Summary
Aim:
The aim of this study was to evaluate microleakage under orthodontic ceramic brackets bonded with direct and different indirect bonding techniques and adhesives using micro-computed tomography.
Materials and methods:
A total of 30 human maxillary premolars were randomly separated into five groups with six teeth in each group. In group I, teeth were bonded directly with Transbond XT (3M Unitek). In group II, group III, group IV, and group V, teeth were bonded through an indirect technique with Custom I.Q. (Reliance Orthodontic Products), Sondhi Rapid-Set (3M Unitek), RMbond (RMO), and Transbond IDB (3M Unitek), respectively, following the manufacturer’s instructions. Micro-CT system model 1172 of Skyscan (Kontich, Belgium) was used to scan all samples. NRecon (Skyscan) version 1.6, CT-Analyser V.1.11 (Skyscan), and TView (SkyScan, Bvba) software programs were used for microleakage evaluation. Microleakage values between the test groups were assessed using the Kruskal–Wallis test, while the Wilcoxon signed rank test was used for within-group comparisons. The level of significance was set at P < 0.05.
Results:
According to the Kruskal–Wallis analysis of variance test, there were no significant differences among the tested groups, with regard to volume and percentage (microleakage/region of interest × 100) of microleakage values (P < 0.05). The Wilcoxon signed rank test showed that coronal microleakage volume and percentage values significantly differed for RMbond and Transbond IDB groups.
Limitations:
In the study, only ceramic brackets were used and microleakage into mini gaps did not show up on the micro-CT image because 50% silver nitrate solution could not penetrate into mini gaps which are smaller than silver nitrate particles.
Conclusion:
Use of direct and indirect bonding techniques with different adhesives did not significantly affect the amount of microleakage.
Introduction
An improvement in aesthetic and hygienic treatment results has occurred following the advent of direct bonding of fixed attachments to the teeth with epoxy-derived resins. In 1974, Silverman and Cohen (1) put new bonding techniques into practice in order to more accurately and precisely locate brackets on teeth, prevent moisture contamination, and decrease doctor chair time for direct bonding techniques, and patient comfort has increased as a result of these advantages (2, 3). However, indirect bonding techniques also have several disadvantages, such as technique sensitivity, the need for an extra set of impressions, increased laboratory time, and the risk of adhesive leakage especially in gingival embrasures (4). Zachrisson and Brobakken (5) compared two different bonding techniques and showed that brackets fit the tooth surface more closely with fewer voids if the direct bonding technique was used.
Microleakage of dental adhesives, which is generated by polymerization shrinkage of methacrylates, can be observed between the adhesive material–enamel surfaces and/or interface of adhesive material–brackets. Microleakage emerging in this region can lead to microgaps by dissolving the adhesive, permitting the passage of bacteria, oral fluids, molecules, or ions, which may cause demineralization (6). Furthermore, microleakage may aggravate the physical properties of orthodontic bonding and banding materials. Polymerization shrinkage also varies from adhesive to adhesive and depends on the amount of filler, the diluents, and the percentage of monomer conversion (7).
A variety of in vitro methods have been used to image and measure microleakage, such as compressed air, neutron activation analysis, reversible radioactive adsorption, radioisotopes, electrochemical, scanning electron microscope, bacterial activity, dye penetration, and micro-computed tomography (µCT) (8–10).
In a previous orthodontic study, James et al. (7) showed the demineralization rate increase caused by microleakage under orthodontic fixed appliances. Uysal et al. (11) observed that when self-etching primers were used, increased leakage was found between the adhesive–enamel interfaces, while Uysal et al. (12) evaluated the microleakage patterns of different cement types for band cementation and found that conventional glass ionomer cements lead to increased microleakage. In addition, some studies have assessed the microleakage pattern of different brackets, composites, and curing types (6, 11, 13, 14). Furthermore, Öztürk et al. (15) and Yagci et al. (14) compared the influence of direct and indirect bonding techniques on microleakage and indicated that type of bonding technique did not significantly affect the amount of microleakage at the enamel–adhesive–bracket complex. All of the aforementioned studies conducted to assess amount of microleakage used two-dimensional (2D) methods, such as dye penetration. However, X-ray µCT technology would appear to offer significant advantages over 2D methods involving sectioning of specimens. With the development of µCT, researchers have been capable of evaluating the microleakage of dental restorative materials, and leakage area and volume determined by three-dimensional (3D) image analysis has been correlated with a variety of materials (10). Moreover, µCT has proven to be a powerful and viable technique in determining polymerization shrinkage and microleakage (16).
To our knowledge, no previous studies have so far assessed the effect of different bonding techniques with different curing methods on microleakage using 3D imaging methods. Thus, this study aimed to compare microleakage under orthodontic brackets bonded with different bonding techniques, using µCT and to determine which technique cause less microleakage and to generate clinical recommendations. The null hypothesis supposed that there were no significant differences under the orthodontic brackets with the different bonding techniques and curing methods.
