Summary
Objectives:
The aim was to identify a prediction model for root resorption (RR) caused by impacted canines based on radiographic variables assessed on 2D panoramic radiographs with the intention to reduce the need for additional cone beam computed tomography (CBCT) imaging.
Materials and methods:
Three hundred and six patients (188 female, 118 male; mean age, 14.7 years; standard deviation, 5.6; range, 8.4–47.2 years) were included in the study. In total, 406 impacted maxillary canines were studied, from 206 patients with unilateral impaction and from 100 patients with bilateral impaction. Initial 2D panoramic radiography was available, and 3D CBCT imaging was obtained upon clinical indication. The generated radiographic variables and specific features investigated were collected on 2D panoramic imaging and were correlated to the presence/absence of RR detected on CBCT. A validation sample consisting of 55 canines from 45 patients with maxillary canine impactions was collected to validate the outcome of the present study.
Results:
The incidence of RR of the adjacent teeth was 33.8%. A prediction model using panoramic images for the possible presence of RR was established [area under the curve (AUC) = 0.74, 95% confidence interval (CI): 0.69–0.79] and validated by applying leave-one-out cross-validation (AUC = 0.71, 95% CI: 0.66–0.77). For the subgroup of presence of severe RR the discriminative ability increased to 0.80. In this prediction model, patient gender, canine apex, vertical canine crown position, and canine magnification were the strongest predictors for RR.
Conclusions:
The final prediction model for RR based on available panoramic radiographs could be a helpful tool in justifying the need of additional CBCT examination.
Introduction
Impaction of the maxillary canine during development of the dentition is a common phenomenon. The most common undesirable, irreversible, and adverse sequela of maxillary canine impaction is root resorption (RR) of the adjacent teeth (1). RR is defined as loss of tooth cementum and/or dentin associated with a physiological or pathological activity of the tooth-resorbing cells (2).
Clinical and radiographic evaluation of impacted maxillary canines involves the assessment of several factors that influence overall treatment and prognosis. The most important factor is confirmation of the presence or absence of RR in adjacent incisors. The presence of RR may have a significant effect on tooth extraction strategies. When RR is diagnosed before orthodontic treatment begins, a decision must be made whether to extract the resorbed tooth, followed by orthodontic alignment of the impacted canine, space closure, and reshaping, or whether to move the impacted canine away from the resorbed tooth. This will likely cause further resorption if the direction of traction is not controlled. Incisor RR is asymptomatic and mainly detected based on radiographic examination. Conventional two-dimensional radiographs, such as panoramic radiographs, are usually taken for initial diagnosis and treatment planning certainly in cases of impacted canines. Furthermore, the use of a combination of 2D radiographs has been suggested (3). For early diagnosis and detection of lateral incisor RR as well as exact canine localization, cone beam computed tomography (CBCT) has been recommended for use in impacted canine cases. The diagnostic ability and reliability of CBCT in detecting RR caused by impacted canines have been demonstrated. A small voxel size with high resolution was recommended for less noise and better image quality (4). Until now, CBCT could not be used as a primary imaging mechanism for impacted canines, replacing the conventional modality, because of radiation dose, equipment availability and cost. Moreover, patients undergoing orthodontic treatment receive repeated X-ray exposure after the initial radiographic examination (5). ALARA principles and SedentexCT guidelines state that CBCT examination should not be used indiscriminately and should be used in selected orthodontic cases in which conventional radiography cannot supply sufficient diagnostic information (6). Therefore, CBCT should not be used routinely to obtain radiographs for orthodontic patients, but should be justified, with caution, for specific patients. Therefore, radiation exposure should be minimized as much as possible for patient benefit.
Using CBCT evaluation of impacted canine improves canine localization to adjacent teeth and provides higher level of confidence in the treatment plan than compared to 2D images (7, 8). However, there is conflicting evidence on the actual usefulness of CBCT in orthodontic treatment planning. Some studies have shown that information from 3D images is better than that from combined conventional 2D radiographs and may alter treatment planning (9, 10). On the other hand, other studies have found that the treatment planning for impacted canines did not differ whether 2D or 3D information is present (7, 8, 11).
Aetiological factors of RR have been proposed (12–19). However, there has been considerable debate regarding the radiographic predisposing factors of RR. More evidence-based research is necessary to define the justified use of CBCT. Moreover, no validation has been performed on suggested predictive factors, nor has a prediction formula been developed based on 2D panoramic radiographs to indicate the risk of possible RR and the need for supplementary CBCT examination. The aim of this study was to identify a prediction model for RR caused by impacted canines based on parameters evaluated on 2D panoramic radiographs with the intention to reduce the need for additional CBCT imaging.
Materials and methods
Three hundred and six patients (188 female, 118 male; mean age, 14.7 years; standard deviation, 5.6; range, 8.4–47.2 years) were included in the study. Patients were identified and selected from among those seeking orthodontic treatment at the Department of Oral Health Sciences, KU Leuven and Dentistry, University Hospitals Leuven, Leuven, Belgium. The selection criteria were: 1. All patients were non-syndromic; 2. each patient presented at least one impacted maxillary canine; 3. no orthodontic treatment had been performed; and 4. each patient had 2D panoramic radiographs and CBCT scans available within a maximum interval of 2 weeks. The study protocol was approved by the medical ethics committee board of UZ-KU Leuven university, Belgium (Approval number: B32220083749, S50910). In total 306 patients were included in the study, 100 of them having a bilateral impaction, resulting in 406 impacted maxillary canines. The diagnosis of impacted canine was determined, from the patients’ dental records, as a failure of the canine to erupt at its appropriate site in the dental, based on clinical and radiographic assessment. For all patients, CBCT scans had been clinically justified prior to the start of this study to define canine location, presence of possible RR on adjacent teeth, and treatment needs.
