Summary
Background
magnetic resonance imaging (MRI) as a noninvasive diagnostic tool may help clinicians in the evaluation of injuries to menisci and ligaments.
Purpose
this study assessed the associations between type of trauma to knee joint, bone bruise, fracture and pathological joint effusion with injuries to menisci and ligaments of knee joint.
Methods
we reviewed knee joint MRI of 175 patients aged less than 45 years old who were referred to MRI center of our University.
Results
statistical analysis showed that tearing of medial meniscus (MM) is significantly more common in sport related trauma (p= 0.045) but tearing of medial collateral ligament (MCL) is significantly more common in non-sport related trauma (p= 0.005). Existence of bone bruise in knee MRI is negatively associated with tearing of medial meniscus (MM) (p=0.004) and positively associated with tearing of anterior cruciate ligament (ACL) (p=0.00047) and medial collateral ligament (MCL) (p = 0.0001). Existence of fracture is associated with decreased risk of the tearing of ACL and MM (p=0.04, p=0.001 respectively). Pathologic joint effusion is significantly more common in ACL and MCL tearing (p=0.0001, p=0.004 respectively).
Conclusions
as diagnostic clues, bone bruise, fracture and joint effusion may help radiologists for better assessment of injury to menisci and ligaments in MRI of patients with knee trauma.
Keywords: magnetic resonance imaging, knee joint, ligaments
Introduction
Magnetic resonance imaging (MRI) is used more commonly in the knee trauma comparing with other joints and is an excellent diagnostic tool that may help clinicians in the evaluation of injuries to menisci and ligaments, osseous structures, articular surfaces and tendon1–9. It plays an important role in clinical decision making6,7.
Bone bruise or contusion in the knee was described for the first time by Yao and Lee in 198810. Bone bruise is considered as a microfracture10, 11. For at least a decade the terms “bone bruise” and “bone marrow edema” have been known and are used synonymously12. It demonstrates a diffuse or localized decreased signal intensity on proton-density or T1-weighted images and increased signal intensity on T2-weighted images, at the short tau inversion recovery sequence (STIR) or fat-suppressed MRI sequences11–13. This appearance is thought to represent areas of hemorrhage, edema, or infarction secondary to trabecular microfractures that may all contribute to the marrow signal alterations11, 13. Areas of bone contusion in MRI that help to understand the mechanism of injury, predict and confirm the presence of capsule ligamentous injuries9. The most common traumatic causes of knee effusion are ligamentous, osseous and meniscal injuries, and overuse syndromes14.
As much as the Authors know, there isn’t any research about the association between fracture around knee joint, joint effusion on one hand and pattern of injury to the menisci and ligaments on the other hand. The main aim of this study is to assess if type of trauma, bone bruise, fracture and joint effusion are associated with the distinguished pattern of injury to menisci and ligaments. These associations may help radiologists to make more accurate diagnosis.
This study assessed the associations between type of trauma to knee joint, bone bruise, fracture and pathological joint effusion with injuries to menisci and ligaments of knee joint.
Materials and methods
Sample
As a consecutive sampling 175 patients with knee trauma who were referred to MRI center of our university were recruited. The study lasted one year. A radiologist reviewed the MRI of the patients. The age of the patients were less than 45 years (range: 18–45). One hundred forty nine (85.1%) were males and 26 (14.9%) were females. Before MRI exam we asked patients about their age, type of trauma (sport related, non-sport related), time of trauma, and history of previous knee injury or surgery of knee. The age limitation in this study was because degenerative changes (degenerative meniscal tears) after the age of 45 years may bias our research finding. We included patients who were within 1 month of an acute knee injury when referred to our center. The time of 1 month was arbitrarily selected to define an acute injury. All patients with previous knee injuries or previous knee surgery were excluded. The study was approved by the ethical committee of our University.
MRI technique
The examination was performed with 0.3 T (Hitachi, Airis 2, Japan) using sagittal and coronal T1&T2 weighted in phase and out of phase as well as fat suppression, fluid suppression, gradient echo images and axial T2 weighted spin echo images. The total imaging time of the standard protocol, including the initial survey sequence was 20 min. The patient is usually imaged in the supine position with the knee nearly or fully extended and slightly rotated externally 10° to align the anterior cruciate ligament parallel to the sagittal plane for better visualization.
