Summary
Background:
The extensive literature concerning the early treatment of anterior open bite (AOB) is still controversial and covers a wide variety of therapeutic approaches.
Objectives:
The objective of this study was to provide a comprehensive review evaluating the effectiveness of the orthodontic correction of AOB in growing individuals.
Search methods:
Search was conducted on PubMed, Embase, Cochrane Library, Web of Science, Scopus, Google Scholar, Scielo, and Lilacs databases. Trials registries were consulted for ongoing trials, and grey literature was also contemplated.
Selection criteria:
Selection process was performed to include controlled trials enrolling growing subjects who underwent orthodontic treatment to correct AOB and/or hyperdivergent facial pattern.
Data collection and analysis:
Data were grouped and analysed descriptively. Qualitative appraisal was performed according to the Cochrane risk of bias tool, for randomized clinical trials (RCTs), and MINORS tool for non-RCTs.
Results:
The 22 studies included in this review mostly considered mixed dentition subjects, and there was a considerable variation regarding therapeutic approaches. Because of poor-quality and/or insufficient evidence, consistent results were not found. However, some useful clinical inferences and suggestions for future studies were provided for each therapeutic modality considered here.
Conclusions:
Additional efforts must still be directed to perform, whenever possible, RCTs; or to conduct prospective controlled trials with adequate sample sizes, consecutively assembled subjects, with the comparison of contemporary and equivalent groups.
Introduction
Anterior open bite (AOB) has been reported to be relatively common during both primary (1) and mixed dentitions (1, 2). This occlusal anomaly has been commonly associated with prolonged sucking habits and hyperdivergent facial characteristics (2).
In younger children, the presence of AOB is mostly associated with oral habits (3) and it might negatively impact quality of life (4). It has been demonstrated that if AOB persist throughout craniofacial pubertal growth spurt, it hardly ever self-corrects (5). On the other hand, in cases with significant vertical skeletal imbalance, an underlying craniofacial pattern seems to be present early before the growth spurt (6), and it tends to either persist (7) or accentuate thereafter (6).
Although extensive literature has been published addressing the effectiveness of early orthodontic treatment of AOB (8, 9), a previous systematic review (8), performed a decade ago, was not able to support any evidence-based conclusions, due to serious methodological issues encountered in the selected studies. However, over the last 10 years, better-designed clinical trials have been published (10–25).
Another systematic review was recently issued (9), and concluded that the evidence is still poor, and not strong enough to support meaningful clinical recommendations. However, this review (9) applied strict inclusion criteria, that is restriction to randomized clinical trials (RCTs), which resulted in the inclusion of only few studies. Non-randomized controlled trials (nRCTs), although not capable of minimizing selection bias, might still be clinically useful (26).
Therefore, the objective of this systematic review was to provide a comprehensive and updated synthesis evaluating the effectiveness of the correction of dental or skeletal open bite of growing individuals. A secondary objective was to identify deficient methodological points in the collected literature, and then suggest directions for future studies to be performed.
Material and methods
Protocol and registration
The Preferred Reporting Item for Systematic Review and Meta-Analysis (PRISMA) (27) checklist was used as a guideline for conducting and reporting this review. This review was registered on the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42014014389).
Eligibility criteria
Inclusion criteria
Primary study objective to assess the effectiveness of any interceptive orthodontic therapy (including orthopedic and oral habit appliances) for the treatment of AOB (negative overbite between upper and lower incisors) or hyperdivergent skeletal pattern (at least one altered vertical cephalometric skeletal parameter).
RCT or nRCT, if the control group (treated or non-treated) was matched to the experimental group according to occlusal (overbite) or skeletal status (at least one vertical cephalometric skeletal parameter).
Enrollment of the sample, as a whole, or any subgroup of it with mean age below 18 years.
Report of changes in overbite or at least one vertical cephalometric skeletal parameter from baseline to post-treatment.
Exclusion criteria
-
Orthodontic treatment performed on any group involved one of the following therapeutic approaches:
use of orthodontic brackets appliances, either with full or partial setups;
orthognathic maxillofacial surgery; or
distraction osteogenesis.
Enrollment of patients with:
lateral open-bites only; or
cleft lip and/or palate, syndromes, or craniofacial malformations.
Duplicate results.
There were no restrictions regarding language, date of publication, or sample size.
Information sources
PubMed, Embase, Cochrane Library, Web of Science, Scopus, Google Scholar, Scielo, Lilacs, ProQuest Dissertations, and Theses Global were searched until March 2015. Furthermore, ClinicalTrials.gov, the European Union Clinical Trials Register, and the Australian New Zealand Clinical Trials Registry were consulted for ongoing trials. A hand search of the reference lists of the selected articles was also conducted.
Search
The terms used for the electronic search were ‘open bite’, ‘open-bite’, ‘hyperdivergen*’, ‘dolichofac*’, ‘management’, ‘treatment’, ‘therapy’, ‘effective*’, ‘correction’, ‘change*’, ‘relapse’, and ‘stability’.
A search strategy was originally designed for PubMed, and subsequently adapted to the remaining databases (Supplementary Appendix 1).
Study selection
During the first selection phase, two authors (MFNF, NMI) independently screened studies that apparently aimed at assessing the effectiveness of interceptive orthodontic therapy for the treatment of AOB or hyperdivergent skeletal pattern.
During the second selection phase, the same reviewers independently evaluated full-texts, and those studies which did not meet all eligibility criteria were excluded. In case of disagreement, consensus was reached after discussion.
Data collection process and data items
Data collection was performed by two reviewers (MFNF, LGA), and all of the authors reviewed the data collection thereafter. Sample characteristics, outcomes, and results were extracted, according to standardized tables.
Risk of bias in individual studies
Randomized clinical trials were assessed according to the Cochrane Collaboration’s tool for assessing risk of bias (28) (Supplementary Appendix 2). For the evaluation of the last item of this tool, the authors considered the following features as sources of bias:
absence of sample size calculation;
significantly different outcome measures at baseline;
inclusion and exclusion criteria incompatible to the study objectives;
inappropriate statistical analysis;
absence of standard-deviation and confidence interval; and
observation period incompatible to the study objectives.
nRCTs were evaluated according to the methodological index for nRCTs (MINORS) (29) (Supplementary Appendix 3).
Summary measures
Overbite or any vertical skeletal parameter concerning mandibular and palatal plane inclinations was considered as outcomes of interest.
Synthesis of results
The results of this manuscript are descriptively presented, since it was not considered adequate to synthesize the data through meta-analyses, as a result of excessive heterogeneity.
Results
Study selection
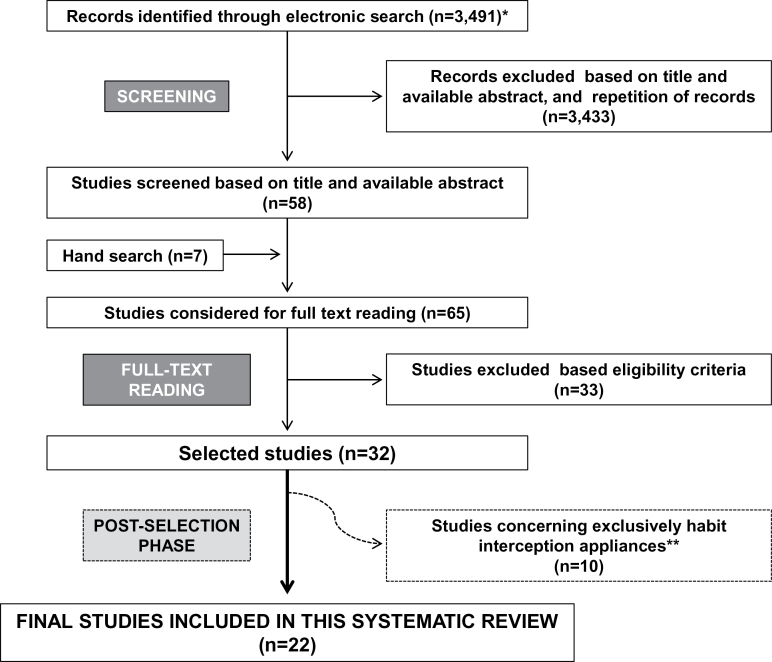
After electronic searching, inclusion of hand-searched studies, and screening phase, 65 studies were pre-selected for full reading. From these, 33 studies were excluded (Supplementary Appendix 4), while 32 studies met the eligibility criteria (10–25, 30–45) (Figure 1).
