Abstract
Study Design
Cost Effectiveness Analysis
Objective
To examine the cost-effectiveness of operative vs. non-operative treatment of type-II odontoid fractures in patients over 64 years old.
Summary of Background Data
Significant controversy exists regarding the optimum treatment of geriatric patients with type-II odontoid fractures. Operative treatment leads to lower rates of non-union but carries surgical risks. Non-operative treatment does not carry surgical risks but has higher non-union rates.
Methods
A decision-analytic model was created to compare operative and non-operative treatment of type-II odontoid fractures among three age cohorts (65–74, 75–84, over-84) based on expected costs, quality-adjusted life years (QALYs) and incremental cost-effectiveness ratios (cost per QALY gained). Age-specific mortality rates for both treatments, costs for treatment, and complication rates were taken from the literature, and data from 2010 US life tables was used for age-specific life expectancy. Costs of complications were estimated using data obtained at a Level-I trauma center using micro-costing. Sensitivity analyses of all model parameters were conducted.
Results
Among the 65–74 year old cohort, operative treatment was more costly ($53,407 vs. $30,553) and more effective (12.00 vs. 10.11 QALY), with an incremental cost effectiveness ratio (ICER) of $12,078/QALY. Among the 75–84 year old cohort, operative treatment was more costly ($51,308 vs. $29,789) and more effective (6.85 vs. 6.31 QALY), with an ICER of $40,467/QALY. Among the over-84 cohort, operative treatment was dominated by non-operative treatment as it was both more costly ($45,978 vs. $28,872) and less effective (2.48 vs 3.73 QALY). The model was robust to sensitivity analysis across reasonable ranges for utility of union, disutility of complications and delayed surgery, and probabilities of non-union and complications.
Conclusions
Operative treatment is cost-effective in patients age 65–84 when using $100,000/QALY as a benchmark but less effective and more costly than non-operative treatment in patients over age 84 years.
Keywords: Odontoid, Type-2, Fracture, Operative Treatment, Non-Operative Treatment, Cost-Effectiveness Analysis, Geriatric, Sensitivity Analyses, Decision Analyses, Quality-Adjusted Life Years, Incremental Cost Effectiveness Ratio
Introduction
Type-II odontoid fracture is the most common cervical spine fracture in patients 65 years of age or older and is the most common fracture type of the second cervical vertebrae.1,2 The rate of C2 fractures in this population is increasing and has been shown to be growing faster than the growth of the elderly population.3–5 Additionally, a recent study reported that the costs for treating C2 fractures are increasing at a rate that outpaces the growing fracture rate.5 This rise in fracture incidence and cost of treatment has important economic consequences for geriatric healthcare. It is estimated that the annual cost of treating all types of geriatric C2 fractures exceeded $1.5 billion dollars in 2010, with type-II being the most common.5,6
Despite the common occurrence and increasing numbers of these fractures, significant controversy exists as to whether to treat these patients operatively or non-operatively.7 Non-operative treatment options include soft cervical orthosis, rigid cervical orthosis and halo-vest orthosis, while operative options include anterior odontoid osteosynthesis and posterior C1–C2 fusion. Treatment with a cervical orthosis avoids the risks of surgery but is associated with a higher non-union rate, while surgical fixation puts patients at risk for surgical complications but leads to a significantly better union rate.8–12
The objective of this study was to perform an age-specific, cost-effectiveness analysis comparing operative to non-operative treatment of type-II odontoid fractures in patients over age sixty-four.
Materials and Methods
Study Design
This study is a cost effectiveness analysis – a type of economic analysis used to compare the value of an intervention to an alternative.13 Our study compares operative to non-operative treatment of type-II odontoid fractures. A decision tree was constructed to model the possible events after the decision to pursue operative or non-operative management (see Figure 1). Data for the likelihood of mortality, complications, and union or non-union were derived from the literature from a mix of retrospective and prospective studies. Cost data for operative and non-operative treatment was taken from the literature, and the cost for complications was derived from a retrospective patient record analysis of all patients who underwent treatment for a type-II odontoid fracture at a level-1 trauma center in New England for one fiscal year.
Figure 1.
