Abstract
Prolonged ER stress (ERS) can be associated with the induction of apoptotic cell death in various heart diseases. In this study, we searched for microRNAs affecting ERS in the heart using in silico and in vitro methods. We found that miR-185 directly targets the 3′-untranslated region of Na+/H+ exchanger-1 (NHE-1), a protein involved in ERS. Cardiomyocyte ERS-triggered apoptosis induced by 100 ng/ml tunicamycin (TM) or 1 μM thapsigargin (TG), ERS inducers, was significantly reduced by miR-185 overexpression. Protein expression of pro-apoptotic markers such as CCAAT/enhancer-binding protein homologous protein (CHOP) and cleaved-caspase-3 was also markedly reduced by miR-185 in a dose-dependent manner. Cariporide (20 μM), a pharmacological inhibitor of NHE-1, also attenuated ERS-induced apoptosis in cardiomyocytes and CHOP protein expression, suggesting that NHE-1 plays an important role in ERS-associated apoptosis in cardiomyocytes. Collectively, the present results demonstrate that miR-185 is involved in cardio-protection against ERS-mediated apoptotic cell death. [BMB Reports 2016; 49(4): 208-213]
Keywords: Cariporide, Caspase-3, CHOP, microRNA, Unfolded protein response
INTRODUCTION
The endoplasmic reticulum (ER) is a cellular organelle that plays an essential role in multiple processes such as protein folding, calcium homeostasis, and lipid biosynthesis (1). Various stimuli such as cardiac pressure-overload, ischemia, oxidative stress, gene mutation, and elevated protein synthesis can potentially lead to the accumulation of unfolded proteins, a condition referred to as ER stress (ERS) (2). When ERS occurs, the ER chaperone Bip/GRP78 dissociates from the three ER trans-membrane sensors such as protein kinase RNA-like ER kinase (PERK), inositol-requiring enzyme 1 (IRE1), and activating transcription factor 6 (ATF6), leading to unfolded protein response (UPR) to maintain ER homeostasis by reducing the accumulation of unfolded proteins (3, 4). In the heart, acute activation of the ERS response is cytoprotective, but if the stress is severe and/or remains unmitigated, it can lead to apoptotic cell death, ultimately resulting in heart failure (5).
MicroRNAs (miRNAs) are a novel class of endogenous small non-coding RNAs which bind to the 3′-untranslated region (3′-UTR) of the target gene, resulting in mRNA degradation/translational inhibition (6). During the last decade, it has become apparent that miRNAs are associated with many cardiac diseases such as myocardial ischemia, cardiac hypertrophy, and heart failure (7, 8). Recently, their roles in cardiac protection have been increasingly evaluated. For example, miR-214 protects the mouse heart from ischemia/reperfusion (I/R) injury through multiple targets, including sodium/calcium exchanger 1 (NCX1), calcium/calmodulin-dependent protein kinase II delta (CaMKIIδ), and cyclophilin D (CypD). miR-139-5p, miR-125b*, and let-7b have cardioprotective effects against I/R injury (8). miR-138, which is up-regulated by hypoxia, attenuates hypoxia-induced apoptosis through the MLK3/JNK/c-jun pathway (9).
The Na+/H+ exchanger isoform-1 (NHE-1) is a plasma membrane glycoprotein responsible for the major Na+ influx pathway in cardiac cells. Among the ten known isoforms of Na+/H+ exchangers (NHE-1 to NHE-10), NHE-1 is the only isoform present in myocardium and is particularly important as it is implicated in many aspects of cardiac pathology (11-13). Increasing evidence suggests that NHE-1 inhibitors such as cariporide (Hoe 642) (11), eniporide (12), and zoniporide (13) could significantly protect against cardiac hypertrophy, I/R injury, and myocardial infarction. NHE-1 activity is regulated by multiple mechanisms such as intracellular acidosis, hormones, mechanical stimuli, and protein kinases (14). However, the miRNA that directly regulates NHE-1 expression remains to be identified.
In the present study, we determined that miR-185 inhibits the expression of NHE-1 by direct binding to two recognition sites within the 3′-UTR and the inhibition could lead to alleviation of ERS-induced myocardial apoptosis. We also found that pharmacological inhibition of NHE-1 by cariporide could mimic the inhibitory effect on ERS-induced apoptosis, further suggesting that regulation of NHE-1 by miR-185 is cardio-protective against ERS. Our results provide a novel mechanistic explanation for myocardial apoptosis, through miR-185 regulation.