Figure 1.
Flowchart of the study selection process. *Including repetitions. **Considered in the second part of the systematic review.
Additional 10 studies (10, 13, 17–20, 22, 23, 39, 44), which only considered habit interception appliances, were not considered in this report, but will be analysed in a different publication. Hence, 22 studies (11, 12, 14–16, 21, 25, 26, 30–38, 40–43, 45) will be considered here.
Study characteristics
Sample mean ages ranged from 7.0 to 12.6 years, and the patients’ occlusal features varied according to the inclusion criteria applied in each study (Supplementary Appendix 5). Time span between examinations varied frequently. Most of the time, it covered the active phase of the treatment (11, 21, 24, 25, 31–37, 38, 40–43); whereas in other instances, the observation period extended through retention phase (12, 14, 16), until comprehensive orthodontic treatment (15, 45), or even afterwards (30).
The studies covered a large variety of orthodontic therapies and appliances:
Fränkel regulator-4 (FR-4): with (33, 38) or without lip seal exercises (30);
Open bite bionator (OBB): only (12, 14) or associated with high-pull headgear (15, 37);
Posterior bite-blocks (PBB): passive splints of diverse thicknesses (31, 34, 40), associated with vertical-pull chin cup (VPCC) (34); magnetic (21, 25, 31, 32, 35, 41) or spring-activated appliances (21, 25, 34, 35);
Maxillary expansion appliances (MEA): slow (42) or rapid (16, 45) associated with VPCC (16, 42, 45);
Rapid maxillary intruder (RMI): combined with conventional (transpalatal and lingual arches) (11) or alternative anchorage systems (maxillary posterior splint) (25);
Class II headgear appliances: high-pull activator (36) and modified Thurow appliance (24); and
VPCC: as an exclusive approach (43).
Risk of bias within studies
From the included studies, there were three RCTs (Table 1). There were no reports regarding allocation sequence generation or concealment (21, 31, 38). Blinding was not described in two studies (21, 38). No apparent sample loss was identified in two studies (31, 38), but all of them were unclear while reporting outcomes (21, 31, 38). Furthermore, all selected RCTs presented other sources of bias, mostly related to the absence of sample size calculation (21, 31, 38) and lack of baseline comparison (21, 38).
Table 1.
Methodological appraisal of RCTs.
| Criteria | ||||||
|---|---|---|---|---|---|---|
| Studies | Sequence generation | Allocation concealment | Blinding | Incomplete outcome data addressed | Outcome reporting | Free of other bias |
| Erbay et al. (38) | Unclear | Unclear | Unclear | Yes | Unclear | No |
| Doshi and Bhad-Patil (21) | Unclear | Unclear | Unclear | Unclear | Unclear | No |
| Kiliaridis et al. (31) | Unclear | Unclear | Yes | Yes | Unclear | No |
RCT, randomized clinical trial.
As for the quality appraisal of nRCTs (Table 2), all of them were adequate in relation to the suitability of the endpoint outcome measure, and the follow-up period length. With the exception of two (34, 35), the studies demonstrated sample size consistency through time points, with no sample loss.
Table 2.
Methodological appraisal of nRCTs.
| Criteria | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Studies | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Total |
| Clear aim | Inclusion of consecutive patients | Prospective data collection | Endpoints appropriate to the aim | Unbiased assessment of the endpoint | Follow-up period appropriate | Follow-up loss less than 5% | Prospective calculation of the study size | Adequate control group | Contemporary groups | Baseline equivalence of groups | Adequate statistical analyses | ||
| Fränkel and Fränkel (30) | 1 | 0 | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 0 | 0 | 1 | 10 |
| Haydar and Enacar (33) | 2 | 0 | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 14 |
| Cozza et al. (12) | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 20 |
| Defraia et al. (14) | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 16 |
| Weinbach and Smith (37) | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 16 |
| Freeman et al. (15) | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 18 |
| Barbre and Sinclair (32) | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 1 | 1 | 2 | 15 |
| Kuster and Ingervall (35) | 2 | 1 | 0 | 2 | 0 | 2 | 0 | 0 | 2 | 2 | 1 | 1 | 13 |
| Işcan et al. (34) | 2 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 2 | 0 | 0 | 2 | 10 |
| Işcan and Sarisoy (40) | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 17 |
| Bazzucchi et al. (41) | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 1 | 1 | 2 | 15 |
| Albogha et al. (25) | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 21 |
| Sankey et al. (42) | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 17 |
| Baccetti et al. (16) | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 20 |
| Schulz et al. (45) | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 18 |
| Cinsar et al. (11) | 2 | 0 | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 14 |
| Jacob et al. (24) | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 16 |
| Ngan et al. (36) | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 16 |
| Işcan et al. (43) | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 16 |
nRCT, non-randomized clinical trial.
All of the studies, with one exception (30) clearly stated their objectives. Incomplete statistical analyses report was identified in two studies (30, 35).
All of the included nRCTs had adequate controls. However, even though most of them had equivalent groups (11, 12, 14–16, 24, 25, 33, 36, 40, 42, 43, 45), some of the studies groups (32, 35, 41) were not equivalent at baseline for some key variables. Only few studies utilized contemporary groups for comparison (25, 35, 37, 40), while most of them relied on historical records of untreated control subjects (12, 14–16, 24, 32, 36, 41–43, 45).
Generally, the selected nRCTs scored poorly in relation to blinded assessment, with only one exception (16). None of the studies reported prospective calculation of the sample size, even though some of them demonstrated that their sample had adequate statistical power (12, 15, 16, 25, 45).
Finally, only two studies prospectively collected information derived from consecutive patients (12, 25), while most of them retrospectively collected at least part of their data (14–16, 24, 32, 36, 37, 40–43, 45).
Results of individual studies
A detailed report of the overbite and skeletal effects of each therapeutic modality can be found at Tables 3, 4, 5, 6, 7, 8, and 9.
Table 3.