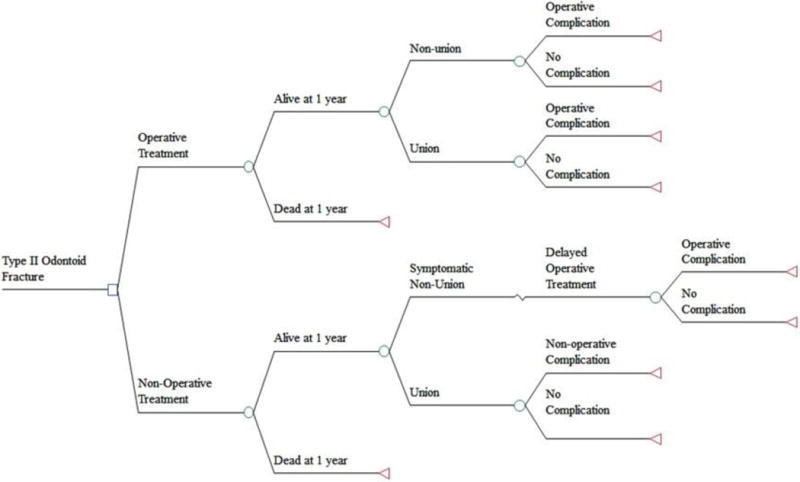
Model showing decision choice and possible complications and outcomes following a geriatric type-II odontoid fracture.
Patient Population
Our patient population includes patients over 64 years old that have experienced a Type II odontoid fracture. We stratified patients into three age cohorts (65–74, 75–84, over-84) based on the convention of recently published studies.3,5,14 Additionally, outcomes have been shown to vary across the different age strata, which could affect the outcomes of a cost-effectiveness analysis.14
Model Structure
A decision tree modeling the possible events after the decision to pursue operative or non-operative management for a type-II odontoid fracture is shown in Figure 1. Subsequent to undergoing operative treatment, patients were either alive or dead at one year. Patients who were alive at one year were classified as having a union or a non-union either with or without surgical complications. The classification of union or non-union followed the parameters determined by each study that the data was extracted from. After non-operative treatment, patients were either alive or dead at one year. Those patients who were alive either went on to union or symptomatic non-union, and those with symptomatic non-union proceeded to delayed operative treatment.9 Patients in this delayed operative treatment cohort were then exposed to the chance of surgical complications at the same rate of those having initially undergone operative treatment. Patients experiencing union after non-operative treatment were then susceptible to non-operative complications.
Utilizing the age-stratified data reported by Schoenfeld et al.,14 the model was run separately for the 65–74 year old, 75–84 year old and over-84 year old cohorts based on projected remaining life expectancy data as provided by the National Center for Health Statistics.15 The model takes into account complications, disutilites, costs, and mortality for one year from the time of injury. After that, due to lack of current literature on long-term outcomes or costs, patients are susceptible to mortality based on age, sex, and race.
Model Parameters
Values and clinically reasonable ranges for mortality, non-union, complications, utilities and life expectancy are shown in Table 1. Probability of 1-year mortality for each age cohort was calculated using the hazard ratios and respective weighting of each cohort within the study by Schoenfeld et al.14 Probabilities of operative and non-operative non-union and complications were based on the AOSpine North America Geriatric Odontoid Fracture Study.9
Utilities of both operative and non-operative complications were estimated based on previously published data.16–25 These were aggregated into a single utility for both operative and non-operative complications, and these values were varied over a wide range during sensitivity analyses. Significant controversy exists regarding the morbidity associated with a “non-union” of a type-II odontoid fracture. It has been reported that pseudarthrosis can lead to decreased function, pain, progressive myelopathy, high cervical-cord injury, and potentially death, though these outcomes are likely quite uncommon.26,27 Other studies have shown no relationship between union status and clinical outcomes, suggesting that non-unions are frequently asymptomatic.28–30 Due to this controversy, a one-year disutility of 0.03 was assigned to the effect of odontoid non-union. This relatively low value was chosen in part due to a publication of the AOSpine study that showed there were no reported differences in outcome between patients treated non-operatively with a union and non-union.31 However, this disutility was an assumption, and, given the uncertainty surrounding the effect of non-union, it was examined across a wide range of values during sensitivity analyses. Delayed surgery due to failed non-operative treatment was assessed a one-year disutility of 0.05. Given the absence of evidence of superiority of operative union over non-operative union, neither event was given a disutility. Remaining years of expected life were calculated for each cohort based on 2010 National Center for Health Statistics for the entire US population.32 For the 65–74 year old cohort the value used was 17.3 years; for 75–84 year old: 10.6 years; and for over-84 years old: 6.5 years (Table 1). Quality Adjusted Life Years (QALYs) were determined as the product of utilities and remaining life expectancy. Future QALYs were discounted at a 3% annual rate.
