Abstract
Background
Pediatric obsessive-compulsive disorder (OCD) is a debilitating psychological anxiety disorder. Cognitive-behavioral therapy (CBT) has been shown to be an effective therapy for OCD, but the evaluation results from various studies are inconsistent and incomprehensive. This meta-analysis examined the efficacy of CBT in treatment of OCD.
Material/Methods
A literature search identified 13 studies that met the inclusion criteria. The efficacy of CBT on OCD was evaluated by comparing post-treatment and pre-treatment Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) scores. Weighted mean difference (WMD) was generated for the statistical evaluation. Heterogeneity was evaluated by I2 index.
Results
A decrease in WMD and a statistical significance (p<0.0001) in both CY-BOCS and CGI scores between pre- and post-CBT treatment were observed in both overall database (−11.73) and USA subgroup (−11.371), which indicates a dramatic relief of OCD symptoms after CBT treatment. Heterogeneity was detected in overall database and USA subgroup, which resulted in an application of the random-effects model to both groups. Publication bias was examined by both Begg’s funnel plot and Egger’s test and no publication bias was detected.
Conclusions
We concluded that CBT is efficacious in treating children’s OCD.
MeSH Keywords: Cognitive Therapy, Meta-Analysis, Obsessive-Compulsive Disorder
Background
Obsessive-compulsive disorder (OCD) is a complex psychological disorder that is characterized by recurrent obsessions and/or compulsions. Obsessions are defined as intrusive, repetitive thoughts, images, or impulses. Compulsions are purposeful, repetitive, overt and covert behaviors or rituals performed in an effort to relieve obsessional distress [1]. OCD affects approximately 1% to 4% of children and adolescents [1,2], which causes marked distress and interferes with daily functioning [3]. As reported, the age of onset for pediatric OCD varies considerably; early onset as early as 3 years of age has been reported [1], but the mean age of onset is around 10.4 years (range, 6.9–12.5 years) [1]. Pediatric OCD is often associated with other psychological disorders, such as tics, attention deficit/hyperactivity disorder (ADHD), depression, multiple anxiety disorders, eating disorders, pervasive developmental disorders, and externalizing behavioral disorders [1]. The comorbidity has been associated with a lower treatment response and a greater percentage of relapse after treatment, both in medication and psychological interventions [4]. Thus, the occurrence of OCD and its comorbidity during childhood is very pernicious in its impact in disrupting functions across multiple domains, including family relationships and everyday life routines, school functioning, and peer relationships, and compounding its negative impact over time to derail normal development, which leads to lifelong suffering if left untreated [5–7]. Thus, the severe consequences of OCD in lives of children and adolescents have motivated physicians and researchers to improve pharmacological and psychological interventions, as well as to develop new assessment instruments.
Cognitive-behavioral therapy (CBT) is the only psychological therapy that has been demonstrated to be effective in treating pediatric OCD in many studies [1,8]. CBT refers to a class of interventions that were developed from the basic premise that psychological disorders are maintained by cognitive and behavioral factors. CBT for OCD in youth involves 4 primary components: psycho-education, cognitive training, mapping of OCD, and exposure with response prevention [9], which aims to weaken the association between obsessions and increased anxiety, and between compulsions and the relief of anxiety. Despite the positive outcome of CBT on OCD treatment, the results delivered by current articles are inconsistent and not comprehensive, mainly because of the huge variations among studies in sample sizes, various ethnic groups, and different outcome assessment tools used. To generate a more comprehensive evaluation of the efficacy of CBT on the treatment of OCD, we carried out this meta-analysis covering 13 studies and 415 OCD patients.
Material and Methods
Literature search
Published reports were searched in the NCBI Global database, including PubMed, PubMed Central, and Google Scholar, using “children’s obsessive-compulsive disorder”, “pediatric OCD”, “cognitive-behavioral therapy”, and “CBT” as key words. Reference lists of articles that were included for review were also examined to further identify reports that were potentially relevant. Unpublished studies were not considered.
Inclusion and exclusion criteria
Studies were included if they: (1) included only children and/or adolescents (age <18) with a primary diagnosis of OCD; (2) had enough participants (10 or more); (3) the participants were only treated with CBT, without any pharmacological interventions; (4) used randomization; (5) used at least 1 reliable and valid measurement for primary outcome; and (6) presented sufficient information to enable calculation of effect sizes.