Summary of studies characteristics and results of the included studies assessing FR-4.
| Reference | Sample | Outcomesa | Results | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline G1 | ΔG1b | Baseline G2 | ΔG2b | ΔG1 − ΔG2 | P-valuec | ||||
| Group 1 | Group 2 | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Fränkel and Fränkel (30) | FR-4 | Untreated | SN.MP (°) | NA | −5.4 (–) | NA | 2.3 (-) | −7.7 | P < 0.01 |
| n = 30 | n = 11 | SN.PP (°) | 2.3 (–) | −0.3 (-) | 2.6 | P < 0.001 | |||
| — | — | PP.MP (°) | −7.4 (–) | 2.6 (-) | −10.1 | P < 0.001 | |||
| 7.0 yrs | 8.0 yyrs | ||||||||
| OP: 96 months | |||||||||
| Erbay et al. (38) | FR-4+ lip seal training | Untreated | Overbite (mm) | −3.9 (1.3) | 5.0 (1.3) | −3.5 (1.4) | 1.4 (1.8) | 3.6 | P < 0.001 |
| n = 20 | n = 20 | SN.GoMe (°) | 43.3 (4.0) | −2.8 (1.1) | 43.8 (3.2) | 0.7 (1.9) | −3.5 | P < 0.001 | |
| 13♀/7♂ | 13♀/7♂ | SN.PP (°) | 7.8 (2.8) | 1.4 (1.3) | 9.0 (3.1) | 0.0 (2.4) | 1.4 | P < 0.05 | |
| 8.7±0.5 yrs | 8.9±1.2 yrs | PP.MP (°) | 35.5 (4.8) | −4.6 (2.6) | 34.7 (3.4) | 0.8 (1.5) | −5.4 | P < 0.001 | |
| OP: 24 months | |||||||||
| Haydar and Enacar (33) | FR-4+ lip seal training | Untreated | Overbite (mm) | −2.6 (1.6) | 2.6 (0.7) | −3.8 (1.3) | 1.1 (1.1) | 1.5 | P < 0.01 |
| n = 11 | n = 10 | FMA (°) | 31.6 (5.7) | 1.0 (1.7) | 32.1 (3.2) | −0.7 (1.2) | 1.7 | P < 0.05 | |
| — | — | BaN.PtGn (°) | 79.0 (4.1) | 0.7 (1.3) | 80.9 (3.1) | 0.6 (1.7) | 0.1 | NS | |
| 8.7±1.1 yrs | 8.2±1.0 yrs | SN.PP (°) | 10.0 (3.2) | −0.5 (0.8) | 8.9 (4.6) | −0.5 (1.1) | 0.0 | NS | |
| OP: 14 months | OP: 12 months | PP.MP (°) | 34.0 (4.7) | 0.7 (1.1) | 32.6 (4.1) | −0.2 (1.1) | 0.9 | NS | |
SD, standard-deviation; ♀, female; ♂, male; yrs, years; G1, group 1; G2, group 2; NS, non-significant; OP, observation period; NA, not available; FR-4, Fränkel regulator-4; ΔG1, difference between final and baseline measurements for group 1; ΔG2, difference between final and baseline measurements for group 2; ΔG1 − ΔG2, difference between changes observed for groups 1 and 2.
aPre-treatment statistically significant (P < 0.05) differences on bold font, and absence of pre-treatment comparison on italic font.
bStatistically significant (P < 0.05) changes on bold font, and absence of intra-group comparison on italic font
cConcerning ΔG1 − ΔG2.
Table 4.
Summary of studies characteristics and results of the included studies assessing OBB.
| Reference | Sample | Outcomesa | Results | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline G1 | ΔG1b | Baseline G2 | ΔG2b | ΔG1 − ΔG2 | P-valuec | ||||
| Group 1 | Group 2 | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Defraia et al. (14) | OBB | Untreated | Overbite (mm) | NA | 2.7 (2.6) | NA | 1.2 (2.0) | 1.5 | P < 0.05 |
| n = 24 | n = 23 | MPA (°) | −1.1 (3.2) | −0.3 (1.4) | −0.8 | NS | |||
| 13♀/11♂ | 10♀/13♂ | FH.PP (°) | 0.2 (2.7) | −1.0 (1.7) | 1.2 | NS | |||
| 9.2 yrs | 9.1 yrs | PP.MP (°) | −1.2 (1.8) | 0.7 (2.7) | −1.9 | P < 0.05 | |||
| OP: 33 months | |||||||||
| Cozza et al. (12) | OBB | QH-Crib | Overbite (mm)1 | NA | 2.7 (2.6) | NA | 4.6 (2.1) | −1.9 | P < 0.05 |
| n = 20 | n = 21 | MPA (°) | −1.1 (3.2) | −0.9 (1.9) | −0.2 | NS | |||
| 9♀/11♂ | 15♀/6♂ | FH.PP (°) | 0.2 (2.7) | 1.1 (2.2) | −0.9 | NS | |||
| 8.3±0.8 yrs | 8.4±1.2 yrs | PP.MP (°) | −1.2 (1.8) | −2.0 (2.4) | 0.8 | NS | |||
| OP: 30 months | OP: 31 months | ||||||||
| Freeman et al. (15) | OBB + HPH | Untreated | Overbite (mm) | 1.3 (3.2) | 1.0 (2.7) | 0.9 (3.2) | 1.2 (2.0) | −0.2 | NS |
| n = 24 | n = 23 | MPA (°) | 30.1 (4.5) | 0.3 (1.5) | 29.4 (3.0) | −0.3 (1.4) | 0.6 | NS | |
| 13♀/11♂ | 13♀/10♂ | FH.PP (°) | 1.9 (3.4) | −1.9 (2.1) | 1.5 (2.6) | −1.0 (1.7) | −0.9 | NS | |
| 8.7±1.1 yrs | 8.2±1.0 yrs | ||||||||
| OP: 40 months | OP: 33 months | ||||||||
| Weinbach and Smith (37) | OBB + HPH | OBB | Overbite (mm) | NA | 2.0 (2.6) | NA | 1.0 (2.5) | 1.0 | NS |
| n = 13 | n = 26 | SN.PP (°) | 0.4 (1.9) | 0.2 (2.1) | 0.2 | NS | |||
| 12♀/27♂ | SN.MP (°) | −0.8 (2.1) | −0.5 (2.0) | −0.3 | NS | ||||
| 10 (7.0–12.9) yrs | NSGn (°) | −0.5 (1.4) | −0.2 (1.4) | −0.3 | NS | ||||
| OP: 20 months | |||||||||
SD, standard-deviation; ♀, female; ♂, male; yrs, years; G1, group 1; G2, group 2; NS, non-significant; OP, observation period; NA, not available; HPH, high-pull headgear; QH-Crib, quad-helix associated with crib; OBB, open bite bionator; ΔG1, difference between final and baseline measurements for group 1; ΔG2, difference between final and baseline measurements for group 2; ΔG1 − ΔG2, difference between changes observed for groups 1 and 2.
aPre-treatment statistically significant (P < 0.05) differences on bold font, and absence of pre-treatment comparison on italic font.
bStatistically significant (P < 0.05) changes on bold font, and absence of intra-group comparison on italic font.
cConcerning ΔG1 − ΔG2.
Table 5.
Summary of studies characteristics and results of the included studies assessing PBB.
