Summary
Objective:
Economic evaluations provide an important basis for allocation of resources and health services planning. The aim of this study was to evaluate and compare the costs of correcting anterior crossbite with functional shift, using fixed or removable appliances (FA or RA) and to relate the costs to the effects, using cost-minimization analysis.
Design, Setting, and Participants:
Sixty-two patients with anterior crossbite and functional shift were randomized in blocks of 10. Thirty-one patients were randomized to be treated with brackets and arch wire (FA) and 31 with an acrylic plate (RA). Duration of treatment and number and estimated length of appointments and cancellations were registered. Direct costs (premises, staff salaries, material, and laboratory costs) and indirect costs (the accompanying parents’ loss of income while absent from work) were calculated and evaluated with reference to successful outcome alone, to successful and unsuccessful outcomes and to re-treatment when required. Societal costs were defined as the sum of direct and indirect costs.
Interventions:
Treatment with FA or RA.
Results:
There were no significant differences between FA and RA with respect to direct costs for treatment time, but both indirect costs and direct costs for material were significantly lower for FA. The total societal costs were lower for FA than for RA.
Limitations:
Costs depend on local factors and should not be directly extrapolated to other locations.
Conclusion:
The analysis disclosed significant economic benefits for FA over RA. Even when only successful outcomes were assessed, treatment with RA was more expensive.
Trial registration:
This trial was not registered.
Protocol:
The protocol was not published before trial commencement.
Introduction
Economic evaluations of health care interventions are assuming increasing importance (1). Cost-effective healthcare requires assessment of the economic implications of different interventions (2). Less cost-effective healthcare for one condition might lead to limitation of services for other important conditions. As part of the overall allocation of resources and planning of health services, it is probable that in future, there will be closer scrutiny of economic aspects of publicly funded orthodontic services: not only will evidence of clinical effectiveness of treatment be required, but also economic data affirming value for money ought to be considered (3).
A comparative analysis of alternative courses of action in terms of their costs and consequences is defined as economic evaluation (4). To gather evidence and to be able to compare the expected costs and consequences of different procedures, four different economic evaluation types can be used. A cost-effectiveness analysis is characterized by analysis of both costs and outcomes. A cost-minimization analysis, which is a form of cost-effectiveness analysis, is used when outcomes of treatment alternatives are equivalent (e.g. anterior crossbite will be corrected irrespective of which treatment is applied) and the aim is to identify which alternative has the lower cost. A utility-based outcome is used in cost-utility analysis, for instance to compare quality of life following treatment. Biological, physical, sociological, or psychological parameters are measured as to how they influence a person′s well-being. In a cost-benefit analysis the consequences (effects) are expressed in monetary units (4).
The reported prevalence of all types of anterior crossbites varies from 2.2 to 12 per cent, depending, for example, on the age and ethnic group of the children studied and whether or not edge-to-edge relationships are included in the data (5–9). For cases of anterior crossbite with functional shift, early treatment is recommended, in order to prevent adverse long-term effects on growth and development of the teeth and jaws, such as disturbance of temporal and masseter muscle activity in children and increased risk of craniomandibular disorders in adolescents (6, 8, 10–12).
Anterior crossbite with functional shift can be corrected by removable appliance (RA) or fixed appliance (FA) therapy (10, 11, 13–15). A recent randomized-controlled trial (RCT) with a 2-year post-retention follow-up indicated that both treatment approaches can achieve similar clinical outcomes (16). Under these circumstances the combined clinical and economic outcomes should be considered. To our knowledge there is to date no study comparing the cost-effectiveness of early correction of anterior crossbite with FAs or RAs. As both methods achieve similar outcomes, a cost-minimization analysis is an appropriate form of economic evaluation. Thus, the aim of this study was to evaluate and compare the costs of FA or RA therapy to correct anterior crossbite with functional shift and to relate the costs to the effects. It was hypothesized that RA and FA would be equally cost-effective.
Subjects and methods
Trial design
This cost-minimization analysis was based on a two centre RCT that performed the effectiveness of anterior crossbite correction including a 2-year follow-up of the corrections. All patients and their parents gave written informed consent before being enrolled in the study. The Ethics Committee of Lund, Sweden, approved the protocol and the informed consent form, reg.no. 3334/2004.