Digital panoramic radiographic images of 137 patients were taken with Cranex TOME® (Soredex, Helsinki, Finland) and 169 patients were taken with Veraviewepocs 2D® (J. Morita, Kyoto, Japan). The exposure parameters of Cranex TOME® were 15 seconds, 65kV, and 15 mA. The Veraviewepocs 2D® panoramic was taken with a high-resolution CCD sensor with exposure parameters 7.4 seconds, 64kV, and 8.9 mA.
CBCT scans were carried out with two CBCT systems. The first involved a 3D Accuitomo-XYZ Slice View Tomograph (J. Morita) with a voxel size of 0.125mm (40mm × 40mm, 60mm × 60mm, and 80mm × 80mm). Parameters included a tube voltage of 80kV, a tube current of 3 mA, and a scanning time of 18 seconds. The second CBCT system was a SCANORA® 3D CBCT (Soredex, Tuusula, Finland) with a voxel size of 0.2mm (FOV 75mm × 100mm), tube voltage of 85kV, current of 10 mA, and a scanning time of 3.7 seconds. One hundred and thirty-seven patients were scanned with Accuitomo CBCT and 169 patients were scanned with Scanora CBCT.
The radiographic measurements along with measurement of specific features, were obtained from 2D panoramic images and correlated to the presence/absence of RR detected on CBCT, which was used as a baseline.
The evaluation protocol
All parameters and measurements were performed by two observers. The radiographic assessment was obtained from 2D panoramic images except parameter 1, 2, and 3 which were evaluated on CBCT.
1. The presence and severity of incisor RR, and whether resorption defects were present in lateral and/or central incisors, were determined. The severity of RR was recorded from CBCT images based on the grading systems suggested by Ericson and Kurol (20).
2. When RR was diagnosed from CBCT images, its location in either the apical, middle, or cervical third was recorded.
3. Canine position in relation to adjacent teeth was determined from CBCT images, to be either palatal, buccal, or in line of the arch.
4. Primary maxillary canine was assigned to one of three categories: (a) missing tooth, where the deciduous canine had been extracted; (b) no RR; or (c) RR.
5. Crowding in the upper anterior region was assessed as a ‘yes/no’ feature.
6. Anterior apical area was defined as the space in the area between the mesial surface of the upper right and left canines. It was evaluated whether this space is adequate for normal eruption or not and this was recorded to be either ‘optimal’ (the space is optimal and adequate), ‘small’ (the space is slightly reduced), or ‘severe apical area’ (the space is severely reduced).
7. Mesio-distal space available for the canine was assigned to one of three categories, modified from Cernochova et al. (18) as follows: (a) lack of space for the erupting canine, (b) complete loss of space, or (c) sufficient space available for the canine.
8. Canine magnification: ‘Yes’: If the impacted canine looks relatively magnified in comparison to the adjacent teeth or in comparison to the contra-lateral canine. ‘No’: if the canine is not magnified or appeared smaller were considered not magnified (3).
9. Canine apex was determined to be either open, closed, or dilacerated.
10. Canine impaction was determined to be either ‘vertical’ if the canine angle to midline was less than 45 degree or ‘horizontal’ if the canine angle to midline was more than 45 degree.
11. Canine development was assigned to one of four categories based on root development: complete development; three-fourth of the root developed; half of the root developed; and one-fourth of the root developed.
12. Presence of abnormalities, such as a mesiodens or supernumerary tooth, peg-shaped lateral incisor, agenesis of permanent teeth, and impaction of other permanent teeth, was identified.
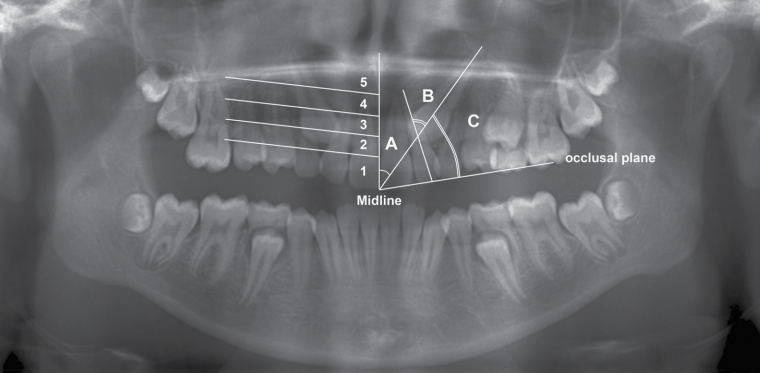
13. Permanent maxillary canine angulations: three angles were measured on the panoramic radiographs: canine angulation to the midline, to the lateral incisor; and to the occlusal plane (Figure 1).
14. The vertical location of the maxillary canine crown was assigned to one of five categories, modified from Power and Short (Figure 1) (21).
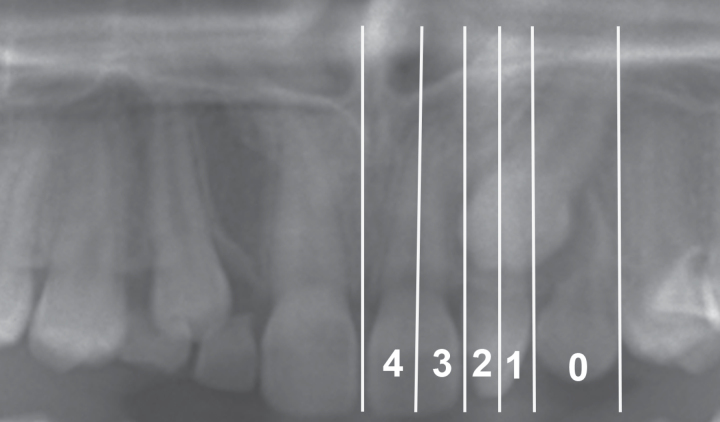
15. The canine overlap with adjacent teeth (sector) was assigned to one of six categories, modified from Ericson and Kurol (Figure 2) (22).
Figure 1.
