 | 0.2° | −0.8° | 0.8° | 4.1° |
| Wits appraisal (n = 6) | (47,48,51,60,61,62) | 143 | 16.0 | −2.6 mm | 24.2 | 12 | 36 | 0.5 mm | 0.1 mm | 1.8 mm | 0.1 mm |
| Sagittal molar relationship (n = 12) | (44,45,46,47,48,50,51,57, 59,60,61,63) | 310 | 15.7 | −5.1mm, −0.8 cw | 49.7 | 12 | 382 | 1.2mm, 0.1 cw | 0.1mm, 0.0 cw | 2.4mm, 0.2 cw | −2.0 mm**, 0.1 cw*** |
| Soft-tissue profile convexity (n = 4) | |||||||||||
| Class II:1 | (44,47,58,63) | 120 | 14.4 | −3.2° | 56.5 | 12 | 74 | 0.0° | −0.8° | 0.6° | 160.6° |
| Overjet (n = 11) | |||||||||||
| Class II:1 | (44,45,47,50,53,55,57,59,60,61,63) | 266 | 14.4 | −6.5 mm | 63.1 | 12 | 382 | 1.8 mm | 0.0 mm | 3.4 mm | 3.8 mm |
| Overbite (n = 8) | |||||||||||
| Class II:1 | (47,50,53,55,57,59,61,63) | 178 | 14.9 | −2.9 mm | 81.4 | 12 | 382 | 1.4 mm | −0.7 mm | 2.3 mm | 3.7 mm |
| Overbite (n = 4) | |||||||||||
| Class II:2 | (46,48,49,62) | 109 | 16.0 | −4.4 mm | 26.3 | 12 | 34 | 1.0 mm | 0.9 mm | 1.2 mm | 2.8 mm |
*Negative Tx and post-Tx changes mean favourable development regarding Class II correction (=no relapse).
**0.0mm means edge-to-edge Class II relationship (=0.5 cw).
***0.0 cw means Class I relationship.
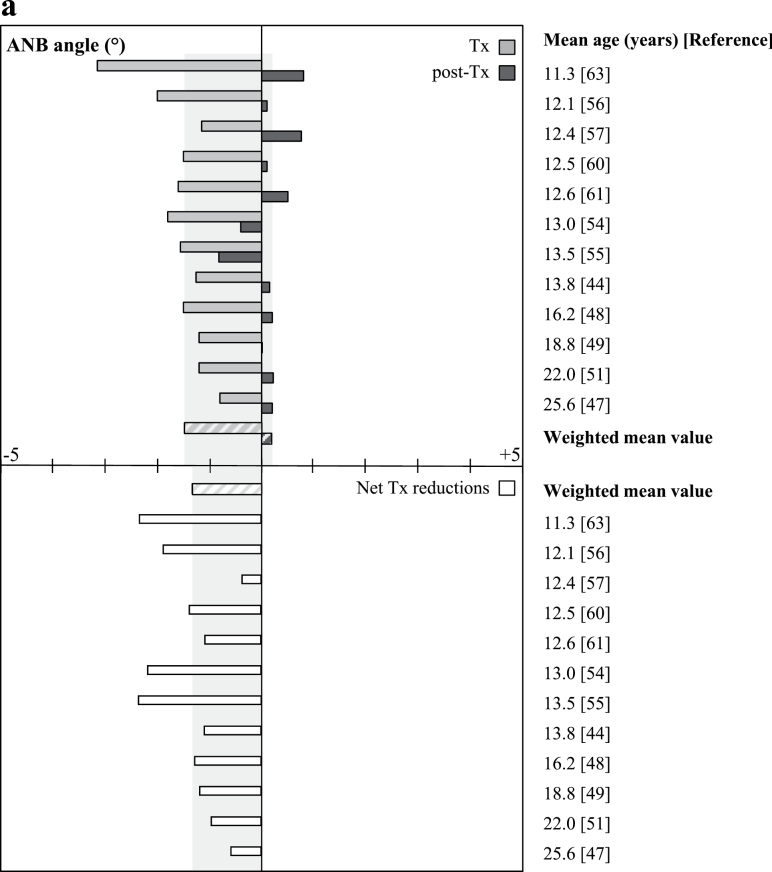
Figure 2.
Chart demonstrating the individual (article-based) Tx, post-Tx and net Tx changes of (a) ANB angle and (b) overjet as well as the weighted mean values (striped bars and grey shaded area) sorted according to mean pre-Tx age (ascending order). The reference of each article is given. Negative (−) changes indicate favourable development regarding Class II correction.
