Abstract
Poor ovarian reserve (POR) is an important limiting factor for the success of any treatment modality for infertility. It indicates a reduction in quantity and quality of oocytes in women of reproductive age group. It may be age related as seen in advanced years of reproductive life or may occur in young women due to diverse etiological factors. Evaluating ovarian reserve and individualizing the therapeutic strategies are very important for optimizing the success rate. Majority or women with POR need to undergo in vitro fertilization to achieve pregnancy. However, pregnancy rate remains low despite a plethora of interventions and is associated with high pregnancy loss. Early detection and active management are essential to minimize the need for egg donation in these women.
KEY WORDS: Anti-Mullerian hormone, antral follicle count, in vitro fertilization, ovarian reserve tests, poor ovarian reserve
INTRODUCTION
Ovarian reserve defines the quantity and quality of the ovarian primordial follicular pool. Poor ovarian reserve (POR) indicates a reduction in the quantity of ovarian follicular pool in women of reproductive age group and is an important cause of infertility in many couples. Existence of POR has been unmasked due to an increasing acceptance of in vitro fertilization (IVF) as a modality of treatment for infertility. It is believed that approximately 10% of the women undergoing IVF will show poor response to gonadotropin stimulation.[1,2,3] However, the incidence may be much higher in the infertile population as many may never undergo a complete evaluation or IVF.
Diminished ovarian reserve is a phenomenon often noted in women in their mid to late thirties, but it may affect younger women as well. It is believed that there is an accelerated decline in follicular pool at the age of 37–38 when it reaches below a critical of 25,000.[4] Subsequently, there remains a very limited time for conception with one's own eggs. It is believed that this phenomenon is accompanied by a declining quality due to aging oocytes, and hence, young women with POR may have better chance at conception.[5,6] However, recent evidence challenges this and POR may be associated with low pregnancy rates irrespective of age[7,8,9] and a high pregnancy loss.[10,11]
Lack of universally accepted diagnostic criteria for POR has limited a meaningful comparison of therapeutic interventions in these women. Majority of women with POR need to undergo IVF and accept lower oocyte yield and lower pregnancy rates than those with normal ovarian reserve. However, role of simple treatment modalities in such women and implications of POR in a general population of women in reproductive years are areas of great clinical relevance.
This review looks at the diagnosis and management of POR and its implications to fertility and long-term health of such women. Literature search was made using the keywords “ovarian reserve” and “poor ovarian reserve,” using electronic database MEDLINE (1966-2016). A total of 2722 articles were found. Further searches were made for individual etiological factors using their titles as keywords. Appropriate cross-references were manually searched.
DIAGNOSIS
Identifying POR, whether age-related or otherwise is important as, such women have a lower pregnancy rate and higher pregnancy loss compared to age-matched controls with normal ovarian reserve.[11] Shortening of the menstrual cycles due to early follicle development and ovulation is an indicator of POR.[12] However, this variable symptom cannot be utilized as a diagnostic criterion. Various ovarian reserve tests (ORTs) have been in use to assess ovarian reserve and predict response to ovarian stimulation.[13,14] Increasing age is associated with a declining oocyte yield in IVF and reduced pregnancy and live birth rate.[15,16] However, POR may occur in young women; hence, other markers of ovarian reserve are needed to identify such women who would otherwise be labeled as having unexplained infertility. Elevated basal follicle-stimulating hormone (FSH) is one of the earliest ORTs found to be associated with poor response. However, a normal FSH does not exclude poor response and elevation happens relatively late in the course of declining ovarian reserve. Hence, basal FSH is not an ideal test to identify poor responders.[16] Antral follicle count (AFC) and anti-Mullerian hormone (AMH) are the most sensitive markers of ovarian reserve identified to date and are ideal for planning personalized ovarian stimulation protocols. These sensitive markers permit prediction of the whole spectrum of ovarian response with reliable accuracy, and clinicians may use either of the two markers as they can be considered interchangeable.[17]
Majority of the attempts at definition of POR have considered certain parameters noted during ovarian stimulation for IVF: Either a low peak estradiol concentration following conventional ovarian stimulation (300–500 pg/ml)[3,4,18] or a low number of follicles (≤five follicles) and/or eggs (≤five eggs).[18,19] Some definitions consider the age of ≥40 years, an abnormal value of ORT, or previous poor response for diagnosing POR.[20,21,22] In essential, it is a retrospective diagnosis following at least one cycle of IVF with conventional stimulation. A review in 1999 had already documented 35 definitions of POR.[23]
To overcome the limitations imposed by lack of universality in definition for conduct of any research and implementation of meaningful interventions, Bologna criteria have been introduced following the consensus meeting of “ESHRE working group on POR definition” held in 2011.[24]
Bologna criteria recommend the presence of at least two of the following three features for diagnosis of POR:
Advanced maternal age (≥40 years) or any other risk factor for POR
A previous POR (≤three oocytes with a conventional stimulation protocol)
An abnormal ORT (i.e. AFC, 5–7 follicles or AMH, 0.5–1.1 ng/ml).