All costs were in 2013 US dollars. Costs associated with operative and non-operative treatment were taken from a recent study that analyzed the cost of treatment for C2 fractures over a ten year period (Table 2).5 Costs were reported in 2010 US dollars and were converted to 2013 US dollars ($36,688 to $39,195 for operative treatment and $18,013 to $19,244 for non-operative treatment) using the consumer price index calculator.33 This study reported only the average cost of treatment and did not report the cost for complications. Given that this study included all C2 fractures, it is possible that the inclusion of other C2 fractures (i.e. Type III dens fractures, traumatic spondylolisthesis of the axis) affected the cost estimates. However, type-II odontoid fractures are the most common type of C2 fractures, and inclusion of other C2 fractures likely had minimal effect on the cost-estimates.2,6,34 To confirm this, we performed a micro-cost analysis (see below) of Type II dens fracture patients treated operatively and non-operatively at our institution and found very similar costs to those included in the base case scenario. Costs at our institution were $38,923 for operative treatment (vs. $39,195 from Daniels et al.) and $10,953 for non-operative treatment (vs. $19,244 from Daniels et al.). To account for the uncertainty in the cost data, costs were varied over a large range during sensitivity analyses.
Complications costs were estimated using data obtained at a Level-I trauma center in New England during the time period July 2012 – June 2013 (Table 2). All patients with ICD-9 Diagnostic-Related Group 805.02 (closed fracture of second cervical vertebra) during Fiscal Year 2013 were identified. Chart review identified those with Type II dens fractures treated non-operatively who had a complication, and the costs for treating those complications was calculated using Allscripts EPSi cost accounting software (Allscripts Healthcare Solutions, Inc., Chicago, IL). Costs were broken down by technical and professional costs. To estimate the cost of surgical complications, all patients with ICD-9 Diagnostic-Related Group 805.02 (closed fracture of second cervical vertebra) and Current Procedural Terminology (CPT) code 22595 (Arthrodesis, posterior technique, atlas-axis (C1–C2)) during Fiscal Year 2013 were identified. Those patients undergoing this procedure for reasons other than type-II odontoid fracture were removed. Patients sustaining operative complications were identified through chart review, and the average cost of an operative complication was then determined as described above. All costs were incurred within the one-year timeframe of the model and thus were not discounted. All costs are reported in 2013 US dollars. Costs of complications were modeled across a wide-range in sensitivity analyses.
In-line with conventional cost effectiveness-analysis, costs were assigned to the initial treatment selected. For example, patients who initially chose non-operative treatment but subsequently underwent surgery for symptomatic non-union had all costs, surgical and non-operative, assigned to the initial non-operative treatment decision.
Analyses
In the base case analysis for each of the three cohorts, the incremental cost effectiveness ratio (ICER) of operative vs. non-operative treatment was expressed as cost per additional QALY gained. All analyses were performed utilizing TreeAge Pro 2014 software (TreeAge Software Inc., Williamstown, MA). All variables were varied in one-way sensitivity analyses in each of the age cohorts. The ranges for sensitivity analyses were determined based on clinical judgment and three systematic reviews published on this topic8,10,35 (Table 1). Ranges for the costs of treatment were defined as ± 50% of the index cost and ranges for costs of complications as $0 – three times the index cost (Table 2). In sensitivity analyses we used $100,000 per QALY gained as the benchmark for assessing cost-effectiveness.36
Results
Base Case Results
Operative treatment was more costly than non-operative treatment in all age groups ($53,407 vs. $30,553 for 65–74; $51,308 vs. $29,789 for 75–84; and $45,978 vs. $28,872 in over-84), yet was only more effective in the youngest two age groups (12.00 vs. 10.11 QALY for 65–74; 6.85 vs. 6.31 QALY for 75–84; and 2.48 vs 3.73 QALY for over-84). This resulted in an incremental cost effectiveness ratio (ICER), a ratio of change in costs to the change in effects,37 of $12,078 per QALY for operative treatment in 65–74 year olds and an ICER of $40,467 per QALY for operative treatment in 75–84 year olds (Table 3). Operative treatment was dominated by non-operative treatment in patients over-84 years old due to it being more costly and less effective.
