Abstract
This report describes the proposed intervention and outcome measurement procedures for the Pathways study. Pathways is a multicenter school-based study aimed at reducing the alanning increase in the prevalence of obesity in American Indian children. It is designed as a randomized clinical trial, involving approximately 2,00 third grade children in 40 schools in seven diferent American Indian communities. During a 3-year feasibility phase, which was just completed, the major components of the intervention (school food service, classroom curriculum, physical education program, and family involvement) were developed and pilot-tested. The measurement instruments for body composition; physical activity; dietary intake; and knowledge, attitudes, and behavior were also developed and validated. Comprehensive process evaluation procedures also were defined. As of this writing, thefull-scale intervention program is being initiated and is scheduled to be completed in the spring of 200. The primary aim of the Pathways intervention is to reduce average percent body fat in intervention-school children by at least 3% compared with control-school children by the end of the 3-year intervention. This goal is to be achieved primarily by an increase in physical activity and a reduction in the perceni of dietary fat intake. The program does not seek to reduce dietary energy intake. Rather, it is based on the assumption that a healthier; lower-fat diet, combined with an increase in energy expenditure by increased physical activity, will result in fewer excess calories deposited as body fat.
Keywords: obesity, prevention, schoolchildren, American Indians
Introduction
Obesity is one of the major public health problems in the United States and in most developed countries. Recent surveys indicate that the number of U.S. children and adolescents with body mass index (BMI) above the 85th percentile has increased from 15% in 1965 to 22% in 1991.1 Although the tracking of childhood obesity into adulthood varies at different times, it is known that over 80% of severely obese adults were obese during late childhood and adolescence.2 Furthermore, several lines of evidence suggest that obesity during adolescence may have long-lasting adverse effects on health even when body weight returns to normal after adolescenc3
American Indian children and adults suffer obesity in much higher proportion than any other group in the United States. The prevalence of overweight (defined as a BMI >85th percentile of National Health and Nutrition Examination Survey [NHANES II] reference population) in American Indian adults is 34% for men and 40% for women, higher than the U.S. rates of 24% and 25%, respectively.4 The prevalence in 5- to 17-year-old American Indian children is shown in Figure 1 (compiled and distributed by Indian Health Service areas). There is evidence of a secular increase in obesity among American Indians over the past 30 to 40 years.5 A dramatic increase in obesity among Pima Indians born after World War II was documented by Price et al.6 in 1993. A comparison of weight for height of Pima children also shows ·a major increase relative to earlier generations: a boy of 165 cm of stature today weighs 69 kg, compared with 58 kg for the same height in 1905.7 In another survey the increase in height and weight among Navajo boys between 1955 and 1989 was 6.1% and 28.8%, respectively.8
Figure 1.
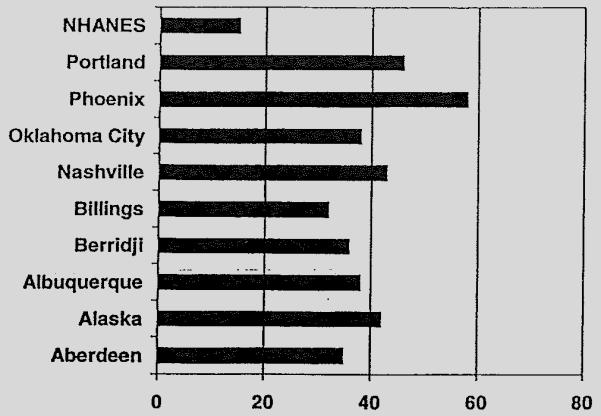
Prevalence of obesity (body mass index above the 85th NHANES percentile) in American Indianchildren ages 5 to 17-years-old, by Indian Health Service area. Data from the Indian Health Service, 1995.
This epidemic of obesity among American Indians is a relatively new phenomenon. Early accounts of life among several tribes in the Southwest do not mention overweight as a characteristic of these populations.9 More specifically, a 1972 survey of White Mountain Apache children in Whiteriver, Arizona, reported that only 8% of children were above the 85th centile for BMI,10 whereas studies in the same community and age group in 1992 found that 35% of children were in that category.11
There have been obvious changes in lifestyle in American Indian communities that can be linked to the epidemic of obesity: an increasingly sedentary lifestyle, increase in consumption of high-fat foods, and less opportunities for recreational activities for children and young adults.
Goals of the Pathways study
The Pathways study’s aim is to develop, implement, and evaluate a school-based intervention for the primary prevention of obesity in American Indian children. That aim will be achieved by increasing moderate to vigorous physical activity, reducing fat content of school meals, and promoting healthier dietary practices at school and at home. The main outcome variable will be percent body fat (PBF) in intervention and control schools. Secondary aims will evaluate the impact of the intervention on physical activity level, dietary fat intake, and knowledge, attitudes, and behaviors related to food choices and physical activity. An extensive process evaluation plan will document the degree to which the intervention was implemented. Finally, data will be collected to monitor the safety of the intervention. These data will be reported regularly to an external monitoring board.
The Pathways project is divided in two phases: a 3-year feasibility phase, which is being completed as of this writing, and a 5-year, full-scale study, which began in the fall of 1997. The objectives of the feasibility phase were (1) to assess the acceptability and support from parents, students, and school and tribal authorities for a comprehensive, school-based program for the prevention of obesity in elementary schoolchildren; (2) to develop and pilot-test the different components of the intervention; and (3) to develop and test approaches and methods for measurement of primary and secondary endpoint variables. It was anticipated that the feasibility phase also would provide an opportunity for establishing strong links with schools and community leaders, and develop a field research team comprised of local American Indians with strong ties with the community.