The results of statistical testing for heterogeneity and the corresponding funnel plots are given in Figure 3a and 3b and Supplementary Figures 2a–2e.
-
ANB angle (Figures 2a and 3a)
- The mean ANB reduction during Tx was 1.5 degrees and the average relapse during the post-Tx period was 0.2 degrees. Looking at the net Tx reduction (mean: −1.3 degrees), investigations in young patients showed notably large variations independent of pre-Tx age. Studies in adults on the other hand exhibit a tendency for generally smaller but still obvious changes.
-
Wits appraisal (Supplementary Figures 1a and 2a)
- The average decrease during Tx was 2.6mm and the mean post-Tx relapse amounted to 0.5mm. The individual studies exhibited a large variation which did not seem to be related to pre-Tx age. The net Tx reductions were similar (mean: 2.1mm) in all studies but the one with the highest mean pre-Tx age, which shows a considerably lower value.
Sagittal molar relationship (Supplementary Figures 1b, 2b-1, and 2b-2)
- Measuring unit mm: The mean amount of correction during Tx was 5.1mm and the average relapse during the post-Tx period amounted to 1.2mm. A tendency of lower ranges was seen in the studies investigating children/early adolescents and adult patients. The net Tx reduction (mean: 3.9mm) was largely independent of pre-Tx age.
- Measuring unit cw: The mean amount of correction during Tx was 0.8 cw and the average relapse 0.1 cw with a net Tx reduction of 0.7 cw. No association of the changes with age was noted.
Soft-tissue profile convexity excluding the nose (Supplementary Figures 1c and 2c)
- Class II division 1: During Tx, an average decrease of 3.2 degrees occurred and the mean relapse during the post-Tx period was less than 0.1 degrees. The Tx changes showed a clear decrease with increasing pre-Tx age. A large variation was also seen for the post-Tx changes: while the investigations in children/adolescents showed small amounts of further decrease, the studies in the older patients showed small amounts of relapse.
Overjet (Figures 2b and 3b)
- Class II division 1: During Tx, an average overjet reduction of 6.5mm was seen. The amount of relapse during the post-Tx period was 1.8mm. Similar net Tx reductions (mean: 4.7mm) were seen in all studies irrespective of age except for the one with the lowest mean pre-Tx age, which shows a considerably higher value.
Overbite
- Class II division 1 (Supplementary Figures 1d and 2d): The average decrease of overbite during Tx was 2.9mm and the mean amount of relapse during the post-Tx period amounted to 1.4mm. The individual studies exhibited a large variation concerning the Tx changes showing a clear tendency towards less decrease in the youngest and the oldest patients. A large variation can be seen for the post-Tx changes as well; however, the investigations with the youngest and oldest patients show the most favourable development (further decrease or small amounts of relapse, respectively). Regarding net Tx reductions (mean: 1.5mm) similar values were seen in all studies but the one with the lowest mean pre-Tx age, which shows a slightly more favourable value.
- Class II division 2 (Supplementary Figures 1e and 2e): The mean reduction of overbite during Tx amounted to 4.4mm and the average relapse during the post-Tx period was 1.0mm. Similar values were seen in all investigations but the one with the lowest mean pre-Tx age which shows a slightly more favourable value for the Tx period. For the net Tx reductions (mean: 3.4mm), again similar values were seen in all studies but the one with the lowest mean pre-Tx age showing a slightly higher value (Supplementary Figure 1e).
Discussion
In accordance with previous studies (7,8,33), the present review identified a large variety of fixed functional appliances (n = 76). The current study is the first review to assess the post-Tx period.
Systematic review
In order to avoid omitting any data on the stability after fixed functional Class II Tx, the inclusion criteria were defined quite wide-ranging. There were no limitations with respect to publication years and many languages were included. In spite of a rather high amount of hits at the beginning of the search, only 20 articles were finally included.
Similar difficulties were faced when searching for comparative literature. The data of the few studies identified are summarized in Supplementary Table 5.
Looking at the results of the present systematic review, one has to admit that the total number of available investigations (n = 20), reporting stability data during a retention period of at least 1 year following fixed functional Tx, is low compared to the high amount of appliances available (n = 76). This is especially true, when considering that these studies analyse the effects of only two of these 76 appliances: Herbst (n = 19) and Twin Force Bite Corrector (n = 1). Thus, for the vast majority of the Herbst appliance derivatives no Tx stability data exist. Even if it might be tempting to expect similar effects from all kinds of fixed functional appliances for Class II correction, it should be remembered, that the amount of dental and skeletal treatment effects, and thus the potential for relapse, may differ.