Participants, eligibility, and setting
The subjects comprised 62 patients, 25 girls and 37 boys, [mean age 9.8 years, standard deviation (SD) 1.43], all with at least one incisor in anterior crossbite.
All patients were recruited consecutively from one Public Dental Clinic in Malmö, Skåne County Council, Sweden and the Department of General Paediatric Dentistry, Faculty of Odontology, Malmö University, Malmö, Sweden. The patients met the following inclusion criteria:
- early to late mixed dentition,
- anterior crossbite involving one or more maxillary incisors, causing functional shift
- moderate space deficiency in the maxilla, up to 4mm,
- a non-extraction treatment plan, ANB angle >0°, and
- no previous orthodontic treatment.
After randomization to removable or fixed appliance treatment (RA or FA group respectively) the patients were treated by a general practitioner under the supervision of two orthodontists, according to a preset concept.
Interventions
Removable appliance
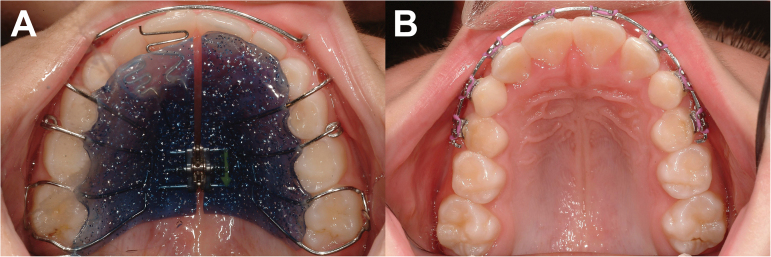
The appliance comprised an acrylic plate, with a protrusion spring for each incisor in anterior crossbite (Figure 1A). Once a month the protrusion springs were activated until normal incisor overjet was achieved. To avoid vertical interlock between the incisors in crossbite and the mandibular incisors, lateral occlusal composite was used. This coverage also increases the retention of the appliance. The occlusal coverage was removed as soon as the anterior crossbite was corrected. An inactive expansion screw was activated during the treatment period only if it was judged to comply with the natural transverse growth of the jaw. The patient was firmly instructed by the dentist to wear the appliance day and night, except for meals and tooth-brushing. Progress was evaluated every 4 weeks, and the current appliance then served as a retainer for the following 3 months.
Figure 1.
Occlusal view of the removable appliance (A), and the fixed orthodontic appliance (B).
Fixed appliance
The appliance consisted of stainless steel brackets (Victory, slot .022, APC PLUS adhesive coated bracket system, 3M Unitek, USA). Usually, eight brackets were bonded to the maxillary incisors, deciduous canines and either to the first deciduous molars or the first premolars, if erupted (Figure 1B). A standard straight-wire concept designed for light forces were used to treat all patients (17). The first arch-wire was: .016 heat-activated nickel-titanium (HANT), then .019 × .025 HANT, and finally .019 × .025 stainless steel wire. To raise the bite, and avoid vertical interlock between the incisors in crossbite and the mandibular incisors, composite (Point Four 3M Unitek, US) was bonded to the occlusal surfaces of both mandibular second deciduous molars. The composite was removed as soon as the anterior crossbite was corrected. Progress was evaluated every 4 weeks, and the same FA then served as a passive retainer for the following 3 months.
Outcomes
Orthodontic outcome measures
The measures to be assessed in the trial were: success rate of anterior crossbite correction (positive overjet for incisors) and overjet in millimetres at two time-points: after active treatment and 2 years post-retention. The overjet was measured with a digital sliding calliper (Digital 6, 8M007906, Mauser-Messzeug GmbH, Oberndorf/Neckar, Germany). All measurements on study casts were blinded, that is the examiner was unaware which treatment the patient had received. One examiner undertook all measurements.
Cost measures
‘Direct costs’ comprised material costs and treatment time needed for manpower of all sessions and for each patient. Material costs (i.e. orthodontic brackets, wires, and bonding, materials for impression, consumables, laboratory material, and fees, etc.) were compiled and calculated according to average commercial prices. Treatment time costs included the costs of the dental equipment, premises, cleaning, and maintenance. It was calculated according to average commercial prices in Sweden; these figures were used to establish estimated costs for each unit in the study. Similarly, staff salaries, including payroll tax, were calculated for the supervising orthodontists, general dental practitioners and assistants, based on a previous economic calculation from 2010 and upgraded in accordance with the Consumer Price Index for 2013 (18). All estimates of treatment time costs were calculated in Swedish currency, at SEK 937 (€108) per hour for a general practitioner. In addition, the number of appointments, scheduled and emergency appointments and cancellations, was noted.
