Abstract
Objectives:
Rates of anxiety in patients with heart failure (HF) vary widely, and not all assessment instruments used in this patient population are appropriate. It is timely to consolidate the evidence base and establish the prevalence and variance of anxiety in HF samples.
Methods:
A systematic review, meta-analysis, and meta-regression were conducted to identify the prevalence, variance, and measurement of anxiety in patients with HF.
Results:
A total of 14,367 citations were identified, with 73 studies meeting inclusion criteria. A random effects pooled prevalence of 13.1% (95% confidence interval [CI], 9.25%–16.86%) for anxiety disorders, 28.79% (95% CI, 23.30%–34.29) for probable clinically significant anxiety, and 55.5% (95% CI, 48.08%–62.83%) for elevated symptoms of anxiety was identified. Rates of anxiety were highest when measured using the Brief Symptom Scale-Anxiety scale (72.3%) and lowest when measured using the Generalised Anxiety Disorder-7 (6.3%).
Conclusion:
Many patients with HF would benefit if screened for anxiety and treated. The conceptualization and measurement of anxiety accounted for most variance in prevalence rates. The Generalised Anxiety Disorder-7 or the Hospital Anxiety and Depression Scale appear to be the most appropriate instruments for this clinical population, with evidence to suggest they can discriminate between depression and anxiety, omit somatic items that may contaminate identification of anxiety in a population with physical comorbidities, and provide thresholds with which to differentiate patients and target treatments. Although there are limitations with the collation of diverse measurement methods, the current review provides researchers and clinicians with a more granular knowledge of prevalence estimates of anxiety in a population of HF patients.
KEY WORDS: anxiety, heart failure, long-term conditions, mental health, prevalence, systematic review
Introduction
More than 30% of individuals with 1 or more physical long-term conditions may experience comorbid mental health problems, such as anxiety and depression,1 leading to increased health complications, consumption of healthcare, and, in turn, estimated increases in healthcare spending of 45%.2 In the past decade, the interest in depression in heart failure (HF) research has increased,3–8 and health professionals are advised to be aware of and screen for potential depression in patients with HF.9 Despite evidence to suggest that anxiety often proceeds depression and that it is as distressing as and often more prevalent than depression,10–12 relatively little research has been conducted to explore the prevalence, nature, and impact of anxiety, particularly in HF. Recent publications in this area reported rates of anxiety varying between 8% and 18%13 for anxiety disorders, 17 % and 28.8 % for clinically significant anxiety,14–16 as well as 40% and 72% for elevated symptoms of anxiety17–19 using a variety of measurement instruments and thresholds to interpret scores from a range of patient samples and settings.
The accurate measurement and identification of depression and anxiety can be challenging owing, in part, to the frequent co-occurrence of these conditions (up to 70% of cases) in clinical and nonclinical samples alike20 and overlap in symptoms, particularly those of a physiological nature. Assessing anxiety within the context of a physical disease process can be considered an even greater challenge because both physical and emotional conditions share many common symptoms including fatigue, palpitations, chest pains, breathlessness, and many more.21 Therefore, measures used to identify anxiety must be appropriate for use in this patient population. Omitting somatic items in the detection of anxiety should allow for the separation of the emotional condition from the physical.22
Consolidating the evidence base on the measurement and prevalence of anxiety in patients with HF is the first step toward a more comprehensive understanding of the scale of the problem as well as the development of interventions to manage anxiety. The only review conducted to date to establish the prevalence of anxiety in HF identified 8 studies to assess the prevalence of anxiety in patients with HF compared with 33 studies that reported prevalence of depression23 and prevalence of anxiety that ranged between 11% and 45%, measured using 6 different measurement instruments. The review by Yohannes et al23 is not comprehensive, and in addition, the authors did not report the way in which anxiety had been conceptualized in the identified articles. It is unclear whether the rates of anxiety relate to anxiety symptoms, clinical anxiety, or specific anxiety disorders, although some of the instruments used to measure anxiety in the identified studies assess only anxious mood; therefore, the rates of anxiety identified in this review must be interpreted with caution. It is appropriate and timely to identify, appraise, and summarize the evidence base in this area.