Diagnostic criteria
Bone bruise was identified as an area of abnormal high signal intensity in the subchondral bone or marrow on the T2-weighted fat suppressed images. Menisci were classified as intact or torn. Meniscal tears were radiologically graded from I to IV. Grades III and IV were considered as “tear” group. As Grade I and II of tears may be related to meniscal degeneration so we categorized them with “Non tear” group.
Cruciate ligaments and collateral ligaments were dichotomized as normal or partial/total rupture.
Statistical test
All analyses were performed using SPSS (version 13.0.1, SPSS Inc, Chicago, Ill). Chi square test was used to test the associations. Logistic regression analysis was used for controlling confounding variables. The level of significance was fixed at p< 0.05. The design and report of this study is according to the standard of the Muscles, Ligaments and Tendons Journal15.
Results
In this study 123 out of 175 (70.3%) had non-sport related trauma and 52 out of 175 (29.7%) had sport related trauma. Regarding the association between type of trauma with injury to menisci and ligaments we found that tearing of medial meniscus (MM) is significantly more common in sport related trauma (p= 0.045) but tearing of medial collateral ligament (MCL) is significantly more common in non-sport related trauma (p= 0.005).
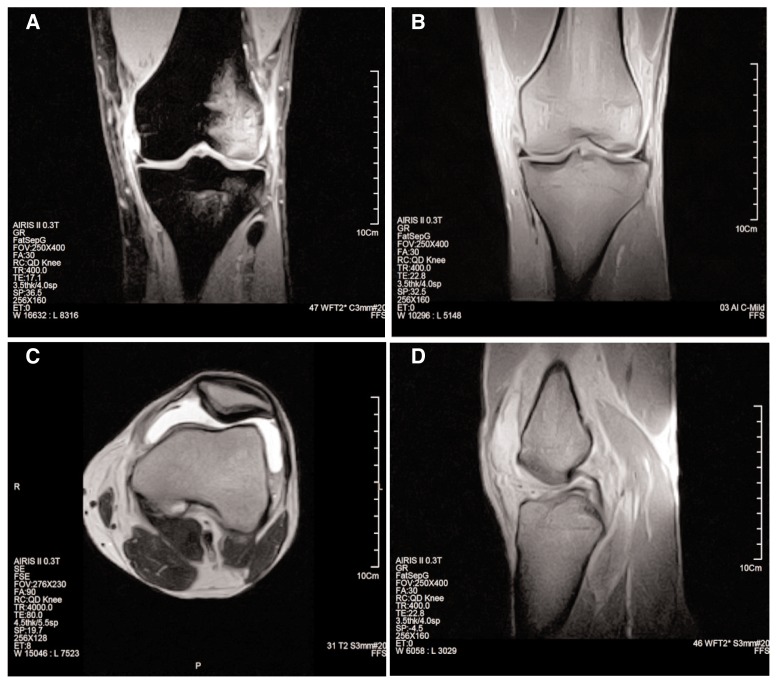
In this study 54 patients out of 175 had bone bruise (30.9%). As Table 1 shows, the existence of bone bruise is associated with decreased risk of tearing of medial meniscus (MM) and increased risk of the tearing of anterior cruciate ligament (ACL) and medial collateral ligament (MCL) but has not any correlation with tearing of other ligaments and lateral meniscus (LM). Figure 1A shows the MRI of a 21-year-old male patient with bone bruise as well as tear of MCL and Figure 1D shows the association of bone bruise with tear of ACL in same patient. Also Figure 1B shows normal MM in same patient.
Table 1.
Association of presence or absence of bone bruises with injury to the menisci and ligaments.
| No bone bruise | Bone bruise | p value | |
|---|---|---|---|
| n | 121 | 54 | |
| ACL tear | 32(26.40) | 29(53.70) | 0.00047 |
| PCL tear | 4(3.30) | 4(7.40) | 0.25 |
| MCL tear | 16(13.20) | 21(38.90) | 0.0001 |
| LCL tear | 3(2.50) | 5(9.30) | 0.11 |
| MM tear | 44(36.40) | 8(14.80) | 0.004 |
| LM tear | 34(28.10) | 13(24.10) | 0.58 |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament; MCL, medial collateral ligament; LCL, lateral collateral ligament; MM, medial meniscus; LM, lateral meniscus.