RESULTS
miR-185 directly targets the 3′-UTR of NHE-1 in two distinct sites
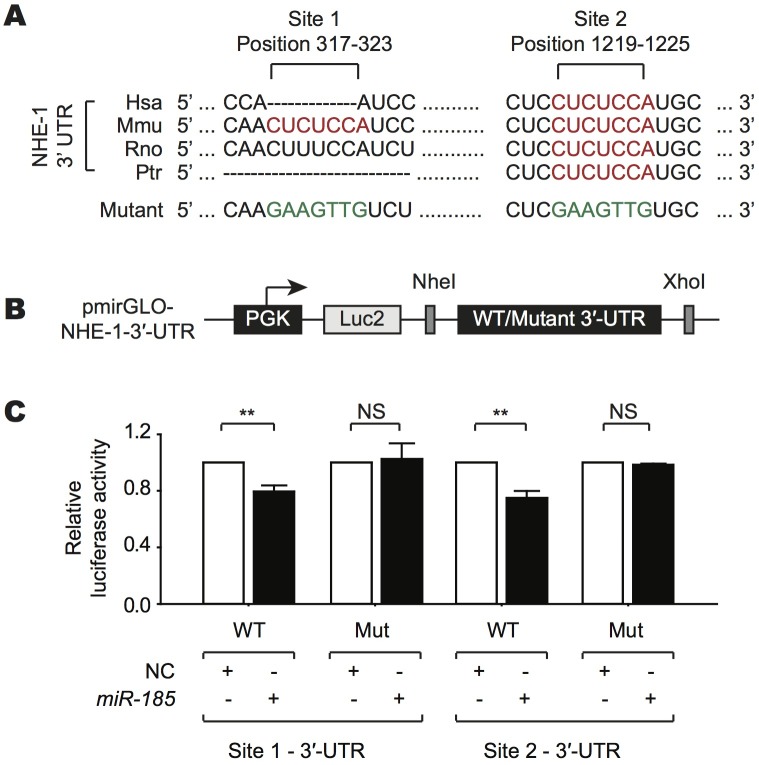
A bioinformatic target prediction using TargetScan showed that two putative binding sites for miR-185 are present in the 3′-UTR of NHE-1 and well-conserved between human, mouse, rat, and chimpanzee (Fig. 1A). To determine whether NHE-1 is a direct target of miR-185, WT or mutated sequences of each predicted miR-185 sites in the 3'-UTR of NHE-1 were inserted in the pmirGLO Dual-Luciferase miRNA target expression vector (Fig. 1B). miR-185 decreased the luciferase activity of the 3'-UTR of WT NHE-1 at both sites significantly, but it did not affect that of the mutant NHE-1 (Fig. 1C).
Fig. 1. miR-185 directly targets two recognition sites within the 3′-UTR of NHE-1. (A) Sequence alignment of the predicted miR-185 binding sites in the 3′-UTR of NHE-1 for several species, including Homo sapiens (Hsa), Mus musculus (Mmu), Rattus norvegicus (Rno), and Pan troglodytes (Ptr). The mutated nucleotides are highlighted in green. (B) Schematic diagram of the pmirGLO chimeric vector showing where the wild type (WT) or mutant complement target sequences for miR-185 were cloned into the 3′-UTR of the luciferase gene. (C) Luciferase assay was performed with reporter containing WT or mutated NHE-1 3′-UTRs in HEK-293 cells transfected with either miR-185 mimic or a negative control (NC) mimic. Note that NHE-1 (mouse) contained 2 putative binding sites for miR-185 and that the effect of site 1 was similar to that of site 2. All data are presented as mean ± SEM; N = 3; Statistical significance is shown as *P < 0.05, **P < 0.001, or NS (not significant). Data were statistically analyzed by student’s t-test.
