Abstract
OBJECTIVE
To evaluate feasibility, safety, and efficacy of day-and-night hybrid closed-loop insulin delivery in adolescents with type 1 diabetes under free-living conditions without remote monitoring or supervision.
RESEARCH DESIGN AND METHODS
In an open-label, randomized, free-living, crossover study design, 12 adolescents receiving insulin pump therapy (mean [±SD] age 15.4 ± 2.6 years; HbA1c 8.3 ± 0.9%; duration of diabetes 8.2 ± 3.4 years) underwent two 7-day periods of sensor-augmented insulin pump therapy or hybrid closed-loop insulin delivery without supervision or remote monitoring. During the closed-loop insulin delivery, a model predictive algorithm automatically directed insulin delivery between meals and overnight; prandial boluses were administered by participants using a bolus calculator.
RESULTS
The proportion of time when the sensor glucose level was in the target range (3.9–10 mmol/L) was increased during closed-loop insulin delivery compared with sensor-augmented pump therapy (72 vs. 53%, P < 0.001; primary end point), the mean glucose concentration was lowered (8.7 vs. 10.1 mmol/L, P = 0.028), and the time spent above the target level was reduced (P = 0.005) without changing the total daily insulin amount (P = 0.55). The time spent in the hypoglycemic range was low and comparable between interventions.
CONCLUSIONS
Unsupervised day-and-night hybrid closed-loop insulin delivery at home is feasible and safe in young people with type 1 diabetes. Compared with sensor-augmented insulin pump therapy, closed-loop insulin delivery may improve glucose control without increasing the risk of hypoglycemia in adolescents with suboptimally controlled type 1 diabetes.
Introduction
Childhood-onset type 1 diabetes is associated with significant morbidity and reduced life expectancy resulting from dysglycemia-related acute and chronic complications (1,2). Adolescence is a particularly vulnerable period for the onset and priming of cardiovascular and renal complications (3,4), whereas the majority of young people with type 1 diabetes do not meet treatment targets (5,6).
Diabetes management in adolescence is complicated by psychological and physiological changes accompanying puberty (7). Apart from hypoglycemia (8), reduced compliance with therapy is a major obstacle to achieving tight glucose control (9). Diabetic ketoacidosis is more common (10,11), omission of or delayed insulin boluses with meals or snacks is widespread (9,12), and discontinuation of insulin pump therapy is highest among adolescents (13). Sensor-augmented insulin pump therapy (14) and threshold-suspend features may alleviate the burden of hypoglycemia and improve outcomes (15,16), but acceptance and use of continuous glucose monitoring systems is notably reduced among teenagers (14,17).
The artificial pancreas or closed-loop systems differ from conventional pump therapy and threshold-suspend approaches through the use of a control algorithm that autonomously and continually increases and decreases subcutaneous insulin delivery based on real-time sensor glucose levels (18). Results from studies under controlled laboratory settings (19–23) and investigations of closed-loop in transitional outpatient settings, incorporating remote monitoring and supervision by research staff in hotels (24) or at diabetes camps (25,26), have demonstrated improved glucose control and reduction of hypoglycemia (25–28). At-home studies (29–32) of 3 weeks to 3 months of application of overnight close-loop insulin delivery have been performed in adolescents and adults. However, home studies (32,33) of unsupervised day-and-night closed-loop application have been restricted to adults only. There has been no previous evaluation of unsupervised day-and-night closed-loop insulin delivery in free-living settings in adolescents 10–18 years of age.
Here, we present the results of a 7-day-long, day-and-night closed-loop home trial in adolescents with type 1 diabetes under free-living conditions. We hypothesized that day-and-night use of hybrid closed-loop insulin delivery without remote monitoring is feasible, safe, and could improve glycemic control compared with sensor-augmented pump therapy in this population.
Research Design and Methods
Study Management and Regulatory Approvals
Prior to study initialization, approval was sought and received from the local independent research ethics committee and the U.K. regulatory authority (Medicines & Health products Regulatory Agency). An independent Data Safety and Monitoring Board oversaw the study and was informed of all unanticipated adverse events that occurred during the study.
Participants
Study participants were recruited between August 2014 and October 2014 through the pediatric diabetes clinic at Addenbrooke’s Hospital, Cambridge, U.K. Key inclusion criteria were age 10–18 years, diagnosis of type 1 diabetes, treatment with insulin pump therapy for at least 3 months, willingness to perform at least four fingerstick glucose measurements per day, and HbA1c level ≤11% (97 mmol/mol). Exclusion criteria included established nephropathy, neuropathy, or proliferative retinopathy; total daily insulin dose of ≥2.0 units/kg or <10 units/day; concurrent illness or medications likely to interfere with interpretation of study results; significant hypoglycemia unawareness, as judged by the clinical investigators; recurrent incidents of severe hypoglycemia, as defined by the International Society for Pediatric and Adolescent Diabetes guidelines, during the previous 6 months; more than one episode of diabetic ketoacidosis within 12 months prior to study enrollment; pregnancy; and breast feeding. Participants ≥16 years of age and parents or guardians of participants <16 years of age signed informed consent; written assent was obtained from minors.
