Summary
Objectives:
Insufficient attention is given in the literature to the early treatment of anterior open bite (AOB) subjects receiving orofacial myofunctional therapy (OMT), which aims to harmonize the orofacial functions. This prospective pilot study investigates the effects of OMT on tongue behaviour in children with AOB and a visceral swallowing pattern.
Materials and methods:
The study comprised of 22 children (11 boys, 11 girls; age range: 7.1–10.6 years). They were randomly assigned into OMT and non-OMT subjects. The randomization was stratified on the presence of a transversal crossbite. At baseline (T0), at the end of treatment (T1) and at 6 months after T1 (T2) maximum tongue elevation strength was measured with the IOPI system (IOPI MEDICAL LLC, Redmond, Washington, USA). Functional characteristics such as tongue posture at rest, swallowing pattern and articulation and the presence of an AOB were observed.
Results:
OMT did significantly change tongue elevation strength, tongue posture at rest, and tongue position during swallowing of solid food. At T2 more OMT subjects had contact between the lower central incisors and their antagonists or palate (P = 0.036). More OMT subjects performed a physiological pattern of water swallowing than non-OMT children at T1 and T2, although the differences were not significant. Articulation of /s,l,n,d,t/ was not improved by OMT. No interaction between OMT and expansion was found for any of the parameters.
Conclusion:
OMT can positively influence tongue behaviour. However, further research is recommended to clarify the success of OMT as an adjunct to orthodontic treatment and to identify possible factors influencing the outcome.
Introduction
Malocclusions such as anterior open bite (AOB) are often associated with orofacial dysfunctions (1). It has a multifactorial etiology comprising inherited skeletal pattern and environmental causes, such as thumb or dummy sucking, mouth breathing, lip or tongue thrusting and posture, tooth ankylosis, and eruption disturbances. Some researchers have focused on the tongue as the primary factor in the etiology of AOB. Proffit (2) and Proffit et al. (3, 4) measured force levels of the tongue against the maxillary incisors and palate during rest and normal swallowing. They concluded that the resting position of the tongue was a more contributing factor than the swallowing position in determining dental arch form. The inadequate tongue position during swallowing must then be regarded as a result of a pre-existing morphological alteration, thus as a consequence and not as a cause of the AOB. Other investigators however have shown that functional tongue movements during deglutition are significantly correlated with certain features of maxillofacial morphology such as AOB (5–7). Individuals with partial AOB and incorrect tongue position exhibit impaired gnostic sensibility of the tongue (8, 9), which is a symptom of disturbed sensorimotor coordination and is connected with the incorrect position of the tongue. This results in imprecise action and reduced vertical movement of the tongue. Cayley et al. (10) reported that children who swallow incorrectly very rarely touch the anterior part of the palate with the tip of the tongue. They perform predominantly horizontal tongue movements and place the tongue between their anterior teeth while speaking and swallowing (11). Although studies have demonstrated that tongue thrust plays an important role in the etiology of AOB as well as in the relapse of treated AOB patients, the exact etiological connection between malocclusion and malfunction during swallowing remains controversial (12). This applies in particular to the extent to which orofacial dysfunctions foster the development of malocclusions and how a dysfunction can be positively influenced by a change in structure (13).
From the standpoint of developmental physiology, a distinction is drawn between visceral, somatic, and inconstant swallowing (12, 14). Visceral swallowing exists at birth and is also termed ‘infantile swallowing’. It is characterized by a forward movement of the tongue tip and pressure against the lingual surfaces of the anterior teeth. A visceral type of swallowing can persist well after the fourth year of life and is then considered as a dysfunction or abnormality because of its association with certain malocclusions (12, 14). Normally, the visceral swallowing pattern changes gradually into a mature or somatic swallowing pattern. The latter is characterized by a cranial movement of the tongue and pressure on the incisive papilla (12). Inconstant swallowing is characterized as a pattern of swallowing during the transitional period between infantile and somatic swallowing. According to Christensen and Hanson, a visceral swallowing pattern is seen in 50% of 5-year olds and in 33% of 8-year olds (15).
In the age range between 6 and 8 years, AOB is a predominant type of malocclusion (16). A prevalence of 1–17.7% of AOB (defined as the lack of overlap between the upper and lower incisors) in the mixed dentition is reported in the literature (1, 16–19). In the mixed dentition AOB is registered more often in girls (1, 19). Keski-Nisula et al. (17) reported in their study that at the onset of the early mixed dentition, 39.1% of the children had no contact either between the mandibular incisors and maxillary incisors or palatal gingiva. In 4.6% no incisal overlap was present. Some authors mention that the prevalence of AOB is not significantly variable with age (20), however, other state that the frequency of AOB undergoes a significant decline from the deciduous to the mixed dentition (1, 18, 21–22). Almost 70% of the AOB cases is self-corrective during the transition from the primary to the early mixed dentition (18). The main factor underlying the self-corrective tendency is the early interception of infantile habits (18, 23). According to Klocke et al. (21) the frequency of AOB also declines from the early to late mixed dentition. AOB associated with orofacial dysfunctions however declines only gradually with increasing age and therefore children whose open bite is associated with substantial dysfunctions are to be regarded as high-risk children for the further development of the dentition (1).
Several treatment approaches with regard to early treatment of AOB can be found in the literature. Many authors agree that clinicians should be able to distinguish an AOB of dental and dentoalveolar origin from a skeletal open bite so that treatment is directed towards the cause of the problem. Unfortunately, in most cases this distinction is not so clear and both dental and skeletal characteristics are present. The treatment modalities for early correction of AOB include functional, fixed, and removable appliances, with the goals of impeding mechanical factors that maintain the open bite (like thumb sucking or tongue thrust) and limiting excessive vertical growth of the craniofacial skeleton (24–31). However, few publications exist on early interceptive treatment in AOB patients with a persistent aberrant swallowing pattern using orofacial myofunctional therapy (OMT) (32–35). Some authors question the clinical use of OMT (22). Others support the reestablishment of a normal oral function after OMT in patients with myofunctional disorders such as tongue thrusting (36, 37).