Panoramic image illustrating the reference lines of the vertical canine location (1) below the level of the cemento-enamel junction of the adjacent lateral incisor, (2) in the cervical third of the adjacent lateral incisor root, (3) in the middle third of the adjacent lateral incisor root, (4) in the apical third of the adjacent lateral incisor root, or (5) above the apical third of the adjacent lateral incisor root as well as the canine angulation measurements (A) to the midline, (B) to the lateral incisor, and (C) to the occlusal plane.
Figure 2.
Panoramic view illustrating reference lines of canine overlap (sectors) assigned to one of five categories: −1= distal to the normal position (in the premolar region), 0 = normal position (primary canine), 1 = distal to the long axis of the lateral incisor, 2 = mesial to the long axis of the lateral incisor, 3 = distal to the long axis of the central incisor, or 4 = mesial to the long axis of the central incisor.
A validation sample was collected to validate the outcome of the present study. The validation sample consisted of 55 canines from 45 patients with maxillary canine impactions (in the period from 1 October 2013 until 18 March 2014)
Statistical methodology
Variables between resorbed and non-resorbed teeth were compared by exact trend, Fisher’s exact and Mann–Whitney U-tests. For each variable, based on its empirical distribution function, the degree of discrimination (resorption versus non-resorption), was quantified with the area under the curve (AUC), known as the concordance index (c-index). This index ranges from 0.5 (random prediction) to 1 (perfect discrimination). The inter- and intra-observer reliability of the measurement was assessed based on the records of 20 patients randomly selected by repeating the linear and angular measurements. Intra-class correlation (ICC) and kappa coefficients were used for continuous and categorical measurements, respectively.
A multivariable prediction model was obtained by a backward selection procedure with 0.157 as the critical level for the P-value, which corresponds to the use of the Aikake information criterion (AIC) for model selection. With AIC, it was required that the increase in model χ2 must be more than twice the degrees of freedom. A bootstrap re-sampling procedure was used to verify if variables retained in the final multivariable model were ‘truly’ independent predictors or were, rather, noise variables (23). In the applied modeling approach, the same data were used to develop and validate the model. Moreover, there was an additional risk of overfitting, originating from the consideration of many predictors compared with the number of resorptions and from the application of an automated model selection procedure (24). The resulting prediction model and its related AUC were therefore overoptimistic, in the sense that future performance in a new study population is overestimated. Therefore, a leave-one-out cross-validation was applied. Further, an optimism-corrected estimate of the performance (AUC) was obtained by a bootstrap re-sampling procedure. Finally, a (uniform) shrinkage factor based on the model χ2 of the final model and the total number of degrees of freedom considered (df = 17) was applied to the estimates from the final model (24). Application of this shrinkage factor will avoid extreme predictions.
The prediction model was constructed on the side level and not on the patient level. As such, P-values obtained in the univariable and multivariable analyses were based on the assumption that both sides were independent. Although this assumption is too simplistic [the ICC equals 0.37; 95% confidence interval (CI): 0.17–0.55; (25) indicating that the probability of having resorption was related between both sides], note that the interest was not in the P-values as such, but in the predictive ability of the model. All analyses were performed with SAS software, version 9.2, of the SAS System for Windows (Copyright© 2002 SAS Institute, Inc. SAS and all other SAS Institute, Inc. product or service names are registered trademarks or trademarks of SAS Institute, Inc., Cary, North Carolina, USA.)
Results
The incidence of RR of adjacent teeth was 33.8%. Table 1 shows the presence, severity, and location of detected RR in adjacent teeth. The intra-observer reliability for most angulations ranged from 0.98 to 0.99 as quantified by the ICC which is excellent. The reliability for the canine angulation to the lateral incisor was 0.99, canine angulation to the midline was 0.99, and canine angulation to the occlusal plan was 0.98. Moreover, the intra-observer reliability of categorical measurements in the prediction model ranged from 0.64 to 1. The intra-observer reliability of anterior apical area was 0.64, canine magnification was 0.92, canine apex was 0.76, type of impaction (horizontal versus vertical) was 1, abnormality was 0.94, vertical canine crown height was 0.94, and for canine overlap of the adjacent teeth was 0.94. The inter-observer reliability for the canine angulations to the lateral incisor, to the midline and to the occlusal plan are equal to 0.99 as quantified by the ICC which is excellent. Moreover, inter-observer reliability for the categorical measurements ranged from 0.8 to 1.
Table 1.
The presence, severity, and location of root resorption in percentages (%).
| Tooth | n | % | ||
|---|---|---|---|---|
| Lateral incisors | Presence of root resorption | No resorption | 282 | 69.46 |
| Resorption | 124 | 30.54 | ||
| Severity | Slight resorption | 64 | 15.76 | |
| Moderate resorption | 26 | 6.40 | ||
| Severe resorption | 34 | 8.37 | ||
| Location | Cervical third | 15 | 3.69 | |
| Middle third | 39 | 9.61 | ||
| Apical third | 70 | 17.24 | ||
| Central incisors | Presence of root resorption | No resorption | 384 | 94.58 |
| Resorption | 22 | 5.42 | ||
| Severity | Slight resorption | 9 | 2.22 | |
| Moderate resorption | 6 | 1.48 | ||
| Severe resorption | 7 | 1.72 | ||
| Location | Cervical third | 2 | 0.49 | |
| Middle third | 4 | 0.99 | ||
| Apical third | 16 | 3.94 | ||
| Premolars | Presence of root resorption | No resorption | 401 | 98.77 |
| Resorption | 5 | 1.23 | ||
| Severity | Slight resorption | 3 | 0.74 | |
| Moderate resorption | 1 | 0.25 | ||
| Severe resorption | 1 | 0.25 | ||
| Location | Cervical third | 0 | 0 | |
| Middle third | 1 | 0.25 | ||
| Apical third | 4 | 0.99 |
Table 2 gives the results of the univariable logistic regression models to predict the presence of resorption. The results from the multivariable model are given in Table 3.