Materials and methods
Teeth
The sample size calculation was obtained by MedCalc Statistical Software 14,12,0 (Ostend, Belgium) considering the use of a binomial two-tailed statistics with 80 per cent power (0.8) and alpha level of 5 per cent able to read a 20 per cent difference between the Meleo et al. article (17). Therefore, the sample size was defined as six teeth for each group for sample size calculation. A total of 30 human maxillary premolars, extracted for orthodontic reasons, were used in the present study. No teeth had any congenital anomaly, surface defects, decay, or restorations. After extraction, soft tissue remnants and plaques were removed with a scalpel, and the teeth were stored in disinfectant solution (0.5 per cent chloramines T). After remaining in this solution for 1 week, the teeth were washed with distilled water and stored in distilled water at room temperature until the experiments were performed (a maximum of 4 months).
Brackets
All teeth were bonded using a Signature III, ceramic (RMO, Denver, Colorado, USA) upper bicuspid bracket. Bracket base surface area was 11.1mm2.
Bonding procedure
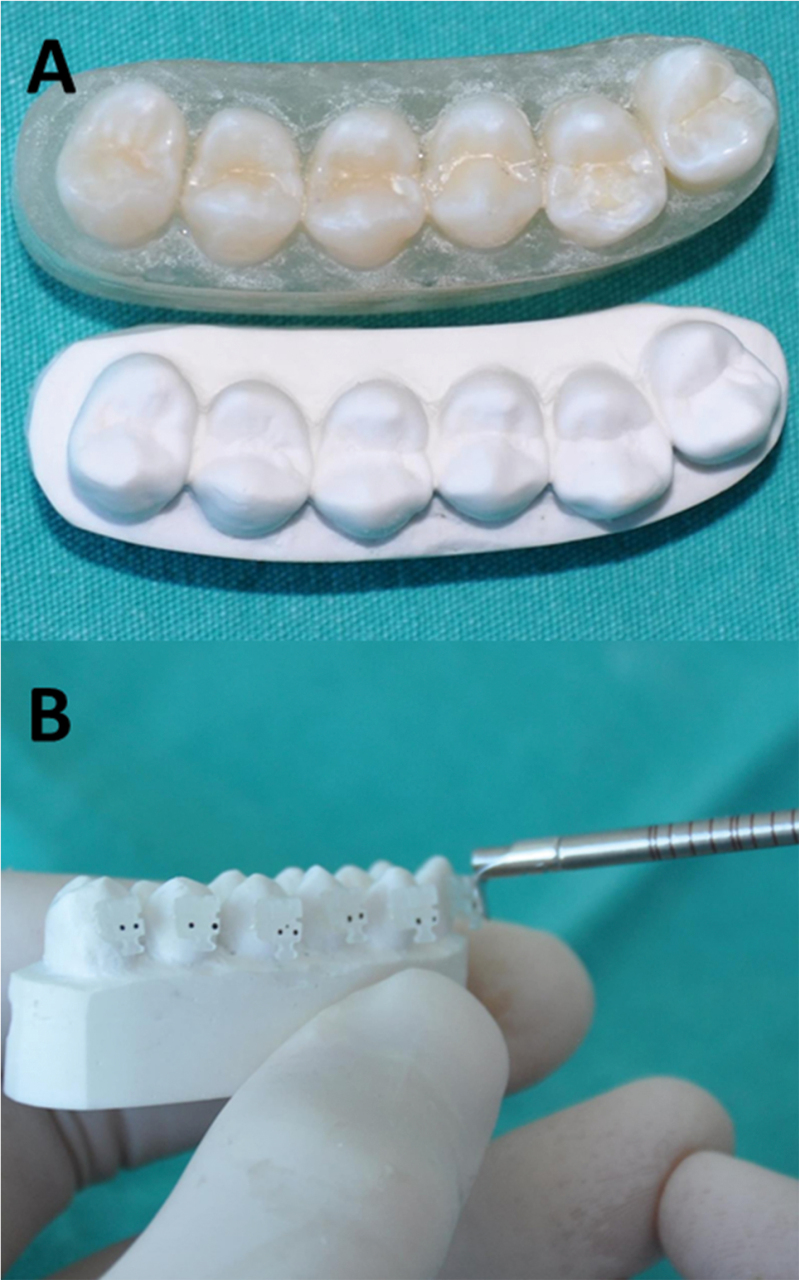
The teeth were randomly separated into five groups, with six teeth in each group. The teeth used in all groups were mounted on acrylic blocks, to simulate the mouth, and an arch form similar to a common dentoform was created (Figure 1). All acrylic blocks were allowed to cure, before storage in deionized water at 37°C. The entire laboratory process was carried out by the same author.
Figure 1.
Images of the teeth mounted on acrylic block and the hard-stone working model occlusal view (A), and each bracket was subjected to a 300g compressive force (B).