Sensitivity Analyses
One-way sensitivity analyses were performed in each age cohort on all variables and demonstrated that our model was most sensitive to changes in the probability of operative and non-operative mortality. The probability of operative mortality was analyzed in the 65–74 year old age cohort and the ICER surpassed $100,000 when the operative mortality rate surpassed 24.3%, and operative treatment was dominated at an operative mortality rate of 25.9%. The ICER surpassed $100,000 in the 75–84 year old age cohort when the operative mortality rate surpassed 28.5%, and operative treatment was dominated at an operative mortality rate of 30.8%. The probability of non-operative mortality was analyzed in the over-84 year old cohort and operative treatment did not become more effective until the non-operative mortality rate exceeded 58.2%, and the ICER didn’t fall under $100,000 until it exceeded 61.7%. The probability of operative mortality needed to be below 36.8% for operative treatment to be more effective and less than 33.2% for the ICER to fall below the $100,000 threshold in this age group.
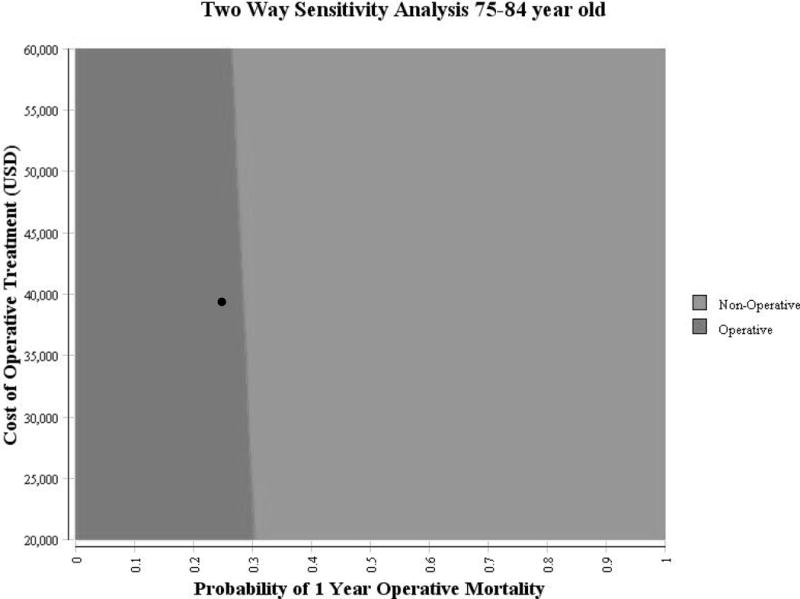
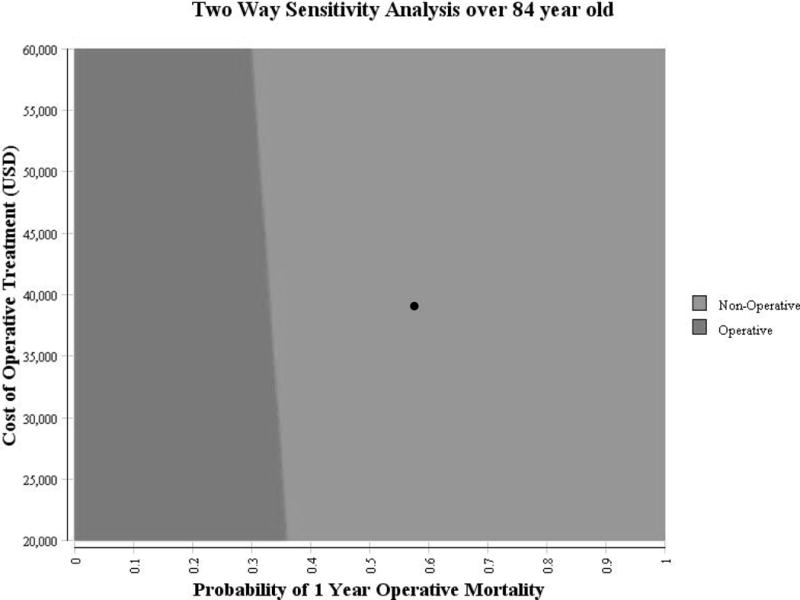
Two-way sensitivity analyses were performed for the probability of operative mortality and the cost of operative treatment for each age cohort with the ICER set at $100,000 – a commonly reported threshold for cost-effectiveness analysis (Figures 2a–2c).36
Figure 2.
