Abstract
Introduction
Radiation therapy (RT), like many allied health professions, has lacked professional practice clarity, which until 2008 had not been comprehensively investigated. This manuscript describes the first phase of a three‐phase project investigating the current and future practices of radiation therapists (RTs) in Australia. The aim of phase 1 was to define the practice of RTs in Australia.
Methods
A quantitative approach was used to gain an understanding of RT practice. A national survey was distributed to RTs in Australia. Descriptive statistics and content analysis were used to analyse the data. RT practice was analysed in relation to core and non‐core roles, where non‐core roles were further divided into basic and advanced practices.
Results
The data from the national survey were representative of the Australian RT population (n = 525). The current practice of RTs is presented in summary tables for each area of work (treatment, planning, simulation, mould room and general).
Conclusion
This study provided clarification of RT practice and indicated there was a desire to relinquish administrative roles to focus on RT–specific practice. There was evidence that some advanced roles were currently practiced in Australia; however, there was no structure to support these roles and they were based only on local need. This study identified that the profession needs to consider how they will maintain core RT practice, while encouraging the development of new roles, and whether some roles need to be relinquished.
Keywords: Mixed method, professional practice, radiation therapist, roles
Introduction
Radiation therapists (RTs) are health professionals who plan and deliver radiation used in the treatment of patients and therefore play an essential role in the treatment of cancer. In the early 2000 there was a critical shortage of radiation therapy (RT) services provided for the Australia population.1, 2 This shortage resulted in 14,233 people in 2008 missing out on RT treatment that could have improved their survival and quality of life.3 Addressing the shortage of RT services can be achieved in a variety of ways, such as by increasing the number of RTs, by decreasing attrition from the workforce or by using the skills of the existing workforce more effectively. These approaches have been highlighted by different authors. Baume1 supported diversifying career pathways for RTs, while Atyeo4 identified reasons for attrition from the profession. The shortage of RTs could be reconceptualised as a shortage of the expertise or skills that are provided by RTs. It may not be that there is a shortage of RTs, but rather increasing demands on existing RTs.
There has been little research into the scope of practice of RT. One key recommendation from the radiation oncology inquiry (ROI) was to make better use of the skills of available RTs by defining and clarifying the practice of RTs – ‘…outlining the role of RTs in the treatment of cancer…’ (p. 8).1 Hence, the lack of response to this key recommendation was a main driver of this study.
This study is part of a larger three‐phased research project. The first phase consisted of a national survey of RTs to determine the actual practice of RTs and the diversity of practice across states and departments. The second phase involved asking nominated experts in RT to consider envisaged changes in the scope of practice in the future (2015) using a Delphi technique. The third phase took the current practice and predicted future changes back to the profession in the form of focus groups to discuss the implications from the perspective of the RTs. This study focuses on the first phase.
Radiation therapy practice in Australia
The Australian RT profession has been changing its scope of practice and the roles of RTs have become increasingly complex due to rapidly advancing technology, broadening of specialty areas and increased demand for service and quality.5, 6
The role of RTs has been described in a number of ways by several researchers in Australia;
A radiation therapist is a technical person skilled in the planning and delivery from the radiation or machine of the prescribed dose to the volumes determined (p. 3).7
The role of the radiation therapist includes localisation, dosimetry calculation, associated treatment planning and treatment delivery as directed by the radiation oncologist (p. 32).2
These definitions lack detail and limit the portrayal of RT practice to technical skills without autonomy. The Australian Institute of Radiography (AIR) is the peak professional body for RTs and radiographers in Australia. The AIR Competency‐Based Standards (CBS)8 and the AIR Education Policy9 included a scope of practice for RTs. However, both documents used broad concepts and are open to individual interpretation with no detail of the importance or frequency of role delivery. No information was provided on how data were collected for the Education Policy9 or the CBS,8 and no sources were cited. Other literature including the AIR Submission to the National Inquiry into Radiation Oncology Services (Baume Inquiry),10 the 2004 AIR RT survey11, 12 and the ACT Health review,13 all indicated a lack of evidence in the area of RT practice and that there was no in‐depth research into RT practice in Australia.
As an understanding of the scope of practice of RTs in Australia is fundamental to provision of services, this article describes the results of a national survey of RTs to capture a detailed insight into what RTs do in the provision of services to patients. The aim of this study was to define the current practice of RTs in Australia in 2008.
Material and Methods
A mixed method research design was selected to identify, describe and understand RT practice in Australia across the three‐phased project.14 The research combined quantitative and qualitative methods to gain both a broad overview and an in‐depth understanding of current RT practice. In this first phase of the project, a quantitative approach was used. A combination of descriptive statistics and content analysis was employed to interrogate the data, to give a holistic and meaningful understanding of the current practice of the RT profession.
Ethical approval was obtained from the University of South Australia's Human Research and Ethics Committee (HREC) (P193/07).
Participants
The target group consisted of all qualified RTs currently working in a RT capacity in Australia.