Meta-analysis (Herbst appliance)
As for natural reasons a meta-analysis could only be performed for the Herbst appliance, the following discussion will be restricted to the stability of Herbst Tx.
Quality of included papers
The evidence level of the 19 Herbst studies was rather low: case series without controls or with controls treated by a different protocol—level III according to the ‘Levels of Evidence’ by Shekelle et al. (41). In addition, a moderate risk for bias existed according to the Downs and Black’s checklist. The partly asymmetrical data distribution in the funnel plots (Figure 3a and 3b, Supplementary Figures 2a–2e) as well as the calculated heterogeneity values and significances (Figure 3a and 3b, Supplementary Figures 2a–2e) also indicated a moderate risk for bias. Due to the low number of studies and mainly small patient samples, however, this data must be interpreted carefully. Nevertheless, despite the fact, that it is ethically difficult or even impossible to obtain long-term stability data of untreated controls, it is also scientifically and clinically less important for the retention period than for the active Tx period, as only minor changes are expected to occur in untreated controls during the time period corresponding to the post-Tx phase.
Due to the low number of studies fulfilling the inclusion criteria, the assessment opportunities were limited and no differentiation regarding factors like age, skeletal maturity, duration of the post-Tx period or duration and mode of any subsequent Tx, type of retention regime and comparison to a control group was made. This, of course, must be considered when interpreting the results; a large range existed especially for the variables age and duration of post-Tx period. Furthermore, as some research groups published more than one of the included studies, some patients might have been included in more than one investigation; this however, was impossible to account for by looking at the data retrospectively.
General patient characteristics
The average pre-Tx age of the Herbst patients was around 15 years with a large amount of patients having completed most of their pubertal growth. The average stability data reported for Herbst Tx (Table 2) show only clinically irrelevant changes, hence on average stability can be considered as being good. However, the range of relapse seen for all analysed variables was large. This is in agreement with the conclusion drawn by Bondemark et al. (64) who performed a systematic review on long-term stability of orthodontic Tx (which included some of the studies being part of the present investigation) and also described a certain amount of relapse to occur after Herbst appliance Tx—which, however, cannot be predicted at the individual level.
ANB angle/Wits appraisal
For the evaluated skeletal variables (ANB angle/Wits appraisal) the post-Tx changes showed weighted mean values of 0.2 degrees (ANB) and 0.5mm (Wits), respectively (Table 2, Figure 2a, Supplementary Figure 1a). Looking at the literature (Supplementary Table 5), similar relapse values can be found in investigations by Fidler et al. (65) (ANB = 0.2 degrees; Wits = 1.4mm) and Franchi et al. (66) (Wits = 0.8mm). While the data for the ANB angle (Figure 2a) showed similar amounts of post-Tx changes for the studies with a mean pre-Tx age of 13.8 years and above, the studies evaluating younger patients exhibited very large inter-study differences. It seemed as if the net Tx reduction was more predictable for older patients. To some extent, the same was true for Wits appraisal (Supplementary Figure 1a). While the post-Tx changes were quite similar in studies with a mean pre-Tx age ≥ 16.2 years, large inter-study differences exist in younger patients.
Sagittal molar relationship
Looking at sagittal molar relationship (Table 3, Supplementary Figure 1b), a weighted mean post-Tx relapse of 1.2mm (measurements on LH) and 0.1 cw (measurements on SM) occurred. The minimal difference between the two methods might on the one hand be due to the differing pre-Tx age (LH = 15.1 years; SM = 16.5 years) and thus, different post-Tx growth potential of the respective studies. On the other hand, the accuracy of the two methods differs—steps of 0.5mm were used for LH-assessment while steps of 0.25 cw (approximately 2.0mm) were applied during SM-assessment. The investigations by Fidler et al. (65) and Franchi et al. (66) show some slightly more favourable values for post-Tx relapse of sagittal molar relationship (Supplementary Table 5): 0.3mm (SM-assessment) and 0.1mm (LH-assessment). Comparing these results to the current findings, however, one has to bear in mind that the mean pre-Tx age of the patients (11.2—Fidler et al.; 10.0—Franchi et al.; 15.7—current meta-analysis) as well as the Tx-changes (3.4 mm—Fidler et al.; 2.9 mm—Franchi et al.; 5.1mm/0.7 cw—current meta-analysis) differ tremendously.