The aim of a myofunctional program is to establish a new neuromuscular pattern and to correct abnormal functional and resting postures. Cayley et al. (38) demonstrated that normal swallowing function resumes after OMT in subjects with AOB. Also the improvement of the resting position of the tongue has been described (35). It has been suggested that an OMT therapist should train the patient to lift the body of the tongue in order to learn a normal resting position of the tongue. Other treatment objectives are strengthening of the orofacial muscles to pave the way for mouth closure, establish nasal breathing, and learn a physiological swallowing pattern (39). However, Smithpeter and Covell (40) cited the following reasons for the lack of enthusiasm for OMT: 1. limited office space for providing therapy, 2. absence of OMT providers, 3. difficulty and amount of time required, 4. inadequate training, 5. hope that a change in function will be induced by a change in form, 6. belief that there is insufficient scientific evidence to support OMT and 7. observation that not all OMT providers have the same expertise, so successful results are unpredictable.
The aim of the present pilot study is to investigate the effects of OMT on tongue behaviour in children with AOB and a visceral swallowing pattern.
Subjects and methods
Twenty-two children (11 males, 11 females; age range: 7.1–10.6 years) were included in this prospective pilot randomized study. The inclusion period started in February 2012 and ended in February 2013. The inclusion and exclusion criteria are described in Table 1. All children were seen at the orthodontic department of the University Hospitals Leuven and informed consent was obtained. The research project was approved by the Ethics Committee of the University Hospitals Leuven (B322201316750).
Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria |
|---|
| Lack of contact between the lower central incisors and the upper central incisors or palate |
| Early or intermediate mixed dentition |
| Visceral swallowing pattern |
| Exclusion criteria |
| Age less than 6 or more than 10 years old |
| Sucking habits not ceased for at least 6 months prior to intake |
| History of myofunctional therapy |
| Mental retardation |
| Orofacial congenital deformities or orofacial syndromes |
| Muscular or connective tissue disorders |
| Macroglossia or ankyloglossia |
| Obstructed nasal airway |
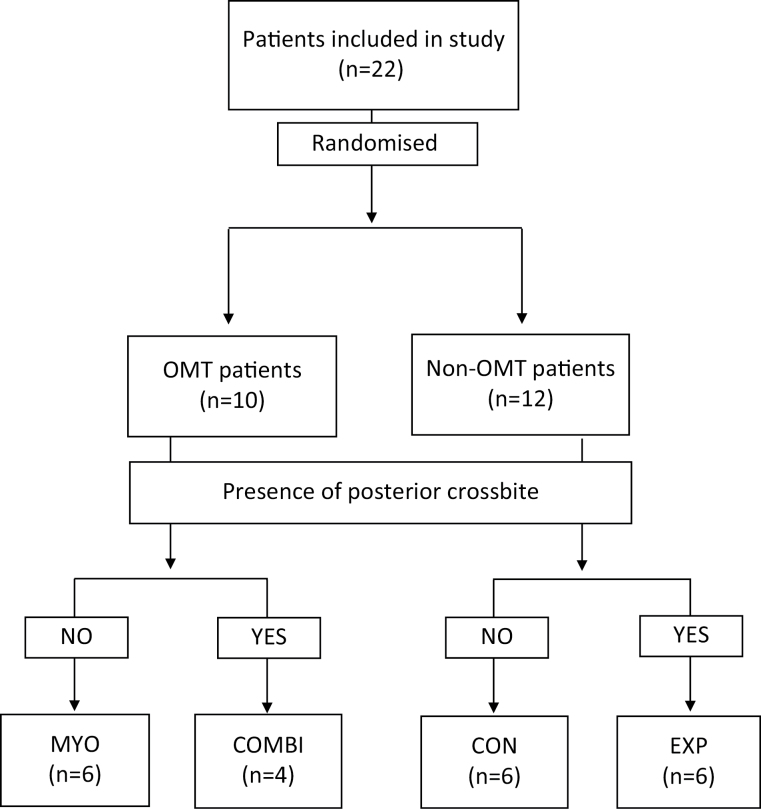
The subjects were randomly assigned into two groups: OMT-patients and non-OMT-patients (Figure 1). The randomisation was stratified on the presence of a transversal crossbite (uni- or bilateral); so each randomized group consisted of two subgroups, patients with and without expansion, respectively. If no crossbite was present, the subjects were randomly assigned in the MYO subgroup (n = 6, mean age 8.3, age range 7.1; 9.3) or CON subgroup (n = 6, mean age 9.1, age range 7.7; 10.6). The MYO subgroup underwent 10 hours of OMT, during 10–20 sessions of 30–60 minutes. The children were furthermore instructed to perform exercises at home. The CON subgroup was observed after 6 months without treatment. However, if a crossbite was present, the subjects were randomly assigned in the EXP subgroup (n = 6, mean age 8.7, age range 7.5; 9.8) or COMBI subgroup (n = 4, mean age 8.4, age range 8.1; 8.7). The EXP subgroup was treated with a removable expansion device and the COMBI subgroup first underwent 10 hours of OMT, followed by a treatment with a removable expansion device.
Figure 1.
Flow chart of patient allocation.
An overview of the different stages of the myofunctional training program is listed in Table 2. The OMT phase of intervention lasted 4–6 months. The sessions were given weekly (30 minutes) or every 2 weeks (60 minutes) and were individually held with each patient. The removable expansion device consisted of an acrylic resin plate with coverage of the occlusal surfaces of the posterior teeth and a jack-screw which was activated 1–2 times a week by the patient. At baseline (T0), at the end of treatment or after 6 months in the CON subgroup (T1) and after 6 months of follow-up (T2) maximum tongue elevation strength was measured. Functional characteristics as tongue posture at rest, swallowing pattern and articulation, were examined by means of a clinical evaluation performed by a speech pathologist.
Table 2.
Overview of the different sessions during the myofunctional training program.
| 1 | Explanation of treatment process and motivation |
|---|---|
| 2–3 | Strengthen tongue and lip musculature |
| 4–5 | Basis of the swallowing process |
| 6 | Strengthen the anterior part of the tongue |
| 7–9 | Strengthen the mid part of the tongue |
| 10–11 | Strengthen the posterior part of the tongue |
| 13–14 | Coordination of the total swallow movement |
| 15–16 | Practice on conscious habit formation |
| 17–18 | Practice on unconscious habit formation |
| 19 | Control of physiological swallowing act |
| 20 | Control of physiological swallowing act and follow-up |
The maximum tongue elevation pressure was measured using the IOPI system (IOPI MEDICAL LLC, Redmond, Washington, USA). The IOPI measures the amount of pressure exerted on a small air-filled bulb. Pressures obtained are digitally displayed (expressed in kiloPascal) on the LCD panel on the instrument. To measure maximal tongue elevation strength, the same procedure as described by Vanderwegen et al. was applied (41).