All teeth were polished with water/pumice slurry in brushes at a slow speed for 15 seconds, then rinsed and dried with an air stream for 10 seconds each. A 37 per cent phosphoric acid gel (3M Dental Products, St Paul, Minnesota, USA) was applied to the buccal surface of the teeth for 30 seconds, and they were then rinsed with water for 20 seconds and dried for 20 seconds with an oil- and moisture-free air spray. In all etched cases, the frosty white appearance of the etched enamel was apparent on the buccal surface. Then bonding process has been applied according to the groups. Details related to bonding materials are listed in Table 1.
Table 1.
Trade names, chemical compositions, and manufacturers of test materials
| Trade name | Chemical composition | Manufacturers | |
|---|---|---|---|
| Transbond XT | BISGMA | 3M Unitek, Monrovia, California, USA | |
| TEGDMA | |||
| 4-(Dimethylamino) benzeneethanol | |||
| Dl-Camphorquinone | |||
| Hydroquinone | |||
| Custom I.Q. | Part A | Part B | Reliance Orthodontics, Itasca, Illinois, USA |
| BISGMA | Bisphenol A diglycidylmethacrylate | ||
| Methylmethacrylate | Methylmethacrylate | ||
| Hydrofluoride methacrylate | Benzoyl peroxide | ||
| Sondhi Rapid-Set | Part A | Part B | 3M Unitek, Monrovia, California, USA |
| TEGDMA | TEGDMA | ||
| BISGMA | BISGMA | ||
| 2,2ʹ-(p-Tolylimino)diethanol | Dimethyl siloxane, reaction | ||
| Dimethyl siloxane, reaction product with silica | Benzoyl peroxide | ||
| Triphenylantimony | Hydroquinone | ||
| Hydroquinone | |||
| RMbond | RMbond LC Flowable Adhesiv | RMbond LC Bonding Resin | RMO, Denver, Colorado, USA |
| BISGMA | HEMA | ||
| TEGDMA | TMPTMA | ||
| EBPADMA | PMGMDM | ||
| Inorganic pigments | Photoinitiator system | ||
| Silan-treated barium | Acetone | ||
| Boro-alumino silicate glass | Ethanol | ||
| Silica | Poss | ||
| Photoinitiators | |||
| Transbond IDB | BISGMA | 3M Unitek, Monrovia, California, USA | |
| TEGDMA | |||
| 2,2ʹ-(p-Tolylimino)diethanol | |||
| Dimethyl siloxane, reaction product with | |||
| Silica | |||
| Triphenylantimony | |||
| Hydroquinone | |||
In the direct bonding group (group I), the procedure was as follows: a thin layer of Transbond XT (3M Unitek) light-cured primer was applied to each tooth and cured with light-emitting diode (LED; LED-C, Guilin Woodpecker, Medical Instrument Co. Ltd, Guangxi, PR China) for 10 seconds with an intensity of 1000 mW/cm2. Transbond XT (3M Unitek) adhesive was then applied to the brackets’ base and they were placed in the centre of the crown, with the centre of the bracket over the long axis of the tooth. Each bracket was subjected to a 300g compressive force using a force gauge (P1025-00, Leone, Firenze, Italy) for 10 seconds (Figure 1), after which excess adhesive was removed with a hand instrument, and the bracket was cured with an LED curing light for 10 seconds from the mesial and 10 seconds from the distal of each tooth. The specimens were stored in deionized water at 37°C before testing.
