Abstract
Radiation dermatitis is one of the most common acute toxicities of both radiotherapy and chemoradiotherapy. Many clinical trials have evaluated the level of toxicity using the Common Terminology Criteria for Adverse Events ver. 4.03. This criterion accounts for severity in a single sentence only, and no visual classification guide has been available. Thus, there is a risk of subjective interpretation by the individual investigator. This contrasts with the situation with hematologic toxicities, which can be interpreted objectively. The aim of this prospective picture collection study was to develop a grading tool for use in establishing the severity of radiation dermatitis in clinical trials. A total of 118 patients who were scheduled to receive definitive or postoperative radiotherapy or chemoradiotherapy were enrolled from the four participating cancer centers. All researchers in our group used the same model of camera under the same shooting conditions to maintain consistent photographic quality. In all, 1600 photographs were collected. Of these, 100 photographs qualified for the first round of selection and were then graded by six experts, basically in accordance with the CTCAE ver. 4.03 (JCOG ver. in Japanese). After further study, 38 photographs were selected as representing typical models for Grade 1–4 radiation dermatitis; the radiation dermatitis grading atlas was produced from these photographs. The atlas will play a major role in ensuring that the dermatitis rating system is consistent between the institutions participating in trials. We hope that this will contribute to improving the quality of clinical trials, and also to improving the level of routine clinical practice.
Keywords: radiation dermatitis, head-and-neck cancer, grading system, radiotherapy, acute toxicity
INTRODUCTION
Radiotherapy (RT) is commonly used in the treatment of head-and-neck cancer. Radiotherapy with concurrent chemotherapy (CRT) is now considered the standard of care for locally advanced squamous cell carcinoma of the head and neck (SCCHN) [1–4] and for high-risk postoperative patients [5–7]. As treatment strength increases, however, so too does the risk of toxicity. Radiation dermatitis is one of the most common acute toxicities of both RT and CRT. Many clinical trials have evaluated toxicity using the Common Terminology Criteria for Adverse Events (CTCAE) ver. 4.03 (http://www.jcog.jp/doctor/tool/ctcaev4.html). This tool categorizes radiation dermatitis under the CTCAE term ‘Dermatitis radiation’, which is defined as burns caused by exposure to chemicals, direct heat, electricity, flames and radiation. Although severity is graded according to symptoms (Grade 0 to 5), the criteria provide no information to aid classification, such as photographs of representative examples. We consider that the judgment of severity based on written descriptions only may result in discrepancies in evaluation between medical staff, and that visual information is an important means of ensuring objective evaluation. To date, however, no such visual classification guide has been available.
Here, we conducted a prospective picture collection study aimed at developing a grading atlas of radiation dermatitis in Japanese head-and-neck cancer patients.
MATERIALS AND METHODS
This study was approved by the Institutional Review Boards of each of the participating institutions.
Eligibility
Patients scheduled to receive definitive or postoperative radiotherapy or chemoradiotherapy (50 Gy) at the four participating institutions linked to our research group were eligible for enrollment. Written informed consent for treatment was obtained from all patients before the initiation of the study. No exclusion criteria were established.
Photographic technique
All institutions in our group used the same type and model of camera (RPowerShotG12, Canon). The camera setting was ‘Portrait mode’, an auto-exposure shooting mode enabling consistent recording of skin findings, regardless of the photographer. The distance from the camera to the patient was ∼1 m, and the orbit and collarbone were included within the photographic field to ensure that the whole irradiation field was included in a single photograph. Patient pictures were taken from three directions (front, and left and right oblique angles) at each session (Fig. 1). To ensure patient privacy, we specified that the photographic field should not include the whole countenance, and in cases where the whole face was within this range, identification was prevented using a trimming technique.
Fig. 1.
Protocol for photography. Patient photos are taken from three directions: front, and left and right oblique angles. A monochromatic background is desirable.
The timing of photography was not strictly scheduled in our protocol. Each patient was photographed once a week from the start to the end of treatment, and sometimes until dermatitis was completely healed.