Soft-tissue profile convexity
The soft-tissue profile convexity excluding nose (Table 3, Supplementary Figure 1c) was the variable with the highest degree of stability in this meta-analysis: on average greater than 0.1 degrees relapse of the Tx-changes. This favourable behaviour probably has to be attributed (at least partially) to favourable growth patterns of the craniofacial soft-tissues. On the other hand, most of the patients probably ended active Tx with only little remaining growth potential (average pre-Tx age 14.4 years). Looking at the detailed data of the four included studies, one can see that favourable post-Tx changes were especially seen in the younger patients while the studies involving older patients showed a moderate relapse of up to 0.6 degrees.
Overjet
For overjet (Table 3, Figure 2b), an average post-Tx relapse of 1.8mm occurred. Even if the range of both Tx and post-Tx changes was large—with a tendency for more uniform values in older patients (mean pre-Tx age ≥ 13.4 years)—the net Tx changes are quite similar in all studies included in the meta-analysis. Comparing the data to the literature (Supplementary Table 5), similar or slightly more favourable relapse values were seen (65–69: 0.1–1.1mm). However, pre-Tx age and corresponding post-Tx growth potential differ between the investigations showing more favourable values for post-Tx development than the current meta-analysis, where the average pre-Tx age was quite high (14.4 years). Furthermore, some of the studies included in the present investigation—in contrast to the other studies cited above—contain data of patients who did not receive any subsequent multibracket appliance Tx after removal of the Herbst appliance, which means that the post-Tx records were taken immediately after Herbst-Tx, and thus before settling. Consequently, these patients exhibited an overcompensation of overjet on the post-Tx records and thus larger tooth movements during the settling period, which was included in the amount of changes of the post-Tx/retention phase.
Overbite—Class II division 1
For overbite in Class II division 1 patients (Table 3, Supplementary Figure 1d), a moderate stability was found: 1.4mm of the reduction seen during Tx (2.9mm) relapsed during the post-Tx period. However, an effective overbite relapse of 1.4mm seems to be of minor clinical relevance. Again, the studies with a higher mean pre-Tx age (greater than or equal to 13.4 years) showed a tendency for more uniform amounts of changes. The investigations in the literature (65–69) show a slightly less post-Tx overbite relapse (0.1–0.9mm; Supplementary Table 5).
Overbite—Class II division 2
Looking at overbite stability in Class II division 2 patients (Table 3, Supplementary Figure 1e), however, a rather good stability showing 1.0mm of relapse was found for the post-Tx period (reduction during Tx: 4.4mm). Furthermore, all studies showed similar changes during both the Tx and post-Tx period resulting in resembling net Tx values. The relapse values described in the literature (70–72) are alike (0.5–1.4mm; Supplementary Table 5).
On average the present meta-analysis shows minor, clinically irrelevant post-Tx changes for Herbst Tx. A tendency for more uniform Tx and post-Tx changes were seen in older compared to younger patients (Figure 2a and 2b, Supplementary Figures 1a–1e). Even if some slightly more favourable post-Tx changes for overjet and overbite after other Tx protocols than Herbst/fixed functional Class II Tx are reported in the literature, it should be kept in mind that the use of fixed functional appliances is especially suggested and indicated in rather severe, challenging malocclusions and patients where other Tx protocols are unlikely to result in a successful Tx outcome. In daily practice and in accordance with the described large interindividual differences the predictability of Tx and post-Tx changes on the individual level seems to be limited.
Conclusions
The scientific evidence concerning the stability of Tx results is inexistent for most fixed functional appliances for Class II correction except for Herbst appliance Tx. Even if the quality of most studies is rather low (evidence level III), good dentoskeletal stability without clinically relevant changes was found for most variables.
Supplementary Material
Supplementary material is available at European Journal of Orthodontics online.
Funding
This study received no funding.