Two episodes of POR after maximal stimulation are sufficient to define a patient as poor responder in the absence of advanced maternal age or abnormal ORT. By definition, the term “POR” refers to the ovarian response and hence a retrospective diagnosis following one stimulated cycle. However, women over 40 years of age with an abnormal ORT may be classified as “expected poor responders” since both advanced age and an abnormal ORT may indicate reduced ovarian reserve and act as a surrogate of ovarian stimulation cycle.[24]
Bologna criteria have been criticized mainly because of the diversity of the risk factors included such as pelvic infection, endometrioma, ovarian surgery, and extensive periovarian adhesions as the impact of each of these factors on ovarian reserve is highly variable. However, ESHRE consensus is acknowledged as the most important step toward a uniform definition of POR and that these criteria be used in any future randomized controlled trial involving intervention strategies for POR.[25,26]
MECHANISM AND ETIOLOGY OF POOR OVARIAN RESERVE
Reproductive aging is a continuous process from before birth till menopause.[27] Women have a finite number of germ cells whose number peaks at 6–7 million by gestation week 20. From mid-gestation onward and throughout reproductive life, an irreversible attrition progressively diminishes the germ cell pool of the gonad.[28]
Fertility peaks before the age of thirty and thereafter, it is believed to decline gradually. This is due to a reducing primordial follicular pool as a result of ovulation and but predominantly because of follicular atresia. A mathematical model proposes that women experience a biphasic exponential decline in ovarian follicles - a slow decay from birth till 38 years of age with an accelerated decline thereafter.[4] Recent evidence challenges this view and suggests that the decline is due to a progressively increasing rate of atresia throughout the reproductive period.[27] This power model also highlights the difference in the size of the nongrowing follicular (NGF) pool between women. Even among those with “normal ovarian reserve” of the same age, the difference in the size of the follicular pool can be as high as 100-fold. However, it is unclear at present whether this is due a difference in the size of the initial follicular pool or due to differences in the rate of depletion. Available data suggest that NGFs at different ages may have a differing response to changes in hormone levels associated with age.[27]
Follicular atresia has important clinical implications for ovarian stimulation as the magnitude of recruited of follicles is proportional to the size of the NGFs. In addition, women of all age groups with NGFs below the normal range would have a suboptimal response to ovarian stimulation and experience a shortened reproductive lifespan. Considering a fixed time interval between end of fertility and menopause, these women would undergo an early menopause.[29]
In addition to the “natural” age-related decline, factors that may further deplete the ovarian reserve during reproductive years are diverse. Endometrioma, certain pelvic infections, ovarian surgery, all can reduce the ovarian reserve. Such etiological factors are believed to induce impairment of intrafollicular endocrine and other regulatory mechanisms, reduced aromatase activity, reduced biological activity of gonadotropin surge-attenuating factor, and altered blood flow.[30,31,32,33]
Endometrioma and its surgical excision is known to cause POR.[34] Mechanical pressure on ovarian cortex, impaired vascular networks, and alteration of cortical stroma are some of the mechanisms attributed to the damage caused to ovarian follicles.[35]
Genital tuberculosis, even in its latent form, is increasingly being recognized as a cause of POR in Indian women. Such women are known to have abnormal ORTs[36] and show signs of poor response, requiring high doses of gonadotropins for ovarian stimulation, and reduced oocyte yield during IVF.[37] The mechanisms involved in the absence of obvious structural damage is not understood at present. Chlamydial infection is known to adversely influence the ovarian response in those undergoing IVF.[3] In recent years, uterine artery embolization for treatment of fibroids is found to be yet another etiological factor for POR.[38]
Improved management modalities in various malignancies have led to an increased survival of affected children and young adults. Both chemotherapy and radiotherapy are known to affect the ovarian reserve adversely.[39,40,41] Obesity and chronic smoking are other factors known to be associated with POR.[42,43]
Women of certain ethnicities are known to have POR as determined by ovarian reserve markers or exhibit signs of POR while undergoing IVF. In a study of Indian women undergoing IVF, ovarian age of Indian women was found to be approximately 6 years older than their Spanish counterparts.[44] In comparison to White European women, those from India, Southeast Asia, Middle-East, and Afro-Caribbean undergoing IVF in the UK showed a lower live birth rate indicating a possible causative role of ethnicity.[45] Another study examining the ovarian reserve markers in women among different ethnicities found that Chinese, Latina, and African women had a lower ovarian reserve compared to Caucasian women of similar age.[46] However, a study evaluating the disparities in ovarian reserve between different ethnicities showed that Bangladeshi women who migrated to UK as adults or living in Bangladesh had lower ovarian reserve compared to those who migrated in childhood or European women. The role of ethnicity may not be a simple one and early developmental factors may need to be taken into consideration while evaluating inter-group variations.[47]
Altered expression of certain genes in cumulus and granulosa cells have been implicated in the etiology of POR in young women.[48,49] FSH receptor (FSHR) polymorphism is considered to be an important cause of unexpected poor response in young women undergoing IVF. Mutations, polymorphisms, and alternatively spliced variants in FSHR have varied effects on receptor function. They are believed to bring about structural change in the receptor, thereby reducing the hormone-binding ability or hormone-induced signaling ability.[50] Certain types of mutations in FMR1 gene are known to be associated with reduced ovarian functional reserve in young women.[51]
MANAGEMENT