Design of the national survey
The content of the online survey was informed by limited evidence,8, 9, 10, 15, 16 and the involvement of a reference group. The reference group consisted of eight members: two RTs, one RT manager, one radiation oncologist, one RT educator, one oncology nurse, one organisational psychologist and one allied health advisor. Only Australian literature was relevant for this study as the research focus was on Australian RT practice. There were no previous instruments that could be used or adapted for this study.
Attention was paid to the construction of questions, ensuring that they were relevant, objectivity was maintained, the wording was kept short and concise for ease of participant response and that a logical progression throughout the survey was maintained.17, 18 Members of the reference group were e‐mailed a copy of the draft survey to provide advice on structure and suggestions for roles to be incorporated to ensure content validity. All reference group members approved the survey prior to pilot testing with six RTs with varying years of experience in the RT profession and four non‐RTs (radiation oncologist, oncology nurse, organisational psychologist and allied health advisor).
In the survey, RT practice was divided into the areas of treatment, planning, mould room, simulator and general. Questions focused on frequency with which RTs performed certain roles with the response options represented on a 5‐point Likert scale every day to never. At the end of each section, participants were asked to provide details of additional activities they carried out. The final section consisted of demographic questions.
The overall appearance of the survey was important in regards to increasing participation; layout organisation, spacing, text font and making the survey visually appealing and user‐friendly all increase the number of participants.18 Although the length of a survey may affect participation, there was limited evidence to suggest that longer surveys result in lower participation.19, 20 The scope of practice for RTs was a broad topic and to investigate it thoroughly, all areas needed to be encompassed, thus making the survey quite lengthy. Pilot testing was completed by the reference group to ensure readability and functionality of the online survey.18
Survey distribution
The national survey was distributed by e‐mail or post to all RTs in Australia who could be contacted via the AIR, RT departments or the Queensland Health Practitioners Registration Board. The survey period extended from 7 January 2008 until the end of February 2008. E‐mail reminders were sent approximately 4 weeks after initial distribution to maximise response rate.19
Data analysis
All survey responses were entered into SurveyMonkey© (Finley 2009). Free text responses were collated and analysed using content analysis to identify RT practice roles. Descriptive statistics were used to analyse the quantitative data, as well as analysis of variance (ANOVA) and chi‐square tests (using Microsoft Excel 2007 and Predictive Analytics SoftWare [PASW] Version 17.0.3; College Station, TX, USA).
Results
Response rate
A total of 2141 national surveys were distributed to RTs in Australia. Five hundred and sixty‐four RTs responded to the survey with 555 valid responses. A valid survey response was defined as a participant providing a complete set of answers to a section of the survey. If more than three questions were missed the response for that section was not valid. There were approximately 1350 RTs in Australia (Badawy, pers. comm., 2008), therefore the approximate response rate was 41.1% (n = 555 valid responses). There was clearly some doubling up of survey distribution, with 2141 surveys distributed and only 1350 RTs however, this increased the chance of capturing more responses.
Participant profile
Of the 555 participants, 94.6% (525) practiced RT in the 12 months prior to the survey. Non‐practicing RTs (5.4%) were excluded from further analysis because this research was interested in the practice of currently employed RTs. Of the 525 practicing participants, 383 were female and 142 were male. The age distribution of participants is presented in Figure 1. Participants’ experience in RT ranged from 1 to 40 years with most having 1–5 years (41.6%). More than 50% of participants had 1–10 years (58.4%) of experience. Various combinations of RT positions were held by participants (basic level RT, senior level RT, management level RT, postgraduate studying RT, education and other). The greatest number of participants held basic level positions (45.1%); however, there were some basic level RTs who held acting senior positions, as well as studying and educational positions. Basic level RTs included the professional development year (PDY) or intern year. Victoria (32.6%), followed by New South Wales (30.3%), had the largest number of responses. One hundred and forty (27.5%) participants practiced in private RT departments with 370 (72.5%) in public RT departments. Ninety (17.6%) RTs practiced in regional departments, while 421 (82.4%) practiced in the metropolitan area.
Figure 1.
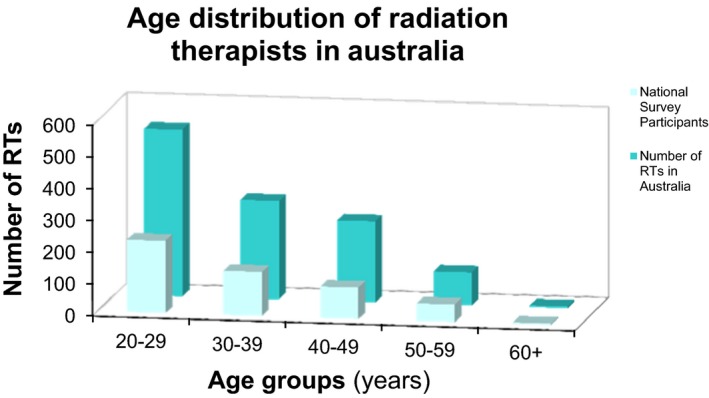
Age distribution in the national survey matched with Australian Institute of Radiography (AIR 2008) data.