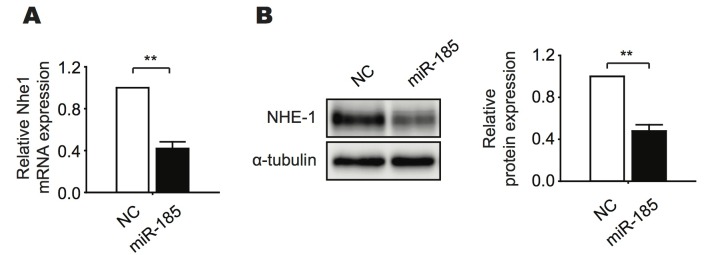
We next examined whether miR-185 overexpression could suppress NHE-1 mRNA and protein expression by qRT-PCR and western blotting, respectively. Both NHE-1 mRNA and protein expression were markedly reduced by miR-185 overexpression in neonatal rat ventricular myocytes (NRVMs) (Fig. 2A, B). Taken together, these data suggest that miR-185 negatively regulates NHE-1 expression both at the mRNA and protein levels and that the negative effect is mediated by direct binding of miR-185 to the 3'-UTR of NHE-1 mRNA.
Fig. 2. miR-185 inhibits both mRNA and protein expression of NHE-1 in NRVMs. (A) qRT-PCR analysis of NHE-1 mRNA expression in NRVMs after transfection with miR-185 mimic or NC mimic for 72 h. (B) Western blotting was performed as in (A), using an antibody against NHE-1 or α-tubulin (left). Quantified western blot results are presented (right). All data are presented as mean ± SEM; N = 3; Statistical significance is shown as **P < 0.001. Data were statistically analyzed by student’s t-test.
miR-185 prevents ERS-induced cardiomyocyte apoptosis
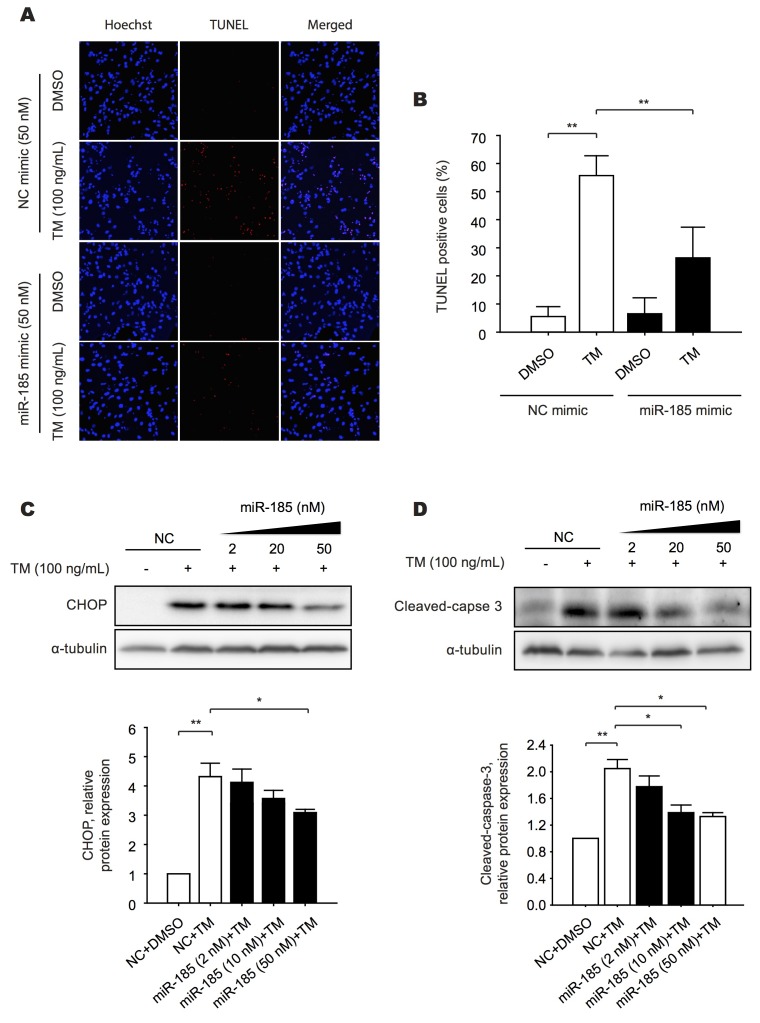
A recent study using NHE-1 transgenic mice presented a significant increase in ERS responsive proteins such as GRP78, GRP94, p-eIF2α, and CCAAT/enhancer-binding protein homologous protein (CHOP) in the heart and spontaneously developed heart failure (16), suggesting that NHE-1 is a critical protein involved in ERS-mediated myocardial apoptosis. To investigate whether miR-185 has an inhibitory effect on myocardial apoptosis through targeting NHE-1, NRVMs were treated with miR-185 mimic or negative control (NC) mimic in conjunction with 100 ng/ml TM, a well-known ERS inducer for 48 h treatment. The results showed that TM induced apoptosis in NRVMs as evidenced by the TUNEL assay results, but this response was significantly attenuated by miR-185 overexpression (Fig. 3A, B).