Study Design
The study adopted an open-label, prospective, single-center, randomized crossover design contrasting automated closed-loop insulin delivery and sensor-augmented pump therapy over 7 days (Supplementary Fig. 1). The study was performed under free-living home conditions without remote monitoring or supervision by research staff, and participants performed their usual activities of daily living. The participants were free to consume any meals of their choice, and no restrictions were imposed on traveling or moderate exercise. All participants had access to a 24-h telephone helpline to contact the study team in the event of study-related issues.
Study Procedures
Blood samples for the measurement of baseline HbA1c and nonhypoglycemia C-peptide levels were obtained at study enrollment. At the start of the run-in phase, participants were trained on the use of the study insulin pump (DANA Diabecare R; Sooil, Seoul, South Korea) and study real-time continuous glucose monitoring device (FreeStyle Navigator II; Abbott Diabetes Care, Alameda, CA). The study insulin pump was programmed with the participant’s usual basal settings, usual insulin-to-carbohydrate ratios and correction factors, and delivered a rapid-acting insulin analog (insulin aspart; Novo Nordisk, Bagsvaerd, Denmark; or insulin lispro; Eli Lilly, Indianapolis, IN). Participants were advised to use the bolus calculator for all meals during the entire study. Ability and competency to use the study devices was formally assessed, and additional training was provided as required. Over a 1- to 2-week run-in phase, participants were required to use the study pump and collect at least 5 days worth of sensor glucose to pass the compliance assessment. Data obtained during the run-in phase were used for therapy optimization as per usual clinical practice.
After the run-in period, participants underwent two 7-day periods, in random order, during which glucose was controlled either by sensor-augmented insulin pump therapy or hybrid closed-loop insulin delivery. The two treatment interventions were separated by a 1- to 4-week washout period, during which the participants could continue using the study insulin pump applying their standard pump settings. Continuous glucose monitoring was discontinued during the washout period.
The participants had the same number of planned contacts with the study team during the two study periods, and used the study pump and the study real-time continuous glucose monitoring device during both study periods.
Randomization assignment was unblinded, but allocation between treatment sequences was concealed to the study staff until after randomization, which occurred the day prior to the first intervention. Random permuted blocks were used for treatment sequence allocation.
On the first day of the closed-loop insulin delivery period, a 2- to 3-h training session was provided by the investigators at the clinical research facility, including initiation and discontinuation of the closed-loop system, switching between closed-loop and usual pump therapy, meal bolus procedure, and the use of study devices during exercise. Prandial boluses were advised to be delivered before the meals using the standard bolus calculator of the pump. Competency on the use of closed-loop system was assessed prior to discharge. After the training session, participants continued the study intervention for the next 7 days under free-living conditions in their home and school environment. Automated closed-loop insulin delivery was continued during exercise of mild to moderate intensity, and exercise was announced to the algorithm. Participants were advised to discontinue closed-loop insulin delivery and follow their usual insulin pump therapy for certain activities, such as periods of strenuous exercise, diving, or contact sports.
Participants were advised to calibrate the continuous glucose monitoring device according to the manufacturer instructions and to use the built-in glucometer for all fingerstick measurements; they were free to make decisions on alarm thresholds for the continuous glucose monitoring device. Participants followed their standard clinic guidelines for hypoglycemia and hyperglycemia treatment.
Closed-Loop System
The FlorenceD2A closed-loop system (University of Cambridge, Cambridge, U.K.) (34) comprised a model predictive control algorithm (version 0.3.30, University of Cambridge) residing on a smartphone (Nexus 4; LG, South Korea), which communicated wirelessly with a continuous glucose monitoring receiver through a purpose-made translator unit (TriTeq, Hungerford, U.K.) (Supplementary Fig. 2). Every 12 min, the control algorithm calculated a new insulin infusion rate, which was automatically set on the study insulin pump. The calculations used a compartment model of glucose kinetics (35) describing the effect of rapid-acting insulin analogs and the carbohydrate content of meals on glucose levels. In this trial, a hybrid closed-loop approach was applied, in which participants additionally administered prandial insulin for all meals using the standard bolus calculator. The control algorithm was initialized using preprogrammed basal insulin doses downloaded from the study pump. Additionally, information about the participant’s weight and total daily insulin dose were entered at setup. During closed-loop operation, the algorithm adapted itself to the particular participant. The treat-to-target control algorithm aimed to achieve glucose levels between 5.8 and 7.3 mmol/L, and adjusted the actual level depending on fasting versus postprandial status and the accuracy of model-based glucose predictions. Though devices were advised to be kept in the vicinity of each other, a wireless transmission range of several meters allowed for flexibility in terms of device wear; and appropriate cases, clips, and pouches were provided.