The tongue posture at rest was clinically visualized and evaluated by asking the child where their tongue was located and the answer was converted in one of the categories represented in Table 3, similar to the protocol used by Stahl et al. (42). To determine the swallowing pattern the child was asked to swallow water and solid food three times (in the form of a cookie). Swallowing patterns were assigned in one of the categories represented in Table 3. During swallowing the lips were gently separated to visualize tongue position. Tongue position during the production of the sounds /l,n,d,t,s/ was recorded as the child spoke Dutch test sentences and words. Articulation findings during speech were categorized as described in Table 3.
Table 3.
Overview of the categories scored during clinical examination.
| Tongue posture at rest | |
|---|---|
| 1. Physiological | Resting position of the tongue in contact with the palate extending to the palatal aspect of the alveolar ridge |
| 2. Inter- or addental | Resting position of the tongue between the anterior and/or posterior teeth |
| 3. Caudal | Resting position of the tongue directed towards the lower anterior teeth |
| Swallowing pattern | |
| 1. Physiological | Characterized by tongue contact with the hard palate and the simultaneous absence of tongue contact with the anterior and canine teeth when swallowing, while the lip and mentalis muscles are inactive |
| 2. Anterior interdental | Tip of the tongue presses between the anterior incisors |
| 3. Anterior addental | Tip of the tongue presses against the lower incisors |
| 4. Lateral interdental | The tongue presses against or between the posterior teeth |
| Articulation | |
| /l,n,d,t/ | |
| 1. Physiological | Tip of the tongue touches the incisive papilla while speaking |
| 2. Inter- or addental | Tip of the tongue presses between or against the anterior teeth while speaking |
| /s/ | |
| 1. Physiological | Tip of the tongue is behind the lower anterior teeth while speaking |
| 2. Addental | Tip of the tongue touches the upper anterior teeth while speaking |
| 3. Interdental | Tip of the tongue is between the anterior teeth while speaking |
| 4. Lateral | Tongue edges are between the posterior teeth while speaking |
The lack of contact between the lower central incisors and their antagonists or the palate was evaluated at T0, T1, and T2.
Statistical analysis
An analysis of covariance (ANCOVA) was performed separately on the tongue pressure measurements at T1 and T2, using the baseline pressure level as a covariate. OMT (no/yes) and expansion (no/yes) are considered factors in the ANCOVA model. An estimate of the difference between OMT and non-OMT patients is given for the patients with and without expansion separately, followed by the effect estimate for both groups of patients combined. Furthermore, it has been verified if the effect of OMT depends on expansion (by evaluating the interaction between expansion and OMT in the ANCOVA).
Since the randomization was stratified on expansion, the comparison of proportions between patients with and without OMT was done based on a common odds ratio (OR) in a stratified 2×2 table. The two-sided P-value from an exact test for the common OR is reported and an exact two-sided 95% confidence interval (CI) has been constructed. The homogeneity of the ORs in the two strata is verified with Zelen’s test.
The alpha-level was set at 0.05 in this pilot study. A single significant P-value needs to be interpreted with caution since due to the exploratory character of the study no corrections for multiple testing are considered. All analyses were performed using SAS software for Windows (SAS Institute Inc., Cary, NC, USA).
Results
At baseline, 31.8% of the children did not have vertical overlap between their lower and upper central incisors. The other individuals (68.2%) did have an anterior non-occlusion. All children showed a non-physiological swallowing pattern (water and/or solid swallow) and 95.5% also had a non-physiological (addental, interdental, or caudal) tongue position at rest.
Age distribution and the mean maximum tongue elevation pressure at T0, T1, and T2 are represented in Table 4. At T1, the difference in maximum tongue pressure between all OMT and non-OMT subjects, aggregated over both strata and using the baseline pressure as a covariate, was significant (estimate difference 5.6 kPa; P = 0.015). The interaction between OMT and expansion was non-significant (P = 0.379), hence reporting the combined effect is meaningful. Note however that whereas in the stratum of patients without expansion the effect was significant (MYO compared with CON, P = 0.016), evidence was lacking in the stratum of patients with expansion (COMBI compared with EXP, P = 0.28). Also at T2, there was a significant higher pressure for OMT subjects compared to non-OMT subjects (estimate difference 7.6 kPa; P = 0.004). Again, no interaction between OMT and expansion was found (P = 0.94). At this timepoint, tongue pressure was found to be significantly increased in MYO and COMBI subgroups, respectively compared with CON and EXP subgroups (P = 0.029 and P = 0.040).
Table 4.
Age distribution and maximum tongue elevation pressure (expressed in kiloPascal).
| No expansion | Expansion | |||
|---|---|---|---|---|
| OMT (MYO) | Non-OMT (CON) | OMT (COMBI) | Non-OMT (EXP) | |
| N | 6 | 4 | 6 | 6 |
| Mean age (SD) | 8.3 (0.8) | 9.1 (1.2) | 8.4 (0.3) | 8.7 (0.9) |
| Mean (SD) pressure at T0 | 36.3 (9.9) | 43.9 (15.0) | 48.2 (7.5) | 38.3 (12.1) |
| Mean (SD) pressure at T1 | 45.4 (7.4) | 44.7 (16.3) | 51.8 (9.3) | 39.6 (11.2) |
| Mean (SD) pressure at T2 | 46.1 (7.4) | 44.2 (14.5) | 52.3 (8.2) | 37.5 (7.6) |
SD, standard deviation.
At the end of treatment 10.0% and 8.3% of the respectively OMT and non-OMT subjects had contact between the lower central incisors and their antagonists or palate. This difference was not significant. However, at T2 there was a significant difference between both groups (OR = 12.200, P = 0.036; 60.0% in the OMT group and 8.3% in the non-OMT group). There was no evidence that the ORs were different in both subgroups with or without expansion (T1, P = 1.000; T2, P = 0.471, Table 5).
Table 5.
