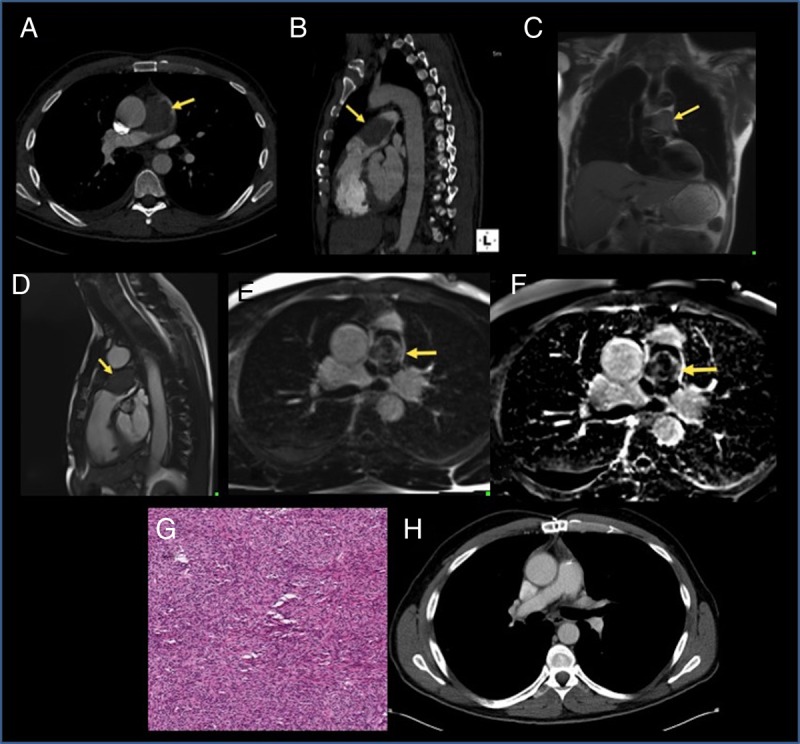
A 49-year-old healthy man presented with 2 months history of progressive shortness of breath and hemoptysis. Physical examination was remarkable for new systolic heart murmur. Chest X-ray revealed a small opacity in the right lower lobe, and non-contrast computed tomography (CT) demonstrated two sub-pleural masses at the right lung base. Computed tomography-guided biopsy showed benign tissue with extensive necrosis and inflammation. To evaluate the heart murmur, echocardiogram was done and showed moderate pulmonary hypertension with flow acceleration in the main pulmonary artery (PA). Contrast CT revealed a large filling defect in the main PA (5.2 × 3.0 cm) concerning for PE and/or tumour (Panels A and B). Cardiac magnetic resonance was obtained and T2-weighted dark blood sequence demonstrated a slightly hyperintense mass confined to the main PA (Panel C). Steady-state free precession (SSFP) cine showed a mass just distal to the pulmonic valve causing significant restriction to blood flow (Panel D, Supplementary material online, Video 1). Post-gadolinium inversion recovery delayed enhancement sequence showed heterogeneous hyperenhancement consistent with malignant tumour, with a small periphery of non-enhancement representing overlying thrombus (Panels E and F). These features were most consistent with primary PA sarcoma. Consequently, a resection of the mass, with en bloc removal and replacement with conduits of the main and proximal PA branch was performed. Pathology showed high-grade sarcoma with extensive rhabdomyoblastic differentiation, representing rhabdomyosarcoma (Panel G). Whole-body positron emission tomography (PET/CT) showed no evidence of residual tumour or distant metastases. The patient received adjuvant chemotherapy, and 16-month surveillance CT has no evidence of disease recurrence (Panel H).
Panels A and B. Contrast-enhanced computed tomography (CT) angiogram axial and sagittal images showing a sharply defined defect (arrow) in the main PA surrounded by a minimal amount of contrast flowing to the origin of the right PA. The PA is mildly distended at the site of obstruction. Panel C. Cardiac magnetic resonance (CMR) T2-weighted dark blood coronal image showing a slightly hyperintense mass in the main pulmonary artery without extension into the branch arteries. Panel D and Supplementary material online, Video 1. Steady state free precession (SSFP) cine imaging of the right ventricular outflow tract shows a normal right ventricle with a mass just distal to the pulmonic valve causing significant restriction to blood flow. Panels E and F. Post-gadolinium inversion recovery magnitude and phase-sensitive images showing heterogenous hyperenhancement of the mass consistent with malignant tumor, with a small periphery of non-enhancement (most evident on phase-sensitive image) representing overlying thrombus. Panel G. Photomicrograph, haematoxylin-eosin stain, of the mass obtained at surgery shows a high-grade sarcoma with extensive rhabdomyoblastic differentiation, most consistent with a rhabdomyosarcoma. Panel H. Surveillance contrast-enhanced CT angiogram obtained 16 months after surgery showing no evidence of any recurrence.
Supplementary material is available at European Heart Journal online.