| Reference | Sample | Outcomesa | Results | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline G1 | ΔG1b | Baseline G2 | ΔG2b | ΔG1 − ΔG2 | P-valuec | ||||
| Group 1 | Group 2 | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Işcan and Sarisoy (40) | Passive PBB 5 mm | Passive PBB 10 mm | |||||||
| n = 13 | n = 12 | Overbite (mm) | −2.3 (1.1) | 2.7 (1.2) | −2.6 (1.6) | 2.5 (1.0) | 0.2 | NS | |
| 9♀/4♂ | 9♀/3♂ | SN.GoGn (°) | 41.5 (3.7) | −0.7 (1.1) | 42.7 (3.3) | −1.2 (1.2) | 0.5 | NS | |
| 10.4±1.2 yrs | 10.9±1.8 yrs | SN.PP (°) | 7.5 (2.6) | −0.3 (1.1) | 8.7 (2.6) | −0.1 (0.8) | −0.2 | NS | |
| OP: 4–10 months | OP: 4–13 months | ||||||||
| Işcan and Sarisoy (40) | Passive PBB 5 mm | Untreated | Overbite (mm) | −2.3 (1.1) | 2.7 (1.2) | −1.6 (0.9) | 0.2 (0.5) | 2.5 | P < 0.01 |
| n = 13 | n = 14 | SN.GoGn (°) | 41.5 (3.7) | −0.7 (1.1) | 41.4 (4.0) | 0.0 (0.9) | −0.7 | NS | |
| 9♀/4♂ | 11♀/3♂ | SN.PP 2 (°) | 7.5 (2.6) | −0.3 (1.1) | 10.3 (2.9) | 0.0 (1.7) | −0.3 | NS | |
| 10.4±1.2 yrs | 10.6±1.4 yrs | ||||||||
| OP: 4–10 months | OP: 7–9 months | ||||||||
| Işcan and Sarisoy (40) | Passive PBB 10 mm | Untreated | Overbite (mm) | −2.6 (1.6) | 2.5 (1.0) | −1.6 (0.9) | 0.2 (0.5) | 2.3 | P < 0.01 |
| n = 12 | n = 14 | SN.GoGn (°) | 42.7 (3.3) | −1.2 (1.2) | 41.4 (4.0) | 0.0 (0.9) | −1.2 | P < 0.05 | |
| 9♀/3♂ | 11♀/3♂ | SN.PP 2 (°) | 8.7 (2.6) | −0.1 (0.8) | 10.3 (2.9) | 0.0 (1.7) | −0.1 | NS | |
| 10.9±1.8 yrs | 10.6±1.4 yrs | ||||||||
| OP: 4–13 months | OP: 7–9 months | ||||||||
| Bazzucchi et al. (41) | Magnetic PBB | Untreated | Overbite 2 (mm) | −2.2 (1.6) | 2.4 (1.8) | 3.4 (2.7) | 0.9 (1.8) | 1.5 | NS |
| n = 29 | n = 29 | MPA (°) | 37.1 (5.1) | 0.8 (1.3) | 34 (4.3) | −0.2 (1.0) | 1.0 | NS | |
| 23♀/6♂ | 23♀/6♂ | ||||||||
| 11.0±3.0 yrs | 11.0±3.0 yrs | ||||||||
| OP: 8 months | OP: 9 months | ||||||||
| Barbre and Sinclair (32) | Magnetic PBB | Untreated | Overbite (mm) | −3.0 (1.6) | −3.2 (1.4) | NA | NA | NA | NA |
| n = 25 | n = 25 | MPA (°) | 29.8 (4.8) | −1.0 (2.0) | 28.6 (0.9) | −0.6 (0.8) | −0.4 | NS | |
| 10.6 | Matched | SN.MP 1 (°) | 38.4 (5.6) | −1.0 (1.4) | 34.4 (0.6) | −0.2 (0.3) | −0.8 | P < 0.05 | |
| (8.2–13.4) yrs | − | SN.PP 2 (°) | 3.5 (2.7) | −0.1 (1.3) | 7.4 (0.6) | 0.2 (0.3) | −0.3 | NS | |
| OP: 7 months | |||||||||
| Kiliaridis et al. (31) | Magnetic PBB | Passive PBB 5 mm | Overbite (mm) | −1.9 (0.8) | 2.4 (1.3) | −3.4 (1.9) | 2.2 (0.7) | 0.2 | NS |
| n = 10 | n = 10 | SN.MP (°) | 39.7 (3.7) | −0.8 (0.5) | 40.3 (5.1) | −1.0 (0.7) | 0.2 | NS | |
| 7♀/3♂ | 7♀/3♂ | PP.MP (°) | 32.7 (4.4) | −1.1 (0.8) | 33.6 (4.2) | −1.3 (1.0) | 0.2 | NS | |
| 12.6±2.6 yrs | 11.9±2.7 yrs | ||||||||
| OP: 5 months | OP: 6 months | ||||||||
| Işcan et al. (34) | Spring PBB | Passive (3–4) mm PBB + VPCC | Overbite (mm) | −2.9 (1.3) | 3.5 (0.4) | −2.9 (1.9) | 4.5 (0.6) | 1.0 | NS |
| n = 11 | n = 12 | SN.GoGn (°) | 41.3 (3.9) | −1.6 (0.4) | 42.3 (3.8) | −2.0 (0.4) | 0.4 | NS | |
| 10.3 | 9.8 | SN.PP (°) | 10.4 (3.2) | 0.4 (0.4) | 8.5 (2.2) | 0.1 (0.3) | 0.3 | NS | |
| (8.6–13.5) yrs | (7.3–11.6) yrs | PP.MP (°) | 33.0 (5.1) | −1.9 (0.5) | 36.3 (4.6) | −1.7 (0.4) | −0.2 | NS | |
| OP: 20 months | |||||||||
| Doshi and Bhad-Patil (21) | Spring PBB | Magnetic PBB | Overbite (mm) | NA | 3.4 (1.2) | NA | 4.9 (1.4) | −1.5 | P < 0.05 |
| n = 10 | n = 10 | SN.GoGn (°) | −1.8 (0.8) | −1.9 (1.2) | 0.1 | NS | |||
| OP: 8 months | |||||||||
| Kuster and Ingervall (35) | Spring PBB | Magnetic PBB | Overbite (mm) | −0.5 (−) | 1.3 (−) | −2.0 (−) | 3.0 (−) | −1.7 | NA |
| n = 22 | n = 11 | SN.MP (°) | 42.1 (−) | 0.2 (−) | 37.1 (−) | −1.1 (−) | 1.3 | ||
| 11♀/11♂ | 7♀/4♂ | NSGn (°) | 72.6 (−) | −0.3 (−) | 71.0 (−) | −1.0 (−) | 0.7 | ||
| 9.3 yrs. | 10.7 yrs. | SN.PP (°) | 6.7 (−) | −0.1 (−) | 6.2 (−) | −0.4 (−) | 0.3 | ||
| OP: 12 months | OP: 3 months | PP.MP (°) | 34.7 (−) | 0.4 (−) | 31.1 (−) | −0.6 (−) | 1.0 | ||
| Albogha et al. (25) | Magnetic PBB | RMI + PBB | Overbite (mm) | −3.9 (1.6) | 3.3 (1.3) | −3.8 (1.9) | 3.1 (1.4) | 0.2 | NS |
| n = 15 | n = 15 | FMA (°) | 32.8 (5.8) | −0.2 (2.5) | 33.9 (5.2) | −0.4 (2.5) | 0.2 | NS | |
| 9♀/6♂ | 11♀/4♂ | SN.MP (°) | 42.8 (3.5) | −1.4 (1.2) | 43.7 (5.4) | −1.1 (2.1) | −0.3 | NS | |
| 11.2±1.6 yrs | 10.9±1.8 yrs | NSPog (°) | 74.9 (2.8) | 0.2 (0.9) | 73.2 (3.2) | 0.4 (1.0) | −0.2 | NS | |
| OP: 4 months | PP.MP (°) | 33.8 (5.3) | −0.8 (1.2) | 35.5 (5.1) | 0.4 (2.8) | −1.2 | NS | ||
| BaN.PtGn (°) | 83.9 (3.0) | 1.6 (1.4) | 83.1 (4.7) | 1.7 (2.0) | −0.1 | NS | |||
SD, standard-deviation; ♀, female; ♂, male; yrs, years; G1, group 1; G2, group 2; NS, non-significant; OP, observation period; NA, not available; PBB, posterior bite-blocks; ΔG1, difference between final and baseline measurements for group 1; ΔG2, difference between final and baseline measurements for group 2; ΔG1 − ΔG2, difference between changes observed for groups 1 and 2.
aPre-treatment statistically significant (P < 0.05) differences on bold font, and absence of pre-treatment comparison on italic font.
bStatistically significant (P < 0.05) changes on bold font, and absence of intra-group comparison on italic font.
cConcerning ΔG1 − ΔG2.
Table 6.