Observed frequencies (%) of positive outcome in OMT and non-OMT patients aggregated over both strata (expansion–no expansion).
| Timepoint | OMT (N = 10) | Non-OMT (N = 12) | OR (CI) | P-value OR | P-value Zelen | |
|---|---|---|---|---|---|---|
| AOB | T1 | 1 (10%) | 1 (8.3%) | 1.00 (0.011; 94.0) | 1.00 | >0.99 |
| T2 | 6 (60%) | 1 (8.3%) | 12.2 (1.1; 669) | 0.036 | 0.47 | |
| Tong posture at rest | T1 | 6 (60%) | 0 (0%) | ND (2.8; ND) | 0.006 | — |
| T2 | 6 (60%) | 1 (8.3%) | 12.2 (1.1; 669) | 0.036 | 0.47 | |
| Swallowing pattern (water) | T1 | 4 (40%) | 1 (8.3%) | 6.67 (0.49; 334) | 0.23 | 0.47 |
| T2 | 5 (50%) | 1 (8.3%) | 25.0 (0.93; 1035) | 0.059 | >0.99 | |
| Swallowing pattern (solid) | T1 | 6 (60%) | 1 (8.3%) | 15.0 (1.12; 669) | 0.036 | >0.99 |
| T2 | 5 (50%) | 0 (0%) | ND (2.19; ND) | 0.015 | — | |
| Articulation /l,n,d,t/ | T1 | 2 (20%) | 0 (0%) | ND (0.35; ND) | 0.40 | — |
| T2 | 1 (10%) | 1 (8.3%) | 1.25 (0.02; 98) | >0.99 | >0.99 | |
| Articulation /s/ | T1 | 6 (50%) | 4 (33.3%) | 3.9 (0.44; 45) | 0.34 | >0.99 |
| T2 | 1 (10%) | 3 (25%) | 0.34 (0.01; 5.36) | 0.76 | >0.99 |
OR, odds ratios for the effect of OMT with exact 95% confidence intervals (CI) and P value. P-value Zelen, test for the interaction between OMT and expansion (homogeneity of the ORs between both strata). ND, not defined due to the presence of cells with zero observations.
Tongue posture at rest was physiological in 10.0% of the OMT subjects and in 0.0% of the non-OMT subjects. At T1, respectively 60.0% and 0.0% demonstrated a normal rest posture and the difference was found to be significant (P = 0.006). At six months follow-up, the difference was also significant (P = 0.036, 60.0% and 8.3%) and no evidence was found that the ORs were different in both subgroups with or without expansion (P = 0.471). The common ORs and 95% CIs are shown in Table 5.
No difference was found between the amount of OMT subjects and non-OMT subjects showing a physiological pattern of water swallowing at T1. At 6 months follow-up, the percentages were respectively 50.0% and 8.3% but were not found to be statistically significant (P = 0.059). The common ORs and 95% CIs are shown in Table 5. During the swallowing assessment on solid food, a significant difference between both groups was observed at T1 and T2 (P = 0.036 and P = 0.015, respectively). There was no evidence that the ORs were different in both subgroups with or without expansion (Table 5).
At baseline, 21 of all subjects showed a non-physiological articulation of /s/. At T1 and T2 no significant difference between the OMT and non-OMT subjects was observed (P = 0.338 and P = 0.758, respectively). Also, the /l,n,d,t/ articulation had not significantly improved in the OMT children at the end of treatment and after short-term follow-up (P = 0.400 and P = 1.000). The common ORs and 95% CIs are represented in Table 5.
Discussion
This pilot study has a strict exploratory character and aims to stimulate further research in the field of OMT. Randomization had been stratified on the presence of a transversal crossbite. If a crossbite was present, expansion of the upper arch was intended to correct the transversal discrepancy and to provide more space for the tongue. The interrelation between maxillary constriction and orofacial dysfunctions is highlighted in the literature (43, 44) and the correction of maxillary constriction has been regarded as an additional target for early treatment in AOB patients (30, 45). Since no interaction between OMT and expansion was found, all OMT subjects with and without expansion might be combined into one major group to investigate the effect of OMT. Although it was assumed that the resin of the expansion plate on the palate may interfere with the tongue position, this was not confirmed by the results. A lack of evidence exists whether OMT should start prior to orthodontic treatment or not. Speech pathologists and orthodontists seem to have different opinions on this subject (46). Mason and Role (47) argue that if a posterior crossbite exists the treatment should be accomplished prior to the initiation of OMT. However in our study, the COMBI first group underwent 10 hours of OMT prior to maxillary expansion due to practical reasons. In this study, all OMT subjects underwent the same standardized protocol of myofunctional training. In typical clinical settings however, OMT exercise regimens and duration of therapy are often tailored to the needs and responses of each individual patient. No consensus can be found in the literature regarding the ideal protocol to treat orofacial dysfunction. More research concerning different treatment protocols would be of value. This study included subjects in the early or intermediate mixed dentition, to correct the aberrant tongue function at an early age. Different opinions are expressed in the literature regarding the ideal age to start OMT (48). Some dentists recommend treatment or have successfully treated pediatric patients under the age of 10 years with the aid of OMT (33, 40, 44). On the other hand, others authors suggest waiting until patients are 10 years of age or older, because of the possibility of spontaneous closure of the AOB (49). OMT aims to harmonize the orofacial functions and to exclude factors interfering with the normal development of the dental arches. In this study, the children were assumed to be old enough to understand the aim and exercises of OMT and the authors do believe in the adaptability of young tissues. A comparable control group, matched for age and gender, was also followed-up to eliminate changes due to growth and maturation. However, at this young age, a tongue thrust can be the result of a ‘gap-filling’ tendency which may impede treatment and the available oral space might not be developed enough in all subjects. It is obvious that there is a lack of evidence defining the ideal age to start OMT and more research is needed.
Patients with oral phase swallowing problems are assumed to have a tongue strength that is significantly lower than in normal subjects (50). Several methods have been used to measure tongue strength as pressure within the oral cavity, including strain-gauge manometry, force sensitive resistors and bulb pressure sensors, like the IOPI system (3, 4, 51–58). The IOPI has been utilized in many published experiments, mainly in speech and language pathology, and has established high inter- and intrajudge reliability (59–62). Potter and Short (56) concluded that maximum tongue strength can reliably be evaluated in pediatric patients using the IOPI. In this study, a significant increase in maximal tongue pressure was found in subjects who received OMT compared to those without at T1. This finding presumes that the tongue musculature was effectively strengthened by the daily exercises of the myofunctional program. The increase was maintained at short-term follow-up. Although there was an increase in strength in the OMT subjects at T1 and T2, the maximum pressure values were not necessarily higher in subjects with OMT compared to subjects without. In cross-sectional studies no differences in maximum tongue pressure are found between children with and without tongue interposition during swallowing (32, 51, 63). This finding can be explained by a large inter-participant variation in tongue strength (3, 64, 65). The authors believe that it would be difficult to control the inter-participant variation because of the varied functional responses among subjects and similarities in occlusion and facial morphology do not account for similarities in functional pattern. This has been described by Di Fazio et al. (64) as well.