‘Indirect costs’ were defined as loss of income (wages plus social security costs), assuming that the patients’ parents were absent from work to accompany the patient to the orthodontic appointment. Data sourced from Swedish National Bureau of Statistics (http://www.scb.se) gave the wages of an average Swedish worker as SEK 243 or €28 per hour. One parent accompanied the patient to the appointments. The parent’s absence from work was estimated at 80–90 minutes per appointment, i.e 20–30 minutes for the appointment and 60 minutes’ travelling time, for parent and child, to and from the dental clinic. Appointments for insertion and removal of FA were scheduled at 30 minutes each; all other appointments for FA or RA were scheduled at 20 minutes each.
The sum of direct and indirect costs was defined as ‘societal costs’. The cost-analysis was based on the intention-to-treat (ITT) principle, i.e. the analysis included data on costs of re-treatment due to non-compliance or relapse.
All costs were based on 2013 prices and were expressed in Euros (€), SEK 100 = €11.56 on mean currency value (http://www.riksbank.se).
Cost-minimization analysis
A cost-minimization analysis (CMA) was chosen, since evidence was found that the treatment alternatives have identical outcomes (i.e. irrespective of which treatment alternative is applied, anterior crossbite will be corrected).
CMa was calculated as follows:
CMa = Societal costs divided by the number of patients. This was calculated for:
-
1.
The mean costs of successful cases only on completion of active treatment in both groups, i.e.
Societal costs for all 31 successful FA treatments/the 31 successful FA patients.
Societal costs for all 30 successful RA treatments/the 30 successful RA patients.
-
2.
The mean costs of the successful and unsuccessful cases on completion of active treatment in both groups, i.e.
Societal costs for all 31 FA treatments / the 31 successful patients.
Societal costs for all 31 RA treatments / the 30 successful patients.
Finally, the societal costs for all patients were calculated, following the ITT approach, including the 2-year follow-up period and all re-treatments, for the total number of patients in each group. Thus, the costs of two re-treatments in the FA and two re-treatments in the RA group were added to the societal costs to calculate the mean societal costs including re-treatments. This implies: CMb = societal costs including re-treatment/number of patients, i.e.
Societal costs for 33 treatments in the FA group/the 31 patients.
Societal costs for 33 treatments in the RA group/the 31 patients.
Randomization
An independent person randomized the patients in blocks of 10, as follows: first preparation of seven opaque envelopes with 10 sealed notes in each (five notes for each group) was performed. Consequently, for every new child in the study, a note was picked from the first envelope. When the envelope was empty, a second envelope was opened, and 10 new notes were picked successively as children were recruited to the study. Six more times this routine was reproduced. One investigator had the responsibility of the envelopes, and was contacted for randomly extraction of a note and then the clinician was informed to which treatment was to be carried out.
Statistical analysis
SPSS software (version 21.0) was used for statistical analysis of the data. The arithmetic means, SD, and confidence intervals were calculated. A Kolmogorov–Smirnov test indicated that the variables did not have a normal distribution and therefore the Mann–Whitney U test was used to compare costs between the groups. A P value of less than 5 per cent (P < 0.05) was regarded as statistically significant.