Fig. 3. Overexpression of miR-185 attenuates ERS-induced apoptosis. (A) Twenty four hours after transfection with miR-185 mimic (in parallel to a negative control(NC)), cardiomyocytes were exposed to 100 ng/ml TM for 48 h. Apoptotic cells represented by the TUNEL-positive cells (magenta in the merged images) were counted. Nuclei were identified by staining with Hoechst 33342 (blue). (B) Quantification of the percentage of TUNEL-positive cardiomyocytes. (C, D) Twenty-four hours after transfection with increasing concentrations of miR-185 mimic, cardiomyocytes were treated with 100 ng/ml TM for 24 h. Western blotting was performed using antibodies against CHOP and cleaved-caspase 3. α-tubulin is shown as a loading control. Results are presented as mean ± SEM; N = 3; Statistical significance is shown as *P < 0.05 or **P < 0.001. Data were statistically analyzed by one-way ANOVA followed by a Bonferroni’s multiple-comparison of multiple means.
The most significant ERS-induced apoptotic pathway is mediated through CHOP, which is regulated by the ATF4 and ATF6 pathways. A recent study suggested that CHOP plays a key role in the transition from cardiac hypertrophy to heart failure, where occurrence of myocardial apoptosis prevails (17). Therefore, to determine whether miR-185 overexpression could inhibit CHOP production, CHOP expression level was measured in TM-treated NRVMs in the presence or absence of miR-185. As shown in Fig. 3C, the transfection with increasing concentration of miR-185 caused a progressive reduction of CHOP expression. A dose-dependent reduction of the proteolytic cleavage of caspase-3 was also observed when miR-185 was overexpressed in NRVMs as shown in Fig. 3D. Similar results were obtained when NRVMs were treated with 1 μM TG, an ERS inducer by irreversible inhibition of sarco/endoplasmic reticulum calcium ATPase (SERCA), in miR-185 overexpressing cells (Fig. S1A-D).
Taken together, these data demonstrate that miR-185 overexpression protects NRVMs from ERS-induced apoptosis.
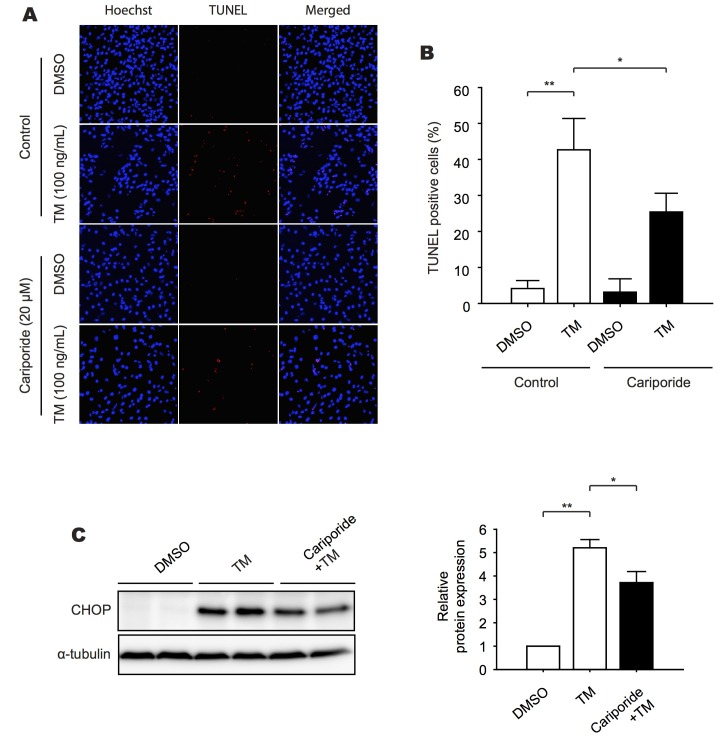
Pharmacological inhibition of NHE-1 inhibits ERS-induced apoptosis
To confirm whether NHE-1, a target of miR-185, is functionally associated with ERS-induced myocardial apoptosis, we treated NRVMs with 20 μM cariporide, a specific blocker of NHE-1 isoform, followed by 100 ng/ml TM treatment for 48 h. Subsequently, the extent of apoptosis was measured by using the TUNEL assay. NRVMs exposed to TM showed approximately 50% of TUNEL positivity and this was significantly reduced in 20 μM cariporide pretreated samples (Fig. 4A, B). The elevated level of CHOP expression by TM was also significantly reduced in cariporide pretreated cells (Fig. 4C). Similarly, cardiomyocyte apoptosis by 1 μM TG treatment was significantly inhibited by 20 μM cariporide pretreatment (Fig. S2A-D), suggesting that NHE-1 inhibition protects cardiomyocytes from apoptotic cell death through suppression of ERS.