We report a systematic review and meta-analysis of research studies that report the prevalence and/or severity of anxiety in samples of patients with HF. The aims of the systematic review were to identify the prevalence of anxiety and methods of measurement in samples of patients with HF and to identify sources of variation in reported rates.
Methods
Eligibility Criteria
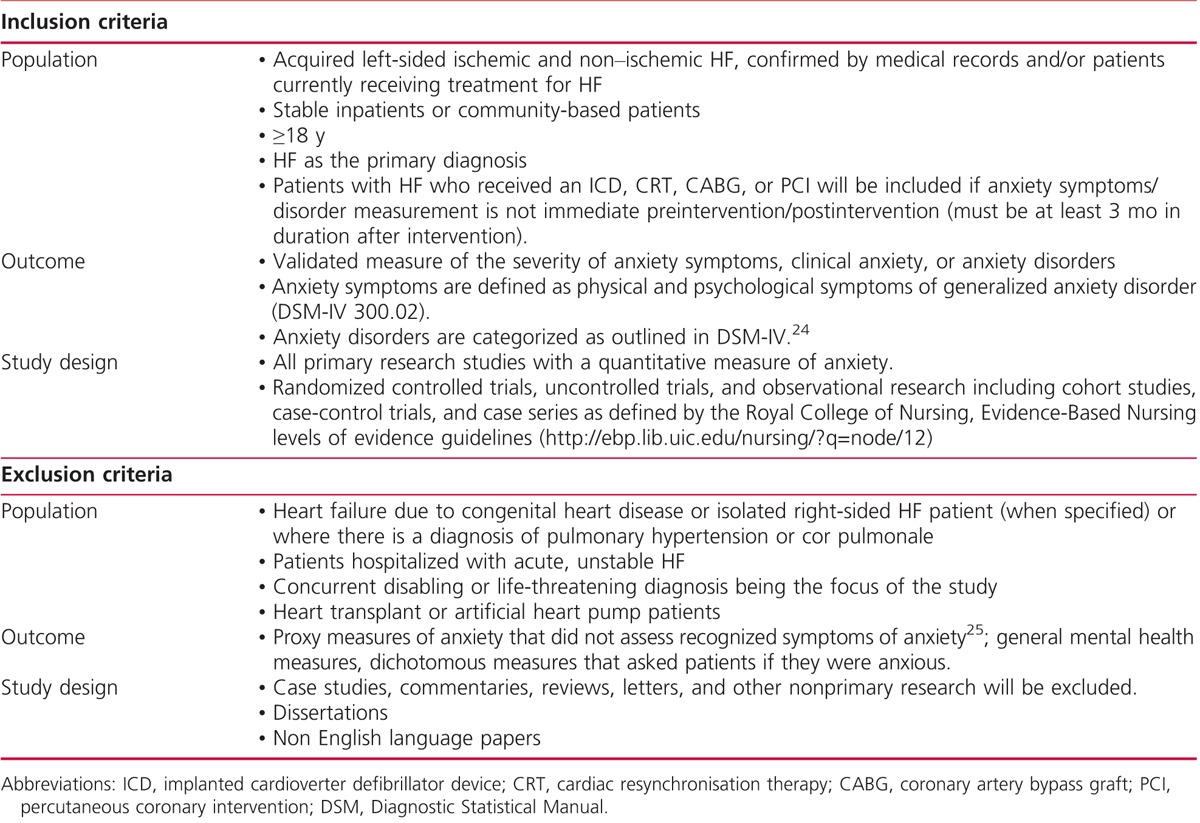
The eligibility criteria are listed in Table 1.
TABLE 1.