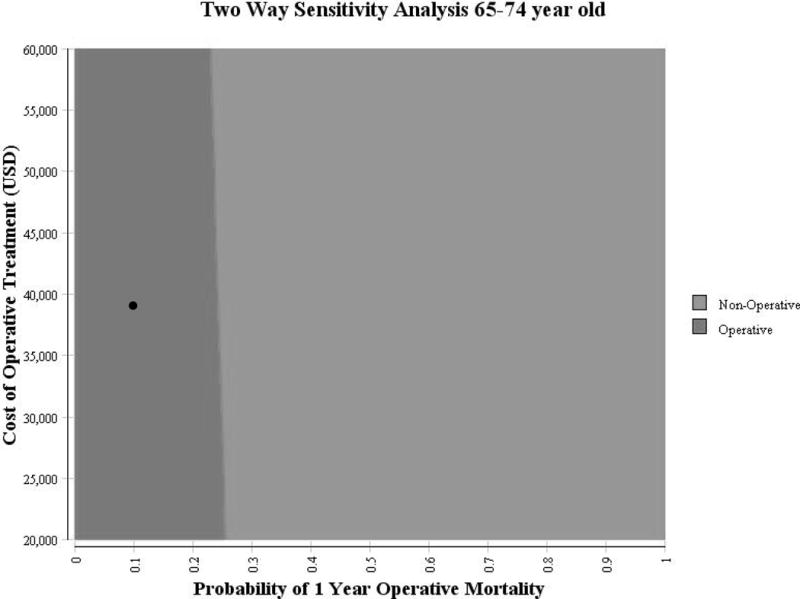
a: Sensitivity analysis on operative mortality and operative cost in 65–74 year old cohort
Two-way sensitivity analysis for probability of 1-year mortality in operative group (x-axis) vs. the cost of operative treatment (y-axis). The boundary between the dark and light region indicates an ICER of $100,000 with the light region favoring non-operative treatment, and the dark region favoring operative treatment. The black circle indicates the base case for the 65–74 year old cohort
b: Sensitivity analysis on operative mortality and operative cost in 75–84 year old cohort
Two-way sensitivity analysis for probability of 1-year mortality in operative group (x-axis) vs. the cost of operative treatment (y-axis). The boundary between the dark and light region indicates an ICER of $100,000 with the light region favoring non-operative treatment, and the dark region favoring operative treatment. The black circle indicates the base case for the 75–84 year old cohort
c: Sensitivity analysis on operative mortality and operative cost in over 84 year old cohort
Two-way sensitivity analysis for probability of 1-year mortality in operative group (x-axis) vs. the cost of operative treatment (y-axis). The boundary between the dark and light region indicates an ICER of $100,000 with the light region favoring non-operative treatment, and the dark region favoring operative treatment. The black circle indicates the base case for the >84 year old cohort
Discussion
This is the first study to evaluate the cost-effectiveness of operative versus non-operative treatment of type 2 odontoid fractures. Regardless of treatment approach, patients tend to do poorly. In a subgroup analysis of the AO Spine study, Fehlings et al. determined that of the 159 patients enrolled in the study, only 44 (27.7%) had a successful outcome.38 The results of our analysis show that the most cost-effective treatment modality is determined by the patient’s age and their associated probability of operative mortality. In the base case analysis, the ICER for surgery vs. non-operative treatment was $12,078 per QALY for the youngest group (65–74), and $40,467 per QALY for the middle group (75–84), both well below the $100,000 per QALY benchmark. In the oldest group (over-84) operative treatment was both more costly and less effective than non-operative care and thus “dominated”. These results suggest that operative treatment is reasonably cost-effective for patients less than 85 years old and generally not indicated for patients over age 84 years.