Photograph selection
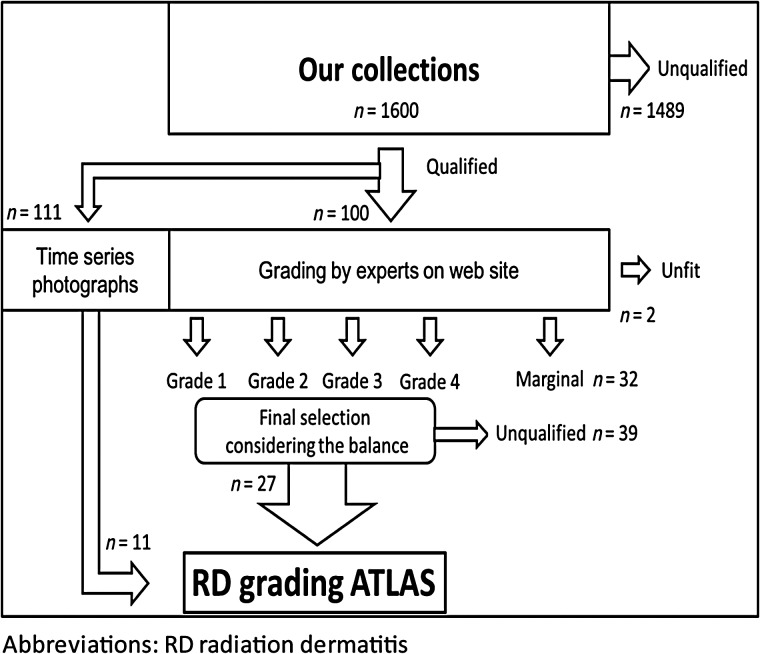
We selected photographs from our collection as suitable for inclusion in the atlas by following steps (illustrated in Fig. 2). Our radiation dermatitis grading atlas steering committee had the final say over selection. Selections were made by group consensus.
Patients were photographed every week during the entire period.
Photos that qualified for the first round of selection were used as ‘Time series photographs’.
The 100 qualifying photographs were selected and hosted on a web-based system and graded into one of five grades (0–4) by six experts (radiologists and nurses). These six experts accessed the photographs from separate locations and without knowledge of the grading of the other five. Photographs that received the same grade from all six experts were designated as ‘Grade x dermatitis’. Photographs that receive the same grade from five experts and an adjacent grade (x ± 1) from one expert were designated as ‘Grade x dermatitis’, using the grade given by the five experts.
Photographs that received the same grade from three or four experts and an adjacent grade (x ± 1) from two or three experts were adopted as ‘marginal Grade x/y dermatitis.’
If a photograph received three or more different grades, it was excluded as ‘unfit’.
Photographs that were best suited for listing as samples in the Radiation Dermatitis Grading Atlas were chosen from the final selection of photographs. The remaining photographs were retained as stock for possible future replacement use, based on user opinions after actual clinical implementation.
Fig. 2.
Photograph selection schema. RD = radiation dermatitis.
Methods of grading of radiation dermatitis in our protocol
Grading was performed basically in accordance with the CTCAE ver. 4.03 (Medical Dictionary for Regulatory Activities; MedDRA v12.0 Code 10061103, Dermatitis radiation).
Grade 1: Faint erythema or dry desquamation
Grading requires comparison with a pretreatment photograph and confirmation of the irradiated field.
Grade 2: Moderate to brisk erythema; patchy moist desquamation, mostly confined to skin folds and creases; moderate edema
To distinguish Grade 2 from Grade 1, the simplest finding is ‘moist desquamation’. With regard to the degree of erythema, forming a consensus often requires discussion among experts (see Discussion section).
Grade 3: Moist desquamation in areas other than skin folds and creases; bleeding induced by minor trauma or abrasion
Because the distinguishing feature of Grade 3 radiation dermatitis in clinical practice is often bleeding induced by minor trauma or abrasion, we evaluated the radiation dermatitis grading using photographs taken just after the removal of the previous gauze and just prior to moisturizing treatment. Gauze for moisturizing that has been applied the previous day is removed just prior to radiation therapy. Since bleeding caused by contact is most easily observed at that time, it is easiest to judge Grade 3 radiation dermatitis from the photograph taken at that time.