Results
Participant flow
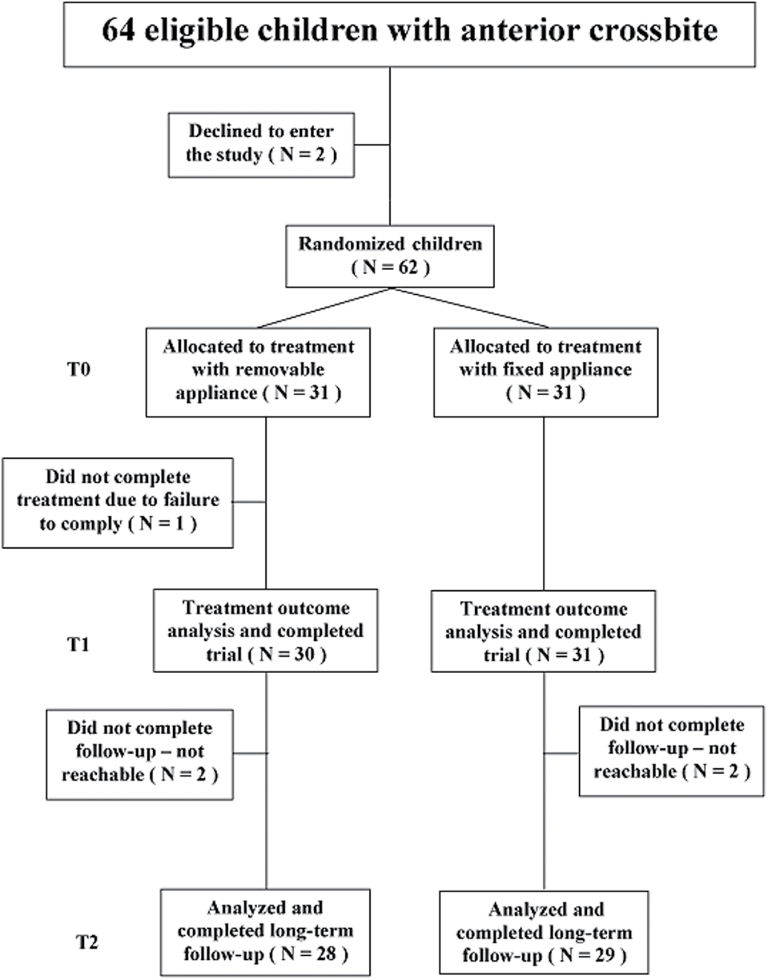
Of the 31 patients in the RA group, one patient with poor compliance failed to complete the study. All 31 patients in the FA group were treated successfully. The mean treatment time, including retention of 3 months, was 5.5 months (SD 1.4) in the FA group and 6.9 months (SD 2.8) in the RA group. During the 2-year post-treatment follow-up, one subject in the RA group experienced a relapse. At the 2-year post-retention evaluation, relapse was observed in two subjects in the FA group. These four patients, two in each group, needed retreatment and this was undertaken with FAs. The patients needing retreatment showed no differences in baseline characteristics from subjects who were treated successfully. The patient flow chart is presented in Figure 2.
Figure 2.
Flow diagram of children in the mixed dentition stage with anterior crossbite.
Societal costs
The mean societal costs for patients with successful outcomes were €630 (SD 198) for FA (31/31) and €945 (SD 302) for RA (30/30) (P < 0.000), (Table 1).
Table 1.
Mean societal costs, direct costs of materials, direct costs for treatment time and indirect costs in Euros. Successful patients only: fixed appliance (FA) n = 31, removable appliance (RA) n = 30. Successful and unsuccessful outcomes: FA, n = 31; RA, n = 31. Including re-treatment: FA, n = 33; RA, n = 33.
| FA | 95% CI for mean | RA | 95% CI for mean | Difference of means | 95% CI for difference | Group difference P-value | |||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Lower–Upper | Mean | SD | Lower–Upper | Lower–Upper | |||
| Successful patients only | |||||||||
| Societal costs | 630 | 198 | 557–702 | 945 | 302 | 832–1057 | 315 | 183–447 | 0.000 |
| Direct costs–material | 32 | 3 | 31–33 | 227 | 79 | 198–257 | 195 | 165 to 223 | 0.000 |
| Direct costs–treatment time | 323 | 102 | 285–360 | 371 | 135 | 320–421 | 48 | −13 to 108 | 0.170 |
| Indirect costs | 275 | 101 | 238–312 | 346 | 104 | 308–385 | 71 | 18–121 | 0.006 |
| Successful and unsuccessful | |||||||||
| Societal costs | 630 | 198 | 557–702 | 972 | 307 | 860–1092 | 342 | 183 to 450 | 0.000 |
| Direct costs–material | 32 | 3 | 31–33 | 234 | 81 | 205–266 | 202 | 166 to 225 | 0.000 |
| Direct costs–treatment time | 323 | 102 | 285–360 | 382 | 137 | 331–435 | 59 | −14 to 110 | 0.139 |
| Indirect costs | 275 | 101 | 238–312 | 356 | 106 | 318–398 | 81 | 19 to 124 | 0.006 |
| Including re-treatment | |||||||||
| Societal costs | 678 | 361 | 546–810 | 1031 | 511 | 824–1117 | 353 | 127–578 | 0.000 |
| Direct costs–material | 35 | 15 | 30–40 | 231 | 82 | 199–261 | 196 | 165–226 | 0.000 |
| Direct costs–treatment time | 351 | 197 | 278–423 | 417 | 262 | 315–451 | 66 | −52 to 184 | 0.189 |
| Indirect costs | 293 | 153 | 236–349 | 383 | 200 | 304–412 | 90 | 0–181 | 0.008 |
The mean societal costs, for both successful and unsuccessful outcomes, were €630 (SD 198) for the FA group (31/31) and €972 (SD 307) for the RA group (31/30) (P < 0.000).