Fig. 4. Inhibition of NHE-1 prevents ERS-induced apoptosis. (A) Effect of pretreatment with NHE-1 specific inhibitor, cariporide, on cardiomyocyte apoptosis. Twenty micromolar of cariporide was added 30 minutes before TM (100 ng/ml) treatment. After 48 h, cardiomyocytes were subjected to TUNEL assay. Apoptotic cells represented by the TUNEL-positive cells (magenta in the merged images) were counted. Nuclei were identified by staining with Hoechst 33342 (blue). (B) Quantification of the percentage of TUNEL-positive cells. (C) NRVMs were treated with cariporide (20 μM) 30 minutes before TM (100 ng/ml) treatment for 24 h. Western blotting was performed using an antibody against CHOP. α-tubulin is shown as a loading control (Left). The quantitative analysis of the western blotting results is presented (Right). All data represent mean ± SEM; N = 3; Statistical significance is shown as *P < 0.05 or **P < 0.001. Data were statistically analyzed by one-way ANOVA followed by a Bonferroni’s multiple-comparison of multiple means.
Collectively, our data indicate that miR-185 has a cardioprotective effect against ERS-induced apoptosis mediated through direct repression of NHE-1.
DISCUSSION
The ER is the primary site for biosynthesis and maturation of secretory proteins and Ca2+ storage. For proper protein folding in the ER, a balance between the levels of Ca2+, molecular chaperones, and redox status in the ER lumen must be maintained. The importance of the ER homeostasis is reflected by its critical roles in the pathogenesis of many diseases such as tumor growth, inflammation, and neurodegenerative disorders, including Parkinson and Alzheimer diseases (18, 19). Especially, ERS has been implicated in a number of cardiac symptoms and diseases such as cardiac hypertrophy, heart failure, cardiomyopathy, and I/R injury (5).
Recently, miRNAs have emerged as central regulators of ER homeostasis and key modulators of UPR signaling. For example, overexpression of the miR-23a~27a~24-2 cluster up-regulates ERS-related proteins such as CHOP, PERK, and IRE1α, inducing apoptosis (20). miR-122 overexpression represses UPR signaling via the CDK4-PSMD10 pathway, thereby altering tumorigenic properties of hepatocellular carcinoma cells (21).
In the present study, we attempted to identify microRNAs regulating UPR- and ERS-induced apoptosis in the heart. The major findings of this study are as follows: 1) miR-185 overexpression prevents ERS-induced apoptosis as shown by TUNEL assay. 2) miR-185 overexpression significantly inhibits CHOP expression and the cleavage of caspase-3, indicative of apoptosis. 3) miR-185 directly targets two distinct sites in the 3′-UTR of NHE-1, thereby inhibiting NHE-1 expression. 4) Pharmacological inhibition of NHE-1 by cariporide significantly inhibited ERS-induced apoptosis. Taken together, the present data suggest that inhibition of NHE-1 activity by either overexpression of miR-185 or treatment with cariporide can protect cardiomyocytes from apoptotic cell death.