The present report describes the development and validation activities carried out during the feasibility phase and the resulting components and procedures included in the final protocol for the full-scale intervention.
Pathways is based on a partnership between five universities and seven American Indian communities: Gila River Indian Community, Tohono O’odham (University of Arizona); White Mountain Apache, San Carlos Apache (Johns Hopkins University); Oglala Lakota. Sicangu Lakota (University of Minnesota); and Navajo (University of New Mexico). The University of North Carolina-Chapel Hill is the coordinating center for the study. The project is directed by a steering committee that is comprised of principal investigators from the grantee institutions, the National Institutes of Health (NIH) project office, and two Arnerican-Indian representatives from the tribes involved.
The study protocol underwent an extensive review and approval process, which included the approval from the institutional review boards of each participating institution, the tribal health authorities and councils, school boards, and an external Protocol Review Committee. In addition, written, informed consent and child assent was obtained for activities involving direct interaction with children, such as measurements and survey questionnaires.
Full-scale study design
The proposed full-scale study is a randomized clinical trial involving 40 schools serving American Indian children in seven commumties. For randomization, schools will be stratified within each field site based on median PBF, measured in children at the end of the second grade. Schools will be ranked at each field site based on their median PBF, and divided in two strata: higher and lower PBF, each containing half the schools of each field site. The study coordinating center will then randomly assign half of the schools within each stratum to intervention and half to control groups. The intervention will begin in children entering third grade in the fall of 1997 and will continue with this cohort until they complete the fifth grade in the spring of 20. The unit of analysis is the school and the primary outcome variable will be the school’s mean PBF, adjusted for baseline PBF.
Eligibility criteria for schools include: (1) third grade enrollment is at least 15 children; (2) 90% or more third grade children are American Indians; (3) the average retention from third to fifth grade over the past 3 years is at least 10%; (4) the school has its own cafeteria and provides lunch on site; (5) the school environment includes the minimum resources to implement the physical activity program; and (6) it is anticipated that the school will remain open and independent for the duration of the study.
Fonnative research
Formative research aims to understand the context of an intervention and the specific behaviors that may be of concern. In Pathways, extensive formative research was conducted in each of the participating communities, and constituted the basis to identify and prioritize risk factors for obesity and potential opportunities for enhancing program delivery.12 Having to develop a common intervention across different American Indian communities posed an additional challenge and emphasized the importance of the formative research phase.
Data was collected with a combination of qualitative and quantitative techniques, which included in-depth interviews, semi-structured interviews, focus groups, and direct observation. Respondents included students, teachers, food service staff, administrators, parents, and community members. Interviewers encouraged people to openly express their views, concerns, and needs on a wide range of issues related to health and nutrition. Quantitative information permitted an objective comparison across sites in terms of school resources, dietary practices, and presence of factors that might constrain the implementation of the intervention. Both qualitative and quantitative data were integrated by means of a conceptual and procedural model. Risk behaviors were scored and prioritized, and common patterns across sites were identified and linked to the intervention development. A major contribution of the formative research data was to identify and prioritize those risk factors, permitting a more targeted development of the intervention (Table 1).
Table 1.
Selected risk factors for obesity in American Indian children: Data from the formative research of Pathways feasibility phase
| High priority |
| Eat a lot of high-fat foods (S, H) |
| Encouraged to finish all their foods (S, H) |
| Have few opportunities to be physically active (S, H) |
| Watch a lot of TV, movies (S, H) |
| Eat seconds of high-fat foods (S) |
| Moderate priority |
| Eat a lot of fast foods outside school/home |
| Eat a lot of high-fat snacks (S, H) |
| Foods high in fat and sugar used as reward (S, H) |
| Eat lunch too quickly (S) |
| Not consuming enough fruits and vegetables (S, H) |
S—school. H—home.
Development of the intervention
Although a number of studies have examined the relationship of obesity to chronic diseases, 13,14 we are not aware of previous large-scale trials for the primary prevention of obesity in children. School-based interventions such as the Children and Adolescent Trial for Cardiovascular Health (CATCH) study have focused on cardiovascular health and have documented several effective approaches to reduce risk factors in school-age children.15 Building on previous studies, indigenous beliefs and values of participating American Indian nations were incorporated to create a program that supports healthier lifestyles and reflects those in the nations’ traditional cultures. 16,17
The Pathways intervention combines elements of social learning theory (SLT) with the rich cultural heritage of American Indians in regard to physical activity and nutritious foods.19 By taking a holistic approach, the intervention aims to positively influence individual, behavioral, and environmental risk factors associated with obesity, particularly physical activity and eating behavior. Pathways seks to enhance children’s knowledge about physical activity- and food choices, their values about health and nutrition, and their sense of personal control over their activity. By providing more opportunities for exercise and for healthier food. choices, the intervention also promotes changes in the children's environment that support healthful dietary and activity practices. It attempts to influence families' food selections, tries to reduce the barriers to exercise and healthful eating, and creates per support for exercising and selecting lower fat foqds. Changes in children's behayioral attributes are promoted by adding to their repertorre of activities and food choices, and by developing skills for the practice of regular activities and for healthy food preparation. The intervention also aims to enhance children's ability for self-monitoring and goal setting.
The intervention design takes into account the specific learnmg patterns common to most native cultures. 17,20 These learning modes are crucial elements for the success of the intervention. These indigenous learning modes include learning through observation and practice, learning from storytelling, learning metaphorically, holistic learning learning by trial and error, learning through play, learning cooperatively, and learning thrQugh reflection. These modes were incorporated in the process of delivery of each component of the intervention.