The overriding concern that women with POR have a limited reproductive lifespan to conceive with their own eggs governs all aspects of the management. The vast majority of available evidence on efficacy of various therapeutic interventions in women with POR is in the context of IVF and shows a lowered pregnancy and live birth rate irrespective of age.[7,8,9,52] Avoiding profound and prolonged pituitary suppression, prevention of premature luteinizing hormone (LH) surge, and controlled ovarian stimulation (COS) to maximize oocyte yield and achieve embryos with good implantation potential form the basis of all therapeutic interventions in poor responders. A common hurdle for comparison of treatment strategies has been the different criteria used by investigators to define POR, and Bologna criteria offer an important step in the right direction to identify homogenous groups for evaluating efficacy of various therapies.[53,54,55]
Controlled ovarian stimulation for in vitro fertilization
Most widely used ovarian COS protocols in poor responders involve stimulation with high doses of FSH (300–450 IU/day) to maximize the oocyte yield.[54,55] The addition of LH in the early follicular phase may have beneficial effect on the oocyte and hence embryo quality. However, the available evidence regarding addition of recombinant LH to FSH is inconclusive.[56] Low-dose HCG supplementation or addition of pure HMG where HCG is the source of LH activity has shown some improvements in the oocyte yield.[57,58] Luteal start of FSH has been used to influence the recruitment of follicles without any reported clinical benefit.[59]
Agonists
Agonists are widely used in poor responders undergoing IVF to prevent an endogenous LH surge. Long agonist protocol increases both duration of treatment and total dose of gonadotropins necessary to effect follicular development in poor responders. However, agonists due to their initial flare effect may help in recruitment of the follicles. Hence, short agonist protocol where agonist administration is initiated in the early follicular phase before gonadotropin administration is one of the most widely used agonist protocols in poor responders.[60] Microdose flare and ultrashort protocols are preferred by some clinicians, in an effort to minimize the pituitary suppression, but have not shown to improve the clinical outcomes.[54,55]
Antagonists
Antagonist protocol is increasingly used in the management of women with POR undergoing IVF in the last decade. Antagonists provide an effective way of preventing premature LH surge without prolonging the treatment duration. Pregnancy rates achieved are similar to short agonist protocol. Two meta-analyses have not found any difference in the pregnancy rate between antagonist and short agonist protocols.[61,62]
Natural cycle in vitro fertilization
Natural cycle IVF is used as an alternative to the high-dose regimens in POR to reduce the gonadotropin burden, with possible improvement in oocyte quality, and to reduce the financial burden of high-dose regimens.[63,64,65] Modified natural cycle IVF with the addition of antagonists and small doses of FSH[66,67,68,69] or minimal stimulation combining oral letrozole or clomiphene citrate along with small doses of gonadotropins[70] to improve the number of follicles and successful oocyte retrieval are alternatives to high-dose protocols in women with POR. Cancellation in natural cycles can be as high as 50%. The pregnancy rates have been reported as 8–18% per patient and these protocols provide an alternative for poor responders when the more widely used high-dose FSH protocols are unsuccessful.[54,55]
Pretreatment
Pretreatment with oral contraceptive pills (OCPs), progesterone, or ethinyl estradiol is meant as a strategy to improve follicular synchronization, prevent premature ovulation, and scheduling of cycles. Even though there are no differences noted in the pregnancy rates, pretreatment with OCP may increase the duration of stimulation.[71,72]
Adjuvant therapy
Androgen supplementation in the form of oral dehydroepiandrosterone or transdermal testosterone in poor responders has been explored as it is believed to improve the intrafollicular environment and follicular sensitivity to exogenous FSH. Available evidence shows a modest improvement in various parameters including number of oocytes, embryo quality, and live birth rates.[73,74,75,76]
Growth hormone (GH) supplementation is another adjuvant therapy used in combination with COS in an attempt to improve oocyte yield and pregnancy rates in poor responders. Limited evidence involving small number of women suggests that GH as an adjuvant may be beneficial in poor responders.[77]
Low-dose aspirin has been used in IVF in an attempt to improve pregnancy and live birth rates, and a recent study shows no improvement in IVF outcomes in poor responders following low-dose aspirin supplementation.[78]
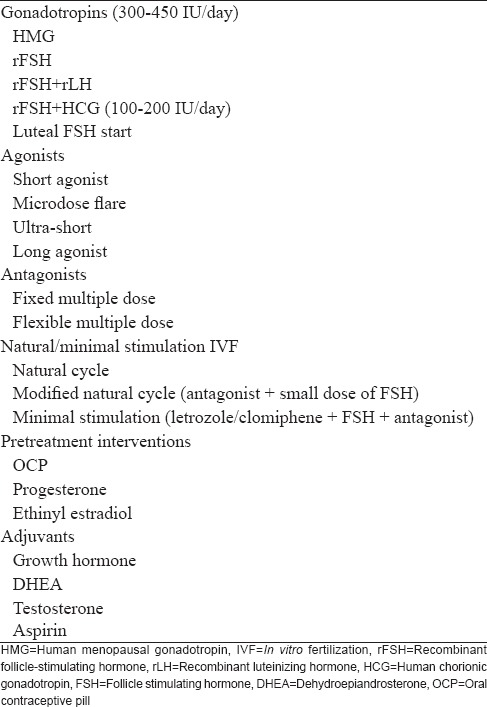
A plethora of therapeutic interventions in the management of POR is summarized in Table 1.
Table 1.
Therapeutic interventions in women with poor ovarian reserve undergoing in vitro fertilization
As mentioned earlier, the existing evidence favors an early recourse to IVF in women with POR as protracted courses of simpler treatment modalities have minimal success rate and IVF offers the highest possibility of live birth in such women.
Limited data available suggest that intrauterine insemination (IUI) yields very few pregnancies with increasing age and it is suggested that in women above 40 years of age, no more than one cycle of COS and IUI should be offered as they still have a reasonable pregnancy rate with IVF.[79,80] Pregnancy rate is low with all modalities of treatment with an increased risk of pregnancy loss across all age groups.[10]
IMPLICATIONS
Ovarian follicular pool undergoes a progressive decline from before birth to menopause.[27] Even though oogonial stem cells have been identified in adult ovaries, there is no conclusive evidence toward their contribution to the size of follicular pool in the postnatal period.[81]
The impact POR is most often seen in the context of infertility where the time available to achieve pregnancy is limited. Pregnancy rates are very low with simple forms of treatment, and IVF in such women offers the highest probability of pregnancy. Irrespective of the age, women with POR have a lower pregnancy rate than those with normal ovarian reserve.[10] Diagnosis of POR imposes a high financial and emotional burden on such couples. When repeated attempts at treatment become unsuccessful, the only options that remain are recourse to oocyte donation or adoption.