The involvement of NHE-1 in the pathogenesis of cardiovascular diseases such as cardiac hypertrophy (22), I/R injury (23), cardiac fibrosis, and heart failure (24) has been reported. Evidence also suggests a cardio-protective effect of NHE-1 inhibition against those cardiac diseases. The possible cardio-protective mechanisms through NHE-1 inhibition involve 1) the blockade of NHE-1-dependent Na+ influx and subsequent attenuation of Ca2+-overload, preventing mitochondrial Ca2+ accumulation and mitochondrial permeability transition (MPT) pore opening (25, 26) and 2) the inhibition of reactive oxygen species (ROS) production, a crucial factor involved in cardiomyocyte apoptosis (27), through direct mitochondrial action (28). However, the effect of NHE-1 inhibition in the ERS-induced cardiomyocyte apoptosis has been largely unknown. In the present study, we identified a novel molecular mechanism linking the inhibition of NHE-1 to the attenuation of ERS and subsequent prevention of cardiomyocyte apoptosis.
Several studies indicated the correlation between ERS and cardiac hypertrophy. For example, hypertrophic hearts present elevated protein synthesis and morphological expansion of the ER (29). ER chaperones were substantially induced in mice with hypertrophic and failing hearts induced by transverse aortic constriction (17). The oral administration of the chemical chaperone PBA (4-phenylbutyric acid) could alleviate ERS and prevented cardiac hypertrophy and ERS-induced apoptosis (30), suggesting that ERS is a part of the hypertrophic response and may contribute, at least in part, to cardiac apoptosis observed during the transition from cardiac hypertrophy to failure.
Since miR-185 was previously shown to simultaneously target several pro-hypertrophic genes such as CaMKIIδ, NCX1, and Nuclear Factor of Activated T-cell (NFAT) C3 (15), we further investigated their roles in ERS-induced cardiomyocyte apoptosis. However, pretreatment of NRVMs with specific inhibitors such as KN-62 (CaMKIIδ inhibitor (31)), cyclosporin A (calcineurin-NFATc signaling inhibitor (32)), and SEA0400 (NCX1 inhibitor (33)) did not significantly affect ERS-induced cardiomyocyte apoptosis, as assessed by CHOP protein expression (Fig. S3), suggesting that the primary effect of miR-185 on the inhibition of ERS-mediated apoptotic cell death was associated with NHE-1 inhibition.
In conclusion, the present study suggests that NHE-1 is an important therapeutic target for the prevention of ERS-mediated apoptotic cell death and miR-185 represents a potential therapeutic strategy for heart diseases associated with apoptotic cell death.
MATERIALS AND METHODS
Materials and methods are available in the Supplemental information.
Acknowledgments
This study was supported by the 2015 GIST Systems Biology Infrastructure Establishment Grant and the National Research Foundation of Korea (NRF) grants funded by the Korea Government, the Ministry of Science, ICT & Future Planning (NRF-2013M3A9A7046297).
References
- 1.Ron D, Walter P. Signal integration in the endoplasmic reticulum unfolded protein resonse. Nat Rev Mol Cell Biol. (2007);8:519–529. doi: 10.1038/nrm2199. [DOI] [PubMed] [Google Scholar]
- 2.Groenendyk J, Agellon LB, Michalak M. Coping with endoplasmic reticulum stress in the cardiovascular system. Annu Rev Physiol. (2013);75:49–67. doi: 10.1146/annurev-physiol-030212-183707. [DOI] [PubMed] [Google Scholar]
- 3.Ryoo HD. Drosophila as a model for unfolded protein response research. BMB Rep. (2015);48:445–453. doi: 10.5483/BMBRep.2015.48.8.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arduíno DM, Raquel Esteves A, Filipa Domingues A, et al. ER-mediated stress induces mitochondrial-dependent caspases activation in NT2 neuron-like cells. BMB Rep. (2009);42:719–724. doi: 10.5483/BMBRep.2009.42.11.719. [DOI] [PubMed] [Google Scholar]
