Abstract
Background/Objectives:
Effective prevention of cardiovascular events in people with hypertension requires optimal control of blood pressure. Despite advances in management, poor adherence to antihypertensive medications is often reported as the major reason attenuating treatment efficacy. Research has provided limited evidence of associations between illness perceptions, satisfaction with consultations, and medication adherence. The aim of this study is to identify factors significantly associated with medication adherence in a group of Chinese older adults with essential hypertension.
Design/Setting/Participants:
A cross-sectional correlational study was conducted. Data were collected from 195 older adults (mean [SD] age, 76 [6.6] years) recruited from 12 community centers.
Measurements:
The Illness Perception Questionnaire–Revised was used to measure illness perceptions, and the Medical Interview Satisfaction Scale was used to measure satisfaction with individual consultations. The Morisky Medication Adherence Scale was used to measure the extent of adherence to antihypertensive medications. Multivariate logistic regression analysis was performed to examine factors, including illness perceptions, consultation satisfaction, and demographic and clinical characteristics, that were significantly associated with medication adherence.
Results:
More than half of the respondents (55.9%) acknowledged some degree of medication nonadherence. Older age, living alone, and perception related to treatment control were independently associated with increased odds of medication adherence, with odds ratios ranging from 1.14 to 1.92 (P < .05).
Conclusion:
The results highlight the importance of cultivating positive beliefs that hypertension is amenable to control by treatment. Furthermore, the adherence behavior of those of younger individuals and living with family should be closely monitored.
KEY WORDS: aged, hypertension, medication adherence
Hypertension is a significant public health problem, causing around 13% of the total deaths worldwide. The overall prevalence of increased blood pressure in people 25 years or older was about 40% in 2008.1 There is about 1 in every 3 adults, accounting for 67 million people, in the United States alone who has high blood pressure. The prevalence of hypertension increases with age so that two-thirds of those with the disease are 60 years or older.2,3 In Hong Kong, the total number of hospitalizations related to essential hypertension was more than 14 000 (0.71%).4 Hypertension is a major risk factor for heart disease and cerebrovascular disease, including stroke.2 In 2012, heart disease and cerebrovascular disease were respectively ranked the third and fourth leading causes of death in Hong Kong.5 Optimal control of blood pressure is paramount to prevent hypertension-related complications.1 However, studies have shown that a substantial proportion of hypertensive patients do not have their blood pressure within control, a major reason being poor adherence to antihypertensive medications.6,7 Thus, identification of factors influencing medication adherence is crucial.
Medication Adherence and Illness Perceptions
The term adherence is preferred over compliance to refer to the patient’s extent of following a healthcare professional’s advice for managing an illness or disease.8,9 According to Haynes et al,10 adherence is nonjudgmental and emphasizes the 2-way communication between the patient and healthcare professional. The 2 parties assume active roles in compromising and executing the therapeutic medication regimen.10 In general, factors influencing medication adherence can be categorized into internal and external11 and intentional and unintentional.12 A systematic review conducted by AlGhurair et al13 about adherence among older adults further summarized the influencing factors into 5 categories, namely, demographic, medical, medication, behavioral, and economic.
Leventhal’s self-regulatory model is a common explanatory model of medication adherence.14,15 In this model, medication adherence is a self-regulatory behavior. People always try to understand their illness or disease by developing their own model, and this may be conceptualized as an illness representation.16 Illness representations are made up of 5 key components, which include what the illness or disease is, its causal factors, consequences to daily life, how long it will last, and whether the condition can be cured or controlled.15 Illness representations are fostered through a variety of past symptoms and illness experiences, as well as the information obtained through different social and cultural associations.15 The uniqueness of an illness representation is its origin primarily in the person’s own intrinsic beliefs. It does not necessarily conform to scientific views. In addition, an illness representation is dynamic and it may change over the course of a disease.16 On the basis of illness representations, individuals subsequently determine their own coping strategies to regulate or minimize their health threats. Medication adherence is 1 of the health-related coping strategies. An individual will choose to adhere or not to adhere to a medication regimen depending on what he/she believes to be true about a disease and the perceived relationship of taking medications to disease management. Continuation of the coping strategy selected is dependent on the outcome appraisals. Individuals may not continue with the regimen if they perceive it as unsuccessful.17
Increasingly, studies have examined the relationship between medication adherence and illness perceptions among hypertensive patients. An early study of 230 hypertensive patients concluded that patients developed their implicit models or beliefs about the disease threats, and the model or belief guided the patients’ treatment behaviors.18 A recent study using multiple linear regression analysis showed that the perceived benefit of medication was the main predictor of adherence among 117 older adults with hypertension.19
Patient Satisfaction
Studies suggest that low treatment satisfaction among patients with hypertension may be an important barrier for achieving high rates of antihypertensive medication adherence.20 Satisfaction with quality of contact with healthcare professionals by people with hypertension during consultations may play a vital part in how they assimilate or make sense of professional advice and thus influence their medication adherence. McDonald-Miszczak et al21 postulated that older adults who were satisfied with either the information received or the behavior of healthcare professionals might perceive adherence as an important self-care task. They would also self-report themselves as more adherent. Hassan et al7 indicated that antihypertensive medication nonadherence among 242 hypertensive patients was associated with age, overall patient satisfaction with healthcare, and medication barriers such as complex regimen and cost. These studies were conducted in Western countries. Whether such relationships hold true in Chinese hypertensive older adults is not clear.