Exclusion criteria were: (1) books and other literature that were not therapy evaluation studies; (2) studies of which the primary goal was not the investigation of the efficacy of CBT in OCD; and (3) articles without comprehensive statistical information or without the retrievable original data. When the studies that were covered in different articles overlapped, only the ones showing the most extensive results were included in this study.
Two investigators independently extracted the data from each eligible study. Disagreements between reviewers were resolved by discussion and a consensus was reached on all items.
Effect size calculation
An effect size θ based on means usually considers the standardized mean difference between 2 populations. In the equation: , where μ1 is the mean for population, μ2 is the mean for the other population, and σ is a standard deviation (SD) based on either or both populations. For clinical trials covered in our meta-analysis, effect sizes were calculated within each trial. Similar to the 2-sample Cohen’s d, the effect size is an estimate of the true difference between pre-treatment and post-treatment outcome divided by SD.
Data collection and synthesis
The primary outcome measure of interest was the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS), which is a psychometrically sound [10], clinician-rated, semi-structured interview assessing the severity of obsessive-compulsive symptoms. The CY-BOCS rates the severity of obsessions and compulsions across 5 items each and provides a total severity score. The score of different scales reflects a difference in the severity of symptoms: 0–7 is sub-clinical, 8–15 is mild, 16–23 is moderate, 24–31 is severe, and 32–40 is extreme. Patients with a mild range or higher score are more likely to experience a significant negative impact on quality of life and should receive professional help in alleviating the symptoms.
The Clinical Global Impression – Severity (CGI-S) score as a secondary outcome measurement was also assessed among studies for which CGI-S score was available. CGI-S is a single-item 7-point clinician rating of severity of OCD. The CGI-S allows the clinician to rate the global severity of anxiety, with scores ranging from 0 (“no illness”) to 6 (“serious illness”), and were completed at baseline and post-treatment. In our analysis, a decrease of CGI-S indicates improvement of the condition. For continuous variables, the mean, standard deviation, and sample size in each group are known. The weight given to each study (how much influence of each study has on the overall analysis result) is determined by the precision of its estimate of effect [11].
Weighted mean difference (WMD) will then be calculated with groups before and after an intervention. In this case, WMD was generated to test the efficacy of CBT, which was calculated by comparing mean and standard deviation of pre- and post-treatment CY-BOCS score and CGI-S score. A positive WMD indicates an increased CY-BOCS or CGI-S score for post-treatment compared to the pre-treatment score. On the other hand, a negative WMD shows a decrease in CY-BOCS or CGI-S score after treatment, indicating an improvement in OCD symptoms. For each study, mean value and standard deviation of CY-BOCS score and the number of patients involved in the trail were used as pooled data.
Statistics
The statistical analysis of the pooled data was conducted using STATA 12.0 (Stata Corp LP, College Station, TX, USA). P-value <0.05 was considered as statistically significant. In addition to the overall database, a subgroup that covered all studies performed in USA was created. For continuous data, inverse variance method should be applied. The Mantel-Haenszel (M-H) fixed-effects model should be used to analyze databases without significant heterogeneity. On the other hand, DerSimonian and Laird (D-L) random-effected model should be used for databases with evident heterogeneity. In our analysis, the heterogeneity between studies was tested using I2 index, with the equation of , where Q is statistical data and DF is its freedom. The higher the I2, the more significant the heterogeneity is. Values of I2 as 25%, 50% and 75% represent low, medium, and high heterogeneity, respectively. When I2 ≤50%, there is no significant heterogeneity between pooled data. In this meta-analysis, the M-H fixed-effects model was used to test the heterogeneity first, and then different models were chosen based on the results. WMD was calculated with each model within 95% confidence intervals. Forest plots were generated to evaluate OR and summarize the results. To evaluate publication bias, Begg’s funnel plots were generated based on the analysis results and database size, and Egger’s test was also performed.
Results
Study characteristics
A total of 118studies were retrieved after the first search, and 105 of them were excluded from the analysis for reasons listed in the Methods section and as shown in the data collection flow chart of Figure 1. As a result, 13 studies [9,12–23] that met the inclusion criteria were included in the final meta-analysis, in which 415 OCD patients were covered. Table 1 shows the characteristics of all studies, including the age range and the countries of the patients employed in each trial, as well as year published.
Figure 1.