Whether ovarian reserve testing should be offered to women who wish to delay childbearing to assist in making an informed decision remains debatable. However, AMH is increasingly being used as a tool to predict fertility potential of such women. They then have the choice of changing their priorities and decide not to delay conception or may undergo IVF to freeze eggs or embryos for future use (social freezing).[82]
Due attention to conserving ovarian cortex during any pelvic surgery including endometrioma excision and, avoiding overenthusiastic ovarian puncture in women with polycystic ovary syndrome are important steps in minimizing the iatrogenic risk of POR. A better understanding of genetic causes may lead to development of molecular markers to assist in choosing the most appropriate COS regimes in such women.[50]
It is known that there is a fixed time interval between onset of POR and menopause.[29] Young women with POR are hence likely to undergo menopause at an earlier age than the normal population. This has long-term health implications beyond fertility to such women, including bone and cardiovascular health.
CONCLUSIONS
POR is an indicator of reduced size of primordial follicular pool, and the resulting eggs are likely to be of suboptimal quality as well. An early recourse to IVF remains the only option with reasonable chance of achieving pregnancy in such women. None of the available therapeutic interventions have the ability to overcome the barriers of low quantity and quality of eggs in women with POR. Women with POR need to be counseled regarding a limited reproductive lifespan, high cost of treatment modalities with lower than normal pregnancy rates. At present, there is no known mechanism to reduce the follicular atresia and prolong fertility. Social egg freezing is a step toward this but does not always ensure pregnancy and childbirth. Delaying childbirth as seen in most of the societies in recent years combined with an increasing incidence of POR poses a great hurdle and challenge to the concerned individuals, the specialists offering fertility services, and the researchers working on various aspects of ovarian reserve.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Garcia JE, Jones GS, Acosta AA, Wright G., Jr Human menopausal gonadotropin/human chorionic gonadotropin follicular maturation for oocyte aspiration: Phase II, 1981. Fertil Steril. 1983;39:174–9. doi: 10.1016/s0015-0282(16)46815-9. [DOI] [PubMed] [Google Scholar]
- 2.Pellicer A, Lightman A, Diamond MP, Russell JB, DeCherney AH. Outcome of in vitro fertilization in women with low response to ovarian stimulation. Fertil Steril. 1987;47:812–5. doi: 10.1016/s0015-0282(16)59170-5. [DOI] [PubMed] [Google Scholar]
- 3.Keay SD, Liversedge NH, Mathur RS, Jenkins JM. Assisted conception following poor ovarian response to gonadotrophin stimulation. Br J Obstet Gynaecol. 1997;104:521–7. doi: 10.1111/j.1471-0528.1997.tb11525.x. [DOI] [PubMed] [Google Scholar]
- 4.Faddy MJ, Gosden RG, Gougeon A, Richardson SJ, Nelson JF. Accelerated disappearance of ovarian follicles in mid-life: Implications for forecasting menopause. Hum Reprod. 1992;7:1342–6. doi: 10.1093/oxfordjournals.humrep.a137570. [DOI] [PubMed] [Google Scholar]
- 5.van Kooij RJ, Looman CW, Habbema JD, Dorland M, te Velde ER. Age-dependent decrease in embryo implantation rate after in vitro fertilization. Fertil Steril. 1996;66:769–75. doi: 10.1016/s0015-0282(16)58634-8. [DOI] [PubMed] [Google Scholar]
- 6.Hanoch J, Lavy Y, Holzer H, Hurwitz A, Simon A, Revel A, et al. Young low responders protected from untoward effects of reduced ovarian response. Fertil Steril. 1998;69:1001–4. doi: 10.1016/s0015-0282(98)00079-x. [DOI] [PubMed] [Google Scholar]
- 7.El-Toukhy T, Khalaf Y, Hart R, Taylor A, Braude P. Young age does not protect against the adverse effects of reduced ovarian reserve – An eight year study. Hum Reprod. 2002;17:1519–24. doi: 10.1093/humrep/17.6.1519. [DOI] [PubMed] [Google Scholar]
- 8.La Marca A, Nelson SM, Sighinolfi G, Manno M, Baraldi E, Roli L, et al. Anti-Müllerian hormone-based prediction model for a live birth in assisted reproduction. Reprod Biomed Online. 2011;22:341–9. doi: 10.1016/j.rbmo.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Khader A, Lloyd SM, McConnachie A, Fleming R, Grisendi V, La Marca A, et al. External validation of anti-Müllerian hormone based prediction of live birth in assisted conception. J Ovarian Res. 2013;6:3. doi: 10.1186/1757-2215-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levi AJ, Raynault MF, Bergh PA, Drews MR, Miller BT, Scott RT., Jr Reproductive outcome in patients with diminished ovarian reserve. Fertil Steril. 2001;76:666–9. doi: 10.1016/s0015-0282(01)02017-9. [DOI] [PubMed] [Google Scholar]