Observation of the tongue movements during swallowing with lips apart is a simple and fast method for diagnosing the swallowing pattern. However, since the lips are involved in the act of swallowing, some authors argue that a forced opening of the lips might disturb an individual swallowing pattern (12, 66). Effort has been made in the literature to evaluate the swallowing type in a more objective way, by using techniques like radiocinematography, electropalatography, and electromagnetic articulography (5, 6, 10, 38). However, due to many reasons, especially the risk of irradiation, these techniques did not prove to be appropriate for observation in small growing children (12, 66). Also the use of ultrasonography to assess swallowing type has been described (12, 66). Yet, the reliability of this method has not been extensively verified. The fact that a clinical diagnosis is subjective in nature and inter-individual variability of tongue position and motility might influence the swallowing type assessment, must be taken into account (67). Another method to overcome this problem is the Payne technique advocated by Garliner, whereby fluorescent orabase paste is applied on the tongue (68). However, for practical reasons it was not used in this study.
As part of OMT the tongue can be re-trained, meaning that optimal motility of the tongue can be created (67). At T1 and T2, OMT did increase the proportion of subjects performing a correct swallow pattern, both during swallowing of water and solid food. This increase might be caused by the fact that some of the OMT children effectively achieved the habit correction, but it might be biased by the fact that some of these children just perform a correct swallow during the clinical trials or by the fact that the evaluation was not performed blindly. However, the transition from conscious to unconscious habit correction can not be assessed during a clinical examination. An intra-oral device sensitive for detecting tongue position and movements during daily activities can elucidate this problem. Cayley et al. (38) have reported that normal swallowing function resumes after OMT in subjects with AOB. However, in this study not all OMT children performed a correct swallow at T1. This might indicate that some children needed more training or more time to achieve a correct conscious swallow or that in some children OMT could not correct the aberrant swallowing pattern. The myofunctional protocol has to be adapted to the needs of every individual. As an active exercise concept, the success of OMT is also crucially dependent on motivation and compliance of both child and parents. An evaluation of patient’s cooperation would be of value for further research. During the OMT the children’s oral awareness increases. Since individuals with AOB and incorrect tongue position exhibit impaired gnostic sensibility of the tongue (8, 9), it has to be determined whether oral sensory perception can improve with training.
Various types of therapy for tongue dysfunction or faulty tongue posture have been reported in the literature like spurs, tongue cribs, vestibular shields, trainer appliances, and functional appliances; resulting in an increase of overbite at the end of treatment (25–27, 29, 31, 68–72). However, little is known about the adaptation of the soft tissues after the discontinuation of treatment, which can influence the stability of the obtained result. When a habit appliance is removed and the cause of the tongue pattern is not addressed, the forward tongue posture and functions are expected to return (73). Sayin et al. demonstrated that during deglutition in subjects with a tongue crib, adaptive changes occurred in selective regions of the tongue’s dorsum, to compensate for the posterior position of the tongue’s tip (71). However, it is not clear if these functional adaptations persist after discontinuation of the crib appliance. Meyer-Marcotty et al. hypothesized that spurs exert continuous control by means of a biofeedback mechanism in which they ‘inform’ the patient of the faulty tongue position (68). The neuro-physiological basis for their clinically observed correction of the dysfunction is a neuromuscular adaptation based on a somato-sensitive feedback. It is unclear if the functional adaptations remain after discontinuation of the spurs, since they did not mention post-treatment data. Knösel et al. mentioned that the instruction to position the tongue at the palate during deglutition or to perform tongue reposition manoeuvres appears to be a valid aid in training tongue-palate contact (70). They stated that the additional use of an oral screen did not produce a significant effect on the duration of the favourable cranial tongue rest position and so it can be dispensed. However, other authors found Face Former therapy (oral screen with lip piece) to be more successful than conventional OMT in establishing nasal breathing and a physiological swallowing pattern within a six months period. More research is needed to explore the benefits of this kind of treatment modality (39).
OMT aims to make the patient conscious of the false static and dynamic tongue position and to learn a physiological myofunctional behaviour. Although some authors assumed the tongue’s position at rest unconsciously except during exercises (68), our study demonstrated a significant increase of subjects with a physiological tongue posture at rest and during swallowing after completion of OMT. At T2 the children with a normal tongue posture at rest did had contact between the lower central incisors and their antagonists or the palate. This finding hypothesized that OMT effectively changed the rest posture of the tongue in some individuals. Since the tongue was positioned at the palatal aspect of the alveolar ridge in these subjects, the further eruption of the lower incisors was no longer impeded by the tongue. This high percentage of subjects with contact is influenced by the fact that at baseline most of the subjects had an anterior non-occlusion. The authors do not presume that OMT per se cause morphological alterations in subjects with more severe or skeletal open bites. OMT is not a substitute for orthodontic treatment and inducing morphological changes is even not a primary purpose of OMT. However, our findings demonstrate that OMT can be a helpful adjunct to orthodontic treatment in patients with aberrant tongue behaviour. Other authors emphasized the potential of myofunctional treatment as well (32,33,35,40). Nevertheless, further research is needed to elucidate factors influencing the outcome of OMT, in order to select the appropriate patients.
Children with articulatory speech disorders are reported to have systematically more inaccurate tongue movements and poor movement coordination than children without speech defects (74). The most common misarticulations associated with orofacial myofunctional disorders are inter- or addental production of apico-alveolar consonants like /s,z,n,l,d,t/. Eslamian and Leilazpour (74) demonstrated in their study that during the pronunciation of these consonants the tongue made contact more anteriorly on the palate in individuals with tongue malfunction than in those without. However during pronunciation of whole words, the contact points were located similarly on the palate in both groups. This study demonstrated a non-significant difference in both groups on the physiological production of /s/ and /l,n,d,t/ during Dutch test sentences at T1 and T2. Korbmacher et al. (39) didn’t find an improvement of the articulation of /s/ after OMT as well. Although the OMT protocol in our study includes some articulation exercises and strengthening of the anterior and mid part of the tongue musculature is intended, no significant improvement was found.
Further research is recommended by means of larger, blindly performed and long-term follow-up studies, to confirm our results, to clarify the success of OMT as an adjunct to orthodontic treatment and to identify possible factors influencing the outcome.
Conclusion
OMT can positively influence tongue behaviour. However, further research is recommended to confirm our results, to clarify the success of OMT as an adjunct to orthodontic treatment and to identify possible factors influencing the outcome.