The continuous glucose monitoring receiver provided hypoglycemia and hyperglycemia alarms, the insulin pump provided standard alarms, and the smartphone alerted the user about aspects related to closed-loop operation such as when closed-loop insulin delivery started or stopped.
Safety Precautions During Closed-Loop
Participants performed a calibration check before breakfast and before the evening meal. If the sensor glucose level was above the fingerstick glucose level by >3.0 mmol/L, the continuous glucose monitoring device was manually recalibrated. There was no recalibration for the sensor under reading. These instructions resulted from an in silico evaluation of hypoglycemia and hyperglycemia risk (36) using the validated Cambridge simulator (37).
If sensor glucose became unavailable or if there was another failure, preprogrammed insulin delivery automatically restarted within 30–60 min. This limited the risk of insulin underdelivery and overdelivery (36). Safety rules limited the maximum insulin infusion and suspended insulin delivery if the glucose level was ≤4.3 mmol/L or when sensor glucose was rapidly decreasing.
Assays
HbA1c level was measured using ion exchange high-performance liquid chromatography (G8 HPLC Analyzer; Tosoh Bioscience Inc., CA; interassay coefficients of variation (CVs): 1.3% at 31.2 mmol/mol, 0.8% at 80.5 mmol/mol). C-peptide measurements were performed using chemiluminescence immunoassay (IV2–004; Invitron Ltd, Monmouth U.K.; interassay variation: 7.8, 4.3, and 6.7% at 268, 990, and 1,862 pmol/L, respectively). Analytical sensitivity for the C-peptide assay was 5.0 pmol/L.
Study Outcomes
The primary outcome was the proportion of time when glucose was in the target range (3.9–10.0 mmol/L) during the 7-day study periods. Secondary outcomes included mean sensor glucose levels, glucose variability, and time spent below and above the target glucose level. Outcomes were calculated during day-and-night, daytime, and overnight periods; daytime was classified as being between 8:00 a.m. and midnight, and nighttime was classified as being between midnight and 8:00 a.m. Glucose variability was assessed by the SD and the CV of sensor glucose levels. Hypoglycemia burden was assessed by calculating the glucose sensor area under the curve (AUC) of <3.5 mmol/L.
Statistical Analysis
The statistical analysis plan was agreed on by investigators in advance. All analyses were undertaken on an intention-to-treat basis. Efficacy and safety data from all randomized participants with and without protocol violation were included in the analyses. The respective values obtained during the 7-day randomized interventions contrasting the closed-loop system against the sensor-augmented pump therapy were compared using a least-squares regression model. Sensor glucose outcomes were adjusted for baseline glucose level and period effect; insulin outcomes were adjusted for period effect. Rank normal transformation analyses were used for highly skewed end points. Outcomes were presented as the mean ± SD for normally distributed values or as the median (interquartile range) for non-normally distributed values. Secondary outcomes for daytime and nighttime periods were excluded from calculating P values to limit multiple comparisons. Outcomes were calculated using GStat software (University of Cambridge, version 2.2). Analysis was done using SAS version 9.4 (SAS Institute, Cary, NC). A 5% significance level was considered statistically significant. All P values are two-sided.
Results
Participants
Fourteen subjects were screened. Supplementary Fig. 3 shows the flow of participants through the study. One participant did not meet the inclusion/exclusion criteria, and another voluntarily withdrew consent and did not complete the run-in phase. Twelve eligible participants were randomized, completed the study, and provided data for analyses (8 males, 4 females; age 15.4 ± 2.6 years; diabetes duration 8.2 ± 3.4 years; HbA1c level 8.3 ± 0.9% [68 ± 10 mmol/mol]; insulin pump therapy duration 5.6 ± 2.9 years; total daily insulin dose 0.84 ± 0.22 units/kg/day) (Supplementary Table 1).