Exclusion and Inclusion Criteria
Search Strategy
The search for relevant articles was conducted by the author in 3 phases: an initial search of databases (June 2008), an updated search the following year (October 2009), and a final update of the main electronic databases in January 2013. The following databases were searched from year of inception to January 2013:
MEDLINE on the OVID platform (1950–January 2013)
British Nursing Index and Archive on the OVID platform (1985–October 2009) and on Proquest (January 2013)
EMBASE on the OVID platform (1980–January 2013)
PsycINFO using the OVID platform (1806–January 2013)
CINAHL (Cumulative Index to Nursing and Allied Health Literature) was search initially using the Ovid platform (1982–June 2008) and for the updated search using its current host EBSCOhost (2008–2013)
ISI Web of Science with conference proceedings (1990–January 2013)
Cochrane Central Register of Controlled Trials using Wiley Interscience (1980–October 2009)
MetaRegister Current Controlled Trials (mRCT) was searched, selecting all registers with the exception of the Leukaemia Research Fund.
Leading experts in the field were emailed to inquire about any unpublished work or work in progress.
Index terms, subheading, and free-text terms were used, along with truncation and combined using Boolean operators AND and OR. Terms including heart failure, cardiac failure, and cardiomyopathy were combined with anxiety, mood disorder, emotional factors, and specific diagnostic terms including generalised anxiety disorder. An example of the search strategy is available in the online appendix, Supplemental Digital Content 1, http://links.lww.com/JCN/A11. Key articles and reviews were hand-searched to identify any additional literature. References were limited in the English language.
Study Selection and Data Extraction
One author (K.E.) screened titles and abstracts against the inclusion criteria and obtained full-text articles for assessment. Data from ongoing research, abstracts, and presentations were obtained from principal investigators. The review team (P.C., K.L., and C.D.) were consulted to clarify uncertainties of inclusion until a consensus was reached. Authors were contacted for additional information when studies contained an HF sample and valid measure of anxiety but no data, where anxiety data were not reported separately for HF in a mixed sample and where demographic and clinical data were reported for a different number of participants compared with anxiety data. When interventional studies were included, only baseline data from control and interventional groups were extracted.
Data extraction was conducted independently by 4 reviewers: K.E. extracted data from all included articles, whereas the other reviewers (P.C., K.L., and C.D.) each extracted data from a third of the studies. Extracted data were compared, and discrepancies in extraction were discussed with the team until consensus was reached. A modified extraction form26 was developed, piloted, and further refined to extract data on the following: sample size; average age; proportion of males; New York Heart Association functional class; left ventricular ejection fraction %; ethnicity; study design, sampling method; response rate/attrition; geographical location; setting; definition of anxiety; measurement instrument; number of people with anxiety; average scores on anxiety measurement; and prevalence rate of anxiety.
Quality Assessment
The quality of studies was assessed in 3 stages.
Firstly, only studies with a validated measure of anxiety symptoms were included in the review.
Secondly, the design of studies was extracted and used as a variable in the meta-regression analyses to identify variance in prevalence estimates correlated to design.
Finally, a component approach was used to assess factors considered important for internal validity.27
Bias must be assessed and acknowledged in a systematic review so that the results can be considered in light of this. The selection of participants, measurement of outcome variables, and appropriate use of analytical methods to control for confounding variables are key components that must be considered to assess the internal validity observational research.28 There is no standard quality assessment instrument for use with observational studies or for use in reviews that seek to document the presence or prevalence of a condition as opposed to measure the effects of an intervention.29 It is therefore advised that key components be chosen relating to an individual review’s context, choice of design inclusion, and outcome.28 The choice of quality components was guided by the Strengthening The Reporting of Observational Studies in Epidemiology statement,30 evaluating reviews of prevalence31 and in consultation with the review team.