Acknowledgments
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- 1. Stahl F. and Grabowski R (2003) Orthodontic findings in the deciduous and early mixed dentition—inferences for a preventive strategy. Journal of Orofacial Orthopedics, 64, 401–416. [DOI] [PubMed] [Google Scholar]
- 2. Proffit W.R. (1978) Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthodontist, 48, 175–186. [DOI] [PubMed] [Google Scholar]
- 3. Proffit W.R. Chastain B.B. and Norton L.A (1969) Linguopalatal pressure in children. American Journal of Orthodontics, 55, 154–166. [DOI] [PubMed] [Google Scholar]
- 4. Proffit W.R. McGlone R.E. and Barrett M.J (1975) Lip and tongue pressures related to dental arch and oral cavity size in Australian aborigines. Journal of Dental Research, 54, 1161–1172. [DOI] [PubMed] [Google Scholar]
- 5. Ichida T. Takiguchi R. and Yamada K (1999) Relationship between the lingual–palatal contact duration associated with swallowing and maxillofacial morphology with the use of electropalatography. American Journal of Orthodontics and Dentofacial Orthopedics, 116, 146–151. [DOI] [PubMed] [Google Scholar]
- 6. Fujiki T. Takano-Yamamoto T. Noguchi H. Yamashiro T. Guan G. and Tanimoto K (2000) A cineradiographic study of deglutitive tongue movement and nasopharyngeal closure in patients with anterior open bite. Angle Orthodontist, 70, 284–289. [DOI] [PubMed] [Google Scholar]
- 7. Cheng C.F. Peng C.L. Chiou H.Y. and Tsai C.Y (2002) Dentofacial morphology and tongue function during swallowing. American Journal of Orthodontics and Dentofacial Orthopedics, 122, 491–499. [DOI] [PubMed] [Google Scholar]
- 8. Premkumar S. Avathvadi Venkatesan S. and Rangachari S (2011) Altered oral sensory perception in tongue thrusters with an anterior open bite. European Journal of Orthodontics, 33, 139–142. [DOI] [PubMed] [Google Scholar]
- 9. Koczorowski M. Gedrange T. and Koczorowski R (2012) Changes of oral sensibility in subjects with partial anterior open bite and the incorrect position of the tongue. Annals of Anatomy, 194, 220–223. [DOI] [PubMed] [Google Scholar]
- 10. Cayley A.S. Tindall A.P. Sampson W.J. and Butcher A.R (2000) Electropalatographic and cephalometric assessment of tongue function in open bite and non-open bite subjects. European Journal of Orthodontics, 22, 463–474. [DOI] [PubMed] [Google Scholar]
- 11. Sayin M.Ö. Akin E. Karaçay Ş. and Bulakbaşi N (2006) Initial effects of the tongue crib on tongue movements during deglutition: a cine-magnetic resonance imaging study. Angle Orthodontist, 76, 400–405. [DOI] [PubMed] [Google Scholar]
- 12. Peng C. Jost-Brinckmann P. Yoshida N. Miethke R. and Lin C (2003) Differential diagnosis between infantile and mature swallowing with ultrasonography. European Journal of Orthodontics, 25, 451–456. [DOI] [PubMed] [Google Scholar]
- 13. Horn H. Kühnast K. Axmann-Krcmar D. and Göz G (2004) Influence of orofacial dysfunctions on spatial and temporal dimensions of swallowing movements. Journal of Orofacial Orthopedics, 65, 376–388. [DOI] [PubMed] [Google Scholar]
- 14. Machado Junior A.J. and Crespo A.N (2012) Radiographic position of the hyoid bone in children with atypical deglutition. European Journal of Orthodontics, 34, 83–87. [DOI] [PubMed] [Google Scholar]
- 15. Christensen M. and Hanson M (1981) An investigation of the efficacy of oral myofunctional therapy as a precursor to articulation therapy for pre-first grade children. Journal of Speech and Hearing Disorders, 46, 160–165. [DOI] [PubMed] [Google Scholar]
- 16. Tausche E. Luck O. and Harzer W (2004) Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need. European Journal of Orthodontics, 26, 237–244. [DOI] [PubMed] [Google Scholar]
- 17. Keski-Nisula K. Lehto R. Lusa V. Keski-Nisula L. and Varrela J (2003) Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition. American Journal of Orthodontics and Dentofacial Orthopedics, 124, 631–638. [DOI] [PubMed] [Google Scholar]
- 18. Grippaudo F. Pantanali F. Paolantonio E.G. Grecolini M.E. Saulle R. La Torre G. and Deli R (2013) Prevalence of malocclusion in Italian schoolchildren and orthodontic treatment need. European Journal of Pediatric Dentistry, 14, 314–318. [PubMed] [Google Scholar]
- 19. Shalish M. Gal A. Brin I. Zini A. and Ben-Bassat Y (2013) Prevalence of dental features that indicate a need for early orthodontic treatment. European Journal of Orthodontics, 35, 454–459. [DOI] [PubMed] [Google Scholar]
- 20. Grippaudo F. Pantanali F. Paolantonio E.G. Grecolini M.E. Saulle R. La Torre G. and Deli R (2013) Orthodontic treatment timing in growing patients. European Journal of Pediatric Dentistry, 14, 231–236. [PubMed] [Google Scholar]
- 21. Klocke A. Nanda R.S. and Kahl-Nieke B (2002) Anterior open bite in the deciduous dentition: longitudinal follow-up and craniofacial growth considerations. American Journal of Orthodontics and Dentofacial Orthopedics, 122, 353–358. [DOI] [PubMed] [Google Scholar]
- 22. Worms F.W. Meskin L.H. and Isaacson R.J (1971) Open-bite. American Journal of Orthodontics, 59, 589–595. [DOI] [PubMed] [Google Scholar]
- 23. Cozza P. Baccetti T. Franchi L. Mucedero M. and Polimeni A (2005) Sucking habits and facial hyperdivergency as risk factors for anterior open bite in the mixed dentition. American Journal of Orthodontics and Dentofacial Orthopedics, 128, 517–519. [DOI] [PubMed] [Google Scholar]
- 24. Giuntini V. Franchi L. Baccetti T. Mucedero M. and Cozza P (2008) Dentoskeletal changes associated with fixed and removable appliances with a crib in open-bite patients in the mixed dentition. American Journal of Orthodontics and Dentofacial Orthopedics, 133, 70–80. [DOI] [PubMed] [Google Scholar]