To ensure that the content of the intervention was acceptable to all participating tribes, all working groups developing each component ihcluded Amencan Indian representatives from each site. In addition, the study Steering Committee, which made the final decisions regarding the study, included two American Indian representatives, elected by all American Indians in Pathways. Furthermore, regular interaction with teachers, parents, and tribal authorities provided useful opportunities for feedback on the content of the intervention and on the other components of the study.
Components of the intervention
The Pathways intervention targets four areas: (1) classroom curculum, (2) physical activity, (3) school food service, and (4) family involvement (Table 2).
Table 2.
Summary of the Pathways intervention
| Component | Objective | Content |
|---|---|---|
| Classroom curriculum |
|
|
| Food service |
|
|
| Physical activity |
|
|
| Family |
|
|
Classroom curriculum
The Pathways curriculum targets children in the third, fourth, and fifth grades, and consists of culturally appropriate school-based lessons that promote healthful eating behaviors and increased physical activity. A culturally appropriate activity or lesson we defined as one acceptable to all the tribes participating in the study from the standpoint of cultural traditions and beliefs. The program is structured in two 45-minute classroom sessions per week for a total of 12 weeks. The sequence integrates several social learning constructs into a series of stories and activities linked through two fictional American Indian children, Amanda and Daryl White Horse, on their journey through the seven Pathways nations. By storytelling and associated activities, children are given the oppoi:tunity to identify with the main characters and to model their healthy behaviors. During the course of the 12 weeks, students taste-test new foods and beverages and practice behaviors related to the goals for healthful eating and physical activity.
An important objective of the Pathways curriculum is to create an integrated school environment in which teachers, food service personnel, physical educators, and the students’ families work together toward the common goal of practicing and sustaining the new behavioral skills introduced by the curriculum.
Physical activity
Although there are only limited data on level of physical activity in children,21 it is generally acknowledged that sedentary lifestyle is an important contributor to the development of obesity, both in children and adults.22,23 Conversely, it has been shown that reducing sedentary activities24 or increasing moderate to intense physical activity leads to significant reductions in PBF in children, without affecting lean body mass.25 School-based physical activity programs aimed at elementary schoolchildren have been successful in increasing level of activity during school time.26
The Pathways physical activity component aims at increasing energy expenditure during school time by increasing the frequency and quality of physical education classes and by introducing classroom activity breaks and encouraging play during recess periods. Three main considerations guided the development of this component: (1) to develop moderate-to-high levels of physical activity for all children, regardless of skill level; (2) to promote health-related fitness through aerobic activities and allow for sports skill development to enhance success and enjoyment of activities; and (3) to be as simple and as easy to implemeqt as possible, not only by a physical education specialist but by classroom teachers as well. The Pathways physical education intervention is modeled after the SPARK program (Sports, Play and Active Recreation for Kids), which has been successfully implemented in earlier school-based health programs.27 The Pathways physical education program aims at increasing physical activity for both motor skill development and fitness lessons. Although the SPARK program was not originally developed for American Indian children, our process evaluation data and pilot tests indicated that American Indian children enjoyed SPARK activities.
In addition to SPARK-based physical education, the Pathways physical activity intervention includes a unit of American Indian games derived from traditional games from each of the Pathways nations. The unit may be used in a variety of ways; by including it in physical education classes, or during recess or other active times.
The Pathways physical activity intervention is divided into 14 type I units (health-related fitness units) and 10 type II units (sport-related fitness units). Other modules include warm-up/cool-down activities, conditioning exercises, inclement weather activities, and American Indian games. The range of activities in units allows for the implementation of the program in a variety of school settings, even those with limited space or equipment. Type I unifs focus on the development of muscular strength and locomotor and nonlocomotor skills. Type II units emphasize development of sport-related skills, especially those with potential for future sports participation in the community. The goal of the intervention is to deliver a minimum of three 30-minute sessions per week. Training for physical education teachers will be offered at the beginning of the spring, fall, and winter periods.
The impact of increased physical activity at the school on total daily energy expenditure can be significant. We estimated that four to five 30-rninute sessions per week would represent over 11,000 kcal over the school year, roughly equivalent to a reduction of 3 lb of body fat.
Food service intervention
The school cafeteria is a major source of daily energy intake for American Indian children attending elementary schools. The U.S. Department of Agriculture (USDA) School Lunch and Breakfast programs provides lunch and breakfast to approximately 25 million children every day, and is free for low-income families. Based on the calorie targets for breakfast and lunch set by the USDA and on attendance records from the school cafeterias, it can be estimated that children attending schools in American Indian communities consume as much as 60% of their daily caloric intake at the school. Thus, school food service provides a good opportunity to introduce healthful food choices.
The main goal of the Pathways food service intervention is to lower the amount of fat in breakfast and lunch meals. Although some studies question the efficacy of reducing dietary fat intake as a means of reducing obesity in adults, other studies have shown a positive correlation between fat intake and measures of body fatness.28 In children, diet energy density, which is largely determined by fat content, is an important determinant of total energy intake. The aim of the food service intervention is to reduce the percent of calories from fat to no more than 30% of the total, which is consistent with general guidelines for this age group. In addition to setting nutrition guidelines, the Pathways program introduces behavioral guidelines for the food service personnel that are aimed at changing and/or enhancing their skills in the planning, purching, preparation, and serving of meals. All food service staff will be trained in the implementation of these nutrient and behavioral guidelines, and the program will be supported by and monitored through periodic visits by a Pathways nutrition specialist
To evaluate the potential impact of the Pathways food service intervention, a theoretical analysis of the nutrient content of 1 week of breakfast and lunch menus from three schools was conducted. The food service staff compiled the menus, which were analyzed using the Nutrition Data System (NDS) at the Nutrition Coordinating Center (NCC) of the University of Minnesota.29 Two of the three schools averaged 34% and 40% calories from fat, and at lunch all three schools averaged 40% or 45% calories from fat. Applying all Pathways food service guidelines, fat content was reduced to 30% or less at breakfast in all three schools. Fat calories at lunch were reduced to 30% or less in one school and to 32 to 33% in the other two. The overall calories from fat at al three schools averaged 31%.