The total mean societal costs for all 31 patients, including two retreatments in each group, were €678 (SD 361) for the FA group (31/29) and €1031 (SD 511) for the RA group (31/29) (P < 0.005), (Table 1).
Direct costs—material
For patients with successful treatment outcomes (31 FA and 30 RA) the mean material costs were €32 (SD 3) for FA and €227 (SD 79) for RA (P < 0.000). The mean material costs for both successful and unsuccessful outcomes (31/31 FA and 31/30 RA) were €32 (SD 3) for FA and €234 (SD 81) for RA (P < 0.000). Including re-treatment, the mean material costs were €35 (SD 15) for FA and €231 (SD 82) for RA (P < 0.000), (Table 1).
Direct costs—treatment time
The mean total treatment time and costs for the patients with successful treatment outcomes (31 FA and 30 RA) were 179 minutes/€323 (102 SD) for FA and 205 minutes/€371 (SD 135) for RA. The mean total treatment time and costs, for both successful and unsuccessful outcomes, (31 in each group) were 179 minutes/€323 (SD 102) for the FA and 212 minutes/€382 (SD 137) for the RA group. Including the re-treatments, the mean total treatment time and costs for the FA group were 194 minutes/€351 (SD 197) and 231 minutes/€417 (SD 262) for the RA group. With respect to treatment time costs, no significant difference was found between FA and RA for any of the groups (Table 1).
Number of appointments
The mean number of appointments for patients with successful treatment outcomes was 7.2 for FA patients and 9.2 for RA patients (P = 0.005). For successful and unsuccessful outcomes, the number of appointments was 7.2 for FA and 9.6 for RA (P = 0.005). Including re-treatment, the mean number of appointments was 7.8 for the FA group and 10.1 for the RA group, with no significant difference between the groups with respect to retreatment.
In each treatment group, an average of one emergency/unscheduled appointment was recorded per treatment, most frequently for loss of brackets in the FA group or fractured clasps or acrylic plate edges in the RA group.
Indirect costs
The mean indirect costs for successful treatments were €275 (SD 101) for the FA group and €346 (SD 104) for the RA group (P < 0.01). The mean indirect costs for both successful and unsuccessful outcomes were €275 (SD 101) for the FA group and €356 (SD 106) for the RA group (P < 0.01). When retreatment was included, the indirect cost for the FA group was €293 (SD 153) and €383 (SD 200) for the RA group, with no significant differences between the groups (Table 1).
The indirect costs comprised 44% of the societal costs for FA therapy and 37% for RA therapy.
Side effects
Intra oral radiographs of the maxillary incisors were routinely taken before and after treatment and no root resorptions could be diagnosed in any of the groups. In addition, there was no lateral incisor that interfered with any maxillary canine in eruption during the treatments.
In both groups, the patients showed good to acceptable oral hygiene before and during the treatments. The presence of white spot lesions before and after treatment was also recorded and no new white spot lesion had occurred in the groups.
Discussion
Main findings
Economic evaluations of orthodontic treatment are seldom presented, but provide important information for planning and management of orthodontic services. This is the first study to evaluate cost-minimization of correction of anterior crossbite by FAs or RAs based on the outcomes of an RCT.
The results reject the initial hypothesis that FA and RA treatment will be equally cost-effective and show that the FA method is the more cost-effective alternative. Thus, comparison of societal costs disclosed that RA treatment was more expensive than FA treatment. This was attributable mainly to the higher material costs in the RA group, including laboratory fabrication of the appliances by a dental technician. Moreover, treatment time was found to be significantly longer in the RA group: this required more appointments, resulting in higher treatment time costs and indirect costs.