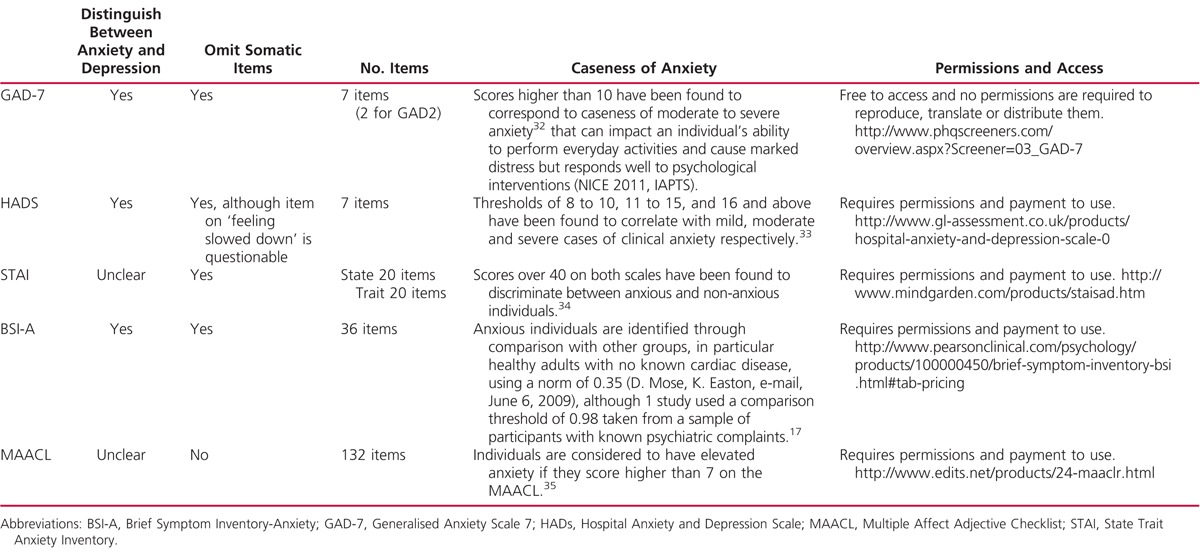
Further to this, the internal and external validity of studies was assessed by narratively evaluating the following components: evidence of probability sampling, adequate reporting of sampling characteristics, adequate response rates (80%> acceptable or 70%> if characteristics of nonresponders match responders), conceptualization of anxiety, standardized data collection, appropriateness of anxiety measure instrument; specifically the omission of somatic items and ability to distinguish between anxiety and depression, as determined through evaluation of available psychometric and empirical literature (Table 2). The assessment of study quality and the appropriateness of measurement instrument analyses can be found in the online appendix, Tables B and C, respectively, Supplemental Digital Content 1, http://links.lww.com/JCN/A11.
TABLE 2.
Characteristics of Selected Anxiety Measures Identified in the Review
In quantitative data analysis, the quality components of sample composition, conceptualization of anxiety, and appropriateness of measurement instrument were entered into sensitivity analysis in the meta-regression to determine whether levels of anxiety varied as a result of these components. The outcomes of the quality appraisal were narratively and statistically synthesized with results from the review.
Data Analysis
Heterogeneity among study outcomes was explored using the Cochran Q (reported as X2 and P value) and I2 statistic. A significance level of P < 0.10 was set for the Q statistic owing to inherent low statistical power in this test.36 The I2 values of 25%, 50%, and 75% are indicative of low, moderate, and high levels of heterogeneity (variance between studies), respectively. When heterogeneity was high (>75%), random effects models were fitted using the command METAN to identify pooled estimates of the prevalence of anxiety in HF samples.37
Meta-analysis was performed using Stata 11.0 software package.38 Studies that identified specific anxiety disorders were clustered together (termed anxiety disorder). Studies that used measures to screen for levels of probable anxiety above a given threshold were clustered together (termed probable clinical anxiety). Studies that used questionnaires to measure anxiety symptoms that reached levels above the norm for the general population were clustered together (termed elevated symptoms of anxiety). The remaining studies that used measures to assess symptoms of anxiety with no reference to thresholds with which to identify anxious cases were clustered together. Not all studies included in the review reported a prevalence rate of anxiety. Where studies report anxiety symptom severity (mean, SD, median, interquartile range), meta-analysis was conducted using measurement instrument to determine how levels of anxiety reported as central tendencies varied as a result of measurement methods.