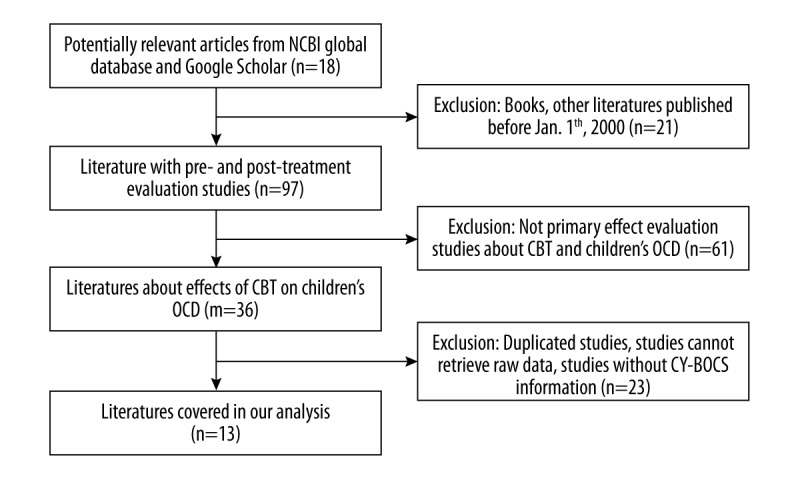
Flow chart of selection of studies and specific reasons for exclusion from the meta-analysis. We identified 118 studies for the first-round exclusion, out of which 13 studies were included in the final meta-analysis.
Table 1.
Pooled Data for evaluation of CY-BOCS score for patients with CBT.
| Study | Year | Age | Pre-treatment | Post-treatment | ES | Country | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Std | n | Mean | Std | n | |||||
| Benazon, 2002 | 2002 | 8–17 | 22.56 | 6.45 | 16 | 11.79 | 6.58 | 16 | 1.65 | USA |
| Farrell, 2011 | 2011 | 9–13 | 20.45 | 6.82 | 43 | 12.43 | 8.18 | 43 | 0.92 | Australia |
| Farrell, 2010 | 2010 | 10–15 | 23.54 | 5.79 | 35 | 10.06 | 6.82 | 35 | 2.13 | Australia |
| Franklin, 2011 | 2011 | 7–17 | 26.08 | 5.12 | 42 | 25.45 | 5.18 | 42 | 0.85 | USA |
| Freeman, 2014 | 2014 | 5–8 | 25.13 | 4.46 | 63 | 12.5 | 2.4 | 63 | 0.84 | USA |
| Keeley, 2011 | 2011 | 10–16 | 25.73 | 4.59 | 25 | 8.27 | 7.19 | 25 | 2.89 | USA |
| Lenhard, 2014 | 2014 | 11–16 | 21.33 | 3.54 | 21 | 12.05 | 4.51 | 21 | 2.29 | Sweden |
| POTS, 2004 | 2004 | 7–17 | 26 | 4.6 | 28 | 14 | 9.5 | 28 | 0.97 | USA |
| Rudy, 2014 | 2014 | 10–16 | 26.54 | 4.54 | 78 | 10.85 | 6.74 | 78 | 2.73 | USA |
| Storch, 2013 | 2013 | 7–17 | 23.64 | 4.48 | 14 | 15.43 | 9.72 | 14 | 1.01 | USA |
| Storch, 2011 | 2011 | 7–16 | 25.38 | 3.61 | 16 | 11.13 | 10.53 | 16 | 1.36 | USA |
| Storch, 2006 | 2006 | 7–17 | 25.9 | 5.6 | 20 | 9.5 | 6.9 | 20 | 2.62 | USA |
| Whiteside, 2014 | 2014 | 7–18 | 25 | 5.55 | 14 | 15.67 | 5.24 | 14 | 1.37 | USA |
Evaluation of heterogeneity
A heterogeneity analysis was conducted to test the variation in study outcomes between studies. I2 index was calculated in this study and significant heterogeneity was detected in both overall database (I2=91.9%) and USA subgroup (I2=93.5%). Thus, the random-effects model, as a more natural choice that allows the study outcomes to vary in a normal distribution between studies, was applied to both groups.