Summary of studies characteristics and results of the included studies assessing MEA and VPCC.
| Reference | Sample | Outcomesa | Results | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline G1 | ΔG1b | Baseline G2 | ΔG2b | ΔG1 − ΔG2 | P-valuec | ||||
| Group 1 | Group 2 | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Sankey et al. (42) | Splint slow MEA + VPCC + lip seal training | Untreated | Overbite (mm) | 0.6 (3.0) | 1.3 (2.0) | NA | 0.0 (0.2) | 1.3 | P < 0.001 |
| n = 38 | n = 38 | MPA (°) | 40.0 (3.9) | −0.3 (1.7) | 40.1 (3.9) | −0.2 (2.1) | −0.1 | NS | |
| 24♀/14♂ | 24♀/14♂ | NSGn (°) | 69.8 (3.1) | 0.1 (1.5) | NA | 0.5 (1.2) | −0.4 | NS | |
| 8,.3±1.2 yrs | 8.2±1.3 yrs | SN.PP (°) | 4.1 (3.0) | 0.3 (1.9) | 0.1 (1.0) | 0.2 | NS | ||
| OP: 15 months | - | ||||||||
| Bacetti et al. (16) | Splint rapid MEA + VPCC | Untreated | |||||||
| n = 21 | n = 18 | Overbite (mm) | NA | 1.9 (1.9) | NA | 1.5 (1.9) | 0.4 | NS | |
| - | - | MPA (°) | −1.2 (2.0) | −1.3 (1.9) | 0.1 | NS | |||
| 8.6±0.7 yrs | 8.4±1.0 yrs | FH.PP (°) | 0.8 (1.4) | 0.4 (2.1) | 0.4 | NS | |||
| OP: 31 months | OP: 32 months | PP.MP (°) | −2.1 (2.6) | −1.7 (1.9) | −0.4 | NS | |||
| Pre-pubertal | |||||||||
| Bacetti et al. (16) | Splint rapid MEA + VPCC | Untreated | Overbite (mm) | NA | 1.8 (1.7) | NA | 0.2 (2.2) | 1.6 | NS |
| n = 15 | n = 14 | MPA (°) | −2.9 (2.2) | −0.7 (2.2) | −2.2 | P < 0.05 | |||
| - | - | FH.PP (°) | −0.3 (1.6) | 0.2 (1.7) | −0.5 | NS | |||
| 9.3±1.0 yrs | 9.8±1.2 yrs | PP.MP (°) | −2.6 (1.9) | −1.1 (2.3) | −1.5 | NS | |||
| OP: 36 months | OP: 38 months | ||||||||
| Pubertal | |||||||||
| Schulz et al. (45) | Splint rapid MEA + VPCC | Splint rapid MEA | Overbite (mm) | 2.4 (2.3) | 1.6 (2.1) | 2.5 (2.3) | 0.9 (1.6) | 0.7 | NS |
| n = 29 | n = 29 | MPA (°) | 29.3 (3.5) | −1.3 (1.5) | 29.6 (3.8) | −0.3 (1.7) | −1.0 | NS | |
| 16♀/13♂ | 16♀/13♂ | FH.PP 1 (°) | 2.5 (2.6) | −1.2 (1.6) | 0.4 (2.8) | −1.4 (1.3) | 0.2 | NS | |
| 9.1±1.0 yrs | 9.0±1.0 yrs | ||||||||
| OP: 33 months | OP: 46 months | ||||||||
SD, standard-deviation; ♀, female; ♂, male; yrs, years; G1, group 1; G2, group 2; NS, non-significant; OP, observation period; NA, not available; MEA, Maxillary expansion appliances; VPCC, vertical-pull chin cup; ΔG1, difference between final and baseline measurements for group 1; ΔG2, difference between final and baseline measurements for group 2; ΔG1 − ΔG2, difference between changes observed for groups 1 and 2.
aPre-treatment statistically significant (P < 0.05) differences on bold font, and absence of pre-treatment comparison on italic font.
bStatistically significant (P < 0.05) changes on bold font, and absence of intra-group comparison on italic font.
cConcerning ΔG1 − ΔG2.
Table 7.
Summary of studies characteristics and results of the included studies assessing RMI.
| Reference | Sample | Outcomesa | Results | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline G1 | ΔG1b | Baseline G2 | ΔG2b | ΔG1 − ΔG2 | P-valuec | |||||
| Group 1 | Group 2 | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Cinsar et al (11) | RMI | Untreated | Overbite (mm) | −2.9 (0.6) | −4.5 (0.4) | −3.4 (1.0) | −0.9 (1.1) | −3,6 | P < 0.001 | |
| n = 10 | n = 10 | FMA (°) | 37.8 (4.1) | 4.8 (2.4) | 37.2 (4.4) | 0.3 (2.9) | 4,5 | P < 0.001 | ||
| 7♀/3♂ | 7♀/3♂ | SN.GoGn (°) | 42.4 (3.5) | 4.8 (1.7) | 42.0 (4.5) | 0.0 (2.5) | 4,8 | P < 0.001 | ||
| 10.8 yrs | 10.5 yrs. | NSGn (°) | 70.3 (2.7) | 3.4 (2.7) | 67.8 (3.3) | −0.3 (2.6) | 3,7 | P < 0.001 | ||
| OP: 9–11 months | OP: 10– 11 months | |||||||||
| Albogha et al. (25) | RMI + splint rapid MEA | Magnetic PBB | Overbite (mm) | −3.8 (1.9) | 3.1 (1.4) | −3.9 (1.6) | 3.3 (1.3) | −0.2 | NS | |
| n = 15 | n = 15 | FMA (°) | 33.9 (5.2) | −0.4 (2.5) | 32.8 (5.8) | −0.2 (2.5) | −0.2 | NS | ||
| 11♀/4♂ | 9♀/6♂ | SN.MP (°) | 43.7 (5.4) | −1.1 (2.1) | 42.8 (3.5) | −1.4 (1.2) | 0.3 | NS | ||
| 10.9±1.8 yrs | 11.2±1.6 yrs | NSPog (°) | 73.2 (3.2) | 0.4 (1.0) | 74.9 (2.8) | 0.2 (0.9) | 0.2 | NS | ||
| OP: 4 months | PP.MP (°) | 35.5 (5.1) | 0.4 (2.8) | 33.8 (5.3) | −0.8 (1.2) | 1.2 | NS | |||
| BaN.PtGn (°) | 83.1 (4.7) | 1.7 (2.0) | 83.9 (3.0) | 1.6 (1.4) | 0.1 | NS | ||||
SD, standard-deviation; ♀, female; ♂, male; yrs, years; G1, group 1; G2, group 2; NS, non-significant; OP, observation period; RMI, rapid maxillary intruder; MEA, Maxillary expansion appliances; PBB, posterior bite-blocks; ΔG1, difference between final and baseline measurements for group 1; ΔG2, difference between final and baseline measurements for group 2; ΔG1 − ΔG2, difference between changes observed for groups 1 and 2.
aPre-treatment statistically significant (P < 0.05) differences on bold font, and absence of pre-treatment comparison on italic font.
bStatistically significant (P < 0.05) changes on bold font, and absence of intra-group comparison on italic font.
cConcerning ΔG1 − ΔG2.
Table 8.