Univariate meta-regression analysis was conducted to explore differences within overall pooled prevalence estimates39 on the following factors: conceptualization of anxiety (anxiety disorders, probable clinical anxiety, and elevated symptoms of anxiety), age (both as a continuous variable of mean age in years and a categorical variable of <59 years, 60–69 years, >70 years), gender (percentage of males in the sample), setting (inpatient, outpatient, or mixed), left ventricular ejection fraction (mean percentage), New York Heart Association (NYHA) class (mild [>70% of the sample in classes I and II], moderate/severe [>70% of the sample in classes III and IV], mixed), design (randomized controlled trial vs uncontrolled trials, cohort, case controlled, case series), country (United States vs United Kingdom and Europe, Asia, Australasia, mixed samples, and Africa). In addition, because conceptualization of anxiety will understandably have an impact on reported rates of anxiety, a planned post hoc analysis was conducted to explore variations in prevalence rates while controlling for conceptualization of anxiety in a 2-factor meta-regression.
Our study is reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.27
Results
Identification of Included Studies
Relevant articles were exported in to Reference Manager for management. After reviewing 14,367 articles and studies, 144 articles met criteria for the review and 72 studies contained sufficient data for inclusion in the narrative synthesis, of which 38 reported prevalence data for the meta-analysis and meta-regression (Figure 1, flowchart of search and screening).
FIGURE 1.
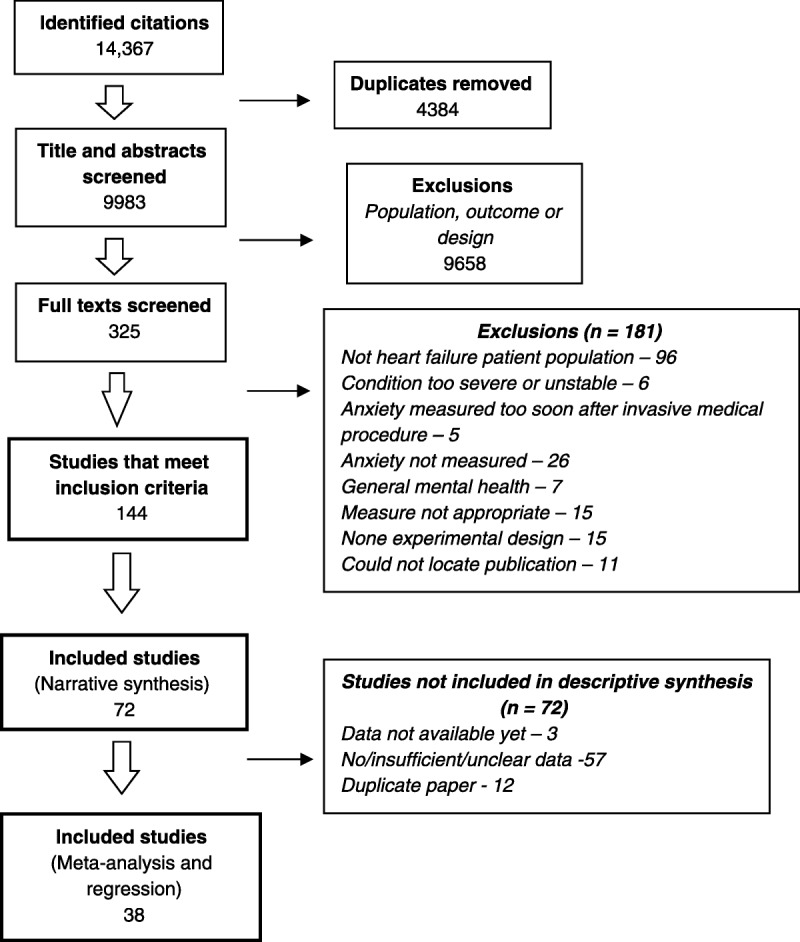
Flow diagram to show flow of studies in the review and reasons for exclusions.
Characteristics of Included Studies
The majority of studies were published between 2009 and 2013, originating mainly in the United States (n = 32), 9 in the United Kingdom, and 16 in Europe. Observational designs were used most frequently (66%), with anxiety being a primary outcome over half the included studies (53%). In total, 26,366 of patients with HF were sampled: 94% (24, 691) were males, with a mean (SD) age of 67.5 (11.4) years. The majority of the studies sampled outpatients (68%). A table of included studies’ characteristics and anxiety data is available in the online appendix D, Supplemental Digital Content 1, http://links.lww.com/JCN/A11.