Quantitative synthesis
The meta-analysis was carried out on both the overall database and the USA subgroup. The pooled data was made up of mean value and standard deviation of the CY-BOCS scores for OCD patients before and after CBT treatments, the total number of patients employed in each trial, and the calculated effect sizes. The 95% confidence interval for effect sizes of the CBT were relatively large and did not contain zero across all 13 studies covered in this meta-analysis, indicating that the effect of CBT on OCD symptoms severity was significantly greater than zero. WMD was calculated and Forest plots of WMD between pre- and post-treatment of CBT on children’s OCD for either entire database or USA subgroup were generated to summarize the results (Figure 2). Significant difference was detected in the CY-BOCS scores between pre-treatment and post-treatment data as judged by WMD. Overall WMD in the entire database was estimated to be −11.371 [95% CI: −14.11 to −8.631, p<0.0001], which indicates that the post-treatment CY-BOCS score decreased by more than 11 compared to the pre-treatment score, demonstrating a significant relief in the OCD symptoms after CBT treatment. Similarly, the WMD in the USA subgroup was estimated to be −11.73 [95% CI: −15.25 to −8.21, p<0.0001], as shown in Table 2 and Figure 3, which also suggests a dramatic efficacy of CBT in improving OCD symptoms of patients in USA.
Figure 2.
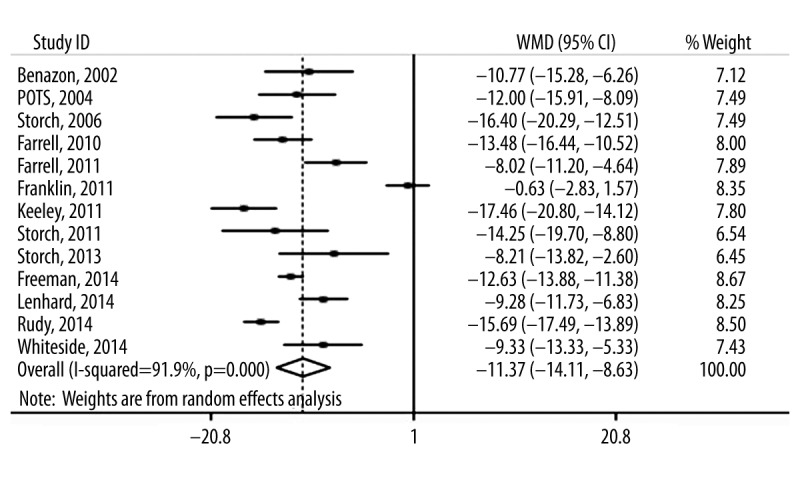
Forest plot of WMD of CY-BOCS score between pre- and post-treatment of CBT on children’s OCD for entire database.
Table 2.
Meta-analysis for overall database and USA subgroup.
| Period | Analysis method | Heterogeneity | WMD | Publication bias | |||||
|---|---|---|---|---|---|---|---|---|---|
| I2 (%) | p-value | Overall | Lower | Upper | p-value | Begg | Egger | ||
| Overall | Random | 91.9 | 0 | −11.37 | −14.11 | −8.63 | <0.0001 | 0.3 | 0.974 |
| USA | Random | 93.5 | 0 | −11.73 | −15.25 | −8.21 | <0.0001 | 0.049 | 0.953 |
Figure 3.
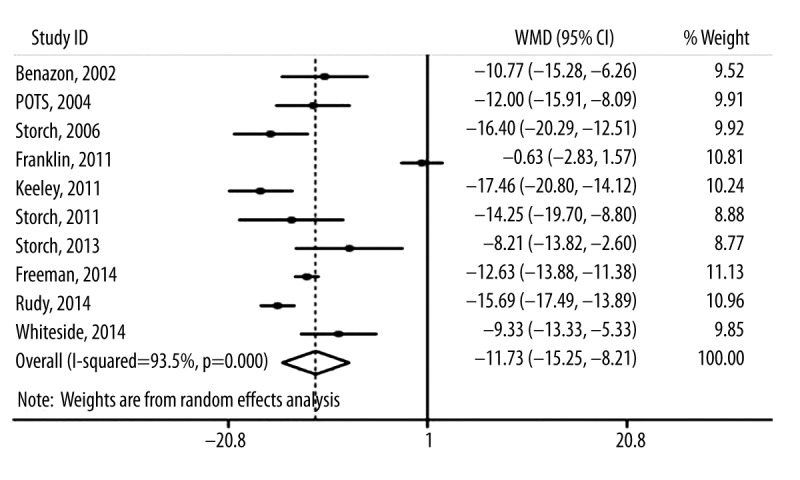
Forest plot of WMD of CY-BOCS score between pre- and post-treatment of CBT on children’s OCD for USA subgroup.