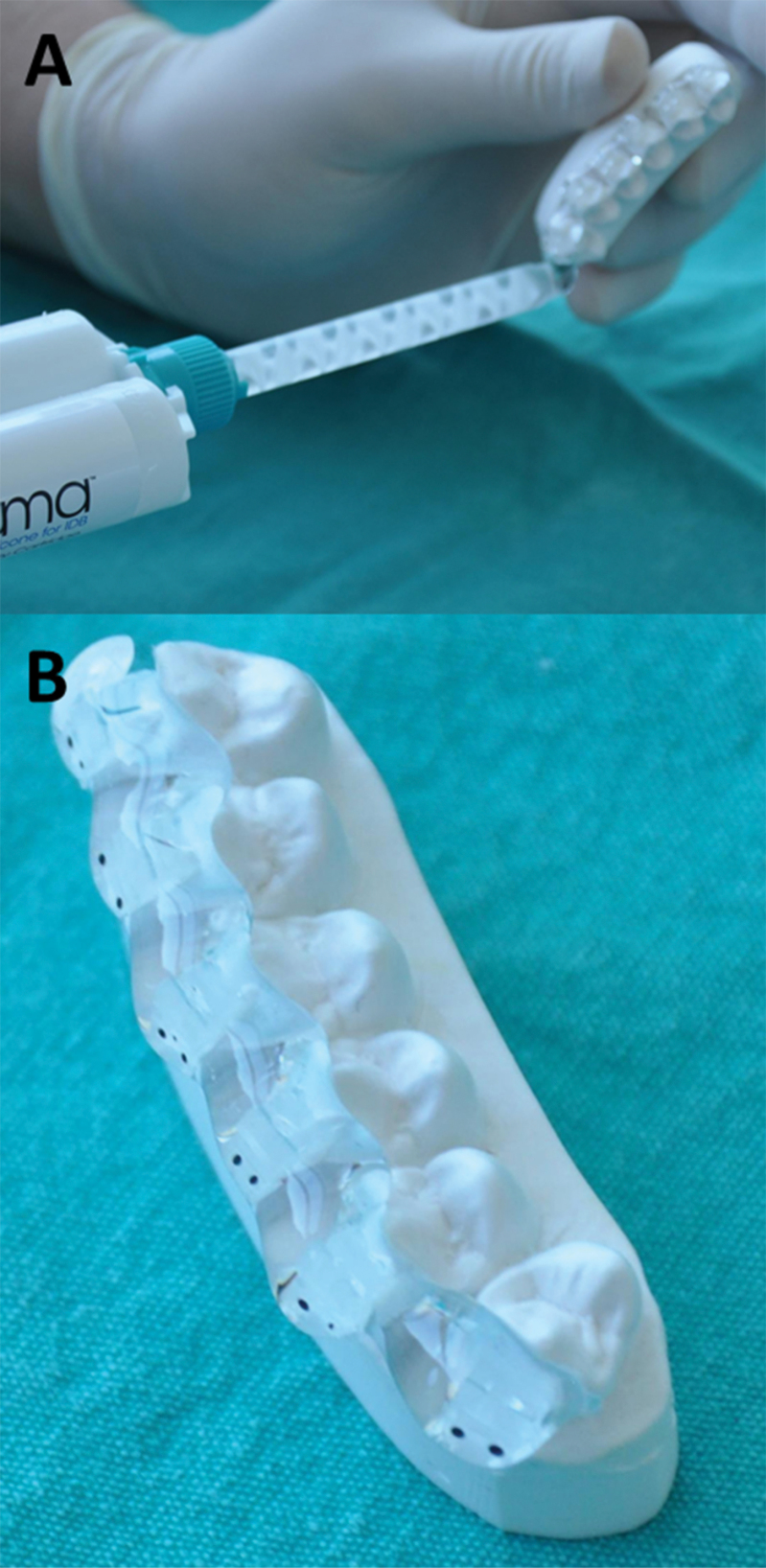
Teeth in the indirect bonding groups (groups II, III, IV, and V) were bonded indirectly, according to the manufacturer’s recommendations. They were mounted in acrylic block, and alginate impressions (Cavex Holland BV, Haarlem, The Netherlands) were taken. After the hard-stone (Amberok, Anadolu Dental Products, Istanbul, Turkey) working models were obtained (Figure 1), separating medium (Dentsply International Inc., York, Pennsylvania, USA) was painted on the stone and allowed to dry. Transbond XT Light Cure adhesive (in groups II, III, and V) and RMbond LC Model Adhesive (RMO) in group IV was placed on the mesh pad of the brackets. All brackets were placed on the model in the manner described previously, with regard to the direct bonding group, and the bracket was cured with an LED curing light for 15 seconds from the mesial and 15 seconds from the distal. This extended curing period was chosen to achieve complete polymerization of the composite materials on plaster models. Before forming the indirect bonding trays, the undercut areas were blocked out with a soft transparent silicone (Emiluma, Ortho Kinetics, and Vista, California, USA; Figure 2). A 0.040-in. (1mm) vacuum-formed essix (Raintree Essix Inc., Los Angeles, California, USA) was used as transfer tray. After the transfer tray material had set, the specimens were soaked in water for 20 minutes to dissolve the separating medium. The transfer tray was removed, and the adhesive bases were gently sandblasted, washed, and dried as advised by Sondhi (4).
Figure 2.
The undercut areas were blocked out with a soft transparent silicone (A) and particular attention was paid to protection of occlusal stop points (B).
Group II, a thin layer of Custom I.Q. part A was applied to each tooth surface and a thin layer of part B was applied at each bracket basis. The set was placed in position and pressed for 30 seconds. The trays were removed after 4 minutes.
Group III, a thin layer of Sondhi Rapid-Set resin A was applied to each tooth surface and a thin layer of resin B was applied at each bracket base. The bonding tray was brought into position and pressed for 30 seconds. The trays were removed after 2 minutes.
Group IV, RMbond LC bonding resin was applied to each tooth surface and RMbond LC Flowable Adhesive was applied to each bracket base. The bonding tray was brought into position and cured with an LED curing light for 10 seconds from the mesial and the distal of each tooth. After completion of bonding, the transfer trays were removed.
Group V, equal amounts of Transbond IDB (3M Unitek) part A and part B were mixed for 10 seconds in a disposable mixing well. A thin layer of mixed adhesive was applied to the tooth surface and each bracket base. The bonding tray was brought into position and pressed for 3 minutes. The trays were removed after 4 minutes. The teeth were removed from the acrylic block after bonding and immersed in silver nitrate 50 per cent w/v dye solution for 4 hours (10).