Quality of Included Studies
The assessment of study quality can be seen in Table B, Supplemental Digital Content 1, http://links.lww.com/JCN/A11, in the online appendices. The evaluation of the appropriateness of measurement instrument analyses can be seen in Table 2 and in Table C, Supplemental Digital Content 1, http://links.lww.com/JCN/A11, in the online appendices. The characteristics used in the assessment were as follows: evidence of probability sampling, adequate reporting of sampling characteristics, adequate response rates (80%> acceptable or 70%> if characteristics of nonresponders match responders), conceptualization of anxiety, standardized data collection, appropriateness of anxiety measure intrument (specifically the omission of somatic items and ability to distinguish between anxiety and depression), as determined through evaluation of available empirical literature.
The majority of the studies did report sufficient demographic and clinical data (76%), although many did not report a response rate (74%). Of the 72 studies in the review, 9 defined or operationalized the construct of anxiety.16,18,34,40–45 The choice of instrument to measure anxiety was a key quality component for the current review. Fourteen studies used instruments that were evaluated by the review team as containing somatic items; that is, items that assessed physical symptoms of anxiety42,46–54 or could not be considered to omit somatic items from assessment of anxiety entirely.35,43,55,56 Twenty-five studies used instruments to evaluate levels of anxiety or identify cases of anxiety that could not be said to effectively distinguish between anxiety and depression based on examination of available empirical literature. In the current review, only the Hospital Anxiety and Depression Scale (HADs), Brief Symptom Inventory-Anxiety (BSI-A), Generalised Anxiety Disorder 7-item (GAD-7), and the Patient Health Questionnaire (PHQ) for panic disorder and other anxiety disorders were evaluated as demonstrating sound psychometric evidence for their ability to distinguish between anxiety and depression. The table of quality assessment data and the table of anxiety measurement instruments are available in the online appendix B and C, Supplemental Digital Content 1, http://links.lww.com/JCN/A11.
Measurement of Anxiety