Representative nature of the data
The respondent characteristics were compared with the 2006 survey21 to determine whether a valid representation of the RT profession was achieved. Figure 1 is an age distribution graph illustrating the similar trends in the current national survey and the 2006 RT Workforce Survey data. One‐way ANOVA calculations indicated there was no significant difference (P > 0.05) between the demographic data. It was therefore concluded that the data were representative of the RT population in Australia at the time of data collection.
Diversity of radiation therapy practice in Australia
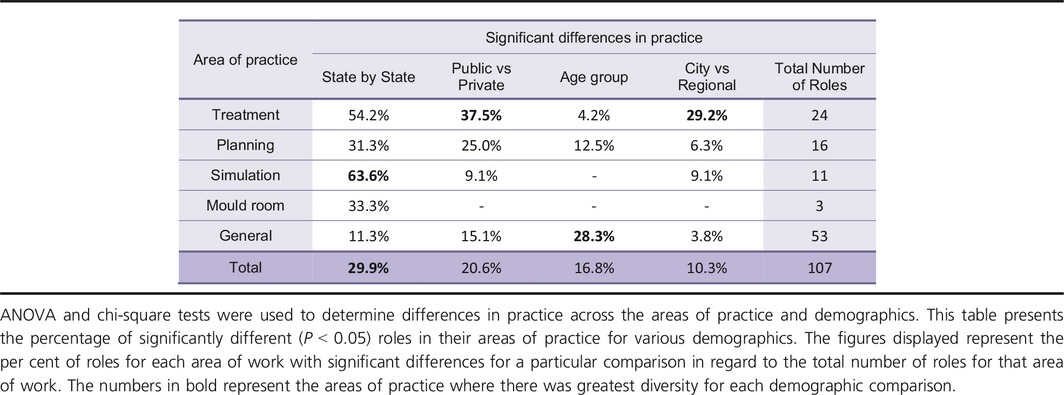
The practice of RTs was compared between states, public and private departments, across age groups, city and rural or regional departments (Table 1). There was greatest variation across the states (29.9%), followed by public versus private departments (20.6%) and age groups (16.8%), and there was least diversity between city and regional (10.3%) practice. Table 1 shows the differences for each type of practice. No particular category or area of RT practice was shown to have the most variation; there was variable across all areas of practice and in all demographics compared.
Table 1.
A representation of the diversity between demographic factors as well as areas of practice
Radiation therapy practice and frequency
Treatment practice
Almost 86% (n = 445) of RTs reported practicing in treatment in the 12 months prior to the survey. Table 2 classifies treatment practice into core and non‐core roles. Core tasks were defined as tasks that could only be performed by a RT or that could not proceed without a RT (AIR 2001). Therefore, core roles in this study were defined as needing RT–specific expertise and were autonomous, where no supervision was needed. For example, a core RT role is delivering a prescribed dose of radiation over a course of treatment. Non‐core tasks could be carried out by RTs, but may also be designated to other staff members in the RT department (AIR 2001). Therefore, non‐core roles in this study included any practice outside RT–specific roles (e.g. cleaning, organising appointments). Core roles were divided into generic, radiation administration methods, quality assurance (QA), technical and education, communication and patient care; and non‐core roles were divided into basic – administration roles and advanced roles. Working as part of a team was the most prevalent part of a treatment RT's practice (96.3%). The second most frequent treatment practice was delivering a prescribed dose of radiation over a course of treatment (91.4%). Administering stereotactic RT was the treatment role carried out least frequently (0.7%).
Table 2.