Grade 4: Life-threatening consequences; skin necrosis or ulceration of full-thickness dermis; spontaneous bleeding from involved site; skin graft indicated
In clinical trials and practice, Grade 4 dermatitis is unusual in radiation therapy. The feature distinguishing Grade 4 from Grade 3 dermatitis is irreversible injury occurring in the skin. Radiotherapy (or chemoradiotherapy) should be interrupted or postponed in the case of Grade 4 dermatitis. The judgment of the clinician is given priority over that of photo interpretation.
RESULTS
A total of 118 patients who were scheduled to receive definitive or postoperative radiotherapy or chemoradiotherapy were enrolled from the four participating cancer centers, and 1600 photographs were collected. We initially estimated that we would require 600–800 photographs from 200 patients, but this number was quickly exceeded during recruitment. Recruitment was, therefore, stopped at 118 patients.
Selection
A total of 111 photographs from nine patients were selected as ‘Series photographs’. Typical series photographs are shown in Fig. 3. Of the remaining photographs, 100 were selected for grading by the specialists. For these photos, all members gave the same grading for 34 photographs (20 in Grade 1, 12 in Grade 2 and 2 in Grade 3), which were thus classified as ‘Grade x dermatitis’; another 32 photographs were given the same grading by five members, and these were classified as ‘Grade x dermatitis’ (1 in Grade 0, 19 in Grade 1, 7 in Grade 2, 4 in Grade 3 and 1 in Grade 4). Two photographs were excluded because they received three different gradings. The remaining 32 photographs were classified as ‘marginal grade dermatitis’.
Fig. 3.
Photographic series, demonstrating how to take a sequence of photos. This patient had T1N0 laryngeal cancer and was treated with radiotherapy alone, scheduled at 66 Gy/33fr. RT = radiotherapy.
Expert grader background and patterns of grading
The six medical staff members participating in the study as ‘experts’ consisted of four radiation oncologists and two expert nurses who worked full time for the radiation oncology division. For the 32 photographs that received the same grading from five members, three participants (two radiation oncologists and a nurse) tended to underestimate radiation dermatitis, whereas the remaining three (two radiation oncologists and a nurse) tended to overestimate radiation dermatitis. Two photographs (2%) received three patterns of grading from the six experts.
Radiation Dermatitis Grading Atlas for Clinical Trials
As a result of this process, 38 photographs were selected. The full text of the Radiation Dermatitis Grading Atlas for Clinical Trials can be found in the online version (http://www.ncc.go.jp/jp/ncce/clinic/pdf/radiation_oncology_01.pdf).
DISCUSSION
The Radiation Dermatitis Grading Atlas will be used by clinical trials as a scaling tool for radiation dermatitis. Our group determined several rules concerning borderline cases of Grades 1–2 and 2–3 before grading.
Erythema
Distinguishing Grade 1 and 2 required defining the degree of erythema. In our group, an erythema color of ‘salmon pink’ or ‘light brown’ was considered to be Grade 1 radiation dermatitis (Fig. 4). Salmon pink erythema occurs before progression to serious dermatitis, whereas light brown erythema is found on recovery from serious dermatitis, and should be distinguished from pigmentation.
Fig. 4.
Typical Grade 1 dermatitis. Salmon pink erythema is observed before the development of serious dermatitis, whereas light brown erythema is found after recovery from serious dermatitis and must be differentiated from pigmentation. For photo interpretation, the photographic conditions should be defined in the protocol.
Area of moist desquamation
Interpreting the distinction of ‘mostly confined to skin folds and creases’ and ‘other than skin folds and creases’ is a difficult problem. In the present study, we attempted to develop a consensus for this interpretation using photographs.