Six studies used clinical interviews or questionnaires to identify specific anxiety disorders including the Structured Clinical Interview,57,58International Classification of Diseases, Ninth Revision, Clinical Modification codes for GAD,59 GAD-7,32 the GAD-2, and the PHQ39 for panic and other anxiety disorders. Forty-five studies assessed symptoms of anxiety using questionnaires that facilitate the interpretation of scores as “normal,” “mild to moderate,” and “severe/probable clinical anxiety.” From these studies, 27 reported a prevalence rate using a range of recommended threshold to identify caseness of anxiety. The most commonly used instrument was HADs22 (n = 28 studies). A range of thresholds were used to identify anxiety using the HADs, ranging from 11> to 7>. Nineteen studies measured symptoms of anxiety using instruments that identify elevated levels of anxiety above a general population norm, with 8 of these studies reporting prevalence rates (Table 3).
TABLE 3.
Prevalence Estimates and Anxiety Symptom Severity from Meta-analysis, Grouped by Anxiety Conceptualiszation and Measurement Instrument
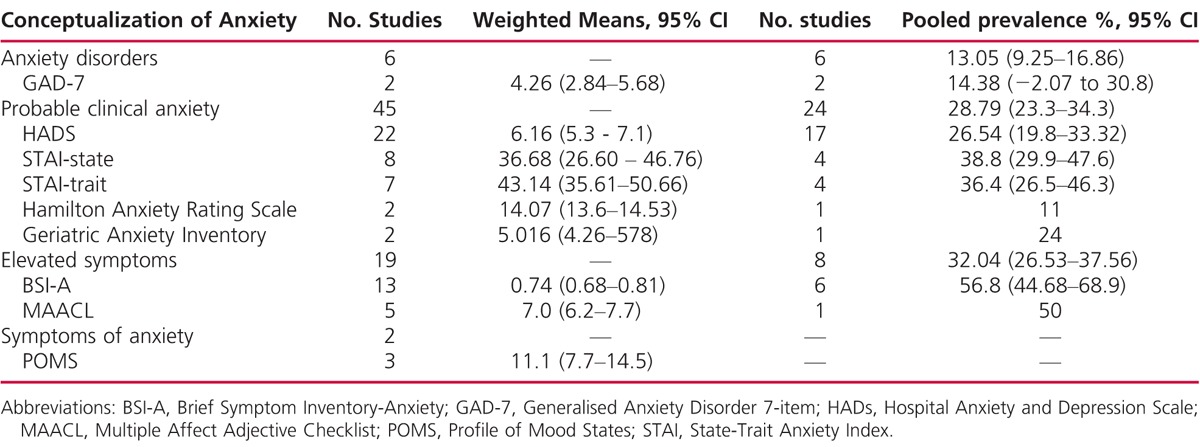
Prevalence of Anxiety: Meta-analysis
The prevalence of reported anxiety from 38 studies ranged from 6.3% to 72.3%, with an overall random effects pooled prevalence of 32% (95% confidence interval [CI], 26.5%–37.6%). Substantial heterogeneity in the rates of reported anxiety was found (x2 = 1745.1, df = 37, P = .000, I2 = 97.9%; Figure 2). Meta-analysis identified a random effects pooled prevalence of 13.1% (95% CI, 9.25%–16.86%) for anxiety disorders, 28.79% (95% CI, 23.30%–34.29%) for probable clinically significant anxiety and 55.5% (95% CI, 48.08%–62.83%) for elevated symptoms of anxiety. Combined prevalence and mean severity scores by measurement instruments identified in the review were also calculated (Table 3). Lower prevalence estimates were identified when studies used the GAD-7, HADs, and State Trait Anxiety Inventory compared with the BSI-A. Rates of anxiety were highest when measured by the BSI-A (56.8%; 95% CI, 44.7%–68.9%) and lowest when measured using an instrument to identify specific anxiety disorder, the Hamilton Anxiety Rating Scale (11%). High levels of heterogeneity were identified in all meta-analysis models (I2 >0.80).
FIGURE 2.
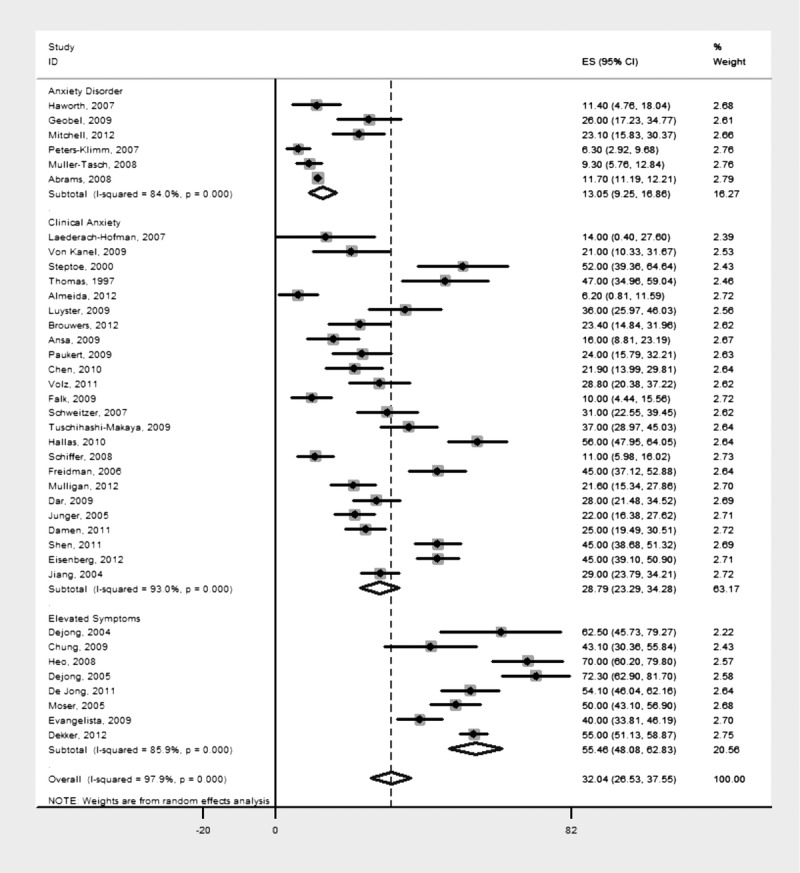
Prevalence of anxiety disorders, probable clinical anxiety, and elevated symptoms of anxiety in samples of patients with HF grouped by type of anxiety. 0 = specific anxiety disorders group; 1 = probable clinical anxiety group; 2 = elevated symptoms of anxiety above general population norms group. ES indicates effect size; CI, confidence interval.