Micro-computed tomography
Skyscan model 1172 (Kontich, Belgium) was the µCT system model used to obtain the X-ray images. Initially, each one of the teeth was stabilized in the sample holder of the system, the X-ray source was set to 100 kV⁄100mA, and a 1mm aluminium filter was used to scan all samples. Each sample was rotated 360 degrees, with a rotation step of 0.50 degrees. The exposure time was 1300ms and the gain was set at 1.0. The magnification was set at 20, which resulted in a pixel size of 9 µm. NRecon (Skyscan) version 1.6 software was used in further cone-beam reconstruction of all the projected X-ray images.
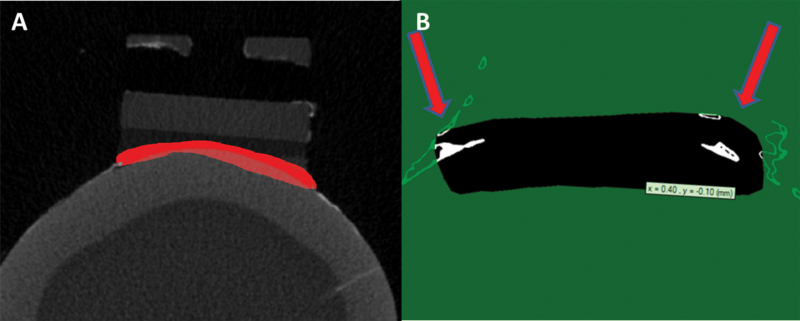
The surface areas of bracket bases were assessed using software TView (SkyScan, bvba), which allows observing of all microscans and identification of microleakage areas. Each microscan was cropped to have a smaller sample including the regions of interest (ROI ). Subsequently, 410–440 micro-CT slices to the 950 slices were selected and saved as BMP (Bit-Mapped Pixels) image files with a resolution of 2000×2000 pixels, showing 2D images. Then, these BMP files were exported to CT-Analyser (CTAn) V.1.11 (Skyscan) software. A circle ROI was selected on each data set slice by slice. All images were thresholded using an automated histogram analysis and binarized to allow the measurement process. Finally microleakage volume and percentage (microleakage/ROI × 100) were evaluated and this evaluation was done blindly (Figure 3). While microleakage analysis was made, each section was scored from the mesial, distal, coronal, and gingival margins to the brackets.
Figure 3.
Selecting area (ROI) for taking measurement of microleakages (A). The arrows indicate microleakages (B).
Statistical analysis
Microleakage values were calculated for each composite group’s composite enamel interface by CTAn computer software. Mesial, distal, coronal, and gingival microleakage volume and percentage values were obtained separately for each group. The normality of data distribution was evaluated by the Shapiro–Wilks test. The data did not show normal distribution, and no homogeneity of variances was observed between groups. Thus, statistical evaluation of microleakage values between test groups was performed using the Kruskal–Wallis test, and the Wilcoxon signed rank test was used for a within-group comparison. The level of significance was set at P < 0.05.
Results
According to the Kruskal–Wallis analysis of variance test, there were no significant differences in percentage and volume microleakage values among the tested groups (P ˃ 0.05). However, when only mean data were evaluated, the Costum IQ, Sondhi, and RMbond generally demonstrated higher values than Transbond XT and Transbond IDB, but these differences were not statistically significant (Table 2).
Table 2.
The volumetric (mm3) and percentage (%) microleakage values
| Transbond XT | Custom I.Q. | Sondhi Rapid-Set | RMbond | Transbond IDB | Kruskal ANOVA* | |
|---|---|---|---|---|---|---|
| Distal volume | 0.0010±0.0017a | 0.0204±0.0380a | 0.0269±0.0390a | 0.0092±0.0170a | 0.0005±0.0008a | Ns |
| Mesial volume | 0.0002±0.0004a | 0.0058±0.0082a | 0.0140±0.0057a | 0.0075±0.0132a | 0.0005±0.0010a | Ns |
| Gingival volume | 0.0005±0.0006a | 0.0109±0.0172a | 0.0173±0.0142a | 0.0096±0.0138a | 0.0009±0.0014a | Ns |
| Coronal volume | 0.0007±0.0010a | 0.0244±0.0426a | 0.0326±0.0509a | 0.0144±0.0223a | 0.0015±0.0022b | Ns |
| Distal percentage | 0.0356±0.0573a | 0.4261±0.7038a | 0.6765±0.9457a | 0.2389±0.4181a | 0.0251±0.0402a | Ns |
| Mesial percentage | 0.0132±0.0238a | 0.1732±0.2229a | 0.3653±0.4110a | 0.2537±0.4638a | 0.0219±0.0452a | Ns |
| Gingival percentage | 0.0242±0.0369a | 0.3087±0.4806a | 0.5124±0.5011a | 0.2949±0.4112a | 0.0272±0.0407a | Ns |
| Coronal percentage | 0.0217±0.0323a | 0.5787±0.8177a | 0.9673±1.4557a | 0.4497±0.6538b | 0.0530±0.0820b | Ns |
*According to Wilcoxon signed rank test, means of the same letter are not significantly different (α = 0.05). ANOVA, analysis of variance.