Family intervention
This component of the intervention has the objective of keeping families informed of and involved with the program’s mission and activities, thus reinforcing the health behaviors introduced in the classroom and in the food service and physical activity components. Although our intervention is essentialy school-based, we seek to extend positive health behaviors to children’s family members as much as possible. Positive health practices in the household will lead to a supportive environment for the child, facilitating their own efforts to make those behavioral changes. The two activities for the family component of the third grade intervention include:
-
Family Packs, which consist of take-home materials linked to the classroom curriculum. Action Packs include printed material that promotes family activities related to physical activity and cooking healthy foods. Snack Packs include locally available, low-fat, low-sugar food items for the student to share with his or her family. These Family Packs are linked to the other components of the intervention and carry on the Pathways story line and health messages presented in the classroom curriculum.
To evaluate the rate of participation, each Family Pack includes a return card, which is to be completed by an adult family member. The return cards provide feedback on specific Family Packs and on the overall impression of the family intervention.
-
Family events, which are family gatherings at the school. The Family Fun Night is in the format of an educational fair and involves families (parents, guardians and/or extended family), students, teachers, and school and tribal administrators. Events will be advertised in literature accompanying Family Packs and in the classroom. Examples of activities to be included in Family Fun Night are interactive booths for taste-testing of low-fat and high-fat foods items, fishing for fruit in a barrel of water, country line dancing, relay races, and distribution of educational materials. A low-fat meal that incorporates traditional American Indian foods also will be served. Attendance and level of participation will be monitored at the entrance and by a registration card given to each attendee to record activities in which they participate.
Another family event, the Family Celebration, consists of a demonstration of Pathways physical activity components by children to parents. Two activities are selected for presentation, giving children and parents an opportunity to share their knowledge and skills.
Development of measurement procedures
During the feasibility phase, instruments and procedures for endpoint and interim measurements were developed. As stated above, the endpoint measure for the study will be PBF, which will be determined by a combination of anthropometric and bioelectrical impedance measurements. Other measurements planned for the full-scale study include knowledge, attitudes and behavior, physical activity (by motion sensor and questionnaire), and dietary intake (by direct observation and 24-hour dietary recall).
Body composition
During the feasibility phase, an approach to assess body fatness in American Indian children was developed.30 Using isotopic dilution as the reference standard, a specific equation to estimate body fat was developed, based on a combination of anthropometric measurements and bioelectrical impedance. Initial variables included six skinfolds, waist circumference, weight and height, and resistance and reactance. Using a stepwise logistic procedure, a regression model was developed to provide optimal predictability with the minimum number of measurement variables. The resulting equation, using bioelectrical impedance, weight, and tricipital and subscapular skinfold, predicts PBF with a root mean square error of 3.2%:30
The following equation was also developed to allow for the estimation of PBF from available BMI data, for comparison purposes:
Project field workers from all sites were trained at one central location. Separate reliability studies were performed after training. Intraclass correlation coefficients were calculated from pooled data from all trainers using a random effects model. A full set of anthropometric measurements is planned at baseline and at the end of the study. Body weight and height will be collected annually during the study, with the purpose of monitoring the safety of the intervention.
Physical activity
The technical difficulty in measuring free-living physical activity in children has limited the available data on this important component of energy balance.31-33 Obtaining quantitative and qualitative information on children’s activity pattern and intensity is essential to evaluate the physical activity component of the Pathways intervention. A number of methods were considered, including heart rate rnonitoring,34,35 doubly labeled water,36–37 and direct observation. The two first methods were ruled out due to cost and parents’ concern regarding attaching electrodes to children (heart rate monitoring) and ingestion of an isotope (although nonradioactive), respectively. Direct observation was considered too intrusive, particularly for after-school monitoring of activity. In the end, two methods for measurement of physical activity were evaluated and adopted: a specially designed 24-hour physical activity recall questionnaire (PAQ), which assesses frequency and type of activities, and a tri-axial accelerometer (Tritrac R3D Research Ergometer) to assess amount of activity.
The Pathways PAQ is adapted from other questionnaires used in studies of children and adolescents.38,39 It uses a checklist format to assess physical activity during the preceding 14 hours and is self-administered in groups. Information obtained by the PAQ includes the number of activities before, during, and after school, and the frequency of different types of activities. The intensity of activities can be estimated by using published metabolic equivalent units values for each activity. The PAQ was pilot-tested in 117 third grade children in six of the participating communities.
The second method adopted for physical activity measurement is the TriTrac R3D ergorneter (Hemokinetics, Inc., Madison, WI USA). As a tri-axial accelerometer (as opposed to the earlier, two-axial model CalTrac), TriTrac is capable of measuring acceleration in three planes and thus is more sensitive to horizontal movement.40–41 Other advantages include small size (4.3″ × 2.7″ × 1.3″), light weight (6 oz), and solid-state circuitry with no external controls, making it more tamper-proof. The device can accumulate up to 14 days of minute-by-minute activity recordings. A proprietary software program permits downloading of data from the device into a desktop computer and standard spreadsheets for detailed analysis. The TriTrac device was tested in 80 of the 117 children who participated in the PAQ pilot study. Data were collected over two consecutive days following a standard protocol. A comparison between average vector magnitudes by TriTrac and PAQ activity indexes was performed using Spearman rank order correlations. Results showed low correlations for before school and after school periods, averaging approximately r = 0.15, and somewhat higher correlations for the period of time during school (r = 0.41). These figures are consistent with previously reported data in older children, ranging from approximately r = 0.3 to r = 0.4.40 It is known that questionnaires give useful information regarding frequency and type of activities, but are of limited value for identifying individual differences in activity. The most important information provided by Tritrac data will be intensity and patterns of activity throughout the day, including before and after school times.