Summary of studies characteristics and results of the included studies assessing Class II headgear appliances.
| Reference | Sample | Outcomesa | Results | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline G1 | ΔG1b | Baseline G2 | ΔG2b | ΔG1 − ΔG2 | P-valuec | ||||
| Group 1 | Group 2 | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Ngan et al. (36) | HPA | Untreated | MPA (°) | NA | 1.8 (2.1) | NA | 0.0 (2.1) | 1.8 | NS |
| n = 8 | n = 8 | SN.PP (°) | 0.8 (1.8) | 0.0 (1.0) | 0.8 | NS | |||
| 6♀/2♂ | 6♀/2♂ | ||||||||
| 10.2 yrs | Age-matched | ||||||||
| OP: 14 months | |||||||||
| Jacob et al. (24) | MTA | Untreated | MPA (°) | 35.9 (5.3) | −0.6 (1.6) | 36.2 (3.6) | −0.1 (0.9) | −0.5 | NS |
| n = 13 | n = 22 | NSPog (°) | 77.2 (5.1) | 0.2 (1.1) | 77.2 (3.0) | 0.3 (0.6) | −0.1 | NS | |
| 12♀/1♂ | 20♀/2♂ | SN.PP 2 (°) | 3.9 (3.4) | 2.1 (1.5) | 6.9 (2.7) | 0.0 (0.8) | 2.1 | P < 0.001 | |
| 8.8±0.7 yrs | 8.8±0.7 yrs | PP.MP (°) | 31.9 (4.6) | −2.7 (1.9) | 29.1 (3.4) | −0.2 (1.1) | −2.5 | P < 0.001 | |
| OP: 12 months | |||||||||
SD, standard-deviation; ♀, female; ♂, male; yrs, years; G1, group 1; G2, group 2; NS, non-significant; OP, observation period; NA, not available; HPA, high-pull activator; MTA, modified Thurow appliance; ΔG1, difference between final and baseline measurements for group 1; ΔG2, difference between final and baseline measurements for group 2; ΔG1 − ΔG2, difference between changes observed for groups 1 and 2.
aPre-treatment statistically significant (P < 0.05) differences on bold font, and absence of pre-treatment comparison on italic font.
bStatistically significant (P < 0.05) changes on bold font, and absence of intra-group comparison on italic font.
cConcerning ΔG1 − ΔG2.
Table 9.
Summary of study characteristics and results of the included study assessing VPCC.
| Reference | Sample | Outcomesa | Results | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline G1 | ΔG1b | Baseline G2 | ΔG2b | ΔG1 − ΔG2 | P-valuec | ||||
| Group 1 | Group 2 | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Işcan et al. (43) | |||||||||
| VPCC | Untreated | Overbite (mm) | −2.9 (2.3) | 3.9 (1.4) | −2.2 (2.2) | 0.4 (−) | 3.5 | P < 0.01 | |
| n = 18 | n = 17 | SN.GoGn (°) | 41.1 (3.5) | −1.4 (1.6) | 41.2 (3.7) | −0.1 (−) | −1.3 | P < 0.05 | |
| 12♀/6♂ | 11♀/6♂ | SN.PP (°) | NA | 0.6 (1.8) | NA | 0.2 (−) | 0.4 | NS | |
| 9.4±0.9 yrs | 10.8±1.3 yrs | ||||||||
| OP: 6–12 months | OP: 7–12 months | ||||||||
SD, standard-deviation; ♀, female; ♂, male; yrs, years; G1, group 1; G2, group 2; NS, non-significant; OP, observation period; NA, not available; VPCC, vertical-pull chin cup; ΔG1, difference between final and baseline measurements for group 1; ΔG2, difference between final and baseline measurements for group 2; ΔG1 − ΔG2, difference between changes observed for groups 1 and 2.
aPre-treatment statistically significant (P < 0.05) differences on bold font, and absence of pre-treatment comparison on italic font.
bStatistically significant (P < 0.05) changes on bold font, and absence of intra-group comparison on italic font.
cConcerning ΔG1 − ΔG2.
Discussion
Summary of evidence
Even though most of the selected literature investigated a restricted age range, particularly growing children during mixed dentition phase, there was considerable variation regarding the follow-up periods, as well as broad diversity in terms of therapeutic approaches. Such variation characterizes the great appliance availability for both AOB and hyperdivergent skeletal pattern management during mixed dentition treatment. This variability introduces a great deal of confusion on which protocols tend to be relatively more effective and stable.
In addition, poor-quality RCTs (21, 31, 38) and just a few good-quality nRCTs (12, 15, 16, 25, 45) were not able to disclose consistent results, which hinders any valid attempt to produce a scientifically reliable answer. Despite this, some useful clinical inferences could still be extracted from this review; and suggestions are also provided, so future clinical studies can successfully move toward a stronger evidence-based answer for clinical questions related to the early open bite treatment.
Fränkel regulator-4
FR-4 appears to be an effective therapeutic approach to treat AOB and steep mandibular plane (33). Furthermore, short- (38) and long-term follow-up data (30) suggest that these changes might be stable.
No consensus could be extrapolated regarding the effect of FR-4 on palatal plane inclination. However, the only study which reported no relevant effects (33) had the shortest period of observation and the smallest sample size among those that were considered, which might have contributed to their reported lack of differences concerning the palatal plane inclination and its angular relationship with the mandibular plane.
Open bite bionator
OBB demonstrated to be effective in terms of closing bites and decreasing the palatal and mandibular planes divergence, even though no relevant effects could be detected when the inclination of both planes were assessed separately (14). The positive effects of OBB are expected to last during retention phase (14).
The Quad-helix appliance associated with crib produced a similar skeletal change as OBB, but the former was significantly more effective than the latter in the correction of AOB (12). However, this result could be attributed to baseline differences between groups, according to which patients treated with the quad-helix/crib appliance had more severe AOB than those treated with OBB (12).
According to one study, (15) the association of OBB with high-pull headgear did not produce significant vertical effects, either dental or skeletal. In addition, the effect of the combined therapy produced no additional effects in relation to the sole use of OBB (37). Therefore, there is still no evidence to support the effectiveness (15) or any significant supplementary effect of high-pull headgear when associated with OBB (37).
Posterior bite-blocks
Passive PBB demonstrated to be effective when treating AOB, regardless the splint thickness (40). Even though 10-mm splints produced more pronounced counterclockwise rotation of the mandibular plane, when it was compared to the 5-mm appliance, differences were not significant (40). In addition to overbite and mandibular plane correction, 3- to 4-mm PBB also decreased the palatal and mandibular planes divergence, when associated with VPCC (34). Therefore, there seems to be no ideal splint height when it comes to either dental or skeletal correction, and VPCC supplementary effect deserves additional testing.
According to one study (41), the magnetic PBB cannot be considered an effective treatment for dental or skeletal open bite. Contrastingly, other investigations observed that this appliance significantly rotated the mandibular plane counter-clockwise (32), or considerably decreased AOB (31). However, this effect was not statistically tested (31), and the reported mandibular plane rotation (32), might be attributed to the fact that the baseline mandibular inclination of the treated group was significantly higher than the one observed for the non-treated group at baseline. Therefore, magnetic PBB, if ever effective, still presents arguable results regarding its therapeutic effects (31,32).
Spring-activated PBB demonstrated to significantly decrease AOB, mandibular plane inclination, and its angulation with the palatal plane (34), but none of those results were compared to untreated controls changes. When active appliances, both spring-activated (34) and magnetic PBB (31) were compared with passive designs, no significant differences were found regarding dental or skeletal therapeutic effects. Therefore, the potential superiority of active splints over passive ones has not been convincingly demonstrated so far.
Between both types of active appliances, there seems to be no obvious advantages of a specific design. Even though there were indications that magnetic PBB might correct overbite more effectively (21, 35), in a methodologically sound article (25), minimum differences between both active therapeutic approaches were demonstrated.
Maxillary expansion appliances + vertical-pull chin cup
The use of VPCC during expansion mechanics seems to have limited effectiveness on vertical imbalances, whether dental (16) or skeletal (16, 42), of pre-pubertal patients. Even though it was reported that it might significantly produce an immediate positive effect on overbite (42), no relevant results that persist during the retention period were reported (16).
In case of pubertal patients, VPCC effectively reduced mandibular plane inclination, (16), when comparisons were performed against untreated controls. However, when another study investigated the isolated effect of VPCC on children of similar ages (45), the differences, even though present, did not reach statistical significance. Thus, neither during pubertal growth spurt does VPCC appear to make a statistically and clinically relevant difference.