References
- 1. Bazant V., Miksa J. (1960) Die Häufigkeit der Okklusionsanomalien in sagittaler Richtung in der Klassifikation nach Angle bei Erwachsenen. Fortschritte der Kieferorthopädie, 21, 328–338. [Google Scholar]
- 2. Brunelle J.A., Bhat M., Lipton J.A. (1996) Prevalence and distribution of selected occlusal characteristics in the US population, 1988–1991. Journal of Dental Research, 75, 706–713. [DOI] [PubMed] [Google Scholar]
- 3. Ingervall B. (1974) Prevalence of dental and occlusal anomalies in Swedish conscripts. Acta odontologica Scandinavica, 32, 83–92. [DOI] [PubMed] [Google Scholar]
- 4. Lippold C., van den Bos L., Hohoff A., Danesh G., Ehmer U. (2003) Interdisciplinary study of orthopedic and orthodontic findings in pre-school infants. Journal of Orofacial Orthopedics, 64, 330–340. [DOI] [PubMed] [Google Scholar]
- 5. Keim R.G., Gottlieb E.L., Nelson A.H., Vogels D.S. (2008) JCO study of orthodontic diagnosis and treatment procedures, part 1: results and trends. Journal of Clinical Orthodontics, 42, 625–640. [PubMed] [Google Scholar]
- 6. Baxmann M. (2012) Festsitzende Apparaturen zur Klasse-II-Therapie. Quintessenz, Berlin, Germany. [Google Scholar]
- 7. Hourfar J., Ludwig B., Ruf S., Kinzinger G., Lisson J. (2012) Fixed treatment of Retroposition of the Mandible—a Literature Review. Informationen aus Orthodontie und Kieferorthopädie, 44, 183–192 [German]. [Google Scholar]
- 8. Papadopoulos M.A. (2006) Orthodontic Treatment of the Class II Noncompliant Patient. Mosby Elsevier, Philadelphia, PA. [Google Scholar]
- 9. Aelbers C.M.F., Dermaut L.R. (1996) Orthopedics in orthodontics: Part I, Fiction or reality—a review of the literature. American Journal of Orthodontics and Dentofacial Orthopedics, 110, 513–519. [DOI] [PubMed] [Google Scholar]
- 10. Al-Jewair T.S., Preston C.B., Moll E.M., Dischinger T. (2012) A comparison of the MARA and the AdvanSync functional appliances in the treatment of Class II malocclusion. The Angle Orthodontist, 82, 907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Baccetti T., Franchi L., Stahl F. (2009) Comparison of 2 comprehensive Class II treatment protocols including the vonded Herbst and headgear appliances: a double-blind study of consecutively treated patients at puberty. American Journal of Orthodontics and Dentofacial Orthopedics, 135, 698e1–e10. [DOI] [PubMed] [Google Scholar]
- 12. Barnett G.A., Higgins D.W., Major P.W., Flores-Mir C. (2008) Immediate skeletal and dentoalveolar effects of the crown- or banded type Herbst appliance on Class II division 1 malocclusion. The Angle Orthodontist, 78, 361–369. [DOI] [PubMed] [Google Scholar]
- 13. Cope J.B., Buschang P.H., Cope D.D., Parker J., Blackwood H.O., III (1994) Quantitative evaluation of craniofacial changes with Jasper Jumper therapy. The Angle Orthodontist, 64, 113–122. [DOI] [PubMed] [Google Scholar]
- 14. Flores-Mir C., Major M.P., Major P.W. (2006) Soft tissue changes with fixed functional appliances in Class II division 1. The Angle Orthodontist, 76, 712–720. [DOI] [PubMed] [Google Scholar]
- 15. Flores-Mir C., Ayeh A., Goswani A., Charkhandeh S. (2007) Skeletal and dental changes in Class II division 1 malocclusions treated with splint-type Herbst appliances. A systematic review. The Angle Orthodontist, 77, 376–381. [DOI] [PubMed] [Google Scholar]
- 16. Franchi L., Alvetro L., Giuntini V., Masucci C., Defraia E., Baccetti T. (2011) Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in Class II patients. The Angle Orthodontist, 81, 678–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ghislanzoni L.T., Toll D.E., Defraia E., Baccetti T., Franchi L. (2011) Treatment and posttreatment outcomes induced by the Mandibular Advancement Repositioning Appliance; a controlled clinical study. The Angle Orthodontist, 81, 684–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guimarães C.H., Jr., Henriques J.F., Janson G., de Almeida M.R., Araki J., Cançado R.H., Castro R., Nanda R. (2013) Prospective study of dentoskeletal changes in Class II division malocclusion treatment with twin force bite corrector. The Angle Orthodontist, 83, 319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jones G., Buschang P.H., Kim K.B., Oliver D.R. (2008) Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. The Angle Orthodontist, 78, 332–338. [DOI] [PubMed] [Google Scholar]