Day-and-Night Glucose Control and Insulin Delivery
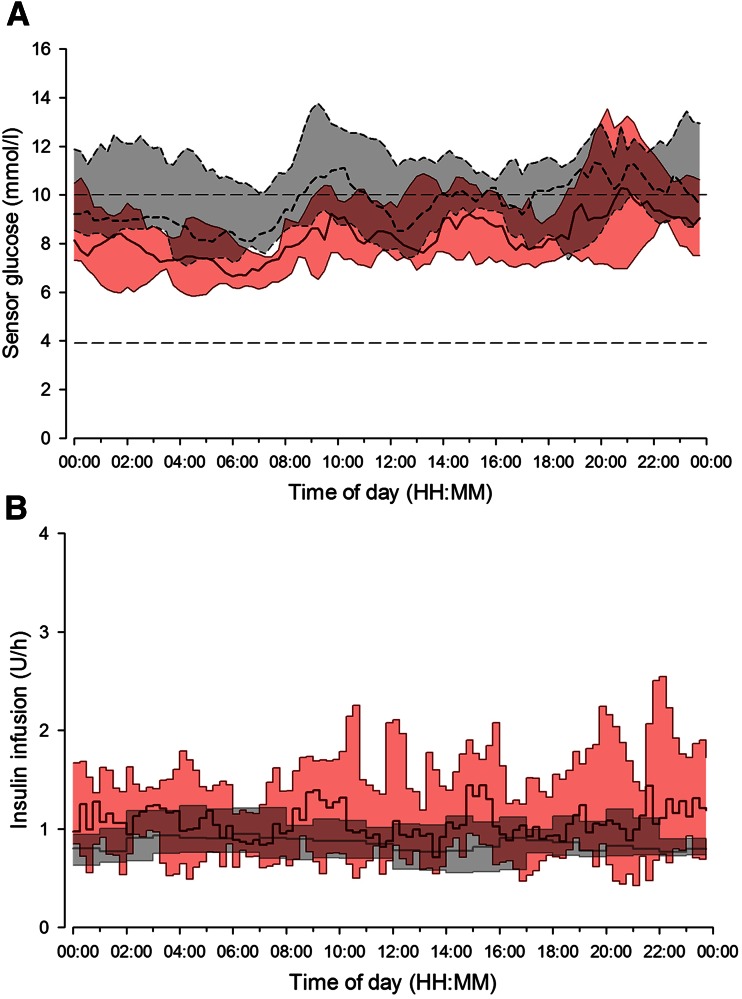
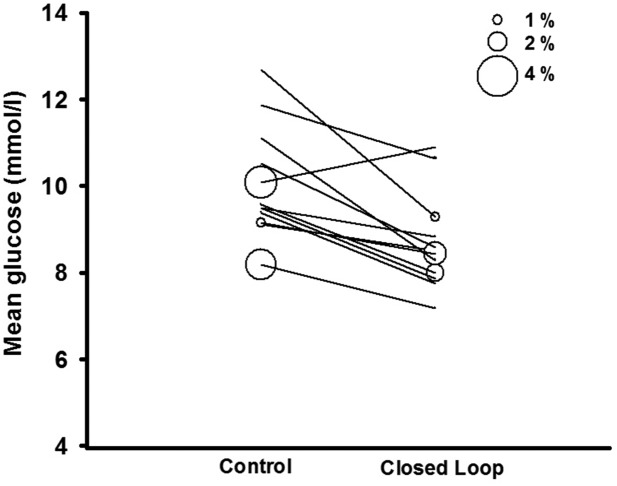
The primary end point, the proportion of time that the sensor glucose level was in the target glucose range of 3.9–10.0 mmol/L, significantly increased during closed-loop (P < 0.001, Table 1). Twenty-four hour sensor glucose and insulin delivery profiles are shown in Fig. 1. Closed-loop insulin delivery significantly reduced the mean glucose level (P = 0.028) and the time spent above target glucose level (P = 0.005) without increasing the time spent in hypoglycemia (Table 1 and Fig. 2). The proportion of time when the sensor glucose level was in the hypoglycemic range (<3.9 and 2.8 mmol/L) and the AUC when the sensor glucose level was <3.5 mmol/L were low and comparable during the study periods.
Table 1.
Comparison of glucose control and insulin delivery during closed-loop and control period
| Closed-loop (n = 12) | Control (n = 12) | P value | |
|---|---|---|---|
| Time spent at glucose level (%) | |||
| 3.9–10.0 mmol/L* | 72 (59–77) | 53 (46–59) | <0.001 |
| >10.0 mmol/L | 26 (21–35) | 43 (38–52) | 0.005 |
| <3.9 mmol/L | 2.9 (1.8–4.8) | 1.7 (0.9–5.1) | 0.87 |
| <2.8 mmol/L | 0.2 (0.0–0.6) | 0.1 (0.0–0.6) | 0.67 |
| AUCday <3.5 mmol/L (mmol/L × min)† | 6.4 (2.8–23.7) | 4.3 (1.8–13.6) | 0.77 |
| Mean glucose (mmol/L) | 8.7 ± 1.1 | 10.1 ± 1.3 | 0.028 |
| Within-day SD of glucose (mmol/L) | 3.5 (3.3–4.2) | 4.0 (3.6–4.6) | 0.21 |
| CV of glucose within day (%) | 41 (40–45) | 39 (38–44) | 0.36 |
| CV of glucose between days (%) | 17 (11–22) | 19 (17–25) | 0.80 |
| Total daily dose (units/day) | 57.3 (45.6–65.2) | 56.6 (44.7–61.3) | 0.55 |
| Total bolus (units/day) | 31.9 (21.2–41.0) | 38.3 (26.4–41.4) | 0.06 |
| Total basal (units/day) | 24.3 (22.8–28.8) | 20.3 (19.1–22.1) | 0.001 |
| CV of basal insulin (%) | 94 (91–103) | 16 (13–26) | <0.001 |
Data are presented as the median (interquartile range) or mean ± SD, unless otherwise indicated.
*Primary end point.
†AUCday, glucose AUC <3.5 mmol/L/day.
Figure 1.