The Wilcoxon signed rank test showed that the coronal microleakage percentage for RMbond and the coronal microleakage volume and percentage values for Transbond IBD groups were significantly different within groups (P ˂ 0.05). There were no significant differences among the Costum IQ, Sondhi, and Transbond XT groups, with regard to percentage and volume microleakage values of IDB (Table 2).
Discussion
Although more accurate and efficient bracket placement and reduction chair time are advantages of indirect bonding techniques, the risk of adhesive leakage is increased because the brackets do not fit well to the tooth surfaces (4, 5). The majority of common indirect bonding techniques are based on a method described by Thomas (18). Although Thomas (18) recommended the use of chemically cured adhesives, excessive resin remained after bonding and removal required extra time when chemically cured composites were used. Consequently, thermal and light-cured adhesives have been used for the fabrication of the custom bracket base over the years (19–21). In the present study, we conducted microleakage analyses of two different bonding methods, direct and indirect bonding, and both adhesive types, chemical- and light-cured adhesives, in the indirect bonding technique.
The polymerization shrinkage of composite material may cause gaps and lead to microleakage (11–15). Microleakage is a major problem, as it leads to the diffusion of bacteria and organic/inorganic substances into the restorative material and the tooth structure area. Microleakage also causes an increase in post-operative pain and the likelihood of secondary caries lesions (22). Today, microleakage is determined by a variety of in vitro techniques such as air pressure, fluid filtration, dye penetration, and µCT (10, 11, 23), and the most commonly used evaluation method is that of dye penetration (11, 14, 15). Researchers use coloured dye agents or chemical tracers, which are able to penetrate into and stain. The specimens are then sectioned longitudinally through the research area and assessed with stereo optical-microscopy or scanning electron microscopy. The depth of dye penetration is recorded from only one or two slices obtained from sectioning; however, this does not represent the entire image of microleakage, which is 3D. Therefore, these methods have low reproducibility and precision. With the advent of new generation imaging techniques, detailed imaging information regarding the internal structures of objects can be non-destructively monitored. In an attempt to resolve the confusion on this issue, we selected X-ray µCT for examination of the gap formation between the enamel–adhesive–bracket complexes.
A 50 per cent silver nitrate solution, lead nitrate solution, and barium nitrate concentration have been used for the microleakage examination when using µCT assessment in previous studies (24). Nguyen (24) was exhibited that 50 per cent silver nitrate solution was an extremely chemically active, successful, and useful buffer formula for future use in µCT studies. Zhao et al. (25) and Eden et al. (10) determined the marginal leakage of composite restorations using µCT and used 50 per cent silver nitrate solution as a dye solution. The 50 per cent silver nitrate solution was also used for assessment between gap formations of the bracket–adhesive–tooth interface and specimens immersed for 4 hours in the present study.
Thermal cycles are often used to mimic thermal changes in the mouth for the production of thermal stress at the tooth–adhesive interface. However, several investigations have shown that number of thermal cycles is not associated with microleakage (26–28). Therefore, we did not perform thermocycling in the present study.
Several previous studies have evaluated the enamel–adhesive and adhesive–bracket interfaces for microleakage on both the gingival and coronal side of the tooth (6, 11, 13–15). The enamel–adhesive interface is critical in terms of white spot lesions because the accumulation of bacteria in this location can cause enamel demineralization. However, the adhesive–bracket interface can play a part in the bracket failure caused by bond degradation (6, 13). Each section was scored from the mesial, distal, coronal, and gingival margins to the brackets between both the bracket–adhesive and adhesive–enamel interface in the present study.
According to our results, there was no significant difference among the tested groups for percentage and volume microleakage values between enamel–bracket interfaces. However, when only the mean data were evaluated, the Costum IQ, Sondi, and RMbond generally demonstrated higher values than Transbond XT and IDB. These results were in accordance with those observed by Öztürk et al. (15) and Yagci et al. (14), who found that the microleakage scores were similar between the two bonding techniques. We did not find any microleakage between adhesive–bracket interfaces. Previous studies have demonstrated that greater gap formation occurs at the adhesive–enamel interface than at the adhesive–bracket (29–31). Microleakage around orthodontic brackets occurs, irrespective of the curing method, type of adhesive, and bracket type used (32). Arhun et al. (6) evaluated microleakage of metal and ceramic brackets and they showed that metallic brackets caused greater microleakage than ceramic brackets, while Arıkan et al. (13) assessed the effect of different light sources on microleakage and found that LED resulted in the lowest microleakage scores. In the present study, we used both ceramic brackets and LED curing units, which may decrease the gap formation or dimension. Furthermore, the adhesive layer is very thin and is pressed between the bracket and tooth, and excess of resin material turns up at the brackets, which can absorb some of the shrinkage. Alternatively, the bracket is free floating and shrinkage would pull it closer to the enamel, which is probably a greater advantage (33); thus, silver nitrate particles do not enter the narrowed gap formation. These factors may play a role in preventing microleakage between adhesive–bracket interfaces.