- 20. Kinzinger G., Diedrich P. (2005) Skeletal effects in class II treatment with the functional mandibular advancer (FMA)? Journal of Orofacial Orthopedics, 66, 469–490. [DOI] [PubMed] [Google Scholar]
- 21. Konik M., Pancherz H., Hansen K. (1997) The mechanism of Class II correction in late Herbst treatment. American Journal of Orthodontics and Dentofacial Orthopedics, 112, 87–91. [DOI] [PubMed] [Google Scholar]
- 22. Küçükkeleş N., Ilhan I., Orgun I.A. (2007) Treatment efficiency in skeletal Class II patients treated with the Jasper Jumper. The Angle Orthodontist, 77, 449–456. [DOI] [PubMed] [Google Scholar]
- 23. McSherry P.F., Bradley H. (2000) Class II correction-reducing patient compliance: a review of the available techniques. Journal of Orthodontics, 27, 219–225. [DOI] [PubMed] [Google Scholar]
- 24. Obijou C., Pancherz H. (1997) Herbst appliance treatment of Class II, division 2 malocclusions. American Journal of Orthodontics and Dentofacial Orthopedics, 112, 287–291. [DOI] [PubMed] [Google Scholar]
- 25. Pancherz H. (1979) Treatment of class II malocclusions by jumping the bite with the Herbst appliance. A cephalometric investigation. American Journal of Orthodontics, 76, 423–442. [DOI] [PubMed] [Google Scholar]
- 26. Pancherz H. (1982) The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. American Journal of Orthodontics, 82, 104–113. [DOI] [PubMed] [Google Scholar]
- 27. Pancherz H. (1997) The effects, limitations, and long-term dentofacial adaptations to treatment with the Herbst appliance. Seminars in Orthodontics, 3, 232–243. [DOI] [PubMed] [Google Scholar]
- 28. Pancherz H., Anehus-Pancherz M. (1993) The headgear effect of the Herbst appliance: a cephalometric long-term study. American Journal of Orthodontics and Dentofacial Orthopedics, 103, 510–520. [DOI] [PubMed] [Google Scholar]
- 29. Pancherz H., Ruf S. (2008) The Herbst Appliance: Research-Based Clinical Management. Quintessence Pub, Berlin, Germany. [Google Scholar]
- 30. Pancherz H., Ruf S., Kohlhas P. (1998) “Effective condylar growth” and chin position changes in Herbst treatment: a cephalometric roentgenographic long-term study. American Journal of Orthodontics and Dentofacial Orthopedics, 114, 437–446. [DOI] [PubMed] [Google Scholar]
- 31. Ruf S., Pancherz H. (1999a) Temporomandibular joint remodeling in adolescents and young adults during Herbst treatment: a prospective longitudinal magnetic resonance imaging and cephalometric radiographic investigation. American Journal of Orthodontics and Dentofacial Orthopedics, 115, 607–618. [DOI] [PubMed] [Google Scholar]
- 32. Ruf S., Pancherz H. (1999) Dentoskeletal effects and facial profile changes in young adults treated with the Herbst appliance. The Angle Orthodontist, 69, 239–246. [DOI] [PubMed] [Google Scholar]
- 33. Schrodt C., Pancherz H., Ruf S. (2006) Scientific evidence for the variety in bite jumping appliances. European Journal of Orthodontics, 28, e259. [Google Scholar]
- 34. Shen G., Hägg U., Darendeliler M. (2005) Skeletal effects of bite jumping therapy on the mandible—removable vs. fixed functional appliances. Orthodontics & Craniofacial Research, 8, 2–10. [DOI] [PubMed] [Google Scholar]
- 35. Stromeyer E.L., Caruso J.M., DeVincenzo J.P. (2002) A cephalometric study of the Class II correction effects of the Eureka Spring. The Angle Orthodontist, 72, 203–210. [DOI] [PubMed] [Google Scholar]
- 36. Stucki N., Ingervall B. (1998) The use of the Jasper Jumper for the correction of Class II malocclusion in the young permanent dentition. European Journal of Orthodontics, 20, 271–281. [DOI] [PubMed] [Google Scholar]