Median (interquartile range) of sensor glucose (top panel) and insulin delivery (bottom panel) levels during closed-loop insulin delivery (solid red line and red-shaded area) and control period (dashed black line and gray-shaded area) from midnight to midnight. The glucose range 3.9–10.0 mmol/L is denoted by horizontal dashed lines (top panel).
Figure 2.
Individual values of mean sensor glucose levels during day-and-night closed-loop study. The size of the bubble indicates the proportion of time spent with low glucose levels <2.8 mmol/L.
There was no difference in glucose variability between study periods as measured by the SD and CV of sensor glucose. Increased time when the glucose level was in the target range and reduced mean glucose level were achieved by closed-loop through the increased variability of basal insulin delivery, but without increasing the total daily insulin dose (P = 0.55). Higher total basal insulin delivery during closed-loop insulin delivery (P = 0.001) was offset by a trend toward lower bolus delivery (P = 0.06), presumably due to lower glucose levels resulting in reduced correction boluses (Table 1).
Daytime and Overnight Glucose Control and Insulin Delivery
Secondary outcomes calculated for daytime and overnight periods are shown in Supplementary Table 2. Daytime and overnight outcomes were similar to outcomes over day-and-night. The proportion of time when the sensor glucose level was in the daytime target range (3.9–10.0 mmol/L) and overnight target range (3.9–8.0 mmol/L) tended to be higher during closed-loop insulin delivery compared with control (daytime 66% [55–68%] vs. 49% [46–51%]; overnight: 63% [49–78%] vs. 40% (30–48%]). The daytime mean glucose levels (9.4 ± 1.2 vs. 10.3 ± 1.4 mmol/L) and overnight mean glucose levels (7.8 ± 1.8 vs. 9.7 ± 1.8 mmol/L) tended to be lower during closed-loop insulin delivery without a difference in total daytime and overnight insulin amount.
Adverse Events
No serious adverse events or severe hypoglycemic episodes were observed during either study period. Two participants measured mild to moderate elevated blood ketone levels (>2.0 mmol/L), which were associated with hyperglycemia, one participant during closed-loop insulin delivery and one participant in the control period. These events were attributed to infusion set failures and were all self-managed.
Utility Analysis
Closed-loop insulin delivery was operational a median of >91% of the time (interquartile range 75–96% of the time). The median availability of sensor glucose was 98% (interquartile range 93–100%) during closed-loop insulin delivery and 97% (interquartile range 92–100%) during the control period. On average, closed-loop insulin delivery was interrupted 1.1 times/subject/day (0.6–1.5 times/subject/day). Apart from two occasions requiring reset of the closed-loop system by the research staff, the participants were able to resolve issues on their own, such as restarting the closed-loop system after the loss of pump connectivity or sensor data unavailability.
Conclusions
To our knowledge, this is the first trial investigating day-and-night application of closed-loop insulin delivery under free-living conditions in adolescents with type 1 diabetes. The results of the current study demonstrate the feasibility of unsupervised free-living home use of 24/7 hybrid closed-loop insulin delivery in this challenging population. The closed-loop system increased the time when the glucose level was in the target range while reducing the mean glucose level. These improvements were achieved without increasing the risk of hypoglycemia and without increasing the total daily insulin dose.
The occurrence of hypoglycemia exposure in the current study was low. Compared with previously published day-and-night adult outpatient studies using single-hormone (32,33) or dual-hormone approaches with glucagon coadministration (27), participants in the current study spent less time at glucose levels <3.9 mmol/L during the control period. During the closed-loop study arm, our results matched the findings observed in adults (Table 2). In our adolescent cohort, the 24/7 hybrid closed-loop insulin delivery system managed to keep the time in hypoglycemia at a low level, while significant reductions in hypoglycemia risk using closed-loop delivery in outpatient settings were observed in more hypoglycemia-prone populations (27,32,33). We instructed study participants to perform a twice-daily calibration check and to recalibrate the sensor when large over-reading occurred but not when under-reading, occurred, to reduce the risk of sensor error–induced hypoglycemia, which is of particular concern during closed-loop insulin delivery.
Table 2.
Comparison of percentage of time spent with glucose levels <3.9 mmol/L during day-and-night closed-loop studies in outpatient settings
| Study population | Settings | Sample size | Intervention period | Time spent at glucose level <3.9 mmol/L (%) |
||
|---|---|---|---|---|---|---|
| Closed-loop | Control | Reference | ||||
| Adults* | Mixed† | 20 | 5 days | 4.1 ± 3.5 | 7.3 ± 4.7 | (27) |
| Adults‡ | Home | 17 | 1 week | 3.1 ± 2.6 | 4.3 ± 3.6 | (33) |
| Adults‡ | Home | 33 | 12 weeks | 3.1 ± 1.9 | 4.3 ± 3.9 | (32) |
| Adolescents‡ | Home | 12 | 1 week | 3.7 ± 2.7 | 3.3 ± 3.7 | Present study |
Data are presented as mean ± SD, unless otherwise indicated.