Table 2.
Results from univariable logistic regression models to predict the presence of root resorption.
| Odds ratio (95% CI) | P-value | AUC (95% CI) | |
|---|---|---|---|
| Age (years) | 1.019 (0.983–1.057) | 0.2969 | 0.595 (0.539–0.651) |
| Female versus male | 0.524 (0.338–0.814) | 0.0040 | 0.574 (0.526–0.623) |
| Resorbed root for primary maxillary canine | 1.012 (0.662–1.546) | 0.9578 | 0.501 (0.451–0.551) |
| Crowding in the upper anterior region | 0.598 (0.364–0.983) | 0.0425 | 0.547 (0.504–0.590) |
| Optimal apical area | 0.933 (0.616–1.415) | 0.7449 | 0.508 (0.457–0.560) |
| Sufficient MD space | 1.054 (0.695–1.598) | 0.8057 | 0.506 (0.455–0.557) |
| Canine location | 0.1460 | 0.555 (0.501–0.609) | |
| Buccally | 0.967 (0.710–1.316) | 0.8302 | |
| Line of the arch | 0.787 (0.555–1.117) | 0.1803 | |
| Canine magnification | 2.412 (1.558–3.735) | <0.0001 | 0.604 (0.555–0.653) |
| Open canine apex | 0.302 (0.193–0.471) | <0.0001 | 0.641 (0.593–0.689) |
| Type of impaction (Horizontal versus vertical) | 1.727 (1.041–2.867) | 0.0345 | 0.544 (0.501–0.586) |
| Complete canine development | 2.722 (1.629–4.547) | 0.0001 | 0.593 (0.551–0.636) |
| Detection of abnormality | 1.322 (0.829–2.110) | 0.2413 | 0.527 (0.481–0.572) |
| Canine angulation to the midline | 1.025 (1.014–1.037) | <0.0001 | 0.657 (0.601–0.714) |
| Canine angulation to the occlusal plane | 1.020 (1.009–1.032) | 0.0004 | 0.610 (0.551–0.669) |
| Canine angulation to the lateral incisor | 0.975 (0.964–0.986) | <0.0001 | 0.644 (0.587–0.701) |
| Vertical canine crown position | 0.0025 | 0.595 (0.541–0.649) | |
| Above middle third | 1.693 (1.255–2.284) | 0.0006 | |
| In the middle third | 0.887 (0.665–1.184) | 0.4172 | |
| Canine overlap distal to the lateral incisor or below | 0.365 (0.237–0.564) | <0.0001 | 0.621 (0.572–0.670) |
AUC, area under the curve; CI, confidence interval.
Table 3.
Results from the final multivariable logistic regression model (obtained after applying a backward selection procedure with 0.157 as the critical level for a P-value to remain in the model) and results from the bootstrap resampling procedure.
| Estimate | Odds ratio (95% CI) | P-value | BIF | |
|---|---|---|---|---|
| Age (years) | −0.031 | 0.968 (0.934–1.003) | 0.0748 | 62 |
| Female versus male | −0.499 | 0.599 (0.369–0.973) | 0.0384 | 82 |
| Optimal apical area | −0.384 | 0.690 (0.429–1.108) | 0.1242 | 61 |
| Canine magnification | 0.585 | 1.801 (1.101–2.947) | 0.0192 | 82 |
| Open canine apex | −1.380 | 0.250 (0.151–0.413) | <0.0001 | 100 |
| Type of impaction (Horizontal versus vertical) | −0.532 | 0.605 (0.309–1.186) | 0.1436 | 38 |
| Detection of abnormality | 0.434 | 1.530 (0.899–2.605) | 0.1172 | 53 |
| Canine angulation to the midline | 0.018 | 1.018 (1.000–1.036) | 0.0523 | 50 |
| Vertical canine crown position | 0.0241 | 90 | ||
| Above middle third | 0.837 | 2.282 (1.104–4.715) | 0.0259 | |
| In the middle third | 0.118 | 1.133 (0.605–2.123) | 0.6959 | |
| Intercept | −0.671 |
Estimate, estimates on the logit scale; CI, confidence interval; BIF, bootstrap importance frequency, which indicates the percentage of the specific predictor that retained in the final model (bootstrap). The AUC of the final model equals 0.744 (95% CI: 0.695–0.794).
The prediction formula of the probability of presence of RR is:
where, µ = (−0.031 × age + 0.499 × female − 0.384 × optimal apical area + 0.585 × canine magnification − 1.380 × open canine apex − 0.532 × horizontal + 0.434 × detection of abnormality + 0.018 × canine angulation to the midline + 0.837 × vertical canine crown above middle third + 0.118 × vertical canine crown position − 0.671).
Predictor not present = 0, Predictor present = 1.
To avoid too extreme predictions due to over-fitting, a shrinkage factor should be applied to each of these estimates (by multiplying each estimate with this factor). The shrinkage factor equals 0.85 which is derived from the model χ2 of 113.1 and the 17 degrees of freedom in the initially considered list of predictors.