Aims
The aims of this study were as follows:
To examine the illness perceptions of essential hypertension, satisfaction with consultations, and adherence to antihypertensive medications among community-dwelling Chinese older adults with hypertension, and
To determine the factors significantly associated with adherence to antihypertensive medications.
Methods
Design and Sample
A cross-sectional study was conducted among a convenience sample of 195 older adults with hypertension who were recruited from 12 community centers in Hong Kong. Inclusion criteria were 65 years or older, had a diagnosis of essential hypertension, attended regular medical consultations for essential hypertension, received at least 1 type of antihypertensive medication, understood and spoke Cantonese, and willing to participate in the study. Participants were excluded if they had secondary hypertension or a psychiatric illness or mental impairment or were unable to give informed consent. The sample size in this study was adequate based on the recommendation by Kline22 that 10 to 20 times as many cases as parameters is sufficient for significance testing of model effects.
Measures
Morisky Medication Adherence Scale
The Morisky Medication Adherence Scale23 was used to measure participants’ adherence to antihypertensive medication. The scale consists of 4 yes/no questions about a participants’ experience of forgetting to or being careless about taking the prescribed antihypertensive medication and stopping to take it because of improvement or deterioration in their health condition. A score of 1 was given to each yes response. The total score ranges from 0 to 4, where a higher score indicates better medication adherence. Reliability of the scale was satisfactory, with a Cronbach’s α of .61.23
Illness Perception Questionnaire–Revised
The Illness Perception Questionnaire–Revised (IPQ-R)24,25 was used to measure participants’ illness perceptions of essential hypertension. The IPQ-R consists of 9 subscales, which include the identity of the illnesses or diseases, timeline (acute/chronic), timeline (cyclical), causes, consequences, personal control, treatment control, emotional representations, and illness coherence. The identity subscale contains 14 yes/no items asking about the participants’ experience of symptoms since the diagnosis of essential hypertension and their perceptions of the relationship between symptoms and essential hypertension. The sum of the yes-rated items constitutes the subscale total score, which ranges from 0 to 14. Higher scores indicate stronger beliefs that the presence of the symptoms was attributed to hypertension. The causes subscale contains 18 items eliciting participants’ perceptions about causal factors of essential hypertension such as aging or emotional problems. The items were rated on a 4-point Likert scale from strongly disagree (1) to strongly agree (4). There was an additional qualitative item asking participants to prioritize the 3 most important causal factors related to their diagnosis of hypertension.
Participants were also asked for their level of agreement to 38 statements corresponding to the remaining 7 subscales. The items were rated on a 5-point Likert scale from strongly disagree (1) to strongly agree (5). The total score of the timeline (acute/chronic), consequences, personal control, and emotional representations subscales ranges from 6 to 30; the treatment control and illness coherence subscales, 5 to 25; and the timeline (cyclical) subscale, 4 to 20. Higher scores represented stronger beliefs in the chronicity and cyclical nature of hypertension, greater negative emotional responses and consequences to daily life, more positive beliefs in controllability and curability of hypertension by the person or medical treatment, and better understanding of hypertension. All of the subscales demonstrated good reliability, with Cronbach’s α ranging from .79 to .89.24 In this study, the Cronbach’s α of all subscales ranged from .69 to .94.
The Morisky Medication Adherence Scale and IPQ-R were translated into Chinese using the instrument back-translation process to ensure equivalence of the scales when used in another language.26,27 The translated versions were rated for appropriateness of translation by a panel of clinical experts (1 advanced practice nurse and 1 registered nurse) and 2 professional translators, all of whom possessed relevant professional postgraduate qualifications. The translated version was piloted in a convenience sample of 10 community-dwelling hypertensive older adults to test for its preliminary reliability and validity.26 Some wording was amended according to the suggestions received and a final translated version was adopted.