The model used in the current study was most sensitive to differences in mortality rates. While studies have suggested that surgical treatment decreases mortality, neither of the recent comparative studies on this topic showed that decrease to be statistically significant. The retrospective review by Schoenfeld et al. reported a one-year mortality rate of 21% for patients treated surgically and 36% for non-operative patients (p=0.06, unadjusted analysis).14 The AO Spine prospective cohort study by Vaccaro et al. reported one year mortality rates of 14% for the surgical group and 26% for the non-operative group (p=0.06, unadjusted analysis).9 Given that these were both non-randomized studies with baseline differences between the two groups, it is possible that the mortality advantage associated with surgery was due to confounding factors rather than a protective effect of surgery. Another possibility is that these studies were simply underpowered to detect the mortality difference, and a meta-analysis including these studies did demonstrate a significant survival advantage associated with surgery.39 The true reduction in mortality that can be attributed to surgery will probably remain unknown until a randomized-controlled trial on the topic can be performed.
Limitations
This cost-effectiveness analysis has several limitations. As with most cost-effectiveness analyses, there is some degree of uncertainty regarding the values assigned to the probabilities and utilities. Additionally, the base-case values were derived from non-randomized studies and are thus susceptible to selection bias, however, this was addressed in some studies by adjustment for baseline variables including co-morbidities. It is also possible that participants in the AO Spine study may have been healthier than typical patients as participants in the AO study had to be able to provide consent and participate in study protocols. Neither the AO Spine study, nor other current literature, provide substantial data regarding the long-term effects or costs of the complications associated with each treatment arm or the rate of surgical complications after delayed treatment. Thus, our model did not assess the cost or disutility of complications beyond the first year and proved insensitive to changes in those parameters. Finally, cost data for complications used in this study was obtained via a micro-costing approach. While costs of complications were measured consistently for each treatment arm, our micro-costing approach is potentially biased by regional trends and may have limited generalizability. We have attempted to mitigate these limitations by performing sensitivity analyses over a broad range of values of all variables.
Conclusions and Future Perspectives
Data is mounting to suggest that surgical fixation of Type II dens fractures in the elderly might reduce mortality and improve outcomes in certain subgroups.9,14 The current analysis suggests that the cost-effectiveness of operative treatment of type-II odontoid fractures in the elderly is highly dependent on patient age and the corresponding probability of one-year operative and non-operative mortality. Based on the results of this study, operative treatment is likely cost effective for patients aged 65–84, while for patients older than 84, operative treatment is probably more costly and less effective. This study, like the Cochrane Review by Shears et al.,7 echoes the need for a well-conducted randomized controlled trial to determine the optimal treatment for type-II odontoid fractures in geriatric patients. Such a study would be challenging to perform given the likely difficulty of enrolling patients and the fact that many surgeons feel there is already a lack of equipoise on the topic. In the absence of such a trial, surgeons and patients will need to continue to base their decisions on the observational data available and patients’ preferences for care.
Supplementary Material
Acknowledgments
The manuscript submitted does not contain information about medical device(s)/drug(s). National Institute of Arthritis and Musculoskeletal and Skin Diseases (P60AR062799) funds were received in support of this work. Relevant financial activities outside the submitted work: employment.
Footnotes
Level of Evidence: 2
References
- 1.Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23:38–40. doi: 10.1016/0020-1383(92)90123-a. [DOI] [PubMed] [Google Scholar]