A secondary outcome measurement using CGI-S score was also performed. The pooled data are shown in Table 3, and the results are given in Table 4 and Figure 4. A significant difference was detected in the CGI-S scores between pre-treatment and post-treatment data as judged by WMD, which was estimated to be −2.318 [95% CI: −2.808 to −1.827, p<0.0001], as shown in Table 4 and Figure 4.
Table 3.
Pooled Data for evaluation of CGI-S score for patients with CBT.
| Study | Year | Age | Pre-treatment | Post-treatment | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | Std | n | Mean | Std | n | |||
| Rudy, 2014a | 2014 | 13.2 | 4.16 | 0.76 | 19 | 1.21 | 0.71 | 19 |
| Rudy, 2014b | 2014 | 13.2 | 4.1 | 0.61 | 30 | 2.03 | 0.93 | 30 |
| Rudy, 2014c | 2014 | 13.2 | 4.69 | 0.6 | 29 | 2.14 | 1.09 | 29 |
| Storch, 2013 | 2013 | 7~17 | 4.63 | 0.72 | 16 | 3.37 | 0.89 | 16 |
| Storch, 2011 | 2011 | 7~16 | 3.75 | 0.93 | 16 | 1.56 | 1.75 | 16 |
| Storch, 2006 | 2006 | 7~17 | 4.2 | 0.8 | 20 | 1.4 | 0.9 | 20 |
Table 4.
Meta-analysis for overall database on CGI-S score.
| Analysis method | Heterogeneity | WMD | Publication bias | |||||
|---|---|---|---|---|---|---|---|---|
| I2 (%) | p-value | Overall | Lower | Upper | p-value | Begg | Egger | |
| Random | 81 | 0 | −2.318 | −2.808 | −1.827 | <0.0001 | 1 | 0.8 |
Figure 4.
Forest plot of WMD of CGI-S score between pre- and post-treatment of CBT on children’s OCD for studies included.
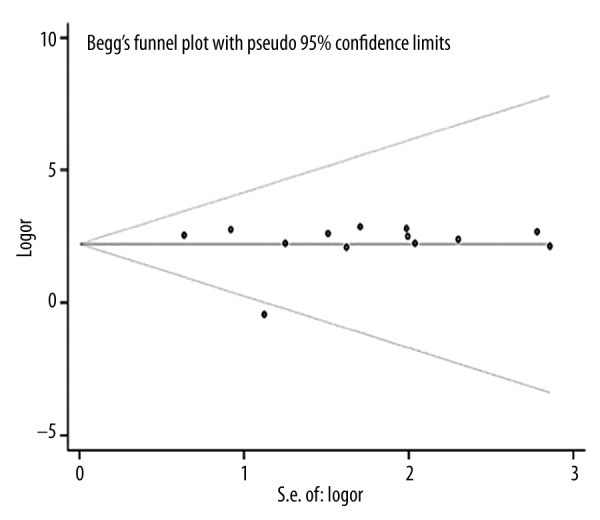
Publication bias
It has been suggested that a potential discrepancy could exist between the number of published trials and the total number of studies that has been carried out. Thus, some non-significant studies could have been missed in a meta-analysis of published studies, so the overall effect size could be overestimated [24]. Therefore, the publication bias of the present meta-analysis was examined and both Begg’s and Egger’s tests were performed to the overall database, as well as the USA subgroup. The funnel plots for either overall database or USA subgroup were also generated. No publication bias was observed among these studies as judged by the results of funnel plots shown in Figures 5–7.
Figure 5.
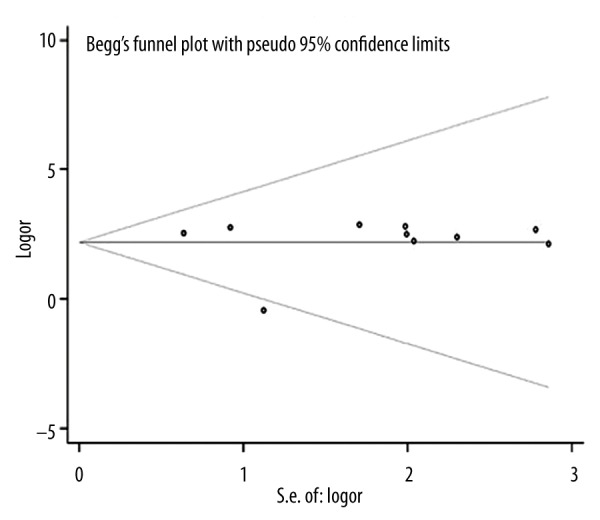
Funnel plot of entire database.