Medical Interview Satisfaction Scale
Satisfaction with individual consultations was measured by the Chinese version of the Medical Interview Satisfaction Scale28 (C-MISS-R) developed and validated by Lam et al.29 The 8 items in the C-MISS-R were scored using a 5-point Likert scale, with responses ranging from strongly agree (5) to strongly disagree (1). The scores of the cognitive and affective subscales are calculated by summing the scores of the corresponding 4 items of each subscale. The scores of all 8 items can also be summed to give a summary score. The subscale scores range from 4 to 20, whereas the summary score ranges from 8 to 40. Higher scores represent greater satisfaction with either the cognitive or affective component of the contact with healthcare professionals during consultations. The translated C-MISS-R demonstrated good internal reliability, with a Cronbach’s α of .84, .74, and .83 for the cognitive and affective subscales and the total score, respectively.29 The Cronbach’s α of the total score and cognitive and affective subscales of the C-MISS-R in the present study was .93, .93, and .90, respectively.
Demographic and Clinical Information
Demographic and clinical information including age, gender, marital status, educational level, occupation if applicable, living condition, current and past medical histories, frequency of medical consultations for essential hypertension, and regimens of antihypertensive medications were also recorded.
Data Collection Procedure
Older adults attending community centers for social activities were approached by a researcher and informed about the nature of the study, invited to participate voluntarily, and assured of their rights to confidentiality. Those who agreed to participate in the study were asked to sign consent. An information sheet describing the details of the study and contact methods for further information was given to each participant. After signing the consent, the participants were interviewed face to face using the structured questionnaire. The whole interview took approximately 20 to 30 minutes.
Ethical Considerations
Ethical approval to conduct the study was obtained from the Survey and Behavioural Research Ethics Committee of the university. Participation in the study was voluntary, written informed consent was obtained from the participants, and questionnaires were anonymized. All information collected was kept strictly confidential and secure. The interviews were scheduled without interfering with the daily functions of the community centers and activities of the older adults.
Statistical Analysis
Data were summarized and presented using descriptive statistics. The normality of continuous variable was assessed by the skewness statistic and graphically by a normal probability plot. Multivariate logistic regression analysis was used to identify factors independently associated with adherence to antihypertensive medications. The independent variables considered in the logistic regression are age, sex, years since diagnosis of hypertension, marital status, educational level, living condition, number and frequency of antihypertensive medications taken per day, subscale scores of the IPQ-R (including identity, timeline [acute/chronic], timeline [cyclical], consequences, personal control, treatment control, emotional representations, and illness coherence), and cognitive and affective subscale scores of the MISS. An Morisky Medication Adherence Scale cutoff score of 3 or below was used to categorize participants as nonadherent, and a score of 4, as adherent to medications. Univariate analyses were first performed on each of the considered independent variables to select candidate variables for the multivariate analysis. Those factors with a P < .25 in the univariate analyses30 were selected as candidate variables for backward stepwise multivariate logistic regression to delineate factors independently associated with medical adherence. The Hosemer-Lemeshow test was used to assess the goodness of fit of the final multivariate logistic regression model obtained. The results of significant factors identified are presented with their odds ratio and 95% confidence interval. All statistical analyses were performed using SPSS 22.0 (SPSS Inc, Chicago, Illinois). All statistical tests were 2 tailed, and the level of statistical significance was set at .05.
Results
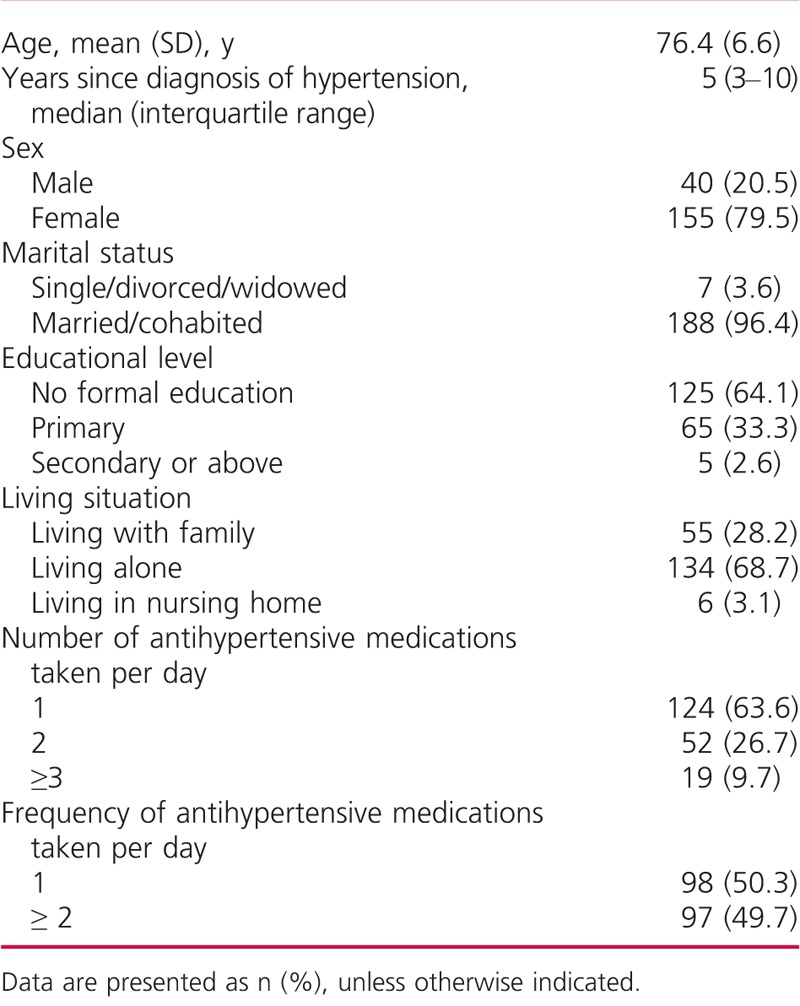
A total of 208 older adults with hypertension were approached. Thirteen were excluded for having a concomitant diagnosis of stroke or dementia. The response rate was 100%. Participants had a mean (SD) age of 76.4 (6.6) years (range, 61–94 years). There were 40 (20.5%) men and 155 (79.5%) women. They had had hypertension for a mean (SD) of 8.4 (7.50) years (range, 1–40 years). More than half (57%) of the participants reported other current health conditions, including osteoarthritis, osteoporosis, asthma, and cataract. Most of them (90.3%) were receiving 1 or 2 types of antihypertensive medication (mean [SD], 1.5 [0.8]) (Table 1).