Cases in which symptoms were affected by skin folds, such as more marked moist desquamation in areas of skin folds than in other areas, were determined to be Grade 2 (Fig. 5). Cases in which moist desquamation was spread evenly (to the extent that skin folds became unclear) were determined to be Grade 3 (Fig. 6).
Fig. 5.
Typical Grade 2 radiation dermatitis. Moderate or brisk erythema (left) is one the main findings in Grade 2 radiation dermatitis. A finding of moist desquamation (right) is often necessary to distinguish it from Grade 1 radiation dermatitis.
Fig. 6.
Typical Grade 3 radiation dermatitis. Left: The presence of bleeding induced by minor trauma or abrasion immediately after removal of the gauze coating. Right: Moist desquamation in areas other than skin folds and creases
There are only six photographs of Grade 3 dermatitis in this atlas. We considered that only typical Grade 3 dermatitis should be selected because distinguishing between Grade 2 and Grade 3 is clinically very important.
Also, in our remaining photographs, there were only a few photographs that all experts identified as typical Grade 3 dermatitis.
In future, we have a plan to increase the number of these photographs by including photographs provided by other institutions.
Life-threatening consequences
There is only one photograph that we considered to represent typical Grade 4 dermatitis (Fig. 7). Because the judgment of Grade 4 should be carried out in a clinical setting, photo interpretation may not suitable for Grade 4–5.
Fig. 7.
Grade 4 dermatitis. This photograph shows typical Grade 4 dermatitis, including spontaneous bleeding from the involved site. Skin necrosis or ulceration of the full-thickness dermis; skin graft indicated. Because Grade 4 dermatitis was unusual, we have not been able to obtain the typical photographs according to the protocol as yet.
With regard to radiation dermatitis in patients with locally advanced head-and-neck cancer receiving radiotherapy with cetuximab, an advisory board of seven leading European specialists published a proposal for a revised grading system. This system defined the degree of moist desquamation as the percentage of these areas in all irradiation fields [8]. Although a good idea, implementation is hindered by the recent availability of intensity-modulated radiotherapy [9–11] and high-precision radiotherapy [12], which irradiate from all directions, making it difficult to precisely determine which areas are to be included as ‘irradiated’.
The control of radiation dermatitis is one of the most important aims in definitive treatment. Any evaluation of the safety profile of a new treatment in a clinical trial should include the frequency of severe dermatitis as a required item. In the CTCAE ver. 4.03, radiation dermatitis is evaluated under the CTCAE term ‘Dermatitis radiation’. However, it is often difficult to set the category of ‘radiation dermatitis’ as a primary endpoint. Because CTCAE ver. 4.03 accounts for severity in a single sentence only, it is at risk of subjective interpretation by the individual investigator. This contrasts with the situation for hematologic toxicities, which can be interpreted objectively.
We therefore sought to establish text that would support interpretation of the category ‘Dermatitis radiation’ in the CTCAE ver. 4.03. It is important that all researchers share the same recognition and understanding of radiation dermatitis of Grades 2 and 3. The Radiation Dermatitis Grading Atlas will play a major role in addressing this need in the dermatitis rating system for institutions participating in trials.
Photo interpretation for the evaluation of radiation dermatitis at central review
Even if the Radiation Dermatitis Grading Atlas is used in participating institutions, evaluation of radiation dermatitis will remain subjective. Accordingly, confirmation by central review using photos may be an effective means of maintaining quality [13, 14]. Prior to the start of the present study, we identified various potential problems in the evaluation of radiation dermatitis through trial and error. If photographic quality is not uniform across the various institutions in a study, radiation dermatitis cannot be appropriately evaluated. We suggest that photographic quality should be incorporated in the protocol of clinical trials.
Limitations of the Radiation Dermatitis Grading Atlas
At present, the Radiation Dermatitis Grading Atlas plays a role as an auxiliary tool for toxicity assessment in clinical trials, and its use in clinical practice requires further research.
Since our present patients are all Japanese, the Atlas is considered useful for assessment in Asian patients, but may not be suitable in other races.