- 37. Wieslander L. (1984) Intensive treatment of severe Class II malocclusions with a headgear-Herbst appliance in the early mixed dentition. American Journal of Orthodontics, 86, 1–13. [DOI] [PubMed] [Google Scholar]
- 38. Dermaut L.R., Aelbers C.M.F. (1996) Orthopedics in orthodontics: Fiction or reality. A review of the literature—Part II. American Journal of Orthodontics and Dentofacial Orthopedics, 110, 667–671. [DOI] [PubMed] [Google Scholar]
- 39. Millett D.T., Cunningham S.J., O’Brien K.D., Benson P.E., de Oliveira C.M. (2012) Treatment and stability of Class II Division 2 malocclusion in children and adolescents: a systematic review. American Journal of Orthodontics and Dentofacial Orthopedics, 142, 159–169e9. [DOI] [PubMed] [Google Scholar]
- 40. Ritto A.K., Ferreira A.P. (2000) Fixed functional appliances–a classification. The Functional Orthodontist, 17, 12–30, 32. [PubMed] [Google Scholar]
- 41. Shekelle P.G., Woolf S.H., Eccles M., Grimshaw J. (1999) Developing clinical guidelines. West J Med, 170, 348–351. [PMC free article] [PubMed] [Google Scholar]
- 42. Moher D., Liberati A., Tetzlaff J., Altman D.G; The Prisma Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Medicine, 3, e123–130. [PMC free article] [PubMed] [Google Scholar]
- 43. Downs S.H., Black N. (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health, 52, 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bock N., Pancherz H. (2006) Herbst treatment of Class II division 1 malocclusions in retrognathic and prognathic facial types. The Angle Orthodontist, 76, 930–941. [DOI] [PubMed] [Google Scholar]
- 45. Bock N.C., Reiser B., Ruf S. (2013) Class II subdivision treatment with the Herbst appliance. The Angle Orthodontist, 83, 327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bock N., Ruf S. (2008) Post-treatment occlusal changes in Class II division 2 subjects treated with the Herbst appliance. European Journal of Orthodontics, 30, 606–613. [DOI] [PubMed] [Google Scholar]
- 47. Bock N.C., Ruf S. (2012) Dentoskeletal changes in adult Class II division 1 Herbst treatment–how much is left after the retention period? European Journal of Orthodontics, 34, 747–753. [DOI] [PubMed] [Google Scholar]
- 48. Bock N.C., Ruf S. (2013) Class II division 2 treatment—does skeletal maturity influence success and stability? Journal of Orofacial Orthopedics, 74, 187–204. [DOI] [PubMed] [Google Scholar]
- 49. Bock N.C., Santo C., Pancherz H. (2009) Facial profile and lip position changes in adult Class II, Division 2 subjects treated with the Herbst-Multibracket appliance. A radiographic cephalometric pilot study. Journal of Orofacial Orthopedics, 70, 51–62. [DOI] [PubMed] [Google Scholar]
- 50. Bock N.C., von Bremen J., Ruf S. (2010) Occlusal stability of adult Class II Division 1 treatment with the Herbst appliance. American Journal of Orthodontics and Dentofacial Orthopedics, 138, 146–151. [DOI] [PubMed] [Google Scholar]
- 51. Chaiyongsirisern A., Rabie A.B., Wong R.W. (2009) Stepwise advancement Herbst appliance versus mandibular sagittal split osteotomy. Treatment effects and long-term stability of adult Class II patients. The Angle Orthodontist, 79, 1084–1094. [DOI] [PubMed] [Google Scholar]
- 52. Chhibber A., Upadhyay M., Uribe F., Nanda R. (2010) Long-term stability of Class II correction with the Twin Force Bite Corrector. Journal of Clinical Orthodontics: JCO, 44, 363–376. [PubMed] [Google Scholar]
- 53. Hansen K., Koutsonas T.G., Pancherz H. (1995) Long-term effects of the Herbst appliance on the dental arches and arch relationships: a biometric study. British Journal of Orthodontics, 22, 123–134. [DOI] [PubMed] [Google Scholar]
- 54. Hansen K., Iemamnueisuk P., Pancherz H. (1997) Long-term effects of Herbst treatment on the mandibular incisor segment: a cephalometric and biometric investigation. American Journal of Orthodontics and Dentofacial Orthopedics, 112, 92–103. [DOI] [PubMed] [Google Scholar]
- 55. Nelson B., Hägg U., Hansen K., Bendeus M. (2007) A long-term follow-up study of Class II malocclusion correction after treatment with Class II elastics or fixed functional appliances. American Journal of Orthodontics and Dentofacial Orthopedics, 132, 499–503. [DOI] [PubMed] [Google Scholar]