- 2.Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine. 1997;22:1843–52. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 3.Zusman NL, Ching AC, Hart RA, et al. Incidence of second cervical vertebral fractures far surpassed the rate predicted by the changing age distribution and growth among elderly persons in the United States (2005–2008) Spine. 2013;38:752–6. doi: 10.1097/BRS.0b013e31827ab62a. [DOI] [PubMed] [Google Scholar]
- 4.Smith HE, Kerr SM, Fehlings MG, et al. Trends in epidemiology and management of type II odontoid fractures: 20-year experience at a model system spine injury tertiary referral center. Journal of spinal disorders & techniques. 2010;23:501–5. doi: 10.1097/BSD.0b013e3181cc43c7. [DOI] [PubMed] [Google Scholar]
- 5.Daniels AH, Arthur M, Esmende SM, et al. Incidence and cost of treating axis fractures in the United States from 2000 to 2010. Spine. 2014;39:1498–505. doi: 10.1097/BRS.0000000000000417. [DOI] [PubMed] [Google Scholar]
- 6.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. The Journal of bone and joint surgery American volume. 1974;56:1663–74. [PubMed] [Google Scholar]
- 7.Shears E, Armitstead CP. Surgical versus conservative management for odontoid fractures. The Cochrane database of systematic reviews. 2008:CD005078. doi: 10.1002/14651858.CD005078.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harrop JS, Hart R, Anderson PA. Optimal treatment for odontoid fractures in the elderly. Spine. 2010;35:S219–27. doi: 10.1097/BRS.0b013e3181f32716. [DOI] [PubMed] [Google Scholar]
- 9.Vaccaro AR, Kepler CK, Kopjar B, et al. Functional and quality-of-life outcomes in geriatric patients with type-II dens fracture. The Journal of bone and joint surgery American volume. 2013;95:729–35. doi: 10.2106/JBJS.K.01636. [DOI] [PubMed] [Google Scholar]
- 10.Nourbakhsh A, Shi R, Vannemreddy P, et al. Operative versus nonoperative management of acute odontoid Type II fractures: a meta-analysis. Journal of neurosurgery Spine. 2009;11:651–8. doi: 10.3171/2009.7.SPINE0991. [DOI] [PubMed] [Google Scholar]
- 11.Jubert P, Lonjon G, Garreau de Loubresse C. Complications of upper cervical spine trauma in elderly subjects. A systematic review of the literature. Orthopaedics & traumatology, surgery & research: OTSR. 2013;99:S301–12. doi: 10.1016/j.otsr.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Smith HE, Kerr SM, Maltenfort M, et al. Early complications of surgical versus conservative treatment of isolated type II odontoid fractures in octogenarians: a retrospective cohort study. Journal of spinal disorders & techniques. 2008;21:535–9. doi: 10.1097/BSD.0b013e318163570b. [DOI] [PubMed] [Google Scholar]
- 13.Brauer CA, Rosen AB, Olchanski NV, et al. Cost-utility analyses in orthopaedic surgery. The Journal of bone and joint surgery American volume. 2005;87:1253–9. doi: 10.2106/JBJS.D.02152. [DOI] [PubMed] [Google Scholar]
- 14.Schoenfeld AJ, Bono CM, Reichmann WM, et al. Type II odontoid fractures of the cervical spine: do treatment type and medical comorbidities affect mortality in elderly patients? Spine. 2011;36:879–85. doi: 10.1097/BRS.0b013e3181e8e77c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murphy SL, Xu J, Kochanek KD. Deaths: final data for 2010. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2013;61:1–117. [PubMed] [Google Scholar]
- 16.Eckman MH, Falk RH, Pauker SG. Cost-effectiveness of therapies for patients with nonvalvular atrial fibrillation. Archives of internal medicine. 1998;158:1669–77. doi: 10.1001/archinte.158.15.1669. [DOI] [PubMed] [Google Scholar]
- 17.Pohl H, Sonnenberg A, Strobel S, et al. Endoscopic versus surgical therapy for early cancer in Barrett’s esophagus: a decision analysis. Gastrointestinal endoscopy. 2009;70:623–31. doi: 10.1016/j.gie.2008.11.047. [DOI] [PubMed] [Google Scholar]
- 18.Ito K, Shrank WH, Avorn J, et al. Comparative cost-effectiveness of interventions to improve medication adherence after myocardial infarction. Health services research. 2012;47:2097–117. doi: 10.1111/j.1475-6773.2012.01462.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rinfret S, Cohen DJ, Lamas GA, et al. Cost-effectiveness of dual-chamber pacing compared with ventricular pacing for sinus node dysfunction. Circulation. 2005;111:165–72. doi: 10.1161/01.CIR.0000151810.69732.41. [DOI] [PubMed] [Google Scholar]