Dietary assessment
The avaHability of appropriately validated instruments for the assessment of dietary intake in children is limited. Specifically, we are not aware of questionnaires developed for use in-elementary school American Indian children. The reliability of adequate survey instruments as well as the accuracy of food composition databases are also limiting factors. Direct observation is a good and reliable alternative to dietary recall,47 but may be too intrusive to be used in the household. However, collecting data on food intake during school time is important in the context of Pathways because (1) a significant percent of total daily calories are consumed at school and (2) the dietary intervention aims primarily at changing intake of foods served at the school. Thus, we adopted direct observation as one of the means to assess dietary intake in children, but limited its use to school time: A random sample of 15 third grade children will be selected at each school for direct observation. Trained observers will record students' food consumption during lunch time at the school’s cafeteria. At the end of the observation period, all food items left on the tray will be measured.
The amount and type of food consumed after school is obviously important as well. Although our program is school-based, it includes as one objective positively modifying eating patterns at home by providing opportunities for family members to try new foods and learn and use healthy culinary practices. The 24-hour dietary recall is considered the best approach for estimating total dietary intake in populationgroups.43 During the Pathways feasibility phase, a food record-assisted 24-hour recall was validated relative to direct observation. Percent calories from fat in breakfast and lunch by the recall method had a good correlation (r = 0.72) with direct observation. The recall method also was shown to be acceptable to children. The procedures for data collection, training, and eertification were also developed, following the guidelines and instruments of the NCC. Because of the cost, this method will be used only for follow-up measurement of dietary intake.
Dietary assessment also will indude menu analysis. Data on menus, recipes, and food vendor information will be systematically collected from all schools participating in the full-scale study. This data will be collected at baseline, annually, and at the end of the study. Results will be used to assess the impact of the intervention on dietary energy intake, percent of calories from fat, and other diet-related variables.
Knowledge, attitudes, and behavior
Although the central outcome measure of the Pathways intervention will be body composition changes, determining the impact of the program on behavior and attitudes related to health and nutrition will be important to assess the effectiveness and cultural appropriateness of intervention components. Earlier studies focusing on grade-school children have relied on self-reported measures to assess changes in knowledge, attitudes, and behavior. In the CATCH study, knowledge and self-efficacy ?out healthful eating in third, fourth, and fifth grade chilClren were measured using a classroom-administered questionnaire.44,45 Follow-up studies in that same cohort confirmed the validity of selfreported knowledge, attitudes, and behavior assessment.46,47 Based on thqs? and other similar findings, our preliminary conclusion is that a self-reported, classroomadministered questionnaire would be a valid tool for use in the Pathways Study.
The Pathways questiqnnaire regarding knowledge, attitudes, and behavior is focused on healthy eating and physical activity. Several previously deveioped instruments were adapted for use, and a few previously tested questions were used intact. However, most of the components of the questionnaire had to be created. The Pathways questionnaire needed to be culturally and developmentally appropriate for third to fifth grade American Indian children and targeted to test the Pathways intervention. The diet-related component of the questionnaire explores what are considered to be determinants of risk behaviors underlying obesity. It also is based on those changes emphasized in the intervention, such as reducing dietary fat intake and consumption of sugary drinks. Target outcomes include knowledge of high-fat foods, self-efficacy to make healthy food choices, perceived social support for eating healthful foods, and intentions to choose healthful foods. The physical activity portion of the questionnaire covers four categories of factors: physical activity self-efficacy, social support for physical activity, perceived barriers to activity, and physical self-perception.
Starting from a set of 248 questions, the instrument used to measure knowledge, attitudes, and behavior was eventually reduced to 170 questions. Further. reductions in this total are anticipated before its final fonn?is defined for the full-scale study. Face validity was tested in a pilot study involving 32 children, and using 64 questions, in a semistructured interview format. A larger subset of 130 questions was subsequently pre-tested in two classrooms at one of the field centers.
Process evaluation
The goals of process evaluation are to link impact and outcome data to intervention activities, to help interpret the mechanisms causing observed changes brought about by the intervention.48,49 This measurement activity will be an important component of the full-scale assessment. Process evaluation will provide the basis for determining the degree of implementation of the program and the type of constraints that individual activities face within the school environment. Therefore, it is closely associated with quality control activities.
During the feasibility phase, the scope of process evaluation activities was defined, and the instruments for data collection were developed and tested.
The Pathways process evaluation is based on dissemination and diffusion theory, SLT, and the desire for triangulation of multiple modes of data collection. The process evaluation will systematically document (1) the training process and content; (2) the implementation of the intervention components within and between sites; (3) the attitudes of school personnel to the intervention; (4) the exposure of staff, family, and students to the intervention components; and (5) the role of the field personnel and other conditions affecting the implementation of the intervention at each site.
Safety
During the Teasibility phase there were no major concerns about the potential adverse effects of the intervention, because only limited components were implemented for short periods of time. However, for the 3-year full-scale intervention, the possibility of adverse effects should be considered. Although the Pathways program is not aimed at reducing total dietary energy intake, it is possible that reductions in the energy density of food items, due to their reduction in fat content, may lead to a decrease in the total daily energy intake. Combined with an increased energy expenditure caused by the physical education component of the program, this could theoretically lead to a negative energy balance and the consequent deceleration of growth velocity.