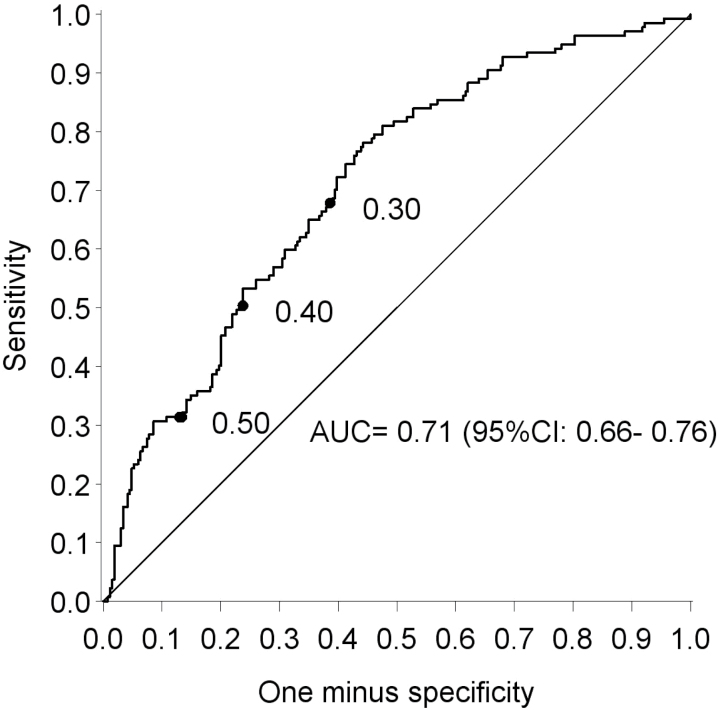
Among the nine variables retained in the final multivariable prediction model (Table 3), four variables (patient gender, canine apex, vertical canine crown position, and canine magnification) are strong independent predictors for RR. The index of discrimination (AUC) of this final model equals 0.75 (0.69–0.79). Application of a leave-one-out cross-validation resulted in an AUC equal to 0.71 (0.66–0.76) (Figure 3). An optimism-corrected estimate of the AUC which also accounted for the model-building approach equals 0.70 (hence, the overoptimism in AUC equals 0.04). The performance on the validation group was comparable with the estimate obtained after cross-validation. The AUC of the prediction model after validation equals 0.687 (CI: 51.4–86.0) with a sensitivity of 50% (CI: 24.7–75.4%) and a specificity of 84.6% (CI: 69.5–94.1%) when 0.50 is used as cutoff.
Figure 3.
The ROC-curve of the final multivariable model. This curve presents the sensitivity and (one minus) specificity of all possible classifications using different cut-offs for the (cross-validated) predicted probability of root resorption. As an illustration, three cut-offs for the probability are labeled.
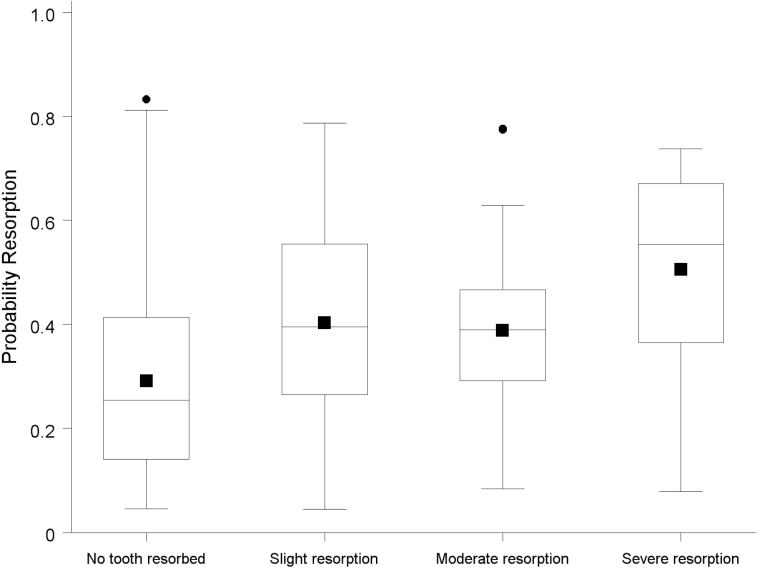
Figure 4 shows the distribution of the (cross-validated) predicted probabilities of RR for patients without RR and for patients with slight, moderate and severe RR. Figure 5 shows the probability of RR for a patient using the final prediction model.
Figure 4.
Boxplots of the cross-validated probabilities for canines without resorption and canines with various degrees of resorption. The AUC quantifying the overlap between root resorption and without resorpion equals 0.673, 0.666, and 0.799 for slight (N = 69), moderate (N = 29), and severe (N = 39) resorption, respectively.
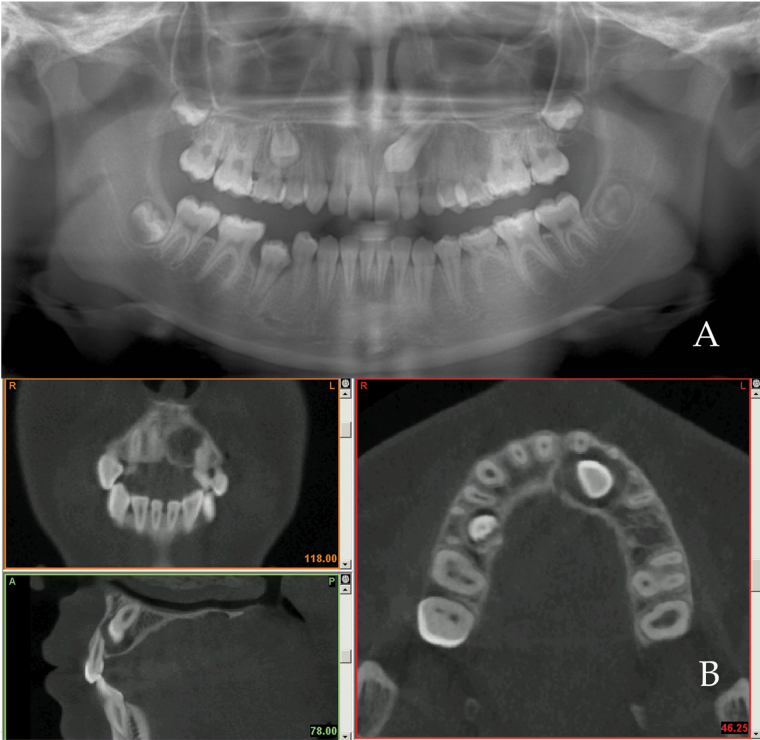
Figure 5.