Comparison of the microleakage scores within the tested groups showed that the coronal microleakage amounts were higher than the gingival amounts in both the direct and indirect bonding groups. However, only the microleakage percentage values for RMbond and the microleakage volume and percentage values for the Transbond IBD groups were statistically significant. Studies interpreted the differences in the microleakage amount between coronal and gingival sides, as being related to the curvature of the tooth anatomy (6, 14, 15). In contrast with our results, Öztürk et al. (15) and Yagci et al. (14) found more leakage at the gingival sides than the coronal sides using both techniques. These disparities may be the result of assessment technique sensitivity, as they conducted leakage evaluation on only a few sections taken from teeth, so the results may not reflect the true situation for the entire tooth.
Limitations
One of limitations of our study was that only ceramic brackets were used, despite the frequent use of metal brackets in orthodontic clinics. The reason metal brackets were not preferred was that metal brackets creates artefacts and have a similar appearance to silver nitrate on micro-CT. Another limitation was that to use a 50% silver nitrate solution for the evaluation of microleakage. Although silver nitrate solution is often used in micro-CT studies (10, 24, 25), this solution cannot penetrate into gaps which are smaller than silver nitrate particles hence microleakage into mini gaps does not show up on the micro-CT image.
Conclusion
The type of bonding techniques used with different adhesive material did not significantly affect the amount of microleakage between enamel–composite–bracket complexes under ceramic brackets.
However, when assessed regionally, microleakage more occurs at coronal region in RMbond and Transbond IBD in indirect bonding groups. Further studies are required to explain these differences.
Acknowledgments
The authors have no conflict of interest related to this research. Brackets and adhesives for the study were generously donated by 3M Unitek, Reliance Orthodontics and RMO but none of the companies played no part in the design of the trial, in the statistical analysis, drafting of the manuscript, or in the approval of the final wording. We thank these companies and their staff.
References
- 1. Silverman E., Cohen M. (1974) Current adhesives for indirect bracket bonding. American Journal of Orthodontics, 65, 76–84. [Google Scholar]
- 2. Aguirre M.J., King G.J., Waldron J.M. (1982) Assessment of bracket placement and bond strength when comparing direct bonding to indirect bonding techniques. American Journal of Orthodontics, 82, 269–276. [DOI] [PubMed] [Google Scholar]
- 3. Milne J.W., Andreassen G.F., Jakobsen J.R. (1989) Bond strength comparison: a simplified indirect technique versus direct placement of brackets. American Journal of Orthodontics and Dentofacial Orthopedics, 96, 8–15. [DOI] [PubMed] [Google Scholar]
- 4. Sondhi A. (1999) Efficient and effective indirect bonding. American Journal of Orthodontics and Dentofacial Orthopedics, 115, 352–359. [DOI] [PubMed] [Google Scholar]
- 5. Zachrisson B.U., Brobakken B.O. (1978) Clinical comparison of direct versus indirect bonding with different bracket types and adhesives. American Journal of Orthodontics, 74, 62–78. [DOI] [PubMed] [Google Scholar]
- 6. Arhun N., Arman A., Çehreli S.B., Arikan S., Karabulut E., Gülsahi K. (2006) Microleakage beneath ceramic and metal brackets bonded with a conventional and an antibacterial adhesive system. The Angle Orthodontist, 76, 1028–1034. [DOI] [PubMed] [Google Scholar]
- 7. James J.W., Miller B.H., English J.D., Tadlock L.P., Buschang P.H. (2003) Effects of high-speed curing devices on shear bond strength and microleakage of orthodontic brackets. American Journal of Orthodontics and Dentofacial Orthopedics, 123, 555–561. [DOI] [PubMed] [Google Scholar]
- 8. Taylor M., Lynch E. (1992) Microleakage. Journal of Dentistry, 20, 3–10. [DOI] [PubMed] [Google Scholar]
- 9. Tjan A.H., Tan D.E. (1991) Microleakage at gingival margins of Class V composite resin restorations rebonded with various low-viscosity resin systems. Quintessence International, 22, 565–573. [PubMed] [Google Scholar]
- 10. Eden E., Topaloglu-Ak A., Topaloglu-Ak V., Cuijpers V., Frencken J. (2008) Micro-CT for measuring marginal leakage of Class II resin composite restorations in primary molars prepared in vivo. American Journal of Dentistry, 21, 393–397. [PubMed] [Google Scholar]
- 11. Uysal T., Ulker M., Ramoglu S.I., Ertas H. (2008) Microleakage under metallic and ceramic brackets bonded with orthodontic self-etching primer systems. The Angle Orthodontist, 78, 1089–1094. [DOI] [PubMed] [Google Scholar]