- 11.Elter K, Kavak ZN, Gokaslan H, Pekin T. Antral follicle assessment after down-regulation may be a useful tool for predicting pregnancy loss in in vitro fertilization pregnancies. Gynecol Endocrinol. 2005;21:33–7. doi: 10.1080/09513590500099313. [DOI] [PubMed] [Google Scholar]
- 12.Klein NA, Harper AJ, Houmard BS, Sluss PM, Soules MR. Is the short follicular phase in older women secondary to advanced or accelerated dominant follicle development? J Clin Endocrinol Metab. 2002;87:5746–50. doi: 10.1210/jc.2002-020622. [DOI] [PubMed] [Google Scholar]
- 13.Jirge PR. Ovarian reserve tests. J Hum Reprod Sci. 2011;4:108–13. doi: 10.4103/0974-1208.92283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Broer SL, van Disseldorp J, Broeze KA, Dolleman M, Opmeer BC, Bossuyt P, et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: An individual patient data approach. Hum Reprod Update. 2013;19:26–36. doi: 10.1093/humupd/dms041. [DOI] [PubMed] [Google Scholar]
- 15.Scott RT., Jr Diminished ovarian reserve and access to care. Fertil Steril. 2004;81:1489–92. doi: 10.1016/j.fertnstert.2003.10.051. [DOI] [PubMed] [Google Scholar]
- 16.Galey-Fontaine J, Cédrin-Durnerin I, Chaïbi R, Massin N, Hugues JN. Age and ovarian reserve are distinct predictive factors of cycle outcome in low responders. Reprod Biomed Online. 2005;10:94–9. doi: 10.1016/s1472-6483(10)60808-5. [DOI] [PubMed] [Google Scholar]
- 17.La Marca A, Sunkara SK. Individualization of controlled ovarian stimulation in IVF using ovarian reserve markers: From theory to practice. Hum Reprod Update. 2014;20:124–40. doi: 10.1093/humupd/dmt037. [DOI] [PubMed] [Google Scholar]
- 18.Raga F, Bonilla-Musoles F, Casañ EM, Bonilla F. Recombinant follicle stimulating hormone stimulation in poor responders with normal basal concentrations of follicle stimulating hormone and oestradiol: Improved reproductive outcome. Hum Reprod. 1999;14:1431–4. doi: 10.1093/humrep/14.6.1431. [DOI] [PubMed] [Google Scholar]
- 19.Surrey ES, Bower J, Hill DM, Ramsey J, Surrey MW. Clinical and endocrine effects of a microdose GnRH agonist flare regimen administered to poor responders who are undergoing in vitro fertilization. Fertil Steril. 1998;69:419–24. doi: 10.1016/s0015-0282(97)00575-x. [DOI] [PubMed] [Google Scholar]
- 20.Barrenetxea G, Agirregoikoa JA, Jiménez MR, de Larruzea AL, Ganzabal T, Carbonero K. Ovarian response and pregnancy outcome in poor-responder women: A randomized controlled trial on the effect of luteinizing hormone supplementation on in vitro fertilization cycles. Fertil Steril. 2008;89:546–53. doi: 10.1016/j.fertnstert.2007.03.088. [DOI] [PubMed] [Google Scholar]
- 21.Massin N, Cedrin-Durnerin I, Coussieu C, Galey-Fontaine J, Wolf JP, Hugues JN. Effects of transdermal testosterone application on the ovarian response to FSH in poor responders undergoing assisted reproduction technique – A prospective, randomized, double-blind study. Hum Reprod. 2006;21:1204–11. doi: 10.1093/humrep/dei481. [DOI] [PubMed] [Google Scholar]
- 22.Yarali H, Esinler I, Polat M, Bozdag G, Tiras B. Antagonist/letrozole protocol in poor ovarian responders for intracytoplasmic sperm injection: A comparative study with the microdose flare-up protocol. Fertil Steril. 2009;92:231–5. doi: 10.1016/j.fertnstert.2008.04.057. [DOI] [PubMed] [Google Scholar]
- 23.Surrey ES, Schoolcraft WB. Evaluating strategies for improving ovarian response of the poor responder undergoing assisted reproductive techniques. Fertil Steril. 2000;73:667–76. doi: 10.1016/s0015-0282(99)00630-5. [DOI] [PubMed] [Google Scholar]
- 24.Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L ESHRE Working Group on Poor Ovarian Response Definition. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: The Bologna criteria. Hum Reprod. 2011;26:1616–24. doi: 10.1093/humrep/der092. [DOI] [PubMed] [Google Scholar]
- 25.Venetis CA. The Bologna criteria for poor ovarian response: The good, the bad and the way forward. Hum Reprod. 2014;29:1839–41. doi: 10.1093/humrep/deu138. [DOI] [PubMed] [Google Scholar]
- 26.Ferraretti AP, Gianaroli L. The Bologna criteria for the definition of poor ovarian responders: Is there a need for revision? Hum Reprod. 2014;29:1842–5. doi: 10.1093/humrep/deu139. [DOI] [PubMed] [Google Scholar]
- 27.Hansen KR, Knowlton NS, Thyer AC, Charleston JS, Soules MR, Klein NA. A new model of reproductive aging: The decline in ovarian non-growing follicle number from birth to menopause. Hum Reprod. 2008;23:699–708. doi: 10.1093/humrep/dem408. [DOI] [PubMed] [Google Scholar]
- 28.Peters H. Intrauterine gonadal development. Fertil Steril. 1976;27:493–500. [PubMed] [Google Scholar]
- 29.Kwee J, Schats R, McDonnell J, Schoemaker J, Lambalk CB. The clomiphene citrate challenge test versus the exogenous follicle-stimulating hormone ovarian reserve test as a single test for identification of low responders and hyperresponders to in vitro fertilization. Fertil Steril. 2006;85:1714–22. doi: 10.1016/j.fertnstert.2005.11.053. [DOI] [PubMed] [Google Scholar]