Figure 1.
A 21-year-old male patient with knee trauma. A. Coronal gradient-echo (GE) fat suppressed image shows bone bruise at lateral femoral condyle and lateral tibial plateau as well as turn of MCL. B. Coronal GE in phase T2-weighted image shows normal MM. C. Axial spin-echo (SE) T2 weighted image shows joint effusion. D. Sagittal GE in phase T2-weighted image shows complete tearing of ACL.
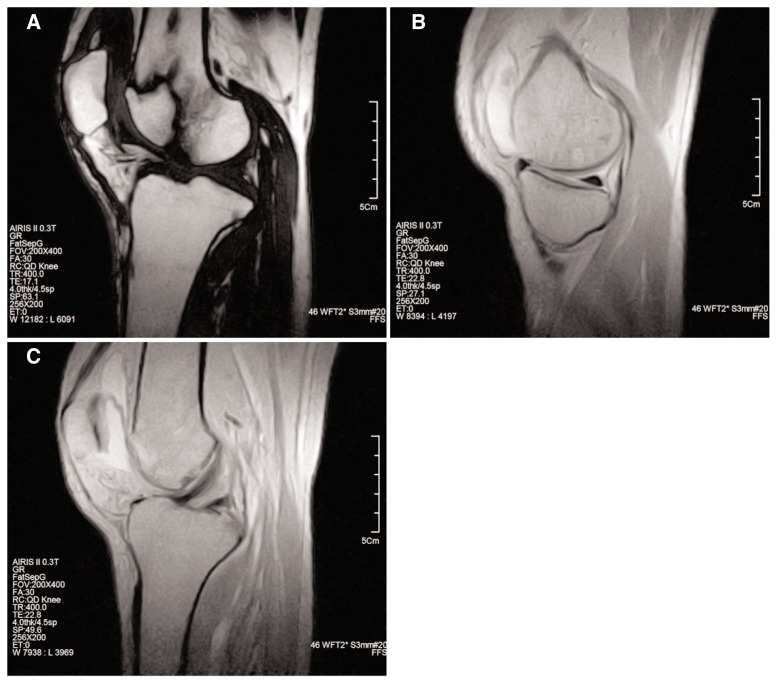
Twenty one out of 175 patients had fracture (12%). As Table 2 shows existence of fracture is associated with decreased risk of tearing of ACL and MM (Fig. 2 A–C) but has not any correlation with tearing of other ligaments and LM.
Table 2.
Association of presence or absence of fracture with injury to the menisci and ligaments.
| No fracture | fracture | p value | |
|---|---|---|---|
| n | 154 | 21 | |
| ACL tear | 80(51.90) | 6(28.60) | 0.04 |
| PCL tear | 7(4.50) | 1(4.80) | 1 |
| MCL tear | 34(22.10) | 3(14.30) | 0.57 |
| LCL tear | 8(5.20) | 0(0.0) | 0.60 |
| MM tear | 52(33.8) | 0(0.0) | 0.001 |
| LM tear | 43(27.90) | 4(19.0) | 0.39 |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament; MCL, medial collateral ligament; LCL, lateral collateral ligament; MM, medial meniscus; LM, lateral meniscus.
Figure 2.
A 37-year-old male patient with knee trauma. A. Sagittal section fluid suppressed GE sequence shows a fracture at anterior aspect of lateral femoral condyle which is extend to joint surface. B. Sagittal section from MM in phase GE T2-weighted image shows normal MM. C. Sagittal section from ACL in phase GE T2-weighted image shows intact ACL.
Eighty two out of 175 patients had joint effusion (53.1%). As Table 3 shows pathologic joint effusion is significantly more common in tearing of ACL and MCL (Fig. 1A–D). In patients with knee injury, tearing of MCL may coincide with tearing of ACL. The association between tearing of MCL and joint effusion may be confounded with ACL tearing. After controlling the effect of ACL the association between MCL and joint effusion didn’t loss its significance (p= 0.09).
Table 3.