- 25. Torres F. Almeida R.R. de Almeida M.R. Almeida-Pedrin R.R. Pedrin F. and Henriques J.F (2006) Anterior open bite treated with a palatal crib and high-pull chin cup therapy. A prospective randomized study. European Journal of Orthodontics, 28, 610–617. [DOI] [PubMed] [Google Scholar]
- 26. Torres F.C. Almeida R.R. Almeida-Pedrin R.R. Pedrin F. and Paranhos L.R (2012) Dentoalveolar comparative study between removable and fixed cribs, associated to chincup, in anterior open bite treatment. Journal of Applied Oral Science, 20, 531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pedrin F. Almeida M.R. Almeida R.R. Almeida-Pedrin R.R. and Torres F (2006) A prospective study of the treatment effects of a removable appliance with palatal crib combined with high-pull chincup therapy in anterior open-bite patients. American Journal of Orthodontics and Dentofacial Orthopedics, 129, 418–423. [DOI] [PubMed] [Google Scholar]
- 28. Menezes L.M. Ritter D.E. and Locks A (2013) Combining traditional techniques to correct anterior open bite and posterior crossbite. American Journal of Orthodontics and Dentofacial Orthopedics, 143, 412–420. [DOI] [PubMed] [Google Scholar]
- 29. Mucedero M. Franchi L. Giuntini V. Vangelisti A. McNamara J.A. and Cozza P (2013) Stability of quad-helix/crib therapy in dentoskeletal open bite: a long-term controlled study. American Journal of Orthodontics and Dentofacial Orthopedics, 143, 695–703. [DOI] [PubMed] [Google Scholar]
- 30. Cozza P. Baccetti T. Franchi L. and McNamara J.A (2006) Treatment effects of a modified quad-helix in patients with dentoskeletal open bites. American Journal of Orthodontics and Dentofacial Orthopedics, 129, 734–739. [DOI] [PubMed] [Google Scholar]
- 31. Cozza P. Mucedero M. Baccetti T. and Franchi L (2007) Treatment and posttreatment effects of quad-helix/crib therapy of dentoskeletal open bite. Angle Orthodontist, 77, 640–645. [DOI] [PubMed] [Google Scholar]
- 32. Andrianopoulos M.V. and Hanson M.L (1987) Tongue-thrust and the stability of overjet correction. Angle Orthodontist, 57, 121–135. [DOI] [PubMed] [Google Scholar]
- 33. Saccomanno S. Antonini G. D’Alatri L. D’Angeloantonio M. Fiorita A. and Deli R (2014) Case report of patients treated with an orthodontic and myofunctional protocol. European Journal of Paediatric Dentistry, 15, 184–186. [PubMed] [Google Scholar]
- 34. Mason R.M. (2008) A retrospective and prospective view of orofacial myology. International Journal of Orofacial Myology, 34, 5–14. [PubMed] [Google Scholar]
- 35. Takahashi O. Iwasawa T. and Takahashi M (1995) Integrating orthodontics and oral myofunctional therapy for patients with oral myofunctional disorders. International Journal of Orofacial Myology, 21, 66–72. [PubMed] [Google Scholar]
- 36. Takahashi S. Kuribayaski G. Ono T. Ishiwata Y. and Kuroda T (2005) Modulation of masticatory muscle activity by tongue position. Angle Orthodontist, 75, 35–39. [DOI] [PubMed] [Google Scholar]
- 37. Benkert K.K. (1997) The effectiveness of orofacial myofunctional therapy in improving dental occlusions. International Journal of Orofacial Myology, 23, 35–46. [PubMed] [Google Scholar]
- 38. Cayley A.S. Tindall A.P. Sampson W.J. and Butcher A.R (2000) Electropalatographic and cephalometric assessment of myofunctional therapy in open-bite subjects. Australian Journal of Orthodontics, 16, 23–33. [PubMed] [Google Scholar]
- 39. Korbmacher H.M. Schwan M. Berndsen S. Bull J. and Kahl-Nieke B (2004) Evaluation of a new concept of myofunctional therapy in children. International Journal of Orofacial Myology, 30, 39–52. [PubMed] [Google Scholar]
- 40. Smithpeter J. and Covell D (2010) Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. American Journal of Orthodontics and Dentofacial Orthopedics, 137, 605–614. [DOI] [PubMed] [Google Scholar]
- 41. Vanderwegen J. Guns C. Van Nuffelen G. Elen R. and De Bodt M (2013) The influence of age, sex, bulb position, visual feedback, and the order of testing on maximum anterior and posterior tongue strength and endurance in healthy belgian adults. Dysphagia, 28, 159–166. [DOI] [PubMed] [Google Scholar]
- 42. Stahl F. Grabowski R. Gaebel M. and Kundt G (2007) Relationship between occlusal findings and orofacial myofunctional status in primary and mixed dentition. Part II: prevalence of orofacial dysfunctions. Journal of Orofacial Orthopedics, 68, 74–90. [DOI] [PubMed] [Google Scholar]
- 43. Ballanti F. Franchi L. and Cozza P (2009) Transverse dentoskeletal features of anterior open bite in the mixed dentition. Angle Orthodontist, 79, 615–620. [DOI] [PubMed] [Google Scholar]
- 44. Seemann J. Kundt G. and Stahl de Castrillon F (2011) Relationship between occlusal findings and orofacial myofunctional status in primary and mixed dentition: part IV: interrelation between space conditions and orofacial dysfunctions. Journal of Orofacial Orthopedics, 72, 21–32. [DOI] [PubMed] [Google Scholar]
- 45. Aznar T. Galán A.F. Marín I. and Domínguez A (2006) Dental arch diameters and relationships to oral habits. Angle Orthodontist, 76, 441–445. [DOI] [PubMed] [Google Scholar]
- 46. Umberger F.G. Weld G.L. and Van Rennen J.S (1985) Tongue thrust: attitudes and practices of speech pathologists and orthodontists. International Journal of Orofacial Myology, 11, 5–13 [PubMed] [Google Scholar]
- 47. Mason R.M. and Role E.B (2009) Did you know? A question and answer dialogue for the orofacial myologist. International Journal of Orofacial Myology, 35, 5–17. [PubMed] [Google Scholar]
- 48. Spreidel T. Isaacson R. and Worms F (1972) Tongue thrust therapy and anterior dental open bite. American Journal of Orthodontics, 62, 287–295. [DOI] [PubMed] [Google Scholar]