- 30.Hurst BS, Zacur HA, Schlaff WD, Berkovitz GD. Use of granulosa-luteal cell culture to evaluate low and high clinical responses to menotropin stimulation. J Endocrinol Invest. 1992;15:567–72. doi: 10.1007/BF03344926. [DOI] [PubMed] [Google Scholar]
- 31.Martinez F, Barri PN, Coroleu B, Tur R, Sorsa-Leslie T, Harris WJ, et al. Women with poor response to IVF have lowered circulating gonadotrophin surge-attenuating factor (GnSAF) bioactivity during spontaneous and stimulated cycles. Hum Reprod. 2002;17:634–40. doi: 10.1093/humrep/17.3.634. [DOI] [PubMed] [Google Scholar]
- 32.Pellicer A, Ardiles G, Neuspiller F, Remohí J, Simón C, Bonilla-Musoles F. Evaluation of the ovarian reserve in young low responders with normal basal levels of follicle-stimulating hormone using three-dimensional ultrasonography. Fertil Steril. 1998;70:671–5. doi: 10.1016/s0015-0282(98)00268-4. [DOI] [PubMed] [Google Scholar]
- 33.Pellicer A, Albert C, Mercader A, Bonilla-Musoles F, Remohí J, Simón C. The follicular and endocrine environment in women with endometriosis: Local and systemic cytokine production. Fertil Steril. 1998;70:425–31. doi: 10.1016/s0015-0282(98)00204-0. [DOI] [PubMed] [Google Scholar]
- 34.Seyhan A, Ata B, Uncu G. The impact of endometriosis and its treatment on ovarian reserve. Semin Reprod Med. 2015;33:422–8. doi: 10.1055/s-0035-1567820. [DOI] [PubMed] [Google Scholar]
- 35.Ho HY, Lee RK, Hwu YM, Lin MH, Su JT, Tsai YC. Poor response of ovaries with endometrioma previously treated with cystectomy to controlled ovarian hyperstimulation. J Assist Reprod Genet. 2002;19:507–11. doi: 10.1023/A:1020970417778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Malhotra N, Sharma V, Bahadur A, Sharma JB, Roy KK, Kumar S. The effect of tuberculosis on ovarian reserve among women undergoing IVF in India. Int J Gynaecol Obstet. 2012;117:40–4. doi: 10.1016/j.ijgo.2011.10.034. [DOI] [PubMed] [Google Scholar]
- 37.Dam P, Shirazee HH, Goswami SK, Ghosh S, Ganesh A, Chaudhury K, et al. Role of latent genital tuberculosis in repeated IVF failure in the Indian clinical setting. Gynecol Obstet Invest. 2006;61:223–7. doi: 10.1159/000091498. [DOI] [PubMed] [Google Scholar]
- 38.Tropeano G, Di Stasi C, Amoroso S, Gualano MR, Bonomo L, Scambia G. Long-term effects of uterine fibroid embolization on ovarian reserve: A prospective cohort study. Fertil Steril. 2010;94:2296–300. doi: 10.1016/j.fertnstert.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 39.Iwase A, Nakamura T, Nakahara T, Goto M, Kikkawa F. Anti-Müllerian hormone and assessment of ovarian reserve after ovarian toxic treatment: A systematic narrative review. Reprod Sci. 2015;22:519–26. doi: 10.1177/1933719114549856. [DOI] [PubMed] [Google Scholar]
- 40.Bala J, Seth S, Dhankhar R, Ghalaut VS. Chemotherapy: Impact on anti-Müllerian hormone levels in breast carcinoma. J Clin Diagn Res. 2016;10:BC19–21. doi: 10.7860/JCDR/2016/15933.7328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sonigo C, Seroka A, Cédrin-Durnerin I, Sermondade N, Sifer C, Grynberg M. History of ABVD alters the number of oocytes vitrified after in vitro maturation in fertility preservation candidates. Future Oncol. 2016 doi: 10.2217/fon-2016-0009. [DOI] [PubMed] [Google Scholar]
- 42.Moy V, Jindal S, Lieman H, Buyuk E. Obesity adversely affects serum anti-Müllerian hormone (AMH) levels in Caucasian women. J Assist Reprod Genet. 2015;32:1305–11. doi: 10.1007/s10815-015-0538-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Firns S, Cruzat VF, Keane KN, Joesbury KA, Lee AH, Newsholme P, et al. The effect of cigarette smoking, alcohol consumption and fruit and vegetable consumption on IVF outcomes: A review and presentation of original data. Reprod Biol Endocrinol. 2015;13:134. doi: 10.1186/s12958-015-0133-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iglesias C, Banker M, Mahajan N, Herrero L, Meseguer M, Garcia-Velasco JA. Ethnicity as a determinant of ovarian reserve: Differences in ovarian aging between Spanish and Indian women. Fertil Steril. 2014;102:244–9. doi: 10.1016/j.fertnstert.2014.03.050. [DOI] [PubMed] [Google Scholar]
- 45.Jayaprakasan K, Pandian D, Hopkisson J, Campbell BK, Maalouf WE. Effect of ethnicity on live birth rates after in vitro fertilisation or intracytoplasmic sperm injection treatment. BJOG. 2014;121:300–6. doi: 10.1111/1471-0528.12504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bleil ME, Gregorich SE, Adler NE, Sternfeld B, Rosen MP, Cedars MI. Race/ethnic disparities in reproductive age: An examination of ovarian reserve estimates across four race/ethnic groups of healthy, regularly cycling women. Fertil Steril. 2014;101:199–207. doi: 10.1016/j.fertnstert.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Begum K, Muttukrishna S, Sievert LL, Sharmeen T, Murphy L, Chowdhury O, et al. Ethnicity or environment: Effects of migration on ovarian reserve among Bangladeshi women in the United Kingdom. Fertil Steril. 