Treatment practice summary
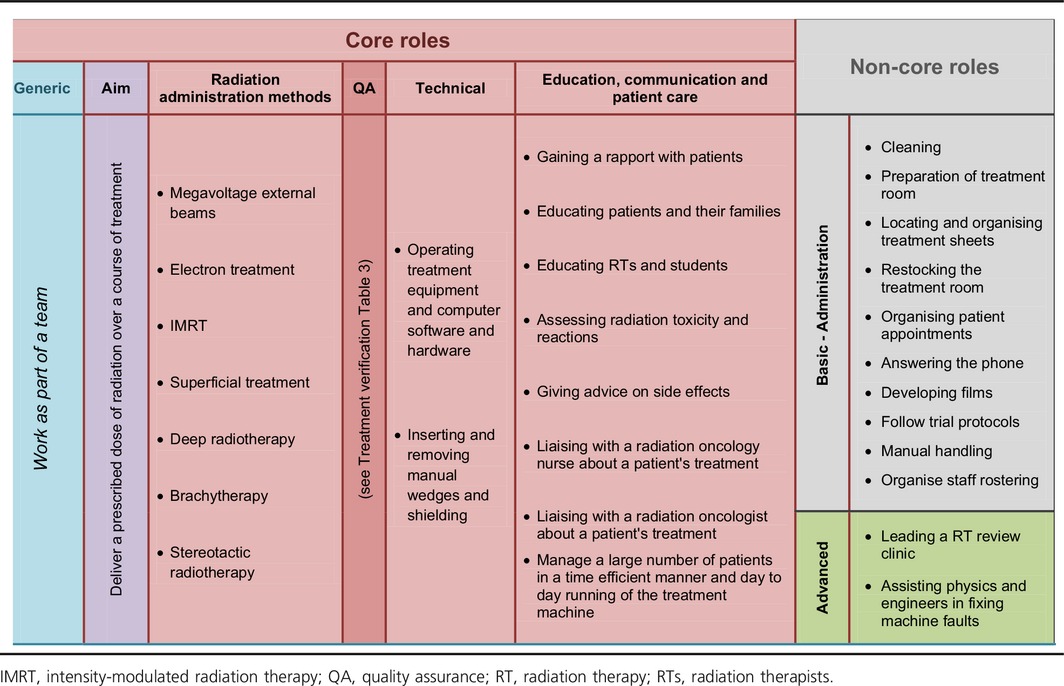
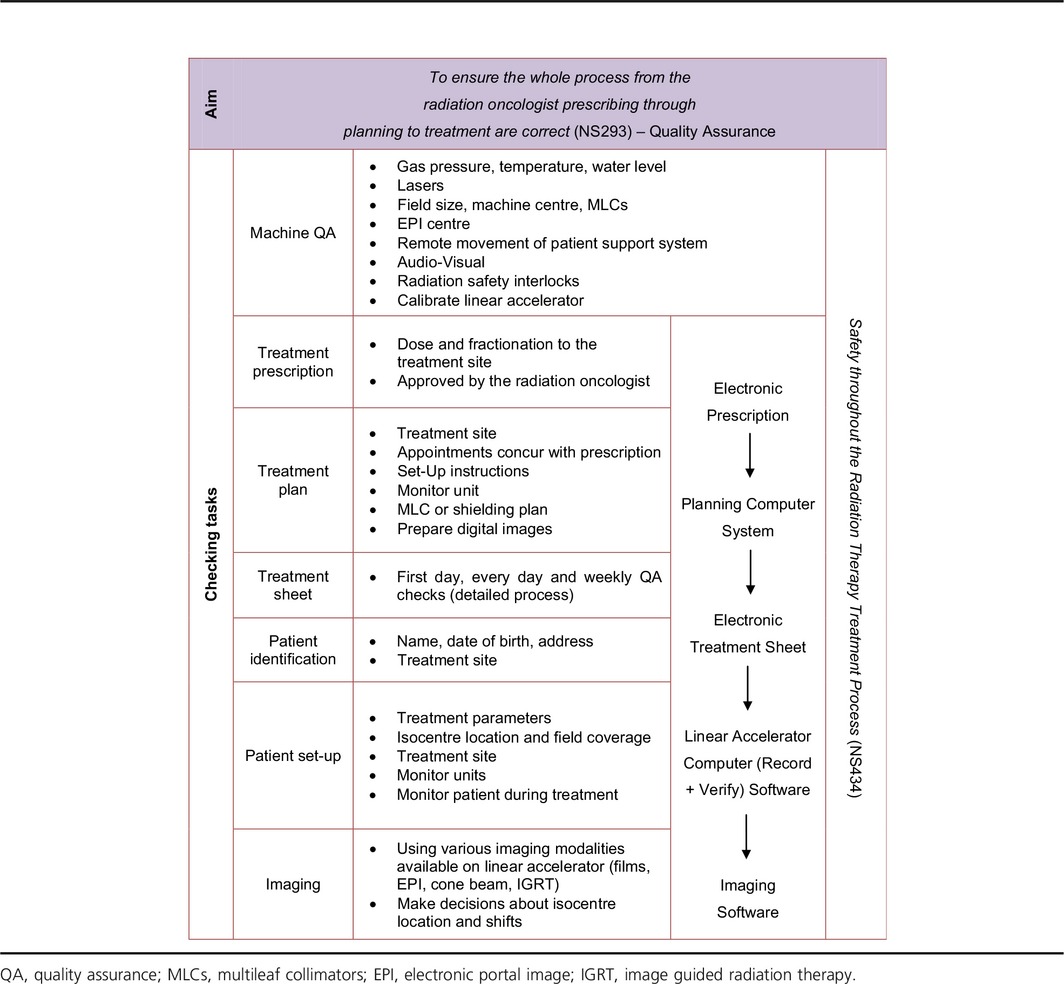
One of the core features when treating patients is the QA process that takes place at every step of the treatment process and is referred to as treatment verification (see Table 3). Patient care plays a large role in providing treatment over a number of weeks. RTs gain a rapport with patients, which can put the RTs in a position of patient advocate with the radiation oncologists or nurses regarding patient treatments. RTs also assess radiation reactions and provide advice to patients on prevention and management of acute side effects. Treatment administration, QA and patient care are referred to as core roles because they require RT‐specific expertise.
Table 3.