Rapid maxillary intruder
According to one study, RMI was considered an effective treatment for the improvement of both AOB and steep mandibular plane (11). However, as previously mentioned, when splint RMI was compared to magnetic PBB, both appliances were similarly effective in the correction of overbite (25).
Due to the positive results presented for the RMI (11, 25), the authors consider it to be a potentially effective mechanical approach for the treatment of vertical dental imbalances or skeletal dysplasia.
Class II headgears appliances
Both high-pull activator (36) and modified Thurow appliance (24) are effective appliances for correcting Class II sagittal deviation. However, vertical outcomes were significantly different (24, 36). Even though both appliances utilized similar designs, the former (36) tested a full coverage maxillary splint, while the latter (24) evaluated the effectiveness of a partial splint, with acrylic covering only posterior teeth.
There is no evidence supporting the effectiveness of high-pull activator (36) or modified Thurow appliance on correcting mandibular plane inclination (24), but the latter appears to produce correction of the vertical aspect of Class II patients by rotating the palatal plane clockwise, and thus reducing the divergence between this plane and the mandibular one (24).
Vertical-pull chin cup
Only one study detected positive results for the isolated use of VPCC; and this therapy was effective on reducing both the overbite and the mandibular plane inclination (43).
Recommendations for future studies
Despite all results and inferences mentioned here, further researches might still be carried out to confirm several assumptions. The authors encourage prospective trials to be conducted to investigate both effectiveness and stability of FR-4, OBB, passive and active PBB, RMI, high-pull activator, modified Thurow appliance, and VPCC in the correction of dental and skeletal open bite.
Ideally, these future controlled trials should consecutively recruit pre-calculated samples, and special attention should be also paid to the formation of contemporary and equivalent groups, as well as to the blinded evaluation of the outcomes. Once confirmed as effective, and whenever ethically acceptable, such therapies might as well be compared to each other, so the most effective treatment modalities can be reliably selected and their indications clearly refined.
At this point, the authors also recommend the conduction of methodologically rigorous RCTs for the following particular purposes:
evaluation of the supplementary effect of lip seal exercises on FR-4 therapy;
evaluation of the supplementary effect of high-pull headgear on OBB therapy;
evaluation of the supplementary effect of VPCC on MEA and PBB therapies; and
comparisons between different PBB designs, either active or passive.
Overall limitations
Unfortunately, no meta-analysis could be executed because of large methodological variability in the included studies, particularly in relation to the therapeutic modalities.
Even though several cephalometric parameters were considered in the selected studies, the authors of this systematic review chose not to synthesize other available ones, since these variables were considered secondary to the main objective of this study. Nevertheless, the authors encourage readers to examine the non-extracted data, so that a comprehensive appreciation of mechanisms of action, as well as reasons for eventual ineffectiveness can be fully appreciated.
Conclusions
A comprehensive and updated review regarding the effectiveness of the orthodontic therapy on the early correction of dental or skeletal open bite was provided. Despite large variability and methodological inaccuracies, specific inferences and directions for future studies were presented. Even though the methodological quality of the studies has been improving, additional efforts must still be directed to perform better and conclusive studies.
Supplementary material
Supplementary material is available at European Journal of Orthodontics online.
Funding
This review was not financially supported by any sources.
References
- 1. Karaiskos N Wiltshire W.A. Odlum O. Brothwell D. and Hassard T H (2005) Preventive and interceptive orthodontic treatment needs of an inner-city group of 6- and 9-year-old Canadian children. Journal (Canadian Dental Association), 71, 649. [PubMed] [Google Scholar]
- 2. Cozza P. Baccetti T. Franchi L. Mucedero M. and Polimeni A (2005) Sucking habits and facial hyperdivergency as risk factors for anterior open bite in the mixed dentition. American Journal of Orthodontics and Dentofacial Orthopedics, 128, 517–519. [DOI] [PubMed] [Google Scholar]
- 3. Montaldo L. Montaldo P. Cuccaro P. Caramico N. and Minervini G (2011) Effects of feeding on non-nutritive sucking habits and implications on occlusion in mixed dentition. International Journal of Paediatric Dentistry, 21, 68–73. [DOI] [PubMed] [Google Scholar]
- 4. Guedes R.S. Piovesan C. Antunes J.L. Mendes F.M. and Ardenghi T.M (2014) Assessing individual and neighborhood social factors in child oral health-related quality of life: a multilevel analysis. Quality of Life Research, 23, 2521–2530. [DOI] [PubMed] [Google Scholar]
- 5. Phelan A., Franchi L., Baccetti T., Darendeliler M.A., McNamara J.A., Jr (2014) Longitudinal growth changes in subjects with open-bite tendency: a retrospective study. American Journal of Orthodontics and Dentofacial Orthopedics, 145, 28–35. [DOI] [PubMed] [Google Scholar]
- 6. Moon S.C. Kim H.K. Kwon T.K. Han S.H. An C.H. and Park Y.S (2013) Patterns of vertical facial growth in Korean adolescents analyzed with mixed-effects regression analysis. American Journal of Orthodontics and Dentofacial Orthopedics, 143, 810–818. [DOI] [PubMed] [Google Scholar]
- 7. Jacob H.B. and Buschang P.H (2011) Vertical craniofacial growth changes in French-Canadians between 10 and 15 years of age. American Journal of Orthodontics and Dentofacial Orthopedics, 139, 797–805. [DOI] [PubMed] [Google Scholar]
- 8. Cozza P. Mucedero M. Baccetti T. and Franchi L (2005) Early orthodontic treatment of skeletal open-bite malocclusion: a systematic review. The Angle Orthodontist, 75, 707–713. [DOI] [PubMed] [Google Scholar]
- 9. Lentini-Oliveira D.A. Carvalho F.R. Rodrigues C.G. Ye Q. Prado L.B. Prado G.F. and Hu R (2014) Orthodontic and orthopaedic treatment for anterior open bite in children. The Cochrane Database of Systematic Reviews, 24, 9, CD005515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cozza P. Baccetti T. Franchi L. and McNamara J.A. Jr (2006) Treatment effects of a modified quad-helix in patients with dentoskeletal open bites. American Journal of Orthodontics and Dentofacial Orthopedics, 129, 734–739. [DOI] [PubMed] [Google Scholar]
- 11. Cinsar A. Alagha A.R. and Akyalçin S (2007) Skeletal open bite correction with rapid molar intruder appliance in growing individuals. The Angle Orthodontist, 77, 632–639. [DOI] [PubMed] [Google Scholar]
- 12. Cozza P. Baccetti T. Franchi L. and Mucedero M (2007) Comparison of 2 early treatment protocols for open-bite malocclusions. American Journal of Orthodontics and Dentofacial Orthopedics, 132, 743–747. [DOI] [PubMed] [Google Scholar]
- 13. Cozza P Mucedero M. Baccetti T. and Franchi L (2007) Treatment and posttreatment effects of quad-helix/crib therapy of dentoskeletal open bite. The Angle Orthodontist, 77, 640–645. [DOI] [PubMed] [Google Scholar]