- 12. Uysal T., Ramoglu S., Ertas H., Ulker M. (2010) Different orthodontic band cements and the microleakage between cement/enamel and cement/band interfaces. American Journal of Orthodontics and Dentofacial Orthopedics, 137, 534–539. [DOI] [PubMed] [Google Scholar]
- 13. Arikan S., Arhun N., Arman A., Cehreli S.B. (2006) Microleakage beneath ceramic and metal brackets photopolymerized with LED or conventional light curing units. The Angle Orthodontist, 76, 1035–1040. [DOI] [PubMed] [Google Scholar]
- 14. Yagci A., Uysal T., Ulker M., Ramoglu S.I. (2010) Microleakage under orthodontic brackets bonded with the custom base indirect bonding technique. The European Journal of Orthodontics, 32, 259–263. [DOI] [PubMed] [Google Scholar]
- 15. Öztürk F., Babacan H., Nalçacı R., Kuştarcı A. (2009) Effects of direct and indirect bonding techniques on bond strength and microleakage after thermocycling. Korean Journal Orthodontics, 39, 393–401. [Google Scholar]
- 16. Sun J., Eidelman N., Lin-Gibson S. (2009) 3D mapping of polymerization shrinkage using X-ray micro-computed tomography to predict microleakage. Dental Materials, 25, 314–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Meleo D., Manzon L., Pecci R., Zuppante F., Bedini R. (2012) A proposal of microtomography evaluation for restoration interface gaps. Annali dell’Istituto superiore di sanità, 48, 83–88. [DOI] [PubMed] [Google Scholar]
- 18. Thomas R.G. (1979) Indirect bonding: simplicity in action. Journal of Clinical Orthodontics, 13, 93–106. [PubMed] [Google Scholar]
- 19. Miles P. (2000) A comparison of retention rates of brackets with thermally-cured and light-cured custom bases in indirect bonding procedures. Australian Orthodontic Journal, 16, 115–117. [PubMed] [Google Scholar]
- 20. Read M., O’Brien K. (1990) A clinical trial of an indirect bonding technique with a visible light-cured adhesive. American Journal of Orthodontics and Dentofacial Orthopedics, 98, 259–262. [DOI] [PubMed] [Google Scholar]
- 21. Kalange J.T. (1999) Ideal appliance placement with APC brackets and indirect bonding. Journal of Clinical Orthodontics, 33, 516–526. [PubMed] [Google Scholar]
- 22. Gladwin M., Bagby M. (2004) Clinical Aspects of Dental Materials Theory, Practice, and Cases. Lippincott Williams & Wilkins, Baltimore, MD, pp. 47–57. [Google Scholar]
- 23. Yavuz I., Aydin H., Ulku R., Kaya S., Tumen C. (2006) A new method: measurement of microleakage volume using human, dog and bovine permanent teeth. Electronic Journal of Biotechnology, 9, 8–17. [Google Scholar]
- 24. Nguyen C. (2007) A new in vitro method for the study of micro-leakage of dental restorative materials. Thesis, The University of Adelaide. [Google Scholar]
- 25. Zhao X., Li S., Gu L., Li Y. (2014) Detection of marginal leakage of class V restorations in vitro by micro-computed tomography. Operative Dentistry, 39, 174–180. [DOI] [PubMed] [Google Scholar]
- 26. Celiberti P., Lussi A. (2005) Use of a self-etching adhesive on previously etched intact enamel and its effect on sealant microleakage and tag formation. Journal of Dentistry, 33, 163–171. [DOI] [PubMed] [Google Scholar]
- 27. Aguiar F., Dos Santos A., Franca F., Paulillo L., Lovadino J. (2002) A quantitative method of measuring the microleakage of thermocycled or non-thermocycled posterior tooth restorations. Operative Dentistry, 28, 793–799. [PubMed] [Google Scholar]
- 28. Bedran-de-Castro A., Cardoso P., Ambrosano G., Pimenta L. (2003) Thermal and mechanical load cycling on microleakage and shear bond strength to dentin. Operative Dentistry, 29, 42–48. [PubMed] [Google Scholar]
- 29. Cucu M., Driessen C., Ferreira P. (2002) The influence of orthodontic bracket base diameter and mesh size on bond strength. SADJ: Journal of the South African Dental Association, 57, 16–20. [PubMed] [Google Scholar]
- 30. Bishara S.E., Ostby A.W., Laffoon J.F., Warren J. (2007) Shear bond strength comparison of two adhesive systems following thermocycling: a new self-etch primer and a resin-modified glass ionomer. The Angle Orthodontist, 77, 337–341. [DOI] [PubMed] [Google Scholar]
- 31. Canbek K., Karbach M., Gottschalk F., Erbe C., Wehrbein H. (2013) Evaluation of bovine and human teeth exposed to thermocycling for microleakage under bonded metal brackets. Journal of Orofacial Orthopedics, 74, 102–112. [DOI] [PubMed] [Google Scholar]
- 32. Abdelnaby Y.L., Al-Wakeel E.E. (2010) Influence of modifying the resin coat application protocol on bond strength and microleakage of metal orthodontic brackets. The Angle Orthodontist, 80, 378–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Oesterle L.J., Newman S.M., Shellhart W.C. (2001) Rapid curing of bonding composite with a xenon plasma arc light. American Journal of Orthodontics and Dentofacial Orthopedics, 119, 610–616. [DOI] [PubMed] [Google Scholar]