*Dual-hormone closed-loop vs. usual care (45% of participants used real-time continuous glucose monitoring during usual care).
†Control: home; closed-loop: restricted geographical area during day and hotel overnight.
‡Single-hormone closed-loop vs. sensor-augmented pump therapy.
The advent of novel technologies such as threshold-suspend insulin pump therapy (15) and, more recently, predictive low-glucose suspend (16) may reduce the risk of hypoglycemia. However, these approaches are not designed to increase insulin delivery and do not address the issue of hyperglycemia, which poses major challenges in diabetes management of adolescents. The important advantage of a closed-loop system is highly responsive graduated modulation of insulin delivery both below and above the preset pump regimen, allowing for improvements in time spent with target glucose values and the reduction of mean glucose without increased hypoglycemia.
Closed-loop insulin delivery use and sensor wear were high in our cohort. This may be attributed to the relatively short intervention period and the motivational bias of study participants. These findings are in line with previous observations (31) regarding overnight closed-loop insulin delivery home application over longer intervention periods in adolescents. In terms of psychosocial impact and acceptance, overnight closed-loop technology was well accepted in this age group, with overall benefits outweighing practical challenges, such as technical difficulties, intrusiveness of alarms, and size of the devices (38). Given high closed-loop insulin delivery system use in adolescents, the positive perception of this technology and its benefits in terms of glycemic control demonstrated by the current study, closed-loop insulin delivery represents a promising tool to address glycemic deterioration that is commonly seen in adolescence (7,39).
The strengths of our study include the integration of closed-loop insulin delivery into normal life, including use at school, and during weekends and holidays. The study was performed without remote monitoring or close supervision. No restrictions were imposed on dietary intake, moderate physical activity, or travel. The comparator was “state-of-the-art” sensor-augmented insulin pump therapy. A crossover design had the benefit of each participant acting as his/her own control. Weaknesses include the small sample size, the relatively short study duration, and restricted use of the closed-loop system during strenuous exercise. The current closed-loop prototype system requires participants to wear and carry multiple devices. Further integration of devices may reduce this burden and enhance the usability of closed-loop systems, particularly during physical activity. A more adaptive control algorithm might further enhance daytime benefits.
In conclusion, we have demonstrated that day-and-night hybrid closed-loop insulin delivery can be used safely in adolescents at home without supervision. Its benefits include an increased time when glucose is in the target range and a reduced mean glucose level. Larger and longer studies are warranted.
Supplementary Material
Article Information
Acknowledgments. The authors thank study volunteers for their participation. The authors also thank the staff at the Addenbrooke’s Wellcome Trust Clinical Research Facility for their support. In addition, the authors thank Jasdip Mangat and John Lum (Jaeb Center) for their support of the development and validation of the closed-loop system; Josephine Hayes (University of Cambridge) for administrative support; Karen Whitehead (University of Cambridge) for laboratory support; the staff at Addenbrooke’s Hospital for their support; Sara Hartnell and Sonja Slegtenhorst for study pump training; and The Core Biochemical Assay Laboratory (Keith Burling), University of Cambridge, and the Institute of Life Sciences (Gareth Dunseath), Swansea University, for carrying out the biochemical analyses.
Funding. This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (grant 1R01-DK-085621-01). Additional support for the Artificial Pancreas work was provided by JDRF, National Institute for Health Research Cambridge Biomedical Research Centre, and Wellcome Strategic Award (100574/Z/12/Z). Abbott Diabetes Care supplied discounted continuous glucose monitoring devices, sensors, and communication protocol to facilitate real-time connectivity. Diasend provided discounted platform for data upload.
Duality of Interest. M.T. has received speaker honoraria from Novo Nordisk. M.E.W. has received license fees from Becton Dickinson and has served as a consultant to Becton Dickinson. M.E.W., D.B.D., and R.H. have reported patent applications. R.H. has received speaker honoraria from Minimed Medtronic, Eli Lilly, BBraun, and Novo Nordisk; has served on an advisory panel for Eli Lilly; has received license fees from BBraun and Medtronic; and has served as a consultant to BBraun, Sanofi, and Profil. No other potential conflicts of interest relevant to this article were reported.
Abbott Diabetes Care read the manuscript before article submission. No sponsor had any role in the study design, data collection, data analysis, data interpretation, or writing of the article.
Author Contributions. M.T. codesigned the studies; was responsible for the screening and enrollment of participants; arranged informed consent from the participants; provided patient care and/or took samples; carried out or supported the data analysis, including the statistical analyses; contributed to the interpretation of the results; and wrote the article. J.M.A. was responsible for the screening and enrollment of participants; arranged informed consent from the participants; and provided patient care and/or took samples. M.E.W. codesigned the studies; provided patient care and/or took samples; managed randomization; and carried out or supported data analysis, including the statistical analyses. H.T. codesigned the studies, provided patient care and/or took samples, and contributed to the interpretation of the results. Z.S. provided patient care and/or took samples, and contributed to the interpretation of the results. P.C. and C.K. carried out or supported the data analysis, including the statistical analyses. C.L.A. and D.B.D. codesigned the studies and contributed to the interpretation of the results. R.H. coordinated the studies; codesigned the studies; carried out or supported data analysis, including the statistical analyses; designed and implemented the glucose controller; contributed to the interpretation of the results; and wrote the article. All authors critically reviewed the article, and no writing assistance was provided. R.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Results of this trial were presented as an oral communication at the 75th Scientific Sessions of the American Diabetes Association, Boston, MA, 5–9 June 2015.