The Pathways food service intervention aims at providing a diet with no more than 30% of total calories derived from fat The data from menu analysis in the feasibility phase indicate that a full implementation of the Pathways program may result in diets having fat-derived calories as low as 25 to 28%. Thus, one safety consideration is whether any adverse effect might be expected from this change. In the Dietary Intervention Study in Children (DISC) study,50 dietary energy from fat was reduced from 33 to 34% at baseline to 28% at follow-up, although total caloric intake remained the same. Measurements at 1 year and at the end of the 3-year follow-up showed no differences in height, body weight, BMI, or sum of skinfolds between intervention and control groups. In the Bogalusa longitudinal study, there were no differences in weight or height between children consuming 30% or less calories from fat, compared with those consuming more than 30.52 These results, along with the expert views of a number of committees and organizations, indicate that the reduction in percent of dietary fat-derived calories is not necessarily associated with adverse effects on growth. Of course, the Pathways food service intervention will comply with all dietary guidelines for healthy children regarding total calories and macronutrient and micronutrient levels.
Conclusions
During the feasibility phase, the four components of the intervention and the instruments for measurement were developed. Pilot tests were performed to validate the use of these instruments in elementary school American Indian children. The feasibility phase also allowed for the development of stable field teams and for building a close working collaboration with school staff and educational and tribal authorities.
Acknowledgments
We would like to extend our sincere appreciation to the children, parents foachers, and staff from the schocls that participated in the feasibility phase: Cibecue Community School, John F. Kennedy Elementary School, St. Peter Mission Indian School, San Xavier Convent School, Mesa Elementary School, Todd County School District, North Elementary School, HeDog School, Wimnded Knee School, and Lukachukai Boarding School.
This paper was delivered at the October 23-25, 1997, conference “The Determination, Treatment, and Prevention of Obesity,” which was sponsored by the Institute of Nutrition, University of North Carolina at Chapel Hill; Department of Nutrition, Schdl of Public Health and School of Medicine, University of North Carolina at Chapel Hill; and School of Medicine, East Carolina University, in cooperation with the North American Association for the Study of Obesity, the National Institutes of Health, the American Cancer Society, and Eli Lilly & Company.
Supported by grants UOI-HL-50869, U01-HL-50905, UDI-HL-50867. U01-HL-50905, U01-HL-50907, and U01-HL-50885 from the National Heart, Lung, and Blood Institute, National Institutes of Health.
References
- 1.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents: The National Health and Nutrition Examination Surveys, 1963 to 1991. Arch. Pediatr. Adolesc. Med. 1995;149:1085–1092. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- 2.Dietz WH. Implications and treatment of adolescent obesity. Clin. Nutr. 1985;4:103–108. [Google Scholar]
- 3.Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. N. Engl. J. Med. 1992;327:1350–1355. doi: 10.1056/NEJM199211053271904. [DOI] [PubMed] [Google Scholar]
- 4.Broussard BA, Johnson A, Himes JH, Story M, Fichtner R, Hauck F, Bachman-Carter K, Hayes J, Frohlich K, Gray N, et al. Prevalence of obesity in American Indians and Alaska Natives. Am. J. Clin. Nutr. 1991;53(suppl. 6):1535S–1542S. doi: 10.1093/ajcn/53.6.1535S. [DOI] [PubMed] [Google Scholar]
- 5.Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults: The National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994;272:205–211. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- 6.Price RA, Charles MA, Pettitt DJ, Knowler WC. Obesity in Pima Indians: Large increases among post-World War II birth cohorts. Am. J. Phys. Anthropol. 1993;92:473–479. doi: 10.1002/ajpa.1330920406. [DOI] [PubMed] [Google Scholar]
- 7.Knowler WC, Pettt DJ, Saad MF, Charles MA, Nelson RG, Howard BV, Bogardus C, Bennett PH. Obesity in the Pima Indians: its magnitude and relationship with diabetes. Am. J. Clin. Nutr. 1991;53(suppl. 6):1543S–1551S. doi: 10.1093/ajcn/53.6.1543S. [DOI] [PubMed] [Google Scholar]
- 8.Sugarman JR, White LL, Gilbert TJ. Evidence for a secular change in obesity, height, and weight among Navajo Indian schoolchildren. Am. J. Clin. Nutr. 1990;52:960–966. doi: 10.1093/ajcn/52.6.960. [DOI] [PubMed] [Google Scholar]
- 9.Schwatka F. Among the Apaches. The Filter Press; Palmer Lake, CO, USA: 1974. [Google Scholar]
- 10.Owen GM, Gar PJ, Seymoure RD, Harrison GG, Acosta PB. Nutrition studies with White Mountain Apache preschool children in 1976 and 1969. Am. J. Clin. Nutr. 1981;34:266–277. doi: 10.1093/ajcn/34.2.266. [DOI] [PubMed] [Google Scholar]