- 5.Groenendyk J, Sreenivasaiah PK, Kim DH, Agellon LB, Michalak M. Biology of endoplasmic reticulum stress in the heart. Circ Res. (2010);107:1185–1197. doi: 10.1161/CIRCRESAHA.110.227033. [DOI] [PubMed] [Google Scholar]
- 6.Valencia-Sanchez MA, Liu J, Hannon GJ, Parker R. Control of translation and mRNA degradation by miRNAs and siRNAs. Genes Dev. (2006);20:515–524. doi: 10.1101/gad.1399806. [DOI] [PubMed] [Google Scholar]
- 7.Leite-Moreira AM, Lourenço AP, Falcão-Pires I, Leite-Moreira AF. Pivotal role of microRNAs in cardiac physiology and heart failure. Drug Discov Today. (2013);18:1243–1249. doi: 10.1016/j.drudis.2013.07.025. [DOI] [PubMed] [Google Scholar]
- 8.Varga Z V, Zvara A, Faragó N, et al. MicroRNAs associated with ischemia-reperfusion injury and cardioprotection by ischemic pre- and postconditioning: protectomiRs. Am J Physiol Heart Circ Physiol. (2014);307:H216–H227. doi: 10.1152/ajpheart.00812.2013. [DOI] [PubMed] [Google Scholar]
- 9.He S, Liu P, Jian Z, et al. MiR-138 protects cardiomyocytes from hypoxia-induced apoptosis via MLK3/JNK/c-jun pathway. Biochem Biophys Res Commun. (2013);441:763–769. doi: 10.1016/j.bbrc.2013.10.151. [DOI] [PubMed] [Google Scholar]
- 10.Nakamura TY, Iwata Y, Arai Y, Komamura K, Wakabayashi S. Activation of Na+/H+ exchanger 1 is sufficient to generate Ca2+ signals that induce cardiac hypertrophy and heart failure. Circ Res. (2008);103:891–899. doi: 10.1161/CIRCRESAHA.108.175141. [DOI] [PubMed] [Google Scholar]
- 11.Chakrabarti S, Hoque AN, Karmazyn M. A rapid ischemia-induced apoptosis in isolated rat hearts and its attenuation by the sodium-hydrogen exchange inhibitor HOE 642 (cariporide). J Mol Cell Cardiol. (1997);29:3169–3174. doi: 10.1006/jmcc.1997.0561. [DOI] [PubMed] [Google Scholar]
- 12.Gumina RJ, Mizumura T, Beier N, Schelling P, Schultz JJ, Gross GJ. A new sodium/hydrogen exchange inhibitor, EMD 85131, limits infarct size in dogs when administered before or after coronary artery occlusion. J Pharmacol Exp Ther. (1998);286:175–183. [PubMed] [Google Scholar]
- 13.Knight DR, Smith AH, Flynn DM, et al. A novel sodium-hydrogen exchanger isoform-1 inhibitor, zoniporide, reduces ischemic myocardial injury in vitro and in vivo. J Pharmacol Exp Ther. (2001);297:254–259. [PubMed] [Google Scholar]
- 14.Alvarez B V, Villa-Abrille MC. Mitochondrial NHE1: a newly identified target to prevent heart disease. Front Physiol. (2013);4:152. doi: 10.3389/fphys.2013.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim JO, Song DW, Kwon EJ, et al. miR-185 plays an Anti-Hypertrophic Role in the Heart via Multiple Targets in the Calcium-Signaling Pathways. PLoS One. (2015);10:e0122509. doi: 10.1371/journal.pone.0122509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cook AR, Bardswell SC, Pretheshan S, et al. Paradoxical resistance to myocardial ischemia and age-related cardiomyopathy in NHE1 transgenic mice: a role for ER stress?. J Mol Cell Cardiol. (2009);46:225–233. doi: 10.1016/j.yjmcc.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 17.Okada K, Minamino T, Tsukamoto Y, et al. Prolonged endoplasmic reticulum stress in hypertrophic and failing heart after aortic constriction: possible contribution of endoplasmic reticulum stress to cardiac myocyte apoptosis. Circulation. (2004);110:705–712. doi: 10.1161/01.CIR.0000137836.95625.D4. [DOI] [PubMed] [Google Scholar]
- 18.Ma Y, Hendershot LM. The role of the unfolded protein response in tumour development: friend or foe?. Nat Rev Cancer. (2004);4:966–977. doi: 10.1038/nrc1505. [DOI] [PubMed] [Google Scholar]