Association of presence or absence of joint effusion with injury to the menisci and ligaments.
| No joint effusion | joint effusion | p value | |
|---|---|---|---|
| N | 93 | 82 | |
| ACL tear | 33(35.50) | 53(64.60) | 0.0001 |
| PCL tear | 2(2.20) | 6(7.30) | 0.15 |
| MCL tear | 12(12.90) | 25(30.50) | 0.004 |
| LCL tear | 3(3.20) | 5(6.10) | 0.48 |
| MM tear | 25(26.90) | 27(32.90) | 0.38 |
| LM tear | 21(22.60) | 26(31.70) | 0.17 |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament; MCL, medial collateral ligament; LCL, lateral collateral ligament; MM, medial meniscus; LM, lateral meniscus.
Discussion
This study found few significant associations between occurrence of bone bruise, fracture and joint effusion on one hand and injury to the menisci and ligaments on the other hand in patients with knee trauma who were referred to the MRI center of our University.
Type of trauma
We divided type of knee trauma into two groups: sport related and non-sport related. The higher prevalence of MM tearing in sport related trauma and MCL tearing in non-sport related trauma in our study may be related to the mechanisms of injury. We didn’t find any study about association between type of trauma and injury to the menisci and ligaments.
Bone bruise
Injury to MM is the most common injury in knee joint trauma. In our study bone bruise is associated with decreased risk of MM tear. Appearance of bone bruise in knee MRI may imply that the force of trauma is absorbed by bone tissue. We hypothesize that such absorption may decrease the intensity of knee joint rotation. This restricted rotation may decrease risk of MM tear. Our result is in contrast with the findings of Bretlau et al.12 and Jelić et al.16 which showed that bone bruise is associated with increased risk of menisci injury and also is in contrast with the study of Vincken et al.17 which showed that bone bruise has not any association with injury to MM. As Table 1 shows, bone bruise is associated with increased risk of ACL and MCL tear. Bertula et al.12 and Vincken et al.17 found similar result.
Fracture
We found that existence of fracture around knee joint is associated with decreased risk of the tearing of ACL and MM but has not any association with tearing of other ligaments and LM. Occurrence of fracture around knee joint may absorb the force of trauma. We hypothesize that such absorption may decrease the intensity of knee joint rotation. This restricted rotation may decrease risk of MM tear. Absorption of the force of trauma in fracture may be more than the absorption of the force of trauma in bone bruise. As Table 1 and Table 2 show, the difference of having MM tear between the group with bone bruise and group with non bone bruise is much less than the difference of having MM tear between the group with fracture and group without fracture. Also none of 21 patients with fracture had MM tear. Absorption of the force of trauma may also decrease the risk of ACL tear.
Joint effusion
As Table 3 shows, only ACL and MCL tear are significantly associated with pathologic joint effusion. Intracapsular inflammation after injury to ACL may explain the positive association between ACL tear and joint effusion. The association of joint effusion with MCL tearing may be related to anatomical proximity of MCL to capsule of knee joint. Also this association may be related to coincidence of ACL and MCL tears. The association between MCL tear and joint effusion didn’t loss its significance after statistical controlling of the ACL tear. So we conclude that MCL tear may affect the capsule too and induce intra-capsular inflammatory response. There isn’t any study about association between joint effusion and tearing of menisci and ligaments in acute knee trauma.
Our study has a limitation. Because of small sample size we could not do statistical analysis separately for partial and complete tear of cruciate and collateral ligament. Further study with larger sample size may reveal any difference between the groups with partial and complete tear.
The findings of this study may be helpful in reporting of the MRI of patients with knee trauma as follow: if there is bone bruise, MCL should be evaluated for any tearing more precisely. And if there is a joint effusion then ACL and MCL should be examined more precisely. Also a radiologist may consider these two points in interpretation of knee MRI in patients with knee trauma: existence of bone bruise or fracture decreases the risk of the MM injury considerably and in patients with fracture around knee joint the risk of ACL injury is lower than patients without fracture.
Footnotes
Conflict of interests
The Authors declare that they have no conflict of interests regarding the publication of this paper.