TABLE 1.
Characteristics of the Study Sample (n = 195)
Illness Perceptions of Essential Hypertension
The 5 most frequently reported symptoms were dizziness (41.0%), headache (29.7%), joint stiffness (13.3%), difficulty in sleep (11.8%), and eye pain (10.8%). However, fewer than half of participants (44.4%) associated these symptoms with their hypertension. Most of them (22.6%) reported to have experienced dizziness in relation to hypertension, followed by headache (13.8%), difficulty in sleeping (2.1%), joint stiffness (0.5%), and eye pain (1.0%).
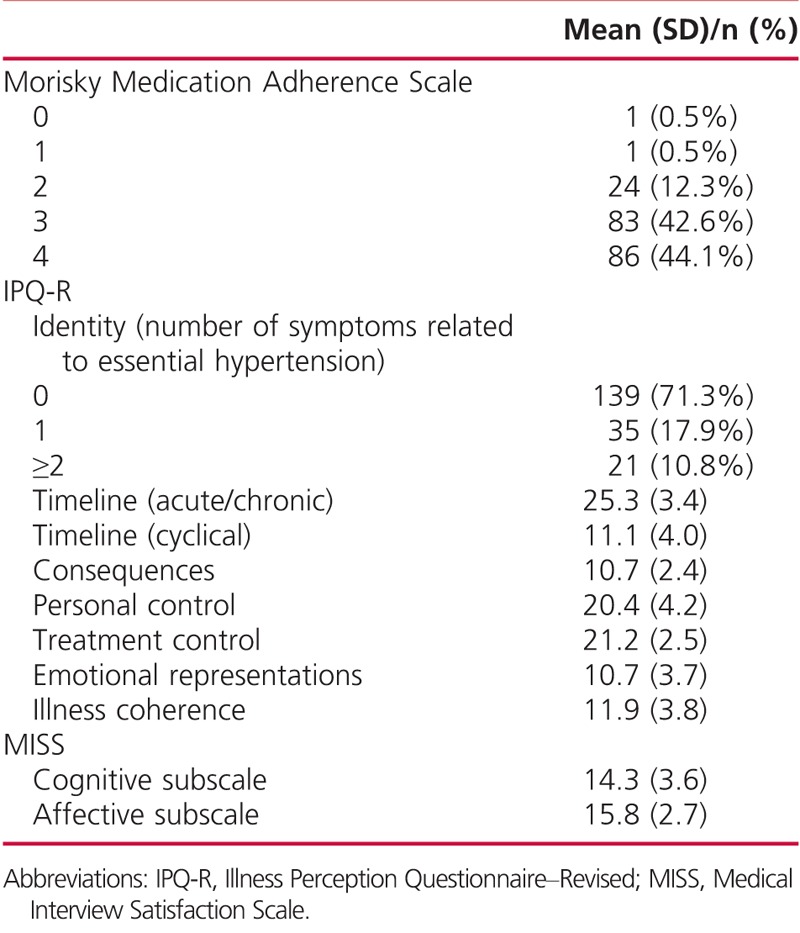
Table 2 shows the mean scores and standard deviations of the 8 subscales of the IPQ-R. The high score in the timeline (acute/chronic) and the low score in the timeline (cyclical) subscales indicate that participants mostly perceived hypertension as a chronic condition, but rather stable over time. Both the consequences and emotional representations subscales recorded a score of approximately 10, indicating that negative impact caused by hypertension was not noticeably apparent among participants. They did not view their hypertension as causing serious consequences to their daily lives. Similarly, the emotional impact of hypertension was reported to be low. Participants scored relatively high in the personal control and treatment control subscales. The mean scores of both subscales exceeded 20, indicating participants’ positive beliefs in having a degree of control over their hypertension, exerted by personal behavior and medical treatment. Nonetheless, they found themselves not to have a clear understanding of hypertension as reflected in the low mean score of illness coherence (mean [SD], 11.9 [3.8]).