2016;105:744–54.e1. doi: 10.1016/j.fertnstert.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 48.Jindal S, Greenseid K, Berger D, Santoro N, Pal L. Impaired gremlin 1 (GREM1) expression in cumulus cells in young women with diminished ovarian reserve (DOR) J Assist Reprod Genet. 2012;29:159–62. doi: 10.1007/s10815-011-9684-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Skiadas CC, Duan S, Correll M, Rubio R, Karaca N, Ginsburg ES, et al. Ovarian reserve status in young women is associated with altered gene expression in membrana granulosa cells. Mol Hum Reprod. 2012;18:362–71. doi: 10.1093/molehr/gas008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Desai SS, Roy BS, Mahale SD. Mutations and polymorphisms in FSH receptor: Functional implications in human reproduction. Reproduction. 2013;146:R235–48. doi: 10.1530/REP-13-0351. [DOI] [PubMed] [Google Scholar]
- 51.Gleicher N, Yu Y, Himaya E, Barad DH, Weghofer A, Wu YG, et al. Early decline in functional ovarian reserve in young women with low (CGGn < 26) FMR1 gene alleles. Transl Res. 2015;166:502–7.e1-2. doi: 10.1016/j.trsl.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 52.Polyzos NP, Nwoye M, Corona R, Blockeel C, Stoop D, Haentjens P, et al. Live birth rates in Bologna poor responders treated with ovarian stimulation for IVF/ICSI. Reprod Biomed Online. 2014;28:469–74. doi: 10.1016/j.rbmo.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 53.Ubaldi FM, Rienzi L, Ferrero S, Baroni E, Sapienza F, Cobellis L, et al. Management of poor responders in IVF. Reprod Biomed Online. 2005;10:235–46. doi: 10.1016/s1472-6483(10)60946-7. [DOI] [PubMed] [Google Scholar]
- 54.Loutradis D, Drakakis P, Vomvolaki E, Antsaklis A. Different ovarian stimulation protocols for women with diminished ovarian reserve. J Assist Reprod Genet. 2007;24:597–611. doi: 10.1007/s10815-007-9181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ubaldi F, Vaiarelli A, D’Anna R, Rienzi L. Management of poor responders in IVF: Is there anything new? Biomed Res Int 2014. 2014 doi: 10.1155/2014/352098. 352098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mochtar MH, Van der Veen, Ziech M, van Wely M. Recombinant luteinizing hormone (rLH) for controlled ovarian hyperstimulation in assisted reproductive cycles. Cochrane Database Syst Rev. 2007;18(2):CD005070. doi: 10.1002/14651858.CD005070.pub2. [DOI] [PubMed] [Google Scholar]
- 57.Madani T, Mohammadi Yeganeh L, Khodabakhshi S, Akhoond MR, Hasani F. Efficacy of low dose hCG on oocyte maturity for ovarian stimulation in poor responder women undergoing intracytoplasmic sperm injection cycle: A randomized controlled trial. J Assist Reprod Genet. 2012;29:1213–20. doi: 10.1007/s10815-012-9854-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Polyzos NP, De Vos M, Corona R, Vloeberghs V, Ortega-Hrepich C, Stoop D, et al. Addition of highly purified HMG after corifollitropin alfa in antagonist-treated poor ovarian responders: A pilot study. Hum Reprod. 2013;28:1254–60. doi: 10.1093/humrep/det045. [DOI] [PubMed] [Google Scholar]
- 59.Kansal Kalra S, Ratcliffe S, Gracia CR, Martino L, Coutifaris C, Barnhart KT. Randomized controlled pilot trial of luteal phase recombinant FSH stimulation in poor responders. Reprod Biomed Online. 2008;17:745–50. doi: 10.1016/s1472-6483(10)60400-2. [DOI] [PubMed] [Google Scholar]
- 60.Padilla SL, Dugan K, Maruschak V, Shalika S, Smith RD. Use of the flare-up protocol with high dose human follicle stimulating hormone and human menopausal gonadotropins for in vitro fertilization in poor responders. Fertil Steril. 1996;65:796–9. doi: 10.1016/s0015-0282(16)58216-8. [DOI] [PubMed] [Google Scholar]
- 61.Griesinger G, Diedrich K, Tarlatzis BC, Kolibianakis EM. GnRH-antagonists in ovarian stimulation for IVF in patients with poor response to gonadotrophins, polycystic ovary syndrome, and risk of ovarian hyperstimulation: A meta-analysis. Reprod Biomed Online. 2006;13:628–38. doi: 10.1016/s1472-6483(10)60652-9. [DOI] [PubMed] [Google Scholar]
- 62.Pu D, Wu J, Liu J. Comparisons of GnRH antagonist versus GnRH agonist protocol in poor ovarian responders undergoing IVF. Hum Reprod. 2011;26:2742–9. doi: 10.1093/humrep/der240. [DOI] [PubMed] [Google Scholar]
- 63.Feldman B, Seidman DS, Levron J, Bider D, Shulman A, Shine S, et al. In vitro fertilization following natural cycles in poor responders. Gynecol Endocrinol. 2001;15:328–34. [PubMed] [Google Scholar]
- 64.Schimberni M, Morgia F, Colabianchi J, Giallonardo A, Piscitelli C, Giannini P, et al. Natural-cycle in vitro fertilization in poor responder patients: A survey of 500 consecutive cycles. Fertil Steril. 2009;92:1297–301. doi: 10.1016/j.fertnstert.2008.07.1765. [DOI] [PubMed] [Google Scholar]