Figure 6.
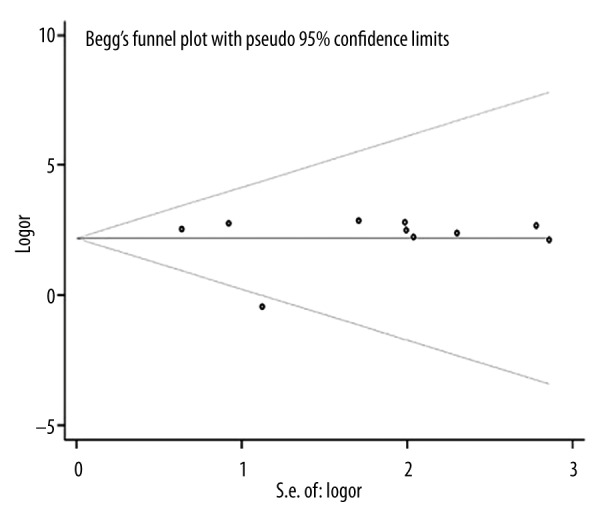
Funnel plot of USA subgroup.
Figure 7.
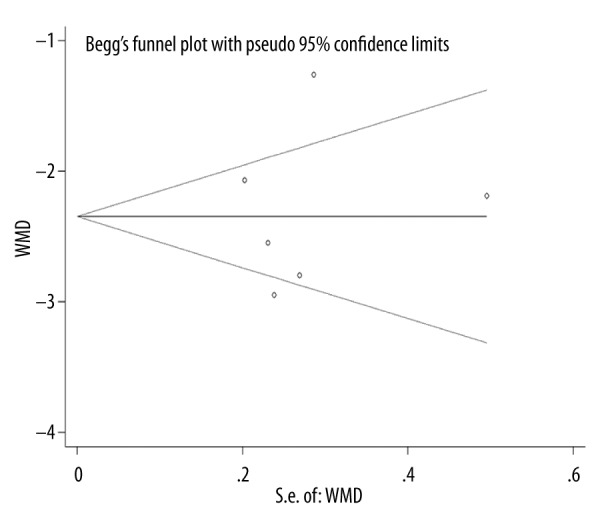
Funnel plot of studies with CGI-S score.
Discussion
In the present study, efficacy of CBT for treatment of pediatric OCD was investigated by a meta-analysis, in which 13 studies and 415 OCD patients were included. The results showed that there was a significant decrease in WMD in overall database (−11.371, p<0.0001) and USA subgroup (−11.73, p<0.0001), and the effect size is large across all studies included, suggesting that OCD symptoms were significantly relieved after CBT treatment. In addition, no publication bias was observed.
Findings from the present study substantiated the results from previous meta-analyses showing that CBT is efficacious in treating pediatric and adult OCD [25–31]. Interestingly, the efficacy for OCD treatment was compared between CBT and certain pharmacological therapeutic strategies, such as the use of serotonergic antidepressants in some of these studies. The results of these comparisons demonstrated that CBT out-performs pharmacotherapy by showing a greater effect size and better improvement in clinical symptoms [25–28]. In addition, potential adverse effects generated by pharmacotherapy still remain a major concern for clinicians when considering the optimal therapeutic strategy for pediatric OCD patients [32]. Thus, CBT is regarded as the first-line therapeutic strategy for pediatric OCD. This was one of the major motivations for us to focus on the efficacy of CBT for OCD in this meta-analysis. One of the merits of the present study is that a number of very recent randomized clinical trials [15,17,19,20] have been for the first time included in our meta-analysis, which made the results very up-to-date. Another merit of the present study is that in addition to the overall database, a meta-analysis was also carried out on the 10 studies that focused on USA patients as a subgroup. Thus, the finding from the present study will definitely add new supplementary information to the evidence base of CBT for pediatric OCD treatment, and contribute to the translation of efficacy research into clinical community practice. A strength of the present study is that to minimize the bias caused by a single assessment tool, we used not only CY-BOCS score as a primary outcome measurement, but also CGI score as a secondary tool to assess the outcome of certain studies.