References
- 1.Espeland A, Natvig NL, Løge I, Engebretsen L, Ellingsen J. Magnetic resonance imaging of the knee in Norway 2002–2004 (national survey): rapid increase, older patients, large geographic differences. BMC Health Serv Res. 2007;7:115. doi: 10.1186/1472-6963-7-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oei EH, Ginai AZ, Hunink MG. MRI for traumatic knee injury: a review. Semin Ultrasound CT MR. 2007;28:141–157. doi: 10.1053/j.sult.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 3.Wörtler K. MR Imaging of the Knee. Radiologe. 2007;47:1131–1143. doi: 10.1007/s00117-007-1581-x. [DOI] [PubMed] [Google Scholar]
- 4.Sanders TG, Miller MD. A systematic approach to magnetic resonance imaging interpretation of sports medicine injuries of the knee. Am J Sports Med. 2005;33:131–148. doi: 10.1177/0363546504272374. [DOI] [PubMed] [Google Scholar]
- 5.Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84:5–23. doi: 10.1093/bmb/ldm022. [DOI] [PubMed] [Google Scholar]
- 6.Maurer EJ, Kaplan PA, Dussault RG, Diduch DR, Schuett A, McCue FC, et al. Acutely injured knee: effect of MR imaging on diagnostic and therapeutic decisions. Radiology. 1997;204:799–805. doi: 10.1148/radiology.204.3.9280263. [DOI] [PubMed] [Google Scholar]
- 7.Stevens KJ, Dragoo JL. Anterior cruciate ligament tears and associated injuries. Top Magn Reson Imaging. 2006;17:347–362. doi: 10.1097/RMR.0b013e3180421cc2. [DOI] [PubMed] [Google Scholar]
- 8.Kapelov SR, Teresi LM, Bradley WG, Bucciarelli NR, Murakami DM, Mullin WJ, et al. Bone contusions of the knee: increased lesion detection with fast spin-echo MR imaging with spectroscopic fat saturation. Radiology. 1993;189:901–904. doi: 10.1148/radiology.189.3.8234723. [DOI] [PubMed] [Google Scholar]
- 9.Blin D, Cyteval C, Kamba C, Blondel M, Lopez FM. Imaging of traumatic injuries of the knee. J Radiol. 2007;88:775–788. doi: 10.1016/s0221-0363(07)91345-1. [DOI] [PubMed] [Google Scholar]
- 10.Yao L, Lee JK. Occult intraosseous fracture: detection with MR imaging. Radiology. 1988;167:749–751. doi: 10.1148/radiology.167.3.3363134. [DOI] [PubMed] [Google Scholar]
- 11.Newberg AH, Wetzner SM. Bone bruises: their patterns and significance. Semin Ultrasound CT MR. 1994;15:396–409. doi: 10.1016/s0887-2171(05)80006-x. [DOI] [PubMed] [Google Scholar]
- 12.Bretlau T, Tuxøe J, Larsen L, Jørgensen U, Thomsen HS, Lausten GS, et al. Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc. 2002;10:96–101. doi: 10.1007/s00167-001-0272-9. [DOI] [PubMed] [Google Scholar]
- 13.Nakamae A, Engebretsen L, Bahr R, Krosshaug T, Ochi M. Natural history of bone bruises after acute knee injury: clinical outcome and histopathological findings. Knee Surg Sports Traumatol Arthrosc. 2006;14:1252–1258. doi: 10.1007/s00167-006-0087-9. [DOI] [PubMed] [Google Scholar]
- 14.Johnson MW. Acute knee effusions: a systematic approach to diagnosis. Am Fam Physician. 2000;61:2391–2400. [PubMed] [Google Scholar]
- 15.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal. Basic principles and recommendations in clinical and field science research. MLTJ. 2013;3( 4):250–252. [PMC free article] [PubMed] [Google Scholar]
- 16.Jelić D, Masulović D. Bone bruise of the knee associated with the lesions of anterior cruciate ligament and menisci on magnetic resonance imaging. Vojnosanit Pregl. 2011;68:762–766. doi: 10.2298/vsp1109762j. [DOI] [PubMed] [Google Scholar]
- 17.Vincken PW, Ter Braak BP, van Erkel AR, Coerkamp EG, Mallens WM, Bloem JL. Clinical consequences of bone bruise around the knee. Eur Radiol. 2006;16:97–107. doi: 10.1007/s00330-005-2735-8. [DOI] [PubMed] [Google Scholar]