TABLE 2.
Scores of the Morisky Medication Adherence Scale, Illness Perception Questionnaire–Revised, and Medical Interview Satisfaction Scale
Nearly two-thirds of participants strongly agreed or agreed that aging (65.7%) and negative emotional state (64.1%) acted as a causal factor contributing to their hypertension. The mean (SD) scores were 3.7 (1.3) and 3.6 (1.4), respectively. To a far lesser degree, participants believed that diet or eating habits (32.8%), stress or worries (28.2%), overwork (23.1%), and family problems (15.4%) were related to their hypertension. The mean (SD) scores were 2.5 (1.4), 2.3 (1.4), 2.3 (1.3), and 2.0 (1.1), respectively. Fewer than 10% of the participants attributed their hypertension to other factors such as hereditary factors, germ or virus, chance or bad luck, personal behaviors, attitudes, alcohol consumption, smoking, accident or injury, personality, and altered immunity.
Consultation Satisfaction
Most participants attended follow-up medical consultations every 2 to 3 months (92.3%) and were satisfied with these, with moderate to high total scores on the cognitive (mean [SD], 14.3 [3.6]) and affective (mean [SD], 15.8 [2.7]) subscales of the MISS (Table 2).
Adherence to Medication Adherence
Only 86 participants (44.1%) were regarded as adherent to antihypertensive medication according to their Morisky Medication Adherence Scale score (mean [SD], 3.3 [0.7]) (Table 2). More than half of the participants (n = 104; 53.3%) reported forgetting to take their antihypertensive medication, although only 22 (11.3%) perceived that they had problems in remembering to take their medication. Nearly all participants denied stopping taking their medication because of improvement (96.4%) or deterioration (97.4%) in their health condition.
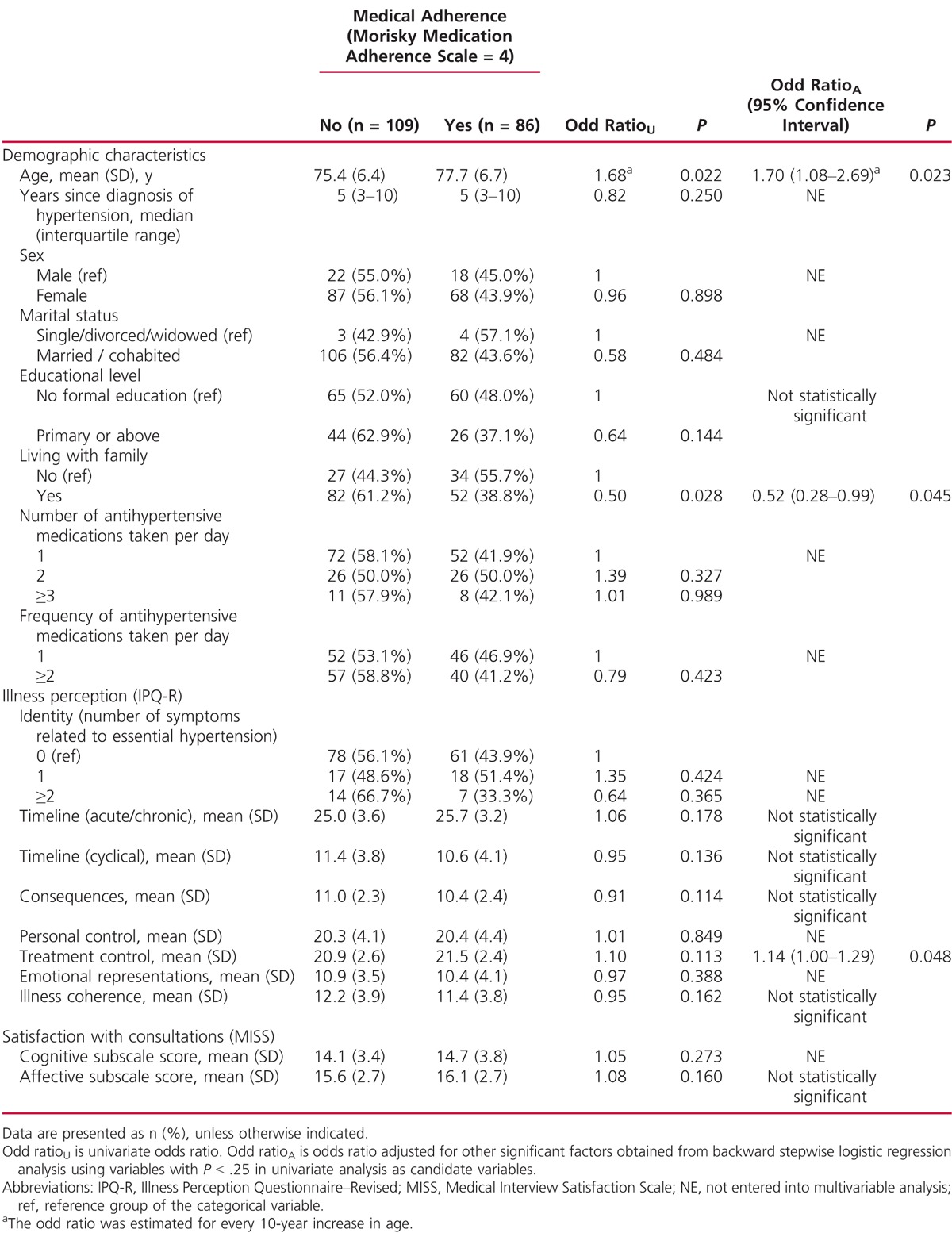
Factors Associated With Medication Adherence
The factors listed in Table 3 were examined for associations with medication adherence. Backward stepwise multivariate logistic regression using those factors with P < .25 in univariate analyses as candidate variables revealed that (1) age, (2) living with family, and (3) illness perception related to treatment control were independently significantly associated with medication adherence. The insignificant result of the Hosemer-Lemeshow test of the final backward model indicated a good fit to the data (P = .898). Older participants were more likely to adhere to their prescribed antihypertensive medication (odd ratio, 1.70; 95% confidence interval, 1.08–2.69; P = .023) for every 10-year increase in age. Those participants living with family were less likely to adhere to their antihypertensive medication (odd ratio, 1.52; 95% Confidence interval, 0.28–0.99; P = .045). Participants with stronger beliefs that hypertension could be controlled by treatment were associated with an increased odd of medication adherence (odd ratio, 1.14; 95% confidence interval, 1.00–1.29; P = .048) for every 1-unit increase in the treatment control subscale score of IPQ-R.