Treatment verification
Two participants reported they fulfilled an advanced practice role; one RT was responsible for an RT led review clinic (cancer type not specified) and one RT fulfilled a physics/engineering role (refer to Table 2).
RTs also carry out a range of administration roles, including cleaning, organising patient appointment, preparing the room, restocking the treatment room with supplies, organising treatment sheets and answering the phone (Table 2). The administration roles were categorised as non‐core basic roles as they did not require RT expertise and were viewed as relatively simple. In the free text responses, RTs reported not wanting to carry out these more basic administration tasks.
Planning practice
Seventy‐seven per cent of RTs (n = 402) reported working in planning. ‘Using computer dosimetry software’ was the most frequent planning practice (89.3% reported they used it every day). Planning stereotactic treatment was the least prevalent planning practice (95.8% never carried out this role). Respondents identified that the aim of RT planning is to produce achievable treatment plans for every patient with an optimal dose distribution that maximises the radiation dose to the tumour volume, while minimising the dose to the surrounding healthy tissue. Table 4 categorises planning practice into core and non‐core roles, under the headings: ‘Dosimetry for…’, ‘Technical’ and ‘Administration’.
Table 4.
Planning practice summary
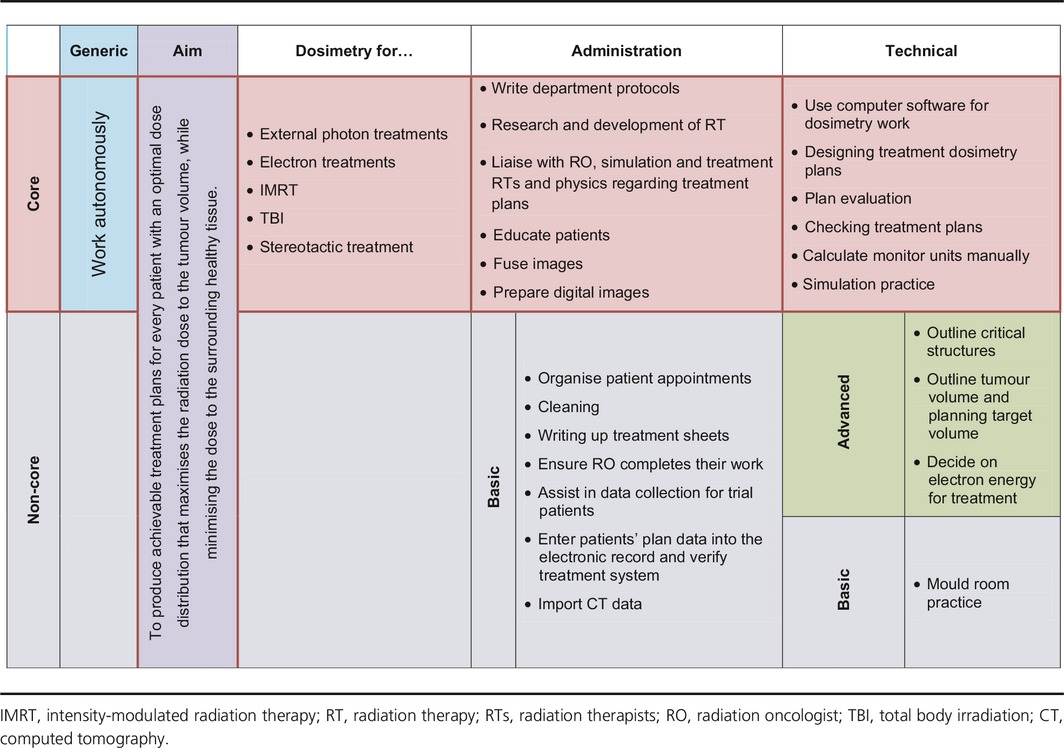
Advanced technical roles were contouring critical structures, the tumour and the planning target volume, making decisions about the electron energy to use for treatment and fusing images. Basic technical roles were writing up treatment sheets and mould room tasks. Basic administration practice included organising patient appointments, cleaning, ensuring the radiation oncologist completes their work, assisting in data collection for trial patients, entering patient data in the treatment system, importing computed tomography data and preparing digital images. In the free text responses, RTs expressed a desire to relinquish some of the basic administration practice, such as cleaning and organising appointments.
Simulation practice
Almost 66% (n = 343) of RTs reported working in simulation. The different roles in simulation are presented in Table 5, divided into core and non‐core roles (advanced and basic) and categorised under procedures: technical; education, communication and patient care and administration. The aim of simulation is to define the treatment region, and determine and record patient data to enable accurate planning and a reproducible treatment position for a patient, with reference to the radiation oncologist's referral. ‘Taking a record of a patient's position and the immobilisation equipment used’ was the most prevalent form of simulation practice, with a mode of 81.3% for every day. Maintaining the film processor was the simulation practice carried out least frequently, with a mode of 55.1% never carrying out this role.
Table 5.