An example of prediction model of root resorption of 13 years and 6 month-old female patient with unilateral impacted canine illustrating the probability of root resorption as follow: µ = (−0.031×13.5 + 0.499×1 − 0.384×1+ 0.585×1 − 1.380×0 − 0.532×0 + 0.434×1 + 0.018×41 + 0.837×1 + 0.118×0 − 0.671) = 1.6164. Probability of RR = exp (1.6164)/(1+ exp (1.6164))= 83%. (A) Panoramic image. (B) CBCT views (coronal, sagittal, and axial) confirming the presence of root resorption of the adjacent lateral incisor.
Discussion
Panoramic radiographs, although they have diagnostic limitations, are used initially for the evaluation of impacted canines. Therefore, it is useful if the information obtained from panoramic image can be transferred to a CBCT and vice versa. This study tested the variables and factors associated with panoramic radiography, and confirmation of the presence of RR as well as canine localization was performed with CBCT images, since the diagnostic ability of CBCT for these application has been demonstrated with high sensitivity and good specificity compared to that achievable with panoramic images (26). The contact relationship between impacted canine and adjacent teeth was not examined and linear measurements were not performed, due to the limitations of panoramic radiographs. The assessment of crowding and in the anterior apical areas of spacing/overlap of roots and crowns in the anterior region were performed radiographically by using panoramic image. However, the radiographic assessment of crowding is less reliable and can be complemented with clinical examination.
Predisposing factors such as patient age and gender have been extensively studied (13, 27). Conversely, no differences have been found in either the severity or location of RR (28). Our results confirmed that female patients exhibit more RR compared with males, because females experience more canine impaction (13, 27). However, other studies have shown no relation between gender and the presence of RR (17–19) while gender has been found to be a factor in RR only in the central incisor (16).
The use of 3D images has shown no relationship between resorption and enlarged dental follicles of impacted canines, as well as the retention or premature loss of the deciduous canine (12, 13, 29, 30). In a 2D study, the combination of mesially located canines, angulations to the midline exceeding 25 degrees, and completed root development, the risk of RR increased by 50% (15). However, there has been considerable debate regarding the radiographic predisposing factors of RR. Several studies have investigated possible radiographic predictors for RR and have shown significant interaction among several factors, including: canine development, space available for the impacted canine, contact relationship, canine overlap, canine position, vertical location of canine, and linear and angular measurements (12, 13, 15–19). With CBCT, studies have shown that there were correlations between RR and contact relationship, closed canine apex, canine position, mesial overlap with adjacent teeth, and space available for the impacted canine (16–18, 31, 32). In contrast, canine overlap (29, 30, 33), contact relationship (29, 30), canine inclinations (17, 18), and canine position (19) were not found in other studies to be factors involved in lateral incisor RR. In addition to the contradictory results of previous studies, those studies only showed the significant relation between RR and radiographic factors. Furthermore, they failed to verify whether those factors were independent predictors or whether they showed interaction between each other and they failed to validate the proposed predictors.
In this study, two CBCT machines were used, with different parameters. Those CBCT systems were evaluated in a pilot study and have been found not to effect the detection of RR (4). Further, two panoramic machines were used, with different parameters. Those parameters may affect detection of RR. However, several studies suggested that the linear measurement is a reliable method for panoramic radiographs, considering the magnification factors and correct patient position (34–36). In the study linear measurements on the panoramic radiographs were not performed owing to the amount of distortion and magnification (26, 37, 38). However, using different machines with different magnification factor may have an effect in accuracy of angular measurements. In present study the magnification factor was considered if the impacted canine is relatively magnified in comparison to the adjacent teeth or in comparison to the contra-lateral canine.
In the present study, univariable analysis revealed that crowding, complete canine development and canine mesial overlap with adjacent teeth have significant relations with presence of RR (Table 2). However, when considering the multivariable analysis, they were not confirmed as predictors of RR. Therefore, they were not incorporated in the final prediction model. Gender, canine apex, vertical canine crown position, and canine magnification were the strongest predictors for RR in the prediction model (Table 3), because they were significant at the P < 0.05 level in the final model (0.03, 0.0001, 0.02, 0.01, respectively). And more importantly, patient gender, canine apex, vertical canine crown position, and canine magnification were also retained in the final multivariable model in at least 80% of the bootstrap samples, when the same model selection method was used as in the original sample (82%, 100%, 90% and 82%, respectively). This is in accordance with results from another CBCT study showing that, when an impacted canine crown is located apically to adjacent teeth with closed apex, a higher prevalence of RR occurs (19).
The ROC-curve shows the implications on sensitivity and specificity of various choices for the cut-off value of the predicted probability (Figure 3). For instance, when 0.50 was used as a cut-off, the specificity equals 85.1% (95% CI: 80.3–89.2). This implies that 85% of the teeth without resorption will be correctly identified as ‘no resorption’. However, this results in a low sensitivity, that is 34.3% (95% CI: 26.4–42.9%) with 0.50 as cut-off, the positive and negative predictive value (PPV and NPV) equal 54% and 71.8%, respectively. To increase the sensitivity, the cut-off needs to be lowered. For example, if one would decide not to undergo CBCT if the probability of RR is lower than 0.30, the sensitivity increases to 71.5% but at the cost of a decreased specificity (60.1%). Even if the emphasis would be put on maximizing the sensitivity by lowering the cutoff, the false-negative rate would remain non-negligible. For example, with the cut-off put at 0.10, still 13.9% of the ‘non-resorption’ predictions would be false. However, the results in Figure 4 indicate that false-negative predictions are less likely for severe resorption. The discriminative ability of the prediction model was indeed substantially higher when comparing the non-resorbed only with the severely resorbed (AUC = 0.799 instead of AUC = 0.709 for all RR combined). It is of interest to develop a prediction model specifically for the presence of severe RR. To accomplish this with a multivariable model, a larger number of severe RR is needed.