TABLE 3.
Factors Associated With Adherence to Antihypertensive Medications
Discussion
This study presents important findings about illness perceptions of hypertension and adherence to antihypertensive medication. First, it is disappointing that fewer than half (44.1%) of the participants adhered fully to antihypertensive medication regimens, as indicated by their Morisky Medication Adherence Scale score. Although other studies have consistently reported that difficulty in recalling information was always a major barrier to medication adherence among older adults,11 nearly 90% of the participants in this study reported no such difficulties. One may postulate that they might have developed their own strategies to remind them to take their medication.
Second, this study shows that older age, not living with family, and having a strong belief in the controllability of hypertension by medical treatment were significantly associated with older adults’ adherence to antihypertensive medication. These findings are consistent with a previous study in Hong Kong that found that younger age was negatively associated with antihypertensive medication adherence among adults with hypertension.31 Most of the participants believed that aging was the most relevant causal factor of hypertension. As older adults 75 years or older constitute around three-quarters of those with hypertension,32 this may explain their likelihood of accepting the diagnosis of hypertension when old. Furthermore, persons living with chronic illness are subjected to greater risk of having negative emotions, resulting in serious consequences for daily lives and a burden to family members and the healthcare system32; participants in this study neither perceived having negative responses to the diagnosis of hypertension nor thought that hypertension had serious consequences for their lives. These findings are similar to those reported by Ross et al25 and may be related to the asymptomatic nature of hypertension.33 About one-third of participants in our study did not experience any symptoms since the diagnosis of hypertension. Among those who reported symptoms, fewer than half perceived a relationship between symptoms and hypertension. Participants viewed readings of their blood pressure as relatively stable and that they were not feeling unwell. Indeed, most participants took 1 or 2 types of antihypertensive medication; simplicity of the medication regimen additionally may have facilitated the participants’ capacity to adhere to the medication regimen, as well as self-manage their hypertension without imposing an undue burden on their lives.