Footnotes
Clinical trial reg. no. NCT01873066, clinicaltrials.gov.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc15-2078/-/DC1.
References
- 1.Livingstone SJ, Levin D, Looker HC, et al.; Scottish Diabetes Research Network epidemiology group; Scottish Renal Registry . Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008-2010. JAMA 2015;313:37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steineck I, Cederholm J, Eliasson B, et al.; Swedish National Diabetes Register . Insulin pump therapy, multiple daily injections, and cardiovascular mortality in 18,168 people with type 1 diabetes: observational study. BMJ 2015;350:h3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho YH, Craig ME, Davis EA, et al.; Adolescent Type 1 Diabetes Cardio-Renal Intervention Trial . Cardiac autonomic dysfunction is associated with high-risk albumin-to-creatinine ratio in young adolescents with type 1 diabetes in AdDIT (Adolescent Type 1 Diabetes Cardio-Renal Interventional Trial). Diabetes Care 2015;38:676–681 [DOI] [PubMed] [Google Scholar]
- 4.Maftei O, Pena AS, Sullivan T, et al.; AdDIT Study Group . Early atherosclerosis relates to urinary albumin excretion and cardiovascular risk factors in adolescents with type 1 diabetes: Adolescent type 1 Diabetes cardio-renal Intervention Trial (AdDIT). Diabetes Care 2014;37:3069–3075 [DOI] [PubMed] [Google Scholar]
- 5.Beck RW, Tamborlane WV, Bergenstal RM, Miller KM, DuBose SN, Hall CA; T1D Exchange Clinic Network . The T1D Exchange clinic registry. J Clin Endocrinol Metab 2012;97:4383–4389 [DOI] [PubMed] [Google Scholar]
- 6.Wood JR, Miller KM, Maahs DM, et al.; T1D Exchange Clinic Network . Most youth with type 1 diabetes in the T1D Exchange Clinic Registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes clinical guidelines. Diabetes Care 2013;36:2035–2037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Acerini CL, Williams RM, Dunger DB. Metabolic impact of puberty on the course of type 1 diabetes. Diabetes Metab 2001;27:S19–S25 [PubMed] [Google Scholar]
- 8.Cryer PE. The barrier of hypoglycemia in diabetes. Diabetes 2008;57:3169–3176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burdick J, Chase HP, Slover RH, et al. Missed insulin meal boluses and elevated hemoglobin A1c levels in children receiving insulin pump therapy. Pediatrics 2004;113:e221–e224 [DOI] [PubMed] [Google Scholar]
- 10.Cengiz E, Xing D, Wong JC, et al.; T1D Exchange Clinic Network . Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D Exchange clinic registry. Pediatr Diabetes 2013;14:447–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karges B, Rosenbauer J, Holterhus PM, et al.; DPV Initiative . Hospital admission for diabetic ketoacidosis or severe hypoglycemia in 31,330 young patients with type 1 diabetes. Eur J Endocrinol 2015;173:341–350 [DOI] [PubMed] [Google Scholar]
- 12.Vanderwel BW, Messer LH, Horton LA, et al. Missed insulin boluses for snacks in youth with type 1 diabetes. Diabetes Care 2010;33:507–508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hofer SE, Heidtmann B, Raile K, et al.; DPV-Science-Initiative and the German working group for insulin pump treatment in pediatric patients . Discontinuation of insulin pump treatment in children, adolescents, and young adults. A multicenter analysis based on the DPV database in Germany and Austria. Pediatr Diabetes 2010;11:116–121 [DOI] [PubMed] [Google Scholar]
- 14.Bergenstal RM, Tamborlane WV, Ahmann A, et al.; STAR 3 Study Group . Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med 2010;363:311–320 [DOI] [PubMed] [Google Scholar]
- 15.Bergenstal RM, Klonoff DC, Garg SK, et al.; ASPIRE In-Home Study Group . Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med 2013;369:224–232 [DOI] [PubMed] [Google Scholar]
- 16.Buckingham BA, Raghinaru D, Cameron F, et al.; In Home Closed Loop Study Group . Predictive low-glucose insulin suspension reduces duration of nocturnal hypoglycemia in children without increasing ketosis. Diabetes Care 2015;38:1197–1204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Langendam M, Luijf YM, Hooft L, Devries JH, Mudde AH, Scholten RJ. Continuous glucose monitoring systems for type 1 diabetes mellitus. Cochrane Database Syst Rev 2012;1:CD008101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hovorka R. Closed-loop insulin delivery: from bench to clinical practice. Nat Rev Endocrinol 2011;7:385–395 [DOI] [PubMed] [Google Scholar]