- 11.Nelson DM. Height and weight changes among White Mountain Apache children. The HIS Provider. 1994 Mar;:50–55. [Google Scholar]
- 12.Gittelsohn J, Evans M, Helitzer D, Anliker J, Story M, Metcalfe L, Davis S, Iron Cloud P. Formative research in a school-based obesity prevention program for Native American schoolchildren (Pathways) Health Ed. Res. 1998;13:251–265. doi: 10.1093/her/13.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Surgeon General’s Report on Nutrition and Health. U.S. Department of Health and Human Services; Washington, DC, USA: 1988. (DHHS publication no. (PHS) 88-50210) [Google Scholar]
- 14.National Academy of Sciences, National Research Council . Diet and health: implication for reducing chronic disease. National Academy Press; Washington, DC, USA: 1989. [Google Scholar]
- 15.Stone EJ, Perry CL, Luepker RV. Synthesis on cardiovascular behavioral research for youth health promotion. Health Ed. Quart. 1989;16(2):155–169. doi: 10.1177/109019818901600202. [DOI] [PubMed] [Google Scholar]
- 16.Freeman WL. Research in rural native communities. In: Bass MJ, Dunn EV, Norton PO, Stewart M, Tudiver F, editors. Conducting Research in the Practice Setting. Research Methods in Primary Care. Sage Publication; Newbury Park, CA, USA: 1993. [Google Scholar]
- 17.Bird ME, Kane WM, Shames L, Jager M. Working cooperatively with Native American communities to educate children and youth. In: Matiella AC, editor. The Multicultural Challenge in Health Education. ETR Associates; Santa Cruz, CA, USA: 1994. pp. 209–232. [Google Scholar]
- 18.Davis SM. General guidelines for an effective and culturally sensitive approach to health education. In: Matiella AC, editor. The Multicultural Challenge in Health Education. ETR Associates; Santa Cruz, CA, USA: 1994. pp. 117–132. [Google Scholar]
- 19.Perry CL, Baranowski T, Parcel G. How individuals, environments, and health behavior interact: Social learning theocy. In: Glantz K, Lewis FM, Rimer B, editors. Health Behavior and Health Education. Jossey-Bass; San Francisco, CA, USA: 1990. pp. 161–186. [Google Scholar]
- 20.More AJ. Native Indian learning styles: A review for researchers and teachers. J. of Am. Indian Education. 1987;26:17–29. [Google Scholar]
- 21.Sallis JF, Simons-Morton BG, Stone EJ, Corbin CB, Epstein LH, Faucette N, Iannotti RJ, Killen JD, Klesges RC, Petray CK, et al. Determinants of physical activity and interventions in youth. Med. Sci. Sports Exerc. 1992;24(6):S248–S257. [PubMed] [Google Scholar]
- 22.Dietz WH, Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing fo children and adolescents. Pediatr. 1985;75:807–812. [PubMed] [Google Scholar]
- 23.Corbin CB, Pangrazi RP, Welk GJ. Toward an understanding of appropriate physical activity levels of youth. The President’s Council on Physical Fitness and Sports, Physical Activity and Fitness Research Digest. 1994;1(8):1–8. [Google Scholar]
- 24.Epstein LH, Valoski A, Vara LS, McCurley J, Wisniewski L, Kalarchian MA, Klein KR, Shrager LR. Effects of decreasing sedentacy behavior and increasing physical activity on weight change in obese children. Health Psychal. 1991;14:109–115. doi: 10.1037//0278-6133.14.2.109. [DOI] [PubMed] [Google Scholar]
- 25.Gutin B, Cucuzzo M, Islam S, Smith C, Moffatt R, Pargman D. Physical training improves body composition of black obese 7- to 11-year-old-girls. Obesity Res. 1995;3:305–312. doi: 10.1002/j.1550-8528.1995.tb00155.x. [DOI] [PubMed] [Google Scholar]
- 26.Luepker RV, Perry CL, McKinlay SM, Nader RR, Parcel GS, Stone EJ, Webber LS, Elder JP, Feldman HA, Johnson CC, Kelder SH, Wu M. Outcomes of a field trial to improve children’s dietacy patterns and physical activity: CATCH. JAMA. 1996;275(10):768–776. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 27.Sallis JF, Patterson TL, McKenzie TL, Nader PR. Family variables and physical activity in preschool children. Dev. Behav. Pediatr. 1988;9(2):57–61. [PubMed] [Google Scholar]
- 28.Tucker LA, Seljaas GT, Hager RL. Body fat percentage of children varies according to their diet composition. J. Am. Diet Assoc. 1994;91:981–986. doi: 10.1016/S0002-8223(97)00237-X. [DOI] [PubMed] [Google Scholar]
- 29.Feskanich D, Sielaff BH, Chong K, Buzzare JM. Computerized collection and analysis of dietary intake information. Computer Methods Programs Buned. 1989;30:47–57. doi: 10.1016/0169-2607(89)90122-3. [DOI] [PubMed] [Google Scholar]
- 30.Lohman TG, Cabalero B, Himes JH, Hunsberger S, Houtkooper L, Going SB, Weber J, Reid R, Davis CE, Stewart D. Estimation of body fat from anthropometry and bioelectrical impedance in Native American children. Am. J. Clin. Nutr. doi: 10.1038/sj.ijo.0801318. in press. [DOI] [PubMed] [Google Scholar]
- 31.Richardson MT, Leon AS, Jacobs DR, Jr., Ainsworth BE, Serfass R. Comprehensive evaluation of the Minnesota Leisure Time Physical Activity Questionnaire. J. Clin. Epidemiol. 1994;47(3):271–281. doi: 10.1016/0895-4356(94)90008-6. [DOI] [PubMed] [Google Scholar]