In our study, participants had a strong perception of the chronicity of hypertension, and nearly all of them reported that they knew they had to take antihypertensive medication for the rest of their lives without discontinuation. They attributed the cultivation of this belief largely to such treatment being emphasized by their physician during consultations. With regard to the self-regulatory model, the interaction with healthcare professionals appeared to form a vital element in shaping illness perceptions in these older adults. They had a strong belief in the controllability of hypertension by medical treatment, a finding consistent with previous reports that perceived concerns about the benefits of medication was a significant factor in predicting adherence.19
A study among 440 Korean American elderly people found that those who lived alone were more likely to have controlled blood pressure compared with those who lived with family. This may be related to their more frequent social interactions and conversations about health in senior group housing, as well as receiving more encouragement in taking medications.34 In our study, the older adults who were not living with family mainly lived alone or in senior group housing estates. The improved antihypertensive medication adherence may be related to their participation in social and health events organized by the community centers and thus impacted positively on their adherence behaviors.34
The literature identifies several risk factors related to hypertension, including genetic factors, obesity, insulin resistance, high alcohol intake, high salt intake, aging, sedentary lifestyle, and stress.35 Our study supports this by showing that aging, negative emotional problems, eating habits, stress, or worries are frequently rated as important risk factors for hypertension. It is important to note that these risk factors, with the exception of aging, are modifiable. It highlights the importance of lifestyle modifications to better control blood pressure.3 Encouragingly, our study found that participants positively perceived their ability to exert personal control of hypertension, and when asked about the kinds of personal control they had, many of them were able to identify at least 1 or 2 recommended lifestyle modifications, including but not limited to restricting sodium intake, engaging in more exercise, or better managing stress. Reinforcement of these and further health education on lifestyle changes would likely promote empowerment of older adults in self-managing their hypertension.
Health education about hypertension is frequently organized by healthcare professionals in hospitals or community centers. Relevant information in forms of leaflets, books, or via the Internet should be easily accessible in local patient resource centers, community centers, libraries, or hospitals. Surprisingly, however, participants in our study expressed a lack of clear understanding of hypertension. Some participants admitted that they easily forgot any information obtained or that the information available was not specific or individualized enough for managing their own hypertension. As better awareness of hypertension is a significant factor in predicting medication adherence,36 more appropriate innovative and targeted health education strategies may be needed for older adults with hypertension. For example, health education strategies should include practical self-management skills training.
There are some limitations to this study. First, the measurement of medication adherence was based solely on self-reported responses to questionnaires. The results may be subjected to recall bias and social desirability bias especially when it comes to sensitive questions such as medication adherence. To ensure the accuracy of data about medication adherence, objective measurement such as prescription refill records and pill counts should be incorporated in future studies. Second, a cross-sectional design with convenience sampling was adopted in this study. Changes in illness perceptions and their influence on medication adherence cannot be measured. Larger scale studies with representative samples in future studies could increase generalizability of our findings. Further investigations are needed to explore other potential determinants of medication adherence that were not examined in this study, such as social support, and types and effectiveness of the reminders of medication taking.
Conclusion
Illness perceptions among older adults with hypertension could potentially influence their adherence to antihypertensive medication. Further studies with representative samples and better reliability of medication adherence measures are necessary to investigate this relationship. Healthcare professionals are obliged to explore the specific health educational needs of older adults with hypertension and thus develop effective and individualized health education.
What’s New and Important
–We found that more than half of the respondents acknowledged some degree of medication nonadherence.
–Older age, living alone, and perception related to treatment control were significant factors independently associated with better medication adherence.
–The results highlight the importance of cultivating positive beliefs that hypertension is amenable to control by treatment. The adherence behavior of those of younger age and living with family should be closer monitored.
Footnotes
The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.World Health Organization. Raised blood pressure. Situation and trends. 2014. http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/. Accessed October 30, 2014.
- 2.Centers for Disease Control and Prevention. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. 2013. http://www.cdc.gov/nchs/data/databriefs/db133.htm Accessed October 30, 2014.
- 3.Centers for Disease Control and Prevention. High blood pressure. 2014. http://www.cdc.gov/bloodpressure/. Accessed October 30, 2014.
- 4.Hospital Authority. Hong Kong. Hospital Authority statistical report 2012–2013. 2014. http://www.ha.org.hk/upload/publication_15/491.pdf. Accessed October 30, 2014.
- 5.Department of Health, Hong Kong. Number of deaths by leading causes of death by sex by age in 2013. 2013. http://www.chp.gov.hk/en/data/4/10/27/340.html. Accessed October 30, 2014.