Both appliances achieved high success rates for correction of anterior crossbite. However, the RA is highly reliant on patient cooperation: thus in theory, the costs for RA therapy could be even higher in a less compliant patient group than that in the present study.
Side effects like root resorptions and white spot lesions were not found in the groups, and the reason for the infrequent side effects was probably due to the short treatment durations, i.e. mean 5.5 and 6.9 months. In both groups, efforts were made to use as low forces as possible. In the FA group a well-known low force system was used (17) and another study (19) has disclosed successful treatment results in 9–10 year-olds treated with 2×4 FA to correct anterior crossbite.
Generalizability
For economic evaluations, an RCT offers several advantages. The random allocation of subjects reduces bias and confounding variables by ensuring that both known and unknown determinants of outcome are evenly distributed among the subjects. The prospective design also ensures that such factors as baseline characteristics, treatment progression, treatment time, number of appointments, and side effects can be strictly controlled and accurately observed. In addition, this cost evaluation was based on the ITT approach, meaning that all cases, successful or not, were included in the analysis.
A search of the literature has failed to identify any study comparing the costs of FA and RA therapy for correction of anterior crossbite. However, a recent study of correction of posterior crossbite in the mixed dentition, analysing the cost-effectiveness of FAs and RAs (Quad-helix versus removable expansion plate) disclosed that the FA was more cost-effective (18). Two other recent studies have evaluated costs related to different types of orthodontic retention devices (20, 21). One study, of three equally efficient retention methods, reported that a canine-to-canine retainer was less cost-effective than stripping or a positioner (20). The other study reported that from all perspectives, a vacuum-formed retainer was more cost-effective than a Hawley retainer (21).
Limitations
It is also important to bear in mind that costs depend on local factors such as staff, technician costs, urban versus rural areas, etc. and thus the figures presented in the present study should not be directly extrapolated to other locations. It may be noted that the dental laboratories are competitive and the laboratory used in this study belonged to the university and such a laboratory must use the average tariff to be neutral. Furthermore, an adhesive brackets system was used and the cost of each bracket was based on an average price of 3.0 euros. Also, the arch-wire prices were average prices (2.0 euros for HANT and 0.8 euros for a steel arch-wire).
The patients in the present study were treated by an experienced general practitioner. In Sweden, especially in urban areas, many general practitioners undertake RA therapy; as these practices are often located nearer the patients’ homes than the orthodontic specialist clinic, the indirect costs would be lower, possibly compensating for the more expensive direct costs of materials for this appliance. On the other hand, in many countries FA treatment is more often provided by a specialist in orthodontics. Conceivably, specialist FA treatment would further reduce treatment time, increasing the difference in treatment time costs between the two appliances, thus further favouring FA treatment.
While the present study addressed the question of cost-effectiveness, other important aspects of early intervention to correct anterior crossbite with functional shift also warrant investigation, such as the perceptions of the patient pain and discomfort associated with treatment by FAs or RAs. This will be evaluated in a forthcoming study.
Conclusions
The results confirm that for correction of anterior crossbite with functional shift, FAs offer significant economic benefits over RAs, including lower direct costs for materials and lower indirect costs. Even when only successful outcomes were considered, treatment with a RA was more expensive.
Funding
This study was supported by grants from the Swedish Dental Society and Skåne Regional Council, Sweden.