- 19.Breton M, Farret A, Bruttomesso D, et al.; International Artificial Pancreas Study Group . Fully integrated artificial pancreas in type 1 diabetes: modular closed-loop glucose control maintains near normoglycemia. Diabetes 2012;61:2230–2237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atlas E, Nimri R, Miller S, Grunberg EA, Phillip M. MD-logic artificial pancreas system: a pilot study in adults with type 1 diabetes. Diabetes Care 2010;33:1072–1076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hovorka R. Artificial Pancreas Project at Cambridge 2013. Diabet Med 2015;32:987–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Castle JR, Engle JM, El Youssef J, et al. Novel use of glucagon in a closed-loop system for prevention of hypoglycemia in type 1 diabetes. Diabetes Care 2010;33:1282–1287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Russell SJ, El-Khatib FH, Nathan DM, Magyar KL, Jiang J, Damiano ER. Blood glucose control in type 1 diabetes with a bihormonal bionic endocrine pancreas. Diabetes Care 2012;35:2148–2155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kovatchev BP, Renard E, Cobelli C, et al. Feasibility of outpatient fully integrated closed-loop control: first studies of wearable artificial pancreas. Diabetes Care 2013;36:1851–1858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phillip M, Battelino T, Atlas E, et al. Nocturnal glucose control with an artificial pancreas at a diabetes camp. N Engl J Med 2013;368:824–833 [DOI] [PubMed] [Google Scholar]
- 26.Ly TT, Breton MD, Keith-Hynes P, et al. Overnight glucose control with an automated, unified safety system in children and adolescents with type 1 diabetes at diabetes camp. Diabetes Care 2014;37:2310–2316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Russell SJ, El-Khatib FH, Sinha M, et al. Outpatient glycemic control with a bionic pancreas in type 1 diabetes. N Engl J Med 2014;371:313–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haidar A, Legault L, Matteau-Pelletier L, et al. Outpatient overnight glucose control with dual-hormone artificial pancreas, single-hormone artificial pancreas, or conventional insulin pump therapy in children and adolescents with type 1 diabetes: an open-label, randomised controlled trial. Lancet Diabetes Endocrinol 2015;3:595–604 [DOI] [PubMed] [Google Scholar]
- 29.Nimri R, Muller I, Atlas E, et al. MD-Logic overnight control for 6 weeks of home use in patients with type 1 diabetes: randomized crossover trial. Diabetes Care 2014;37:3025–3032 [DOI] [PubMed] [Google Scholar]
- 30.Thabit H, Lubina-Solomon A, Stadler M, et al. Home use of closed-loop insulin delivery for overnight glucose control in adults with type 1 diabetes: a 4-week, multicentre, randomised crossover study. Lancet Diabetes Endocrinol 2014;2:701–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hovorka R, Elleri D, Thabit H, et al. Overnight closed-loop insulin delivery in young people with type 1 diabetes: a free-living, randomized clinical trial. Diabetes Care 2014;37:1204–1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thabit H, Tauschmann M, Allen JM, et al.; APCam Consortium; AP@home Consortium . Home use of an artificial beta cell in type 1 diabetes. N Engl J Med. 2015;373:2129–2140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leelarathna L, Dellweg S, Mader JK, et al.; AP@home Consortium . Day and night home closed-loop insulin delivery in adults with type 1 diabetes: three-center randomized crossover study. Diabetes Care 2014;37:1931–1937 [DOI] [PubMed] [Google Scholar]
- 34.Elleri D, Allen JM, Biagioni M, et al. Evaluation of a portable ambulatory prototype for automated overnight closed-loop insulin delivery in young people with type 1 diabetes. Pediatr Diabetes 2012;13:449–453 [DOI] [PubMed] [Google Scholar]
- 35.Hovorka R, Shojaee-Moradie F, Carroll PV, et al. Partitioning glucose distribution/transport, disposal, and endogenous production during IVGTT. Am J Physiol Endocrinol Metab 2002;282:E992–E1007 [DOI] [PubMed] [Google Scholar]
- 36.Wilinska ME, Budiman ES, Taub MB, et al. Overnight closed-loop insulin delivery with model predictive control: assessment of hypoglycemia and hyperglycemia risk using simulation studies. J Diabetes Sci Technol 2009;3:1109–1120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilinska ME, Chassin LJ, Acerini CL, Allen JM, Dunger DB, Hovorka R. Simulation environment to evaluate closed-loop insulin delivery systems in type 1 diabetes. J Diabetes Sci Technol 2010;4:132–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnard KD, Wysocki T, Allen JM, et al. Closing the loop overnight at home setting: psychosocial impact for adolescents with type 1 diabetes and their parents. BMJ Open Diabetes Res Care 2014;2:e000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diabetes Control and Complications Trial Research Group Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr 1994;125:177–188 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.