- 14. Defraia E. Marinelli A. Baroni G. Franch L. and Baccetti T (2007) Early orthodontic treatment of skeletal open-bite malocclusion with the open-bite bionator: a cephalometric study. American Journal of Orthodontics and Dentofacial Orthopedics, 132, 595–598. [DOI] [PubMed] [Google Scholar]
- 15. Freeman C.S. McNamara J.A. Jr. Baccetti T. Franchi L. and Graff T.W (2007) Treatment effects of the bionator and high-pull facebow combination followed by fixed appliances in patients with increased vertical dimensions. American Journal of Orthodontics and Dentofacial Orthopedics, 131, 184–195. [DOI] [PubMed] [Google Scholar]
- 16. Baccetti T. Franchi L. Schulz S.O. and McNamara J.A. Jr (2008) Treatment timing for an orthopedic approach to patients with increased vertical dimension. American Journal of Orthodontics and Dentofacial Orthopedics, 133, 58–64. [DOI] [PubMed] [Google Scholar]
- 17. Giuntini V. Franchi L. Baccetti T. Mucedero M. and Cozza P (2008) Dentoskeletal changes associated with fixed and removable appliances with a crib in open-bite patients in the mixed dentition. American Journal of Orthodontics and Dentofacial Orthopedics, 133, 77–80. [DOI] [PubMed] [Google Scholar]
- 18. Suwwan I.Y. (2008) Longitudinal effects of habit-breaking appliances on tongue and dento-alveolar relations and speech in children with oral habits. Master’s thesis, University of Toronto, Toronto, Canada: p. 183. [Google Scholar]
- 19. Torres F.C. (2008) Estudo comparativo entre as grades palatinas removível e fixa, associadas à mentoneira, no tratamento da mordida aberta anterior. Doctor’s thesis. Faculdade de Odontologia de Bauru, Bauru, Brazil: p. 174. [Google Scholar]
- 20. Cassis M.A. (2009) Tratamento da mordida aberta anterior com esporão colado e mentoneira estudo comparativo dos efeitos dentoalveolares e esqueléticos. Master’s thesis. Faculdade de Odontologia de Bauru, Bauru, Brazil: p. 205. [Google Scholar]
- 21. Doshi U.H. and Bhad-Patil W.A (2010) Early management of skeletal open bite with spring-loaded and magnetic bite blocks. World Journal of Orthodontics, 11, 107–116. [PubMed] [Google Scholar]
- 22. Madiraju G.S. and Harika L (2011) Effectiveness of appliance therapy in reducing overjet and open bite associated with thumb sucking habit. Minerva Stomatologica, 60, 333–338. [PubMed] [Google Scholar]
- 23. Mucedero M. Franchi L. Giuntini V. Vangelisti A. McNamara J.A. Jr. and Cozza P (2013) Stability of quad-helix/crib therapy in dentoskeletal open bite: a long-term controlled study. American Journal of Orthodontics and Dentofacial Orthopedics, 143, 695–703. [DOI] [PubMed] [Google Scholar]
- 24. Jacob H.B. dos Santos-Pinto A. and Buschang P.H (2014) Dental and skeletal components of Class II open bite treatment with a modified Thurow appliance. Dental Press Journal of Orthodontics, 19, 19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Albogha M.H. Takahashi I. and Sawan M.N (2015) Early treatment of anterior open bite: comparison of the vertical and horizontal morphological changes induced by magnetic bite-blocks and adjusted rapid molar intruders. Korean Journal of Orthodontics, 45, 38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Flores-Mir C. (2007) Can we extract useful and scientifically sound information from retrospective nonrandomized trials to be applied in orthodontic evidence-based practice treatments? American Journal of Orthodontics and Dentofacial Orthopedics, 131, 707–708. [DOI] [PubMed] [Google Scholar]
- 27. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Checklist (2009). http://www.prisma-statement.org/ (10 October 2014, date last accessed).
- 28. Higgins J.P., et al. (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical Research Ed), 343, d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Slim K. Nini E. Forestier D. Kwiatkowski F. Panis Y. and Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ Journal of Surgery, 73, 712–716. [DOI] [PubMed] [Google Scholar]
- 30. Fränkel R. and Fränkel C (1983) A functional approach to treatment of skeletal open bite. American Journal of Orthodontics, 84, 54–68. [DOI] [PubMed] [Google Scholar]
- 31. Kiliaridis S. Egermark I. and Thilander B (1990) Anterior open bite treatment with magnets. European Journal of Orthodontics, 12, 447–457. [DOI] [PubMed] [Google Scholar]
- 32. Barbre R.E. and Sinclair P.M (1991) A cephalometric evaluation of anterior openbite correction with the magnetic active vertical corrector. The Angle Orthodontist, 61, 93–102. [DOI] [PubMed] [Google Scholar]
- 33. Haydar B. and Enacar A (1992) Functional regulator therapy in treatment of skeletal open-bite. The Journal of Nihon University School of Dentistry, 34, 278–287. [DOI] [PubMed] [Google Scholar]
- 34. Işcan H.N. Akkaya S. and Koralp E (1992) The effects of the spring-loaded posterior bite-block on the maxillo-facial morphology. European Journal of Orthodontics, 14, 54–60. [DOI] [PubMed] [Google Scholar]
- 35. Kuster R. and Ingervall B (1992) The effect of treatment of skeletal open bite with two types of bite-blocks. European Journal of Orthodontics, 14, 489–499. [DOI] [PubMed] [Google Scholar]
- 36. Ngan P. Wilson S. Florman M. and Wei S (1992) Treatment of Class II open bite in the mixed dentition with a removable functional appliance headgear. Quintessence International, 23, 323–333. [PubMed] [Google Scholar]
- 37. Weinbach J.R. and Smith R.J (1992) Cephalometric changes during treatment with the open bite Bionator. American Journal of Orthodontics and Dentofacial Orthopedics, 101, 367–374. [DOI] [PubMed] [Google Scholar]
- 38. Erbay E. Uğur T. and Ulgen M (1995) The effects of Frankel’s function regulator (FR-4) therapy on the treatment of Angle Class I skeletal anterior open bite malocclusion. American Journal of Orthodontics and Dentofacial Orthopedics, 108, 9–21. [DOI] [PubMed] [Google Scholar]
- 39. Villa N.L. and Cisneros G.J (1997) Changes in the dentition secondary to palatal crib therapy in digit-suckers: a preliminary study. Pediatric Dentistry, 19, 323–326. [PubMed] [Google Scholar]
- 40. Işcan H.N. and Sarisoy L (1997) Comparison of the effects of passive posterior bite -blocks with different construction bites on the craniofacial and dentoalveolar structures. American Journal of Orthodontics and Dentofacial Orthopedics, 112, 171–178. [DOI] [PubMed] [Google Scholar]
- 41. Bazzucchi A. Hans M.G. Nelson S. Powers M. and Parker S (1999) Evidence of correction of open bite malocclusion using active vertical corrector treatment. Seminars in Orthodontics, 5, 110–120. [DOI] [PubMed] [Google Scholar]
- 42. Sankey W.L. Buschang P.H. English J. and Owen A.H. III (2000) Early treatment of vertical skeletal dysplasia: the hyperdivergent phenotype. American Journal of Orthodontics and Dentofacial Orthopedics, 118, 317–327. [DOI] [PubMed] [Google Scholar]
- 43. Işcan H.N. Dinçer M. Gültan A. Meral O. and Taner-Sarisoy L (2002) Effects of vertical chincap therapy on the mandibular morphology in open-bite patients. American Journal of Orthodontics and Dentofacial Orthopedics, 122, 506–511. [DOI] [PubMed] [Google Scholar]
- 44. Ferreira F.P.C. (2004) Estudo cefalométrico dos efeitos do aparelho removível com grade palatina, associado à mentoneira, no tratamento de mordida aberta anterior. Master’s thesis, Faculdade de Odontologia de Bauru, Bauru, Brazil: p. 155. [Google Scholar]
- 45. Schulz S.O. McNamara J.A. Jr. Baccetti T. and Franchi L. (2005) Treatment effects of bonded RME and vertical-pull chincup followed by fixed appliance in patients with increased vertical dimension. American Journal of Orthodontics and Dentofacial Orthopedics, 128, 326–336. [DOI] [PubMed] [Google Scholar]