The AUC index of the final model was overoptimistic, since the same data were used to build and validate the model (leave-one-out cross-validation). Therefore, a new validation sample was used to validate the final prediction model. The AUC index of the prediction model after validation of new sample equals 0.68 (CI: 51.4–86.0) with a sensitivity of 50.0% (CI: 24.7–75.4%) and a specificity of 84.6% (CI: 69.5–94.1%) when 0.50 is used as cutoff.
This study was not carried out to emphasize that panoramic radiographs could be used to detect RR. However, the prediction model was generated and tested to help the clinician to estimate the probability of presence of RR based on the available panoramic radiograph in order to justify the use of CBCT. Moreover, using CBCT is justified when conventional radiographs do not provide the required diagnostic information. Several 2D radiographic methods are available for diagnosis and treatment planning for impacted canines and these may be varying between countries, that is panoramic radiographs versus the use of intraoral radiography (periapical and/or occlusal). One has to consider that using different diagnostic techniques may render the prediction model useless because parameters studied may be render different results when i.e. measured on apical radiographies. This study outcome and prediction model may be useful in countries applying a similar referral strategy but not to deviating orthodontic referral protocols including intraoral radiographs. Furthermore one has to consider as well that the present study was a retrospective study which introduces a potential weakness when applying the findings in clinic. Therefore, the need for CBCT diagnosis of RR due to maxillary canine impaction can be judged by using the prediction model together with clinical parameters, and specific treatment plan options such as extraction in patients who show lack of space, extraction of severely resorbed lateral incisor may be better than removing intact premolars.
Conclusions
Prediction of RR based on panoramic radiographs is difficult. The final prediction model for RR based on available panoramic radiographs may help justifying the need of additional CBCT examination.
References
- 1. Alqerban A. Jacobs R. Lambrechts P. Loozen G. and Willems G (2009) Root resorption of the maxillary lateral incisor caused by impacted canine: a literature review. Clinical Oral Investigations, 13, 247–255. [DOI] [PubMed] [Google Scholar]
- 2. Tronstad L. (1988) Root resorption—etiology, terminology and clinical manifestations. Endodontics Dental Traumatology, 4, 241–252. [DOI] [PubMed] [Google Scholar]
- 3. Mason C. Papadakou P. and Roberts G.J (2001) The radiographic localization of impacted maxillary canines: a comparison of methods. European Journal of Orthodontics, 23, 25–34. [DOI] [PubMed] [Google Scholar]
- 4. Alqerban A. Jacobs R. Fieuws S. Nackaerts O. and Willems G (2011) Comparison of 6 cone-beam computed tomography systems for image quality and detection of simulated canine impaction-induced external root resorption in maxillary lateral incisors. American Journal of Orthodontics and Dentofacial Orthopedics, 140, e129–e139. [DOI] [PubMed] [Google Scholar]
- 5. Hujoel P. Hollender L. Bollen A.M. Young J.D. McGee M. and Grosso A (2006) Radiographs associated with one episode of orthodontic therapy. Journal of Dental Education, 70, 1061–1065. [PubMed] [Google Scholar]
- 6. European Commission. (2012) Radiation Protection N°172. Cone Beam CT for Dental and Maxillofacial Radiology: Evidence Based Guideline http://ec.europa.eu/energy/en/content/172 (March 2012, date last accessed).
- 7. Alqerban A., Hedesiu M., Baciut M., Nackaerts O., Jacobs R., Fieuws S; SedentexCT Consortium and Willems G. (2013) Pre-surgical treatment planning of maxillary canine impactions using panoramic vs cone beam CT imaging. Dentomaxillofacial Radiology, 42, 20130157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alqerban A. Willems G. Bernaerts C. Vangastel J. Politis C. and Jacobs R (2014) Orthodontic treatment planning for impacted maxillary canines using conventional records versus 3D CBCT. European Journal of Orthodontics. First published on January 9, 2014, 10.1093/ejo/cjt100. [DOI] [PubMed] [Google Scholar]
- 9. Haney E. Gansky S.A. Lee J.S. Johnson E. Maki K. Miller A.J. and Huang J.C (2010) Comparative analysis of traditional radiographs and cone-beam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. American Journal of Orthodontics and Dentofacial Orthopedics, 137, 590–597. [DOI] [PubMed] [Google Scholar]
- 10. Botticelli S. Verna C. Cattaneo P.M. Heidmann J. and Melsen B (2011) Two- versus three-dimensional imaging in subjects with unerupted maxillary canines. European Journal of Orthodontics, 33, 344–349. [DOI] [PubMed] [Google Scholar]
- 11. Wriedt S. Jaklin J. Al-Nawas B. and Wehrbein H (2012) Impacted upper canines: examination and treatment proposal based on 3D versus 2D diagnosis. Journal of Orofacial Orthopedics, 73, 28–40. [DOI] [PubMed] [Google Scholar]
- 12. Ericson S. Bjerklin K. and Falahat B (2002) Does the canine dental follicle cause resorption of permanent incisor roots? A computed tomographic study of erupting maxillary canines. Angle Orthodontist, 72, 95–104. [DOI] [PubMed] [Google Scholar]
- 13. Rimes R.J. Mitchell C.N. and Willmot D.R (1997) Maxillary incisor root resorption in relation to the ectopic canine: a review of 26 patients. European Journal of Orthodontics, 19, 79–84. [DOI] [PubMed] [Google Scholar]
- 14. Ericson S. and Kurol P.J (2000) Resorption of incisors after ectopic eruption of maxillary canines: a CT study. Angle Orthodontist, 70, 415–423. [DOI] [PubMed] [Google Scholar]