- 56. Pancherz H. (1981) The effect of continuous bite jumping on the dentofacial complex: a follow-up study after Herbst appliance treatment of class II malocclusions. European Journal of Orthodontics, 3, 49–60. [DOI] [PubMed] [Google Scholar]
- 57. Pancherz H. (1991) The nature of Class II relapse after Herbst appliance treatment: a cephalometric long-term investigation. American Journal of Orthodontics and Dentofacial Orthopedics, 100, 220–233. [DOI] [PubMed] [Google Scholar]
- 58. Pancherz H., Anehus-Pancherz M. (1994) Facial profile changes during and after Herbst appliance treatment. European Journal of Orthodontics, 16, 275–286. [DOI] [PubMed] [Google Scholar]
- 59. Pancherz H., Bjerklin K., Lindskog-Stokland B., Hansen K. (2014) Thirty-two-year follow-up study of Herbst therapy: a biometrical dental cast analysis. American Journal of Orthodontics and Dentofacial Orthopedics, 145, 15–27. [DOI] [PubMed] [Google Scholar]
- 60. Pancherz H., Hansen K. (1986) Occlusal changes during and after Herbst treatment: a cephalometric investigation. European Journal of Orthodontics, 8, 215–228. [DOI] [PubMed] [Google Scholar]
- 61. Phan K.L., Bendeus M., Hägg U., Hansen K., Rabie A.B. (2006) Comparison of the headgear activator and Herbst appliance–effects and post-treatment changes. European Journal of Orthodontics, 28, 594–604. [DOI] [PubMed] [Google Scholar]
- 62. Schweitzer M., Pancherz H. (2001) The incisor-lip relationship in Herbst/multibracket appliance treatment of Class II, Division 2 malocclusions. The Angle Orthodontist, 71, 358–363. [DOI] [PubMed] [Google Scholar]
- 63. Soytarhan A., Isiksal A. (1990) Treatment of Angle Class II/1 malocclusions with the Herbst appliance. Turk Ortodonti Dergisi, 3, 94–101. [PubMed] [Google Scholar]
- 64. Bondemark L., Holm A.K., Hansen K., Axelsson S., Mohlin B., Brattstrom V., Paulin G., Pietila T. (2007) Long-term stability of Orthodontic Treatment and Patient Satisfaction. A Systematic review. The Angle Orthodontist, 77, 181–191. [DOI] [PubMed] [Google Scholar]
- 65. Fidler B.C., Årtun J., Joondeph D.R., Little R.M. (1995) Long-term stability of Angle Class II, Division 1 malocclusions with successful occlusal results at the end of active treatment. American Journal of Orthodontics and Dentofacial Orthopedics, 107, 276–285. [DOI] [PubMed] [Google Scholar]
- 66. Franchi L., Pavoni C., Faltin K., Jr, McNamara J.A., Jr, Cozza P. (2013) Long-term skeletal and dental effects and treatment timing for functional appliances in Class II malocclusion. The Angle Orthodontist, 83, 334–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Dyer K.C., Vaden J.L., Harris E.F. (2012) Relapse revisited—again. American Journal of Orthodontics and Dentofacial Orthopedics, 142, 221–227. [DOI] [PubMed] [Google Scholar]
- 68. Glenn G., Sinclair P.M., Alexander R.G. (1987) Nonextraction orthodontic therapy: posttreatment dental and skeletal stability. American Journal of Orthodontics and Dentofacial Orthopedics, 92, 321–328. [DOI] [PubMed] [Google Scholar]
- 69. Lang G., Alfter G., Göz G., Lang G.H. (2002) Retention and stability—taking various treatment parameters into account. Journal of Orofacial Orthopedics, 63, 26–41. [DOI] [PubMed] [Google Scholar]
- 70. Canut J.A., Arias S. (1999) A long-term evaluation of treated Class II division 2 malocclusions: a retrospective study model analysis. European Journal of Orthodontics, 21, 377–386. [DOI] [PubMed] [Google Scholar]
- 71. Kim T.W., Little R.M. (1999) Postretention assessment of deep overbite correction in Class II Division 2 malocclusion. The Angle Orthodontist, 69, 175–186. [DOI] [PubMed] [Google Scholar]
- 72. Lapatki B.G., Klatt A., Schulte-Mönting J., Stein S., Jonas I.E. (2004) A Retrospective Cephalometric Study for the Quantitative Assessment of Relapse Factors in Cover-Bite Treatment. Journal of Orofacial Orthopedics, 65, 475–488. [DOI] [PubMed] [Google Scholar]