- 32.Baecke JAH, Burema J, Frijters JER. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am. J. Clin. Nutr. 1982;36:936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 33.Sallis JF. Epidemiology of physical activity and fitness in children and adolescents. Crit. Rev. Food Sci. Nutr. 1993;33(4-5):403–498. doi: 10.1080/10408399309527639. [DOI] [PubMed] [Google Scholar]
- 34.Freedson PS. Electronic motion sensors and heart rate as measures of physical activity in children. J. Sch. Health. 1991;61:220–223. doi: 10.1111/j.1746-1561.1991.tb06018.x. [DOI] [PubMed] [Google Scholar]
- 35.Treiber FA, Musante L, Hartdagan S, Davis H, Levy J, Strong WB. Validation of a heart rate monitor with children in laboratory and field settings. Med. Sci. Sports Exerc. 1989;21:338–342. [PubMed] [Google Scholar]
- 36.Livingstone MB, Coward WA, Prentice AM, Davies PS, Strain JJ, McKenna PO, Mahoney CA, White JA, Stewart CM, Kerr MJ. Daily energy expenditure in free-living children: Comparison of heart-rate monitoring with the doubly labeled water (2H2 18O) method. Am. J. Clin. Nutr. 1992;56:343–352. doi: 10.1093/ajcn/56.2.343. [DOI] [PubMed] [Google Scholar]
- 37.Fontvielle AM, Harper l.T., Ferraro RT, Spraul M, Ravussin E. Daily energy expenditure by five-year-old children, measured by doubly labeled water. J. Pediatr. 1993;123:200–207. doi: 10.1016/s0022-3476(05)81689-0. [DOI] [PubMed] [Google Scholar]
- 38.Sallis JF, Strikmiller PK, Harsha DW, Feldman HA, Ehlinger S, Stone EJ, Williston J, Woods S. Validation of interviewer- and self-administered physical activity checklists for fifth grade students. Med. Sci. Sports Exerc. 1996;28(7):840–851. doi: 10.1097/00005768-199607000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Sallis JF, Condon SA, Goggin KJ, Roby JJ, Kolody B, Alcaraz E. The development of self-administered physical activity suryeys for 4th grade students. Res. Q. Exerc. Sport. 1993;64(1):25–31. doi: 10.1080/02701367.1993.10608775. [DOI] [PubMed] [Google Scholar]
- 40.Welk GJ, Corbin CB. The validity of the TritracR3D-R3d Activity Monitor for the assessment of physical activity in children. Res, Q. Exerc. Sport. 1995;56:161–165. doi: 10.1080/02701367.1995.10608834. [DOI] [PubMed] [Google Scholar]
- 41.Epstein LH, Paluch RA, Coleman KJ, Vito D, Anderson K. Determinants of physical activity in obese children assessed by accelerometer and self-repbtt. Med. Sci. Sports Exerc. 1996;28(9):1157–1164. doi: 10.1097/00005768-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Domel SB, Baranowksi T, Leonard SB, Davis H, Riley P, Baranowski J. Accuracy of fourth- and fifth-grade students’ records compared with school lunch observations. Am. J. Clin. Nutr. 1995;56:218–220S. doi: 10.1093/ajcn/59.1.218S. [DOI] [PubMed] [Google Scholar]
- 43.Wright JD, Ervin B, Briefer RR. Consensus Workshop on Dietary Assessment: Nutrition Monitoring and Tracking the Year 20 Objectives. U.S. Department of Health and Human Services, CDCJNCHS; Hyattsville, MD, USA: 1994. [Google Scholar]
- 44.Raizman DJ, Montgomery DH, Osganian SK, Ebzery MK, Evans MA, Nicklas TA, Zive MM, Hann BJ, Snyder MP, Clesi AL. CATCH: Food service program process evaluation in a multicenter trial. Heath Ed. Quart. 1994;2:S51–S71. doi: 10.1177/10901981940210s105. [DOI] [PubMed] [Google Scholar]
- 45.Perry CL, Stone EJ, Parcel GS, Ellison RC, Nader PR, Webber LS, Luepker RV. School-based cardiovascular health promotion: The child and adolescent trial for cardiovascular health (CATCH) J. Sch. Health. 1990;60:406–413. doi: 10.1111/j.1746-1561.1990.tb05960.x. [DOI] [PubMed] [Google Scholar]
- 46.Kelder S, Perry C, Klepp K, Leslie L. Londitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. Am. J. Public Health. 1994;84:1121–1126. doi: 10.2105/ajph.84.7.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kelder S, Perry C, Lytle L, Klepp K. Communitywide youth nutrition education, long-term outcome of the Minnesota Heart Health Program. Health,Educ. Res. 1995;10:119–131. doi: 10.1093/her/10.2.119-a. [DOI] [PubMed] [Google Scholar]
- 48.Windsor RA, Baranowski T, Clark N, Cotter G. Evaluation of Health Promotion and Educanon Programs. Mayfield Publishing Co; Mountain View, CA USA: 1994. [Google Scholar]
- 49.McGraw SA, Stone EJ, Osganian SK, Elder JP, Perry CL, Johnson CC, Parcel GS, Webber LS, Leupker RV. Design of process evaluation within the child and adolescent trial for cardiovascular health (CATCH) Health Educ. Quart. 1994;(suppl. 2):S5–S26. doi: 10.1177/10901981940210s103. [DOI] [PubMed] [Google Scholar]
- 50.Lauer RM, Obarzanek E, Kwiterovich PO, et al. Efficacy and safety of lowering dietacy intake of fat and cholesterol in children with elevated low-density lipoprotein cholesterol: The dietacy intervention study in children (DISC) JAMA. 1995;273(18):1429–1435. doi: 10.1001/jama.1995.03520420045036. [DOI] [PubMed] [Google Scholar]
- 51.Webber LS, Frank GC, Smoak CG, Freedman DS, Berenson GS. Cardiovascular risk factors from birth to 7 years of age: The Bogalusa heart study. Pediatrics. 1987;80:767–815. [PubMed] [Google Scholar]