References
- 1. Elixhauser A. Luce B.R. Taylor W.R. and Reblando J (1993) Health care CBA/CEA: an update on the growth and composition of literature. Medical Care, 31, 1–149. [DOI] [PubMed] [Google Scholar]
- 2. Kumar S. Williams A.C. and Sandy J.R (2006) How do we evaluate the economics of health care? European Journal of Orthodontics, 28, 513–519. [DOI] [PubMed] [Google Scholar]
- 3. Buck D. (2000) Economic evaluation and dentistry. Dental Update, 7, 66–73. [DOI] [PubMed] [Google Scholar]
- 4. Drummond M.F. Sculpher M.J. Torrance G.W. O’Brian B. and Stoddart G.L (2005) Methods for the Economic Evaluation of Health Care Programmes. Oxford Medical Publications, Oxford. [Google Scholar]
- 5. Keski-Nisula K. Lehto R. Lusa V. Keski-Nisula L. and Varrela J (2003) Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition. American Journal of Orthodontics and Dentofacial Orthopedics, 124, 631–638. [DOI] [PubMed] [Google Scholar]
- 6. Karaiskos N. Wiltshire W.A. Odlum O. Brothwell D. and Hassard T.H (2005) Preventive and interceptive orthodontic treatment needs of an inner-city group of 6- and 9-year-old Canadian children. Journal of the Canadian Dental Association, 71, 649a–649e. [PubMed] [Google Scholar]
- 7. Lux C.J. Ducker B. Pritsch M. Komposch G. and Niekusch U (2009) Occlusal status and prevalence of occlusal malocclusion traits among 9-year-old schoolchildren. European Journal of Orthodontics, 31, 294–999. [DOI] [PubMed] [Google Scholar]
- 8. Schopf P. (2003) Indication for and frequency of early orthodontic therapy or interceptive measures. Journal of Orofacial Orthopedics, 64, 186–200. [DOI] [PubMed] [Google Scholar]
- 9. Thilander B. and Myrberg N (1973) The prevalence of malocclusion in Swedish schoolchildren. Scandinavian Journal of Dental Reseach, 81, 12–20. [DOI] [PubMed] [Google Scholar]
- 10. Lee B.D. (1978) Correction of cross-bite. Dental Clinics of North America, 22, 647–668. [PubMed] [Google Scholar]
- 11. Ngan P. Hu A.M. and Fields H.W. Jr (1997) Treatment of class III problems begins with differential diagnosis of anterior crossbites. Pediatric Dentistry, 19, 386–395. [PubMed] [Google Scholar]
- 12. Väkiparta M.K. Kerosuo H.M. Nyström M.E. and Heikinheimo K.A (2005) Orthodontic treatment need from eight to 12 years of age in an early treatment oriented public health care system: a prospective study. The Angle Orthodontist, 75, 344–349. [DOI] [PubMed] [Google Scholar]
- 13. Galbreath R.N. Hilgers K.K. Silveira A.M. and Scheetz J.P (2006) Orthodontic treatment provided by general dentists who have achieved master′s level in the Academy of General Dentistry. American Journal of Orthodontics and Dentofacial Orthopedics, 129, 678–686. [DOI] [PubMed] [Google Scholar]
- 14. Rabie A.B. and Gu Y (1999) Management of pseudo Class III malocclusion in southern Chinese children. British Dental Journal, 186, 183–187. [DOI] [PubMed] [Google Scholar]
- 15. Gu Y. Rabie A.B. and Hagg U (2000) Treatment effects of simple fixed appliance and reverse headgear in correction of anterior crossbites. American Journal of Orthodontics and Dentofacial Orthopedics, 117, 691–699. [PubMed] [Google Scholar]
- 16. Wiedel A.P. and Bondemark L (2015) Stability of anterior crossbite correction: A randomized controlled trial with a 2-year follow-up. The Angle Orthodontist, 85, 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McLaughlin R.P. Bennett J. and Trevisi H (2001) Systemized Orthodontic Treatment Mechanics. Mosby International Ltd, London. [Google Scholar]
- 18. Petrén S. Bjerklin K. Marké L.Å. and Bondemark L (2013) Early correction of posterior crossbite—a cost-minimization analysis. European Journal of Orthodontics, 35, 14–21. [DOI] [PubMed] [Google Scholar]
- 19. Hägg U., Tse A., Bendeus M., Rabie A.B. (2004) A follow-up study of early treatment of pseudo Class III malocclusion. The Angle Orthdontics, 74, 465–472. [DOI] [PubMed] [Google Scholar]
- 20. Edman Tynelius G. Lilja-Karlander E. and Petrén S (2014) A cost-minimization analysis of an RCT of three retention methods. European Journal of Orthodontics, 36, 436–441. [DOI] [PubMed] [Google Scholar]
- 21. Hichens L. Rowland H. Williams A. Hollinghurst S. Ewings P. Clark S. Ireland A. and Sandy J (2007) Cost-effectiveness and patient satisfaction: Hawley and vacuum-formed retainers. European Journal of Orthodontics, 29, 372–378. [DOI] [PubMed] [Google Scholar]