A major limitation of the present study is that although the findings suggest that CBT is efficacious for treatment of pediatric OCD, many of the studies included were uncontrolled trials that did not have controls for effects of time and other nonspecific factors, which might also contribute to the relief of symptoms.
Conclusions
A significant difference (a decreased WMD) in CY-BOCS and CGI-S score between pre-treatment and post-treatment was observed in the overall database and USA subgroup, suggesting that CBT is efficacious in treating pediatric OCD.
Footnotes
Source of support: Self financing
Conflict of interest declaration
No conflict of interest.
References
- 1.Turner CM. Cognitive-behavioural theory and therapy for obsessive-compulsive disorder in children and adolescents: current status and future directions. Clin Psychol Rev. 2006;26:912–38. doi: 10.1016/j.cpr.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Douglass HM, Moffitt TE Dar R. et al. Obsessive-compulsive disorder in a birth cohort of 18-year-olds: prevalence and predictors. J Am Acad Child Adolesc Psychiatry. 1995;34:1424–31. doi: 10.1097/00004583-199511000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Shaffer D, Gould MS, Fisher P, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53:339–48. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- 4.Li Z, Ji W, Li D, et al. Microstructural abnormality in left nucleus accumbens predicts dysfunctional beliefs in treatment-resistant obsessive-compulsive disorder. Med Sci Monit. 2014;20:2275–82. doi: 10.12659/MSM.891102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper M. Obsessive-compulsive disorder: effects on family members. Am J Orthopsychiatry. 1996;66:296–304. doi: 10.1037/h0080180. [DOI] [PubMed] [Google Scholar]
- 6.Toro J, Cervera M, Osejo E, Salamero M. Obsessive-compulsive disorder in childhood and adolescence: a clinical study. J Child Psychol Psychiatry. 1992;33:1025–37. doi: 10.1111/j.1469-7610.1992.tb00923.x. [DOI] [PubMed] [Google Scholar]
- 7.Allsopp M, Verduyn C. Adolescents with obsessive-compulsive disorder: a case note review of consecutive patients referred to a provincial regional adolescent psychiatry unit. J Adolesc. 1990;13:157–69. doi: 10.1016/0140-1971(90)90005-r. [DOI] [PubMed] [Google Scholar]
- 8.Freeman JB, Choate-Summers ML, Moore PS, et al. Cognitive behavioral treatment for young children with obsessive-compulsive disorder. Biol Psychiatry. 2007;61:337–43. doi: 10.1016/j.biopsych.2006.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benazon NR, Ager J, Rosenberg DR. Cognitive behavior therapy in treatment-naive children and adolescents with obsessive-compulsive disorder: an open trial. Behav Res Ther. 2002;40:529–39. doi: 10.1016/s0005-7967(01)00064-x. [DOI] [PubMed] [Google Scholar]
- 10.Scahill L, Riddle MA, McSwiggin-Hardin M, et al. Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36:844–52. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Guy W. ECDEU Assessment Manual for Psychopharmacology: 1976. National Institute of Mental Health; 1976. [Google Scholar]
- 12.Farrell L, Waters A, Milliner E, Ollendick T. Comorbidity and treatment response in pediatric obsessive-compulsive disorder: a pilot study of group cognitive-behavioral treatment. Psychiatry Res. 2012;199:115–23. doi: 10.1016/j.psychres.2012.04.035. [DOI] [PubMed] [Google Scholar]
- 13.Farrell LJ, Schlup B, Boschen MJ. Cognitive-behavioral treatment of childhood obsessive-compulsive disorder in community-based clinical practice: clinical significance and benchmarking against efficacy. Behav Res Ther. 2010;48:409–17. doi: 10.1016/j.brat.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Franklin ME, Sapyta J, Freeman JB, et al. Cognitive behavior therapy augmentation of pharmacotherapy in pediatric obsessive-compulsive disorder: the Pediatric OCD Treatment Study II (POTS II) randomized controlled trial. JAMA. 2011;306:1224–32. doi: 10.1001/jama.2011.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freeman J, Sapyta J, Garcia A, et al. Family-based treatment of early childhood obsessive-compulsive disorder: the Pediatric Obsessive-Compulsive Disorder Treatment Study for Young Children (POTS Jr) – a randomized clinical trial. JAMA Psychiatry. 2014;71:689–98. doi: 10.1001/jamapsychiatry.2014.