- 6.Borzecki AM, Oliveria SA, Berlowitz DR. Barriers to hypertension control. Am Heart J. 2005;149:785–794. [DOI] [PubMed] [Google Scholar]
- 7.Hassan NB, Hasanah CI, Foong K, et al. Identification of psychosocial factors of noncompliance in hypertensive patients. J Hum Hypertens. 2006;20:23–29. [DOI] [PubMed] [Google Scholar]
- 8.MacLaughlin EJ, Raehl CL, Treadway AK, et al. Assessing medication adherence in the elderly: which tools to use in clinical practice? Drugs Aging. 2005;22:231–255. [DOI] [PubMed] [Google Scholar]
- 9.Thrall G, Lip GYH, Lane D. Compliance with pharmacological therapy in hypertension: can we do better, and how? J Hum Hypertens. 2004;18:595–597. [DOI] [PubMed] [Google Scholar]
- 10.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;16:1–97CD000011. [DOI] [PubMed] [Google Scholar]
- 11.Marshall IJ, Wolfe CDA, McKevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. BMJ. 2012;345:e3953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lowry KP, Dudley TK, Oddone EZ, et al. Intentional and unintentional nonadherence to antihypertensive medication. Ann Pharmacother. 2005;39:1198–1203. [DOI] [PubMed] [Google Scholar]
- 13.AlGhurair SA, Hughes CA, Simpson SH, et al. A systematic review of patient self-reported barriers of adherence to antihypertensive medications using the world health organization multidimensional adherence model. J Clin Hypertens. 2012;14:877–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–567. [DOI] [PubMed] [Google Scholar]
- 15.Leventhal M, Cameron L. Behavioural theories and the problem of compliance. Patient Educ Couns. 1987;10:117–138. [Google Scholar]
- 16.Morrell RW, Park DC, Kidder DP, et al. Adherence to antihypertensive medications across the life span. Gerontologist. 1997;37:609–19. [DOI] [PubMed] [Google Scholar]
- 17.Horne R, Clatworthy J, Polmear A, et al. Do hypertensive patients’ beliefs about their illness and treatment influence medication adherence and quality of life? J Hum Hypertens. 2001;15:S65–S68. [DOI] [PubMed] [Google Scholar]
- 18.Meyer D, Leventhal H, Gutmann M. Common-sense models of illness: the example of hypertension. Health Psychol. 1985;4:115–135. [DOI] [PubMed] [Google Scholar]
- 19.Rajpura J, Nayak R. Medication adherence in a sample of elderly suffering from hypertension: evaluating the influence of illness perceptions, treatment beliefs, and illness burden. J Manag Care Pharm. 2014;20:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zyoud SH, Al-Jabi SW, Sweileh WM, et al. Relationship of treatment satisfaction to medication adherence: findings from a cross-sectional survey among hypertensive patients in Palestine. Health Qual Life Outcomes. 2013;11:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDonald-Miszczak L, Maki SA, Gould ON. Self-reported medication adherence and health status in late adulthood: the role of beliefs. Exp Aging Res. 2000;26:189–207. [DOI] [PubMed] [Google Scholar]
- 22.Kline RB. Principles and Practice of Structural Equation Modeling. 2nd ed New York: Guilford Press; 2005. [Google Scholar]
- 23.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. [DOI] [PubMed] [Google Scholar]
- 24.Moss-Morris R, Weinman J, Petrie KJ, et al. The Revised Illness Perception Questionnaire (IPQ-R). Psychol Health. 2002;17:1–16. [Google Scholar]
- 25.Ross S, Walker A, MacLeod MJ. Patient compliance in hypertension: role of illness perceptions and treatment beliefs. J Hum Hypertens. 2004;18:607–13. [DOI] [PubMed] [Google Scholar]
- 26.Chang AM, Chau JPC, Holroyd E. Translation of questionnaires and issues of equivalence. J Adv Nurs. 1999;29:316–322. [DOI] [PubMed] [Google Scholar]
- 27.Maneesriwongul W, Dixon JK. Instrument translation process: a methods review. J Adv Nurs. 2004;48:175–186. [DOI] [PubMed] [Google Scholar]
- 28.Wolf MH, Putman SM, James SA, et al. The Medical Interview Satisfaction Scale: development of a scale to measure patient perceptions of physician behavior. J Behav Med. 1978;1:391–401. [DOI] [PubMed] [Google Scholar]
- 29.Lam WWT, Fielding R, Chow L, et al. The Chinese Medical Interview Satisfaction Scale–Revised (C-MISS-R): development and validation. Qual Life Res. 2005;14:1187–1192. [DOI] [PubMed] [Google Scholar]
- 30.Hosmer DW, Lemeshow S, Sturdivant R. Applied Logistic Regression. 3rd ed Hoboken, NJ: Wiley; 2013. [Google Scholar]
- 31.Lee GK, Wang HH, Liu KQ, et al. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS One. 2013;8:e62775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lam CLK, Lauder IJ. The impact of chronic diseases on the health-related quality of life (HRQOL) of Chinese patients in primary care. Fam Pract. 2000;17:159–166. [DOI] [PubMed] [Google Scholar]
- 33.Centre for Health Protection. Hypertension. 2014. http://www.chp.gov.hk/en/content/9/25/35390.html. Accessed October 30, 2014.
- 34.Han HR, Song Y, Song HK, et al. Influence of living arrangements on the management and control of hypertension: a mixed-methods study of Korean American elderly. J Immigr Minor Health. 2013;15:944–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carretero OA, Oparil S. Essential hypertension, part I: definition and etiology. Circulation. 2000;101:329–335. [DOI] [PubMed] [Google Scholar]
- 36.Hashmi SK, Afridi MB, Abbas K, et al. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS One. 2007;2:e280. [DOI] [PMC free article] [PubMed] [Google Scholar]