Concurrent use of cetuximab is reported as hindering accurate assessment with CTCAE ver. 4.03. Rules for individual protocols should be specified in detail.
Future direction
We have succeeded in creating the first version of the Radiation Dermatitis Grading Atlas. A validation study is the next step necessary. Two suggestions are made for ongoing development. The first is to produce regularly updated versions by increasing or decreasing the number of photographs so as to refine the atlas as a tool for use in clinical trials. The second is to produce the atlas in book form for use in not only clinical trials, but clinical practice as well. We hope that this study will contribute to improving the quality of clinical trials, and also to improving the level of routine clinical practice.
FUNDING
This study was supported in part by The National Cancer Center Research and Development Fund (26-A-29) (27-A-3) from Ministry of Health, Labour and Welfare. Funding to pay the open access publification charge for this article was provided by The National Cancer Center Research and Development Fund.
REFERENCES
- 1.Forastiere AA, Goepfert H, Maor M et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. New Engl J Med 2003;349:2091–8. [DOI] [PubMed] [Google Scholar]
- 2.Adelstein DJ, Li Y, Adams GL et al. An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol 2003;21:92–8. [DOI] [PubMed] [Google Scholar]
- 3.Pignon JP, Bourhis J, Domenge C et al. Chemotherapy added to locoregional treatment for head and neck squamous-cell carcinoma: three meta-analyses of updated individual data. MACH-NC Collaborative Group. Meta-Analysis of Chemotherapy on Head and Neck Cancer. Lancet 2000;355:949–55. [PubMed] [Google Scholar]
- 4.Pignon JP, le Maître A, Maillard E et al. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiother Oncol 2009;92:4–14. [DOI] [PubMed] [Google Scholar]
- 5.Cooper JS, Pajak TF, Forastiere AA et al. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. New Engl J Med 2004;350:1937–44. [DOI] [PubMed] [Google Scholar]
- 6.Bernier J, Cooper JS, Pajak TF et al. Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (#9501). Head Neck 2005;27:843–50. [DOI] [PubMed] [Google Scholar]
- 7.Bernier J, Domenge C, Ozsahin M et al. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. New Engl J Med 2004;350:1945–52. [DOI] [PubMed] [Google Scholar]
- 8.Bernier J, Bonner J, Vermorken JB et al. Consensus guidelines for the management of radiation dermatitis and coexisting acne-like rash in patients receiving radiotherapy plus EGFR inhibitors for the treatment of squamous cell carcinoma of the head and neck. Ann Oncol 2008;19:142–9. [DOI] [PubMed] [Google Scholar]
- 9.Marta GN, Silva V, de Andrade Carvalho H et al. Intensity-modulated radiation therapy for head and neck cancer: systematic review and meta-analysis. Radiother Oncol 2014;110:9–15. [DOI] [PubMed] [Google Scholar]
- 10.Nutting CM, Morden JP, Harrington KJ et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol 2011;12:127–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishimura Y, Shibata T, Nakamatsu K et al. A two-step intensity-modulated radiation therapy method for nasopharyngeal cancer: the Kinki University experience. Japn J Clin Oncol 2010;40:130–8. [DOI] [PubMed] [Google Scholar]
- 12.Gregoire V, Jeraj R, Lee JA et al. Radiotherapy for head and neck tumours in 2012 and beyond: conformal, tailored, and adaptive? Lancet Oncol 2012;13:e292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zenda S, Ishi S, Kawashima M et al. A Dermatitis Control Program (DeCoP) for head and neck cancer patients receiving radiotherapy: a prospective phase II study. Int J Clin Oncol 2013;18:350–5. [DOI] [PubMed] [Google Scholar]
- 14.Zenda S, Ishi S, Akimoto T et al. DeCoP, a Dermatitis Control Program using a moderately absorbent surgical pad for head and neck cancer patients receiving radiotherapy: a retrospective analysis. Japn J Clin Oncol 2015;45:433–8. [DOI] [PubMed] [Google Scholar]