Simulation practice summary
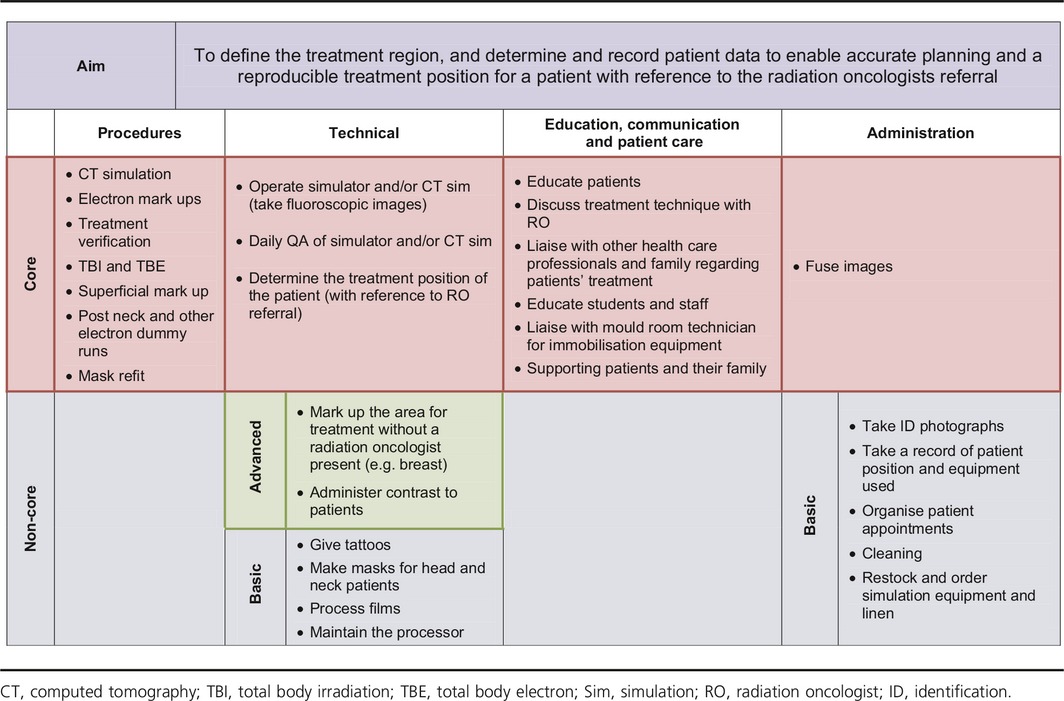
Educating patients was a key theme to emerge for simulation RTs, involving department tours, providing information about treatment, talking about side effects of radiation treatment and finally answering any questions patients have about their treatment.
Advanced technical roles in simulation identified were marking up an area for treatment and administering contrast during simulation. There were numerous administrative roles that RTs carry out which were categorised as basic. These roles were taking identification photographs, recording a patient's position and the equipment used for the treatment set up, organising appointments, cleaning, restocking and ordering equipment and linen. Again RTs expressed not wanting to carry out tasks such as cleaning, taking photographs or organising appointments.
Mould room practice
The smallest group of RTs (26.3% or n = 136) practiced in mould room. All mould room practice was classified as basic non‐core as it did not require RT‐specific expertise. ‘Producing immobilisation devices’ was the most frequently carried out practice in the mould room, with a mode of 33.8% for carrying out this task ‘occasionally’; however, ‘every day’ and ‘most days’ responses made up to 46.4% (19.8% and 26.6% consecutively). RTs expressed not wanting cleaning to be part of their practice. The mould room section only includes practice that is exclusively in a mould room and does not include planning or simulation practice that encompasses mould room tasks. For example, pouring shielding blocks or making electron shields.
Discussion
Professional practice is a complex issue and until this study RT practice remained unexplored at a national level in Australia. RT practice has been investigated in other countries including New Zealand, United Kingdom and Canada, and the issues explored within this research are not unique to Australian RTs.22, 23, 24, 25 This study was conducted to address key recommendations from the Radiation Oncology Inquiry considered to be ‘vital’ for RT services in Australia (p. 18).1 Ultimately, better utilisation of the skills of RTs should contribute to improved provision of treatment for cancer patients. This study consisted of a national survey of RTs to determine the actual practice of RTs and the diversity of practice across states and departments. The findings of this study depicted the complex nature of RT practice in Australia. The results highlighted the large number of roles assumed by RTs and the diversity across states, departments and age groups.
Summary of the key findings from the national survey were:
There was a disparity in RT practice across Australia.
A large portion of the RT profession were aged in their 20s.
Some advanced roles were currently practiced in Australia by some RTs; however, there was no evidence of structure to support these roles in the current system and they were based on local need.
RTs working in all areas (treatment, planning, simulation and mould room practice) expressed a desire to relinquish administrative roles to focus their time on RT‐specific practice.
There was evidence to show that relinquishment of roles was already occurring in some departments in Australia.