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keeley ML, Geffken GR, Ricketts E, et al. The therapeutic alliance in the cognitive behavioral treatment of pediatric obsessive-compulsive disorder. J Anxiety Disord. 2011;25:855–63. doi: 10.1016/j.janxdis.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 17.Lenhard F, Vigerland S, Andersson E, et al. Internet-delivered cognitive behavior therapy for adolescents with obsessive-compulsive disorder: an open trial. PLoS One. 2014;9:e100773. doi: 10.1371/journal.pone.0100773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pediatric OCD Treatment Study (POTS) Team. Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: the Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA. 2004;292:1969–76. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- 19.Rudy BM, Lewin AB, Geffken GR, et al. Predictors of treatment response to intensive cognitive-behavioral therapy for pediatric obsessive-compulsive disorder. Psychiatry Res. 2014;220(1–2):433–40. doi: 10.1016/j.psychres.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Storch EA, Bussing R, Small BJ, et al. Randomized, placebo-controlled trial of cognitive-behavioral therapy alone or combined with sertraline in the treatment of pediatric obsessive-compulsive disorder. Behav Res Ther. 2013;51:823–29. doi: 10.1016/j.brat.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Storch EA, Caporino NE, Morgan JR, et al. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Res. 2011;189:407–12. doi: 10.1016/j.psychres.2011.05.047. [DOI] [PubMed] [Google Scholar]
- 22.Storch EA, Geffken GR, Merlo LJ, et al. Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: comparison of intensive and weekly approaches. J Am Acad Child Adolesc Psychiatry. 2007;46:469–78. doi: 10.1097/chi.0b013e31803062e7. [DOI] [PubMed] [Google Scholar]
- 23.Whiteside SP, McKay D, De Nadai AS, et al. A baseline controlled examination of a 5-day intensive treatment for pediatric obsessive-compulsive disorder. Psychiatry Res. 2014;220(1–2):441–46. doi: 10.1016/j.psychres.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 24.Sterling TD. Publication decisions and their possible effects on inferences drawn from tests of significance – or vice versa. Journal of the American Statistical Association. 1959;54:30–34. [Google Scholar]
- 25.Abramowitz JS, Whiteside SP, Deacon BJ. The effectiveness of treatment for pediatric obsessive-compulsive disorder: a meta-analysis. Behavior Therapy. 2005;36:55–63. [Google Scholar]
- 26.Sanchez-Meca J, Rosa-Alcazar AI, Iniesta-Sepulveda M, Rosa-Alcazar A. Differential efficacy of cognitive-behavioral therapy and pharmacological treatments for pediatric obsessive-compulsive disorder: a meta-analysis. J Anxiety Disord. 2014;28:31–44. doi: 10.1016/j.janxdis.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 27.Watson HJ, Rees CS. Meta-analysis of randomized, controlled treatment trials for pediatric obsessive-compulsive disorder. J Child Psychol Psychiatry. 2008;49:489–98. doi: 10.1111/j.1469-7610.2007.01875.x. [DOI] [PubMed] [Google Scholar]
- 28.Romanelli RJ, Wu FM, Gamba R, et al. Behavioral therapy and serotonin reuptake inhibitor pharmacotherapy in the treatment of obsessive-compulsive disorder: a systematic review and meta-analysis of head-to-head randomized controlled trials. Depress Anxiety. 2014;31:641–52. doi: 10.1002/da.22232. [DOI] [PubMed] [Google Scholar]
- 29.Rosa-Alcazar AI, Sanchez-Meca J, Gomez-Conesa A, Marin-Martinez F. Psychological treatment of obsessive-compulsive disorder: a meta-analysis. Clin Psychol Rev. 2008;28:1310–25. doi: 10.1016/j.cpr.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 30.Hofmann SG, Asnaani A, Vonk IJ, et al. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognit Ther Res. 2012;36:427–40. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olatunji BO, Davis ML, Powers MB, Smits JA. Cognitive-behavioral therapy for obsessive-compulsive disorder: a meta-analysis of treatment outcome and moderators. J Psychiatr Res. 2013;47:33–41. doi: 10.1016/j.jpsychires.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 32.Geller DA, Biederman J, Stewart SE, et al. Which SSRI? A meta-analysis of pharmacotherapy trials in pediatric obsessive-compulsive disorder. Am J Psychiatry. 2003;160:1919–28. doi: 10.1176/appi.ajp.160.11.1919. [DOI] [PubMed] [Google Scholar]