- 15. Ericson S. and Kurol J (1988) Resorption of maxillary lateral incisors caused by ectopic eruption of the canines. A clinical and radiographic analysis of predisposing factors. American Journal of Orthodontics and Dentofacial Orthopedics, 94, 503–513. [DOI] [PubMed] [Google Scholar]
- 16. Yan B. Sun Z. Fields H. and Wang L (2012) Maxillary canine impaction increases root resorption risk of adjacent teeth: a problem of physical proximity. American Journal of Orthodontics and Dentofacial Orthopedics, 142, 750–757. [DOI] [PubMed] [Google Scholar]
- 17. Kim Y. Hyun H.K. and Jang K.T (2012) The position of maxillary canine impactions and the influenced factors to adjacent root resorption in the Korean population. European Journal of Orthodontics, 34, 302–306. [DOI] [PubMed] [Google Scholar]
- 18. Cernochova P. Krupa P. and Izakovicova-Holla L (2011) Root resorption associated with ectopically erupting maxillary permanent canines: a computed tomography study. European Journal of Orthodontics, 33, 483–491. [DOI] [PubMed] [Google Scholar]
- 19. Lai C.S. Bornstein M.M. Mock L. Heuberger B.M. Dietrich T. and Katsaros C (2012) Impacted maxillary canines and root resorptions of neighbouring teeth: a radiographic analysis using cone-beam computed tomography. European Journal of Orthodontics, 35, 529–538. [DOI] [PubMed] [Google Scholar]
- 20. Ericson S. and Kurol J (2000) Incisor root resorptions due to ectopic maxillary canines imaged by computerized tomography: a comparative study in extracted teeth. Angle Orthodontist, 70, 276–283. [DOI] [PubMed] [Google Scholar]
- 21. Power S.M. and Short M.B (1993) An investigation into the response of palatally displaced canines to the removal of deciduous canines and an assessment of factors contributing to favourable eruption. British Journal of Orthodontics, 20, 215–223. [DOI] [PubMed] [Google Scholar]
- 22. Ericson S. and Kurol J (1988) Early treatment of palatally erupting maxillary canines by extraction of the primary canines. European Journal of Orthodontics, 10, 283–295. [DOI] [PubMed] [Google Scholar]
- 23. Austin P.C. and Tu J.V (2004) Bootstrap methods for developing predictive models. The American Statistician, 58, 131–137. [Google Scholar]
- 24. Steyerberg E. (2009) Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating. Springer-Verlag, New York. [Google Scholar]
- 25. Zou G. and Donner A (2004) Confidence interval estimation of the intraclass correlation coefficient for binary outcome data. Biometrics, 60, 807–811. [DOI] [PubMed] [Google Scholar]
- 26. Alqerban A. Jacobs R. Fieuws S. and Willems G (2011) Comparison of two cone beam computed tomographic systems versus panoramic imaging for localization of impacted maxillary canines and detection of root resorption. European Journal of Orthodontics, 33, 93–102. [DOI] [PubMed] [Google Scholar]
- 27. Ericson S. and Kurol J (1986) Radiographic assessment of maxillary canine eruption in children with clinical signs of eruption disturbance. European Journal of Orthodontics, 8, 133–140. [DOI] [PubMed] [Google Scholar]
- 28. Ericson S. and Kurol J (1987) Radiographic examination of ectopically erupting maxillary canines. American Journal of Orthodontics and Dentofacial Orthopedics, 91, 483–492. [DOI] [PubMed] [Google Scholar]
- 29. Schmuth G.P. Freisfeld M. Koster O. and Schuller H (1992) The application of computerized tomography (CT) in cases of impacted maxillary canines. European Journal of Orthodontics, 14, 296–301. [DOI] [PubMed] [Google Scholar]
- 30. Preda L. La F.A. Di Maggio E.M. Dore R. Schifino M.R. Campani R. Segù C. and Sfondrini M.F (1997) The use of spiral computed tomography in the localization of impacted maxillary canines. Dentomaxillofacial Radiology, 26, 236–241. [DOI] [PubMed] [Google Scholar]
- 31. Jung Y.H. Liang H. Benson B.W. Flint D.J. and Cho B.H (2012) The assessment of impacted maxillary canine position with panoramic radiography and cone beam CT. Dentomaxillofacial Radiology, 41, 356–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schindel R.H. and Sheinis M.R (2013) Prediction of maxillary lateral-incisor root resorption using sector analysis of potentially impacted canines. Journal of Clinical Orthodontics, 47, 490–493. [PubMed] [Google Scholar]
- 33. Amlani M.S. Inocencio F. and Hatibovic-Kofman S (2007) Lateral incisor root resorption and active orthodontic treatment in the early mixed dentition. European Journal of Paediatric Dentistry, 8, 188–192. [PubMed] [Google Scholar]
- 34. Laster W.S. Ludlow J.B. Bailey L.J. and Hershey H.G (2005) Accuracy of measurements of mandibular anatomy and prediction of asymmetry in panoramic radiographic images. Dentomaxillofacial Radiology, 34, 343–349. [DOI] [PubMed] [Google Scholar]
- 35. Stramotas S. Geenty J.P. Petocz P. and Darendeliler M.A (2002) Accuracy of linear and angular measurements on panoramic radiographs taken at various positions in vitro. European Journal of Orthodontics, 24, 43–52. [DOI] [PubMed] [Google Scholar]
- 36. Volchansky A. Cleaton-Jones P. Drummond S. and Bonecker M (2006) Technique for linear measurement on panoramic and periapical radiographs: a pilot study. Quintessence International, 37, 191–197. [PubMed] [Google Scholar]
- 37. Schubert M. and Baumert U (2009) Alignment of impacted maxillary canines: critical analysis of eruption path and treatment time. Journal of Orofacial Orthopedics, 70, 200–212. [DOI] [PubMed] [Google Scholar]
- 38. Fleming P.S. Scott P. Heidari N. and Dibiase A.T (2009) Influence of radiographic position of ectopic canines on the duration of orthodontic treatment. Angle Orthodontist, 79, 442–446. [DOI] [PubMed] [Google Scholar]