- 19.Lindholm D, Wootz H, Korhonen L. ER stress and neurodegenerative diseases. Cell Death Differ. (2006);13:385–392. doi: 10.1038/sj.cdd.4401778. [DOI] [PubMed] [Google Scholar]
- 20.Chhabra R, Dubey R, Saini N. Gene expression profiling indicate role of ER stress in miR-23a~27a~24-2 cluster induced apoptosis in HEK293T cells. RNA Biol. (2011);8:648–664. doi: 10.4161/rna.8.4.15583. [DOI] [PubMed] [Google Scholar]
- 21.Yang F, Zhang L, Wang F, et al. Modulation of the unfolded protein response is the core of microRNA-122-involved sensitivity to chemotherapy in hepatocellular carcinoma. Neoplasia. (2011);13:590–600. doi: 10.1593/neo.11422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cingolani HE, Ennis IL. Sodium-hydrogen exchanger, cardiac overload, and myocardial hypertrophy. Circulation. (2007);115:1090–1100. doi: 10.1161/CIRCULATIONAHA.106.626929. [DOI] [PubMed] [Google Scholar]
- 23.Karki P, Fliegel L. Overexpression of the NHE1 isoform of the Na+/H+ exchanger causes elevated apoptosis in isolated cardiomyocytes after hypoxia/reoxygenation challenge. Mol Cell Biochem. (2010);338:47–57. doi: 10.1007/s11010-009-0337-5. [DOI] [PubMed] [Google Scholar]
- 24.Engelhardt S. Inhibition of Na+-H+ exchange prevents hypertrophy, fibrosis, and heart failure in beta1-adrenergic receptor transgenic mice. Circ Res. (2002);90:814–819. doi: 10.1161/01.RES.0000014966.97486.C0. [DOI] [PubMed] [Google Scholar]
- 25.Javadov S, Choi A, Rajapurohitam V, Zeidan A, Basnakian AG, Karmazyn M. NHE-1 inhibition-induced cardioprotection against ischaemia/reperfusion is associated with attenuation of the mitochondrial permeability transition. Cardiovasc Res. (2008);77:416–424. doi: 10.1093/cvr/cvm039. [DOI] [PubMed] [Google Scholar]
- 26.Teshima Y, Akao M, Jones SP, Marbán E. Cariporide (HOE642), a selective Na+-H+ exchange inhibitor, inhibits the mitochondrial death pathway. Circulation. (2003);108:2275–2281. doi: 10.1161/01.CIR.0000093277.20968.C7. [DOI] [PubMed] [Google Scholar]
- 27.Von Harsdorf R, Li PF, Dietz R. Signaling pathways in reactive oxygen species induced cardiomyocyte apoptosis. Circulation. (1999);99:2934–2941. doi: 10.1161/01.CIR.99.22.2934. [DOI] [PubMed] [Google Scholar]
- 28.Garciarena CD, Caldiz CI, Correa MV, et al. Na+/H+ exchanger-1 inhibitors decrease myocardial superoxide production via direct mitochondrial action. J Appl Physiol. (2008);105:1706–1713. doi: 10.1152/japplphysiol.90616.2008. [DOI] [PubMed] [Google Scholar]
- 29.Maron BJ, Ferrans VJ, Roberts WC. Myocardial ultrastructure in patients with chronic aortic valve disease. Am J Cardiol. (1975);35:725–739. doi: 10.1016/0002-9149(75)90065-X. [DOI] [PubMed] [Google Scholar]
- 30.Park CS, Cha H, Kwon EJ, Sreenivasaiah PK, Kim DH. The chemical chaperone 4-phenylbutyric acid attenuates pressure-overload cardiac hypertrophy by alleviating endoplasmic reticulum stress. Biochem Biophys Res Commun. (2012);421:578–584. doi: 10.1016/j.bbrc.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 31.Backs J, Song K, Bezprozvannaya S, Chang S, Olson EN. CaM kinase II selectively signals to histone deacetylase 4 during cardiomyocyte hypertrophy. J Clin Invest. (2006);116:1853–1864. doi: 10.1172/JCI27438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eckstein LA, Van Quill KR, Bui SK, Uusitalo MS, O’Brien JM. Cyclosporin A inhibits calcineurin/nuclear factor of activated T-cells signaling and induces apoptosis in retinoblastoma cells. Investig Ophthalmol Vis Sci. (2005);46:782–790. doi: 10.1167/iovs.04-1022. [DOI] [PubMed] [Google Scholar]
- 33.Matsuda T, Arakawa N, Takuma K, et al. SEA0400, a novel and selective inhibitorof the Na+-Ca2+ exchanger, attenuates reperfusion injury in the in vitro and in vivo cerebral ischemic models. J Pharmacol Exp Ther. (2001);298:249–256. [PubMed] [Google Scholar]