- 49. Proffit W.R. and Mason R.M (1975) Myofunctional therapy for tongue-thrusting: background and recommendations. Journal of the American Dental Association, 90, 403–411. [DOI] [PubMed] [Google Scholar]
- 50. Lazarus C.L. Logemann J.A. Pauloski B.R. Rademaker A.W. Larson C.R. Mittal B.B. and Pierce M (2000) Swallowing and tongue function following treatment for oral and oropharyngeal cancer. Journal of Speech Language and Hearing Research, 43, 1011–1023. [DOI] [PubMed] [Google Scholar]
- 51. Lambrechts H. De Baets E. Fieuws S. and Willems G (2010) Lip and tongue pressure in orthodontic patients. European Journal of Orthodontics, 32, 466–471. [DOI] [PubMed] [Google Scholar]
- 52. Youmans S.R. and Stierwalt J.A (2006) Measures of tongue function related to normal swallowing. Dysphagia, 21, 102–111. [DOI] [PubMed] [Google Scholar]
- 53. Stierwalt J.A. and Youmans S.R (2007) Tongue measures in individuals with normal and impaired swallowing. American Journal of Speech-Language Pathology, 16, 148–156. [DOI] [PubMed] [Google Scholar]
- 54. Hewitt A. Hind J. Kays S. Nicosia M. Doyle J. Tompkins W. Gangnon R. and Robbins J (2008) Standardized instrument for lingual pressure measurement. Dysphagia, 23, 16–25. [DOI] [PubMed] [Google Scholar]
- 55. Utanohara Y. Hayashi R. Yoshikawa M. Yoshida M. Tsuga K. and Akagawa Y (2008) Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device. Dysphagia, 23, 286–290. [DOI] [PubMed] [Google Scholar]
- 56. Potter N.L. and Short R (2009) Maximal tongue strength in typically developing children and adolescents. Dysphagia, 24, 391–397. [DOI] [PubMed] [Google Scholar]
- 57. Yoshikawa M. Yoshida M. Tsuga K. Akagawa Y. and Groher M.E (2011) Comparison of three types of tongue pressure measurement devices. Dysphagia, 26, 232–237. [DOI] [PubMed] [Google Scholar]
- 58. Clark H.M. and Solomon N.P (2012) Age and sex difference in orofacial strength. Dysphagia, 27, 2–9. [DOI] [PubMed] [Google Scholar]
- 59. Clarck H.M. Henson P.A. Barber W.D. Stierwalt J.A. and Sherrill M (2003) Relationships among subjective and objective measures of tongue strength and oral phase swallowing impairments. American Journal of Speech-Language Pathology, 12, 40–50. [DOI] [PubMed] [Google Scholar]
- 60. Vanderwegen J. Guns C. Van Nuffelen G. Elen R. and De Bodt M (2013) Factors affecting tongue strength and endurance. Dysphagia, 28, 159–166. [DOI] [PubMed] [Google Scholar]
- 61. Youmans S.R. and Stierwalt J.A (2006) Measures of tongue function related to normal swallowing. Dysphagia, 21, 102–111. [DOI] [PubMed] [Google Scholar]
- 62. Adams V. Mathisen B. Baines S. Lazarus C. and Callister R (2013) A systematic review and meta-analysis of measurements of tongue and hand strength and endurance using the Iowa Oral Performance Instrument (IOPI). Dysphagia, 28, 350–369. [DOI] [PubMed] [Google Scholar]
- 63. Dworkin J.P. and Culatta R.A (1980) Tongue strength: its relationship to tongue thrusting, open-bite, and articulatory proficiency. Journal of Speech and Hearing Disorders, 45, 277–282. [DOI] [PubMed] [Google Scholar]
- 64. Di Fazio D. Lombardo L. Gracco A. D’Amico P. and Siciliani G (2011) Lip pressure at rest and during function in 2 groups of patients with different occlusions. American Journal of Orthodontics and Dentofacial Orthopedics, 139, e1–e6. [DOI] [PubMed] [Google Scholar]
- 65. Posen A.L. (1972) The influence of maximum perioral and tongue force on the incisor teeth. Angle Orthodontist, 42, 285–309. [DOI] [PubMed] [Google Scholar]
- 66. Ovsenik M. Volk J. and Music Marolt M (2014) A 2D ultrasound evaluation of swallowing in children with unilateral posterior crossbite. European Journal of Orthodontics, 36, 665–671. [DOI] [PubMed] [Google Scholar]
- 67. Mehnert J. Landau H. Orawa H. Kittel A. Krause M. Engel S. Jost-Brinkmann P.G. and Müller-Hartwich R (2009) Validity and reliability of logopedic assessments of tongue function. Journal of Orofacial Orthopedics, 70, 468–484. [DOI] [PubMed] [Google Scholar]
- 68. Meyer-Marcotty P. Hartmann J. and Stellzig-Eisenhauer A (2007) Dentoalveolar open bite treatment with spur appliances. Journal of Orofacial Orthopedics, 68, 510–521. [DOI] [PubMed] [Google Scholar]
- 69. Knösel M. Klein S. Bleckmann A. and Engelke W (2011) Tongue position after deglutition in subjects with habitual open-mouth posture under different functional conditions. Orthodontics and Craniofacial Research, 14, 181–188. [DOI] [PubMed] [Google Scholar]
- 70. Bosio J.A. and Justus R (2013) Treatment and retreatment of a patient with a severe anterior open bite. American Journal of Orthodontics and Dentofacial Orthopedics, 144, 594–606. [DOI] [PubMed] [Google Scholar]
- 71. Sayin M.Ö. Akin E. Karaçay Ş. and Bulakbaşi N (2006) Initial effects of the tongue crib on tongue movements during deglutition: a cine-magnetic resonance imaging study. Angle Orthodontist, 76, 400–405. [DOI] [PubMed] [Google Scholar]
- 72. Koskimies M. Pahkala R. and Myllykangas R (2011) Palatal training appliances in children with mild to moderate oral dysfunctions. Journal of Clinical Pediatric Dentistry, 36, 149–154. [DOI] [PubMed] [Google Scholar]
- 73. Mason R.M. and Franklin H (2009) Position statement of the International Association of Orofacial Myology regarding: appliance use for oral habit patterns. International Journal of Orofacial Myology, 35, 74–76. [PubMed] [Google Scholar]
- 74. Eslamian L. and Leilazpour A.P (2006) Tongue to palate contact during speech in subjects with and without a tongue thrust. European Journal of Orthodontics, 28, 475–479. [DOI] [PubMed] [Google Scholar]