- 20.Shih V, Chan A, Xie F, et al. Health State Utility Assessment for Breast Cancer. Value in Health Regional Issues. 2012;1:93–7. doi: 10.1016/j.vhri.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Coello R, Charlett A, Wilson J, et al. Adverse impact of surgical site infections in English hospitals. The Journal of hospital infection. 2005;60:93–103. doi: 10.1016/j.jhin.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 22.Shmueli A. Subjective health status and health values in the general population. Medical decision making: an international journal of the Society for Medical Decision Making. 1999;19:122–7. doi: 10.1177/0272989X9901900202. [DOI] [PubMed] [Google Scholar]
- 23.Oostenbrink R, Oostenbrink JB, Moons KG, et al. Cost-utility analysis of patient care in children with meningeal signs. International journal of technology assessment in health care. 2002;18:485–96. [PubMed] [Google Scholar]
- 24.Post PN, Stiggelbout AM, Wakker PP. The utility of health states after stroke: a systematic review of the literature. Stroke; a journal of cerebral circulation. 2001;32:1425–9. doi: 10.1161/01.str.32.6.1425. [DOI] [PubMed] [Google Scholar]
- 25.Sonnenberg FA, Burkman RT, Hagerty CG, et al. Costs and net health effects of contraceptive methods. Contraception. 2004;69:447–59. doi: 10.1016/j.contraception.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Schatzker J, Rorabeck CH, Waddell JP. Non-union of the odontoid process. An experimental investigation. Clinical orthopaedics and related research. 1975:127–37. doi: 10.1097/00003086-197505000-00020. [DOI] [PubMed] [Google Scholar]
- 27.Crockard HA, Heilman AE, Stevens JM. Progressive myelopathy secondary to odontoid fractures: clinical, radiological, and surgical features. Journal of neurosurgery. 1993;78:579–86. doi: 10.3171/jns.1993.78.4.0579. [DOI] [PubMed] [Google Scholar]
- 28.Molinari RW, Dahl J, Gruhn WL, et al. Functional outcomes, morbidity, mortality, and fracture healing in 26 consecutive geriatric odontoid fracture patients treated with posterior fusion. Journal of spinal disorders & techniques. 2013;26:119–26. doi: 10.1097/BSD.0b013e31823e99e4. [DOI] [PubMed] [Google Scholar]
- 29.Muller EJ, Schwinnen I, Fischer K, et al. Non-rigid immobilisation of odontoid fractures. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2003;12:522–5. doi: 10.1007/s00586-003-0531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molinari W, Khera O, Gruhn W, et al. Functional outcomes, morbidity, mortality and fracture healing rates in 58 consecutive geriatric odontoid fracture patients treated with cervical collar or posterior fusion. Evidence-based spine-care journal. 2011;2:55–6. doi: 10.1055/s-0030-1267115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith JS, Kepler CK, Kopjar B, et al. Effect of type II odontoid fracture nonunion on outcome among elderly patients treated without surgery: based on the AOSpine North America geriatric odontoid fracture study. Spine. 2013;38:2240–6. doi: 10.1097/BRS.0000000000000009. [DOI] [PubMed] [Google Scholar]
- 32.Murphy S, XU J, Kochanek K. Deaths: Final Data for 2010. Department of Health and Human Services CfDCaP, National Center for Health Statistics ed; 2013. [PubMed] [Google Scholar]
- 33.Statistics BoL. CPI Inflation Calculator. 2014 Available at: http://www.bls.gov/data/inflation_calculator.htm. Accessed Sept 9, 2014.
- 34.Rizvi SA, Fredo HL, Lied B, et al. Surgical management of acute odontoid fractures: surgery-related complications and long-term outcomes in a consecutive series of 97 patients. The journal of trauma and acute care surgery. 2012;72:682–90. doi: 10.1097/TA.0b013e318236b675. [DOI] [PubMed] [Google Scholar]
- 35.Sime D, Pitt V, Pattuwage L, et al. Non-surgical interventions for the management of type 2 dens fractures: a systematic review. ANZ journal of surgery. 2013 doi: 10.1111/ans.12401. [DOI] [PubMed] [Google Scholar]
- 36.Laupacis A, Feeny D, Detsky AS, et al. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ: Canadian Medical Association journal = journal de l’Association medicale canadienne. 1992;146:473–81. [PMC free article] [PubMed] [Google Scholar]
- 37.Drummond MF, OB B, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 2nd. N.Y.: Oxford University Press; 1997. [Google Scholar]
- 38.Fehlings MG, Arun R, Vaccaro AR, et al. Predictors of treatment outcomes in geriatric patients with odontoid fractures: AOSpine North America multi-centre prospective GOF study. Spine. 2013;38:881–6. doi: 10.1097/BRS.0b013e31828314ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Robinson Y, Robinson AL, Olerud C. Systematic review on surgical and nonsurgical treatment of type II odontoid fractures in the elderly. Biomed Res Int. 2014;2014:231948. doi: 10.1155/2014/231948. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