The disparity in RT practice across Australia was attributed to local practice and based around individual professional relationships; therefore, formalisation of practice with agreed standards and detailed documentation on the practice of RTs is required. Lack of standardisation limits the movement of RTs between departments in Australia and internationally and has been indicated as a barrier to developing practice26 where there is no clear baseline from which to develop. There is a need for unity in the structural development of RT practice, including education, remuneration and career structure.13 Formalisation of practice with agreed standards could provide clarity to the work of RTs. This study provides the first step in providing the structure and support required to develop the practice of Australian RTs.
The RT profession in Australia moved to national registration in 2012, where some standardisation of terminology across states has been required. National registration and accreditation may provide the catalyst for promoting formalisation of practice to provide clarity around what RTs do and do not do – there is some evidence of this with documents such as Accreditation Standards: Medical Radiation Practice.27 Clarity will assist in strengthening the professional status of RTs, as it will enable RTs to have greater certainty in practice, as well as an opportunity to measure patient outcomes more consistently, may provide better patient care, allows transferability of RTs from one place to another, it could lead to improved quality and safety if the role of the RTs is more clearly understood.
Currently, RTs in advanced positions are not formally acknowledged and work at the same level as senior therapists, where no further qualifications are required. There is a need to align the education model more closely with the current and future practice of RTs and to develop advanced practitioner courses to provide RTs with the support they need to confidently undertake advanced positions.
The demands on RT services necessitate that basic non‐core roles be relinquished to other personnel, and that career pathways and advancement opportunities be provided to RTs to make better use of their skills. This change would improve job satisfaction and assist in retaining RTs in the profession in light of increasing future demands. The Advanced Practice Advisory Panel has been looking at ways to develop advanced practice opportunities for RTs in Australia and a new group at the AIR will be assembled in the near future to investigate the idea and place of assistant practitioners in the Australian medical radiation profession (Harris, pers. comm., 2015).
Limitations of the study
The length of the survey was considered long. Every effort was used to minimise the number of questions, but the scope of practice for RTs was a broad topic and to investigate it thoroughly, all areas needed to be encompassed. The length of the survey may have impacted on the quality or quantity of responses. As the data for this study were collected in 2008 and much advancement in RT practice have been made over the past decade, this limits the applicability of the study in the current practicing climate. However, this study continues to provide an understanding of the scope of RT practice and areas that need to be improved for the profession.
Conclusion
This study provides an overview of the current scope of practice for RTs in Australia. The results highlighted the large number of roles assumed by RTs. There was support for the notion of non‐core (basic) roles, specifically administrative activities being relinquished to other personnel to focus RTs time on RT‐specific practice. There was evidence to show that some roles were already performed by other allied health professionals or administrators in some departments in Australia, but it was not the norm. Some RTs currently have advanced practice roles in Australia; however, there was no structure to support these roles and they were only based on local need.
A career structure needs to be developed to ensure that the RT profession can provide optimum treatment for the Australian population. For current practice, a career structure could provide improved equity between states and levels of career progression, enabling RTs to move between departments more freely. With an aligned educational model and pay levels this will provide even more equity between states. A carefully considered national career structure will help improve the strength of the profession.
This article concludes with two recommendations:
There is a need to formalise RT practice in Australia with agreed standards;
The findings from this study need to be used to improve the documentation around the practice of RTs in Australia in conjunction with the AIR.
For current practice, there is a need for RTs to increase their influential power to make changes within the profession. The power to change the profession of RT lies with the professional body, the AIR, with the support of local champions within the profession and educational institutions. Cooperation from the Federal and State Departments of Health, Australian Health Practitioner Regulation Agency (AHPRA) and The Royal Australian and New Zealand College of Radiologists (RANZCR) will be needed. Formalisation of current practice of RTs will reduce the amount of diversity across Australia. The diversity in RT practice between states and even public and private departments has limited the descriptive quality of documentation around RT practice. It has resulted in vague statements that provide little insight into what RTs do. The findings of this study can assist in improving the accuracy of this documentation. The national survey determined the practice of RTs in 2008 and informed phases 2 and 3 providing a baseline for projecting future practice for the profession.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The authors thank all of the RTs who participated in this study. The authors also thank Sheila Scutter for her support and guidance throughout this research. This research was carried out at the University of South Australia, GPO Box 2471, Adelaide South Australia 5001.