- 65.Polyzos NP, Blockeel C, Verpoest W, De Vos M, Stoop D, Vloeberghs V, et al. Live birth rates following natural cycle IVF in women with poor ovarian response according to the Bologna criteria. Hum Reprod. 2012;27:3481–6. doi: 10.1093/humrep/des318. [DOI] [PubMed] [Google Scholar]
- 66.Elizur SE, Aslan D, Shulman A, Weisz B, Bider D, Dor J. Modified natural cycle using GnRH antagonist can be an optional treatment in poor responders undergoing IVF. J Assist Reprod Genet. 2005;22:75–9. doi: 10.1007/s10815-005-1496-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kedem A, Tsur A, Haas J, Yerushalmi GM, Hourvitz A, Machtinger R, et al. Is the modified natural in vitro fertilization cycle justified in patients with “genuine” poor response to controlled ovarian hyperstimulation? Fertil Steril. 2014;101:1624–8. doi: 10.1016/j.fertnstert.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 68.Lainas TG, Sfontouris IA, Venetis CA, Lainas GT, Zorzovilis IZ, Tarlatzis BC, et al. Live birth rates after modified natural cycle compared with high-dose FSH stimulation using GnRH antagonists in poor responders. Hum Reprod. 2015;30:2321–30. doi: 10.1093/humrep/dev198. [DOI] [PubMed] [Google Scholar]
- 69.Polyzos NP, Drakopoulos P, Tournaye H. Modified natural cycle IVF for poor ovarian responders: Rethink before concluding. Hum Reprod. 2016;31:221–2. doi: 10.1093/humrep/dev272. [DOI] [PubMed] [Google Scholar]
- 70.Jovanovic VP, Kort DH, Guarnaccia MM, Sauer MV, Lobo RA. Does the addition of clomiphene citrate or letrazole to gonadotropin treatment enhance the oocyte yield in poor responders undergoing IVF? J Assist Reprod Genet. 2011;28:1067–72. doi: 10.1007/s10815-011-9643-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.al-Mizyen E, Sabatini L, Lower AM, Wilson CM, al-Shawaf T, Grudzinskas JG. Does pretreatment with progestogen or oral contraceptive pills in low responders followed by the GnRHa flare protocol improve the outcome of IVF-ET? J Assist Reprod Genet. 2000;17:140–6. doi: 10.1023/A:1009462004650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hauzman EE, Zapata A, Bermejo A, Iglesias C, Pellicer A, Garcia-Velasco JA. Cycle scheduling for in vitro fertilization with oral contraceptive pills versus oral estradiol valerate: A randomized, controlled trial. Reprod Biol Endocrinol. 2013;11:96. doi: 10.1186/1477-7827-11-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gleicher N, Barad DH. Dehydroepiandrosterone (DHEA) supplementation in diminished ovarian reserve (DOR) Reprod Biol Endocrinol. 2011;9:67. doi: 10.1186/1477-7827-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jirge PR, Chougule SM, Gavali VG, Bhomkar DA. Impact of dehydroepiandrosterone on clinical outcome in poor responders: A pilot study in women undergoing in vitro fertilization, using bologna criteria. J Hum Reprod Sci. 2014;7:175–80. doi: 10.4103/0974-1208.142477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bosdou JK, Venetis CA, Dafopoulos K, Zepiridis L, Chatzimeletiou K, Anifandis G, et al. Transdermal testosterone pretreatment in poor responders undergoing ICSI: A randomized clinical trial. Hum Reprod. 2016;31:977–85. doi: 10.1093/humrep/dew028. [DOI] [PubMed] [Google Scholar]
- 76.Nagels HE, Rishworth JR, Siristatidis CS, Kroon B. Androgens (dehydroepiandrosterone or testosterone) for women undergoing assisted reproduction. Cochrane Database Syst Rev. 2015;11:CD009749. doi: 10.1002/14651858.CD009749.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Duffy JM, Ahmad G, Mohiyiddeen L, Nardo LG, Watson A. Growth hormone for in vitro fertilization. Cochrane Database Syst Rev. 2010;20(1):CD000099. doi: 10.1002/14651858.CD000099.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Frattarelli JL, McWilliams GD, Hill MJ, Miller KA, Scott RT., Jr Low-dose aspirin use does not improve in vitro fertilization outcomes in poor responders. Fertil Steril. 2008;89:1113–7. doi: 10.1016/j.fertnstert.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 79.Harris ID, Missmer SA, Hornstein MD. Poor success of gonadotropin-induced controlled ovarian hyperstimulation and intrauterine insemination for older women. Fertil Steril. 2010;94:144–8. doi: 10.1016/j.fertnstert.2009.02.040. [DOI] [PubMed] [Google Scholar]
- 80.Kaser DJ, Goldman MB, Fung JL, Alper MM, Reindollar RH. When is clomiphene or gonadotropin intrauterine insemination futile. Results of the fast track and standard treatment trial and the forty and over treatment trial, two prospective randomized controlled trials? Fertil Steril. 2014;102:1331–7.e1. doi: 10.1016/j.fertnstert.2014.07.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Virant-Klun I. Postnatal oogenesis in humans: A review of recent findings. Stem Cells Cloning. 2015;8:49–60. doi: 10.2147/SCCAA.S32650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tremellen K, Savulescu J. Ovarian reserve screening: A scientific and ethical analysis. Hum Reprod. 2014;29:2606–14. doi: 10.1093/humrep/deu265. [DOI] [PubMed] [Google Scholar]