J Med Radiat Sci 63 (2016) 104–113
References
- 1. Baume P. The Radiation Oncology Inquiry (P. Baume, Commissioner), Commonwealth of Australia, Canberra, Australia, 2002. [Google Scholar]
- 2. The Royal Australian and New Zealand College of Radiologists (RANZCR) . National Strategic Plan for Radiation Oncology, The Tripartite Committee; [2001; cited 2009 Jan 12]. Available from: http://www.ranzcr.edu.au/documents/detail.cfm?ophileEntry=823&ophileLibrary=29&ophileReturnpage=list.cfm&llLetter=All. [Google Scholar]
- 3. Morgan G, Barton M, Atkinson C, Millar J, Gogna NK, Yeoh E. The ‘GAP’ in radiotherapy services in Australia and New Zealand in 2009. J Med Imaging Radiat Oncol 2010; 54: 287–97. [DOI] [PubMed] [Google Scholar]
- 4. Atyeo J. Factors Influencing the Workforce Attrition of Australian Radiation Therapists. PhD thesis, The University of Sydney, 2008. [Google Scholar]
- 5. Professional Advancement Working Party (PAWP) . Professional Advancement Working Party Report – April 2006. Australian Institute of Radiography, Melbourne, Australia, 2006. [Google Scholar]
- 6. Advanced Practice Working Group (APWG) . Discussion Paper: A Model of Advanced Practice in Diagnostic Imaging and Radiation Therapy in Australia. Australian Institute of Radiography, Melbourne, 2009. [Google Scholar]
- 7. The Royal Australian and New Zealand College of Radiologists (RANZCR) . Clinician's Guide to Radiation Oncology – How Radiotherapy is Given [2004; cited 2009 Aug 26]. Available from: http://www.ranzcr.edu.au/documents/detail.cfm?ophileEntry=466&ophileLibrary=29&ophileReturnpage=list.cfm&llLetter=All.
- 8. Australian Institute of Radiography (AIR) . Competency Based Standards for the Accredited Practitioner – August 2005. AIR, Melbourne, Australia, 2005. [Google Scholar]
- 9. Australian Institute of Radiography (AIR) . Educational Policies, revised January 2004. AIR, Melbourne, Australia, 2004. [Google Scholar]
- 10. Australian Institute of Radiography (AIR) . Submission to the National Inquiry into Radiation Oncology Services: Radiation Therapy Profession. AIR, Melbourne, Australia, 2001. [Google Scholar]
- 11. Australian Institute of Radiography (AIR) . AIR survey profiles the duties and responsibilities of radiographers and radiation therapists: Part II. Spectrum 2005; 12: 10–3. [Google Scholar]
- 12. Australian Institute of Radiography (AIR) . AIR survey profiles the duties and responsibilities of radiographers and radiation therapists: Part II. Spectrum 2005; 12: 9–11. [Google Scholar]
- 13. Australian Capital Territory (ACT) Health . A Systematic Review of the Literature – Extend Scope of Practice Radiation Therapy, Final Report. ACT Government, Canberra, Australia, 2009. [Google Scholar]
- 14. LoBiondo‐Wood G, Haber J. Nursing Research: Methods, Critical Appraisal, and Utilization, 2nd edn The C.V. Mosby Company, Missouri, USA, 1990. [DOI] [PubMed] [Google Scholar]
- 15. Australian Institute of Radiography (AIR) . Guidelines for Professional Conduct for Radiographers, Radiation Therapists and Sonographers – April 2003. AIR, Melbourne, Australia, 2003. [Google Scholar]
- 16. Lombardo P. Concerns for medical radiation programs in Australian universities. Radiography 2006; 12: 332–8. [Google Scholar]
- 17. Brace I. Questionnaire Design: How to Plan, Structure and Write Survey Material for Effective Market Research, Market Research in Practice Series, London, UK, 2004. [Google Scholar]
- 18. Iarossi G. The Power of Survey Design: A User's Guide for Managing Surveys, Interpreting Results, and Influencing Respondents. World Bank Publications, Washington DC, USA, 2006. [Google Scholar]
- 19. Nakash RA, Hutton JL, Jørstad‐Stein EC, Gates S, Lamb SE. Maximising response to postal questionnaires – a systematic review of randomised trials in health research. BMC Med Res Methodol 2006; 6: 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Edwards P, Roberts I, Clarke M, et al. Increasing response rates to postal questionnaires: systematic review. BMJ 2002; 324: 1183–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Australian Institute of Radiography (AIR) . Radiation therapy workforce survey. Spectrum 2006; 2008(15): 17–9. [Google Scholar]
- 22. Coleman K, Jasperse M, Herst P, Yielder J. Establishing radiation therapy advanced practice in New Zealand. J Med Radiat Sci 2014; 61: 38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Eddy A. Advanced practice for therapy radiographers – a discussion paper. Radiography 2008; 14: 24–31. [Google Scholar]
- 24. Harnett N, Bak K, Zychla L, Lockhart E. A Roadmap for change: charting the course of the development of a new, advanced role for radiation therapists. J Allied Health 2014; 43: 110–6. [PubMed] [Google Scholar]
- 25. Bolderston A, Smoke M, Lewis D, Harnett N. Ten years of advanced practice in Ontario: reflections and recollections. J Med Radiat Sci 2013; 44: 163–5. [DOI] [PubMed] [Google Scholar]
- 26. Martino S, Odle T. Advanced Practice in Radiation Therapy. American Society of Radiologic Technologists, Albuquerque, 2007. [Google Scholar]
- 27. Australian Health Practitioners Regulatory Agency (AHPRA) . Accreditation Standards: Medical Radiation Practice. Medical Radiation Practice Board of Australia, Melbourne, Australia, 2013. [Google Scholar]