Variations in Reported Anxiety: Meta-Regression
In univariate meta-regression analyses, studies in which anxiety had been conceptualized as specific anxiety disorders identified lower rates of anxiety compared with studies that measured clinical levels of anxiety symptoms (β = −14.40 standard error [SE(β)] = 5.63, P = 0.015 [)] and studies that measured symptoms of anxiety, identifying anxious individuals as those who scored higher than a general population norm (β = −41.24, standard error [SE(β)] = 6.77, P = .000 [)]. In addition, studies with a younger mean age (in years) reported higher prevalence rates of anxiety (compared with studies with an older mean age) (β = −1.01, standard error [SE(β)] = 0.41, P = .020), and studies with samples that had a higher proportion of females to males (as opposed to a higher proportion of males) had higher prevalence of anxiety (β = −0.62, standard error [SE(β)] = 0.21, P = .006). Studies conducted in the United States reported a higher prevalence of anxiety when compared with studies conducted in the United Kingdom and mainland Europe (β = −19.98, SE[β] = 5.78, P = .002). No other factors were found to explain the heterogeneity in overall prevalence rates to a significant level. A table of all meta-regression results is available in the online appendix E, Supplemental Digital Content 1, http://links.lww.com/JCN/A11.
In post hoc analysis, using a 2-factor meta-regression when controlling for the variance in rates of anxiety accounted for by the conceptualization and measurement of anxiety only, age (mean in years), NYHA functional class, and country of origin explained variations in anxiety prevalence to a significant degree. Studies with samples of a lower mean age (β = −0.79, SE[β] = 0.29, P = .009) and higher proportion of individuals with milder NYHA functional class (β = −15.06, SE[β] = 6.98, P = .041) originating from the United States (β = −11.20, SE[β] = 5.48, P = .050) reported increased prevalence rates of anxiety.
Discussion
This review identified and collates a vast amount of literature and offers the reader finer granularity regarding the prevalence of anxiety in populations of patient with HF. There are 3 main findings from the systematic review. First, random effects pooled prevalence estimate of anxiety was 32%. The pooled prevalence estimates of anxiety disorders (13%) are not considered unique to HF samples and have been observed in older adult community samples and clinical samples alike.12,60 The pooled prevalence estimates of probable clinical anxiety symptoms (29%) and elevated symptoms of anxiety (56%) were slightly higher than the rates found in older adult community samples (15%–52%),60 in clinical samples (15%–56%),60 samples of patients with CAD (20%–25%),61 after acute cardiac events (20%–25%),62 and after ICD intervention (24%–87%).63
Second, there was substantial heterogeneity among study prevalence estimates, indicating that pooled prevalence estimates should be interpreted with caution. Prevalence estimates ranged from 6.3% to 72.3%. In meta-regression analysis, the way in which anxiety had been conceptualized and measured in studies was most strongly associated with heterogeneity. Inflated rates of anxiety reported in the literature are most likely an artifact of measurement method.
Third, many different measurement instruments were used to identify anxiety in the included studies, some of which could be considered to have more clinical utility and are more appropriate for screening for anxiety in individuals with a diagnosis of HF than others.
Prevalence Rates
In a critical review of the literature in 2010, Yohannes et al23 identified only 8 studies that explored anxiety comorbid to HF, with prevalence estimates from 11%64 to 45%.65 The current review was designed to be more comprehensive with regard to methods and analysis and has identified considerably more studies that included a measure of anxiety in samples of individuals with a diagnosis of HF. The review shows that prevalence estimates of anxiety range substantially from 6.3% to 72.3%, with lower prevalence estimates found in studies measuring specific anxiety disorders as opposed to elevated levels of anxiety symptoms.
Meta-regression indicated that younger samples and those with a higher ratio of females to males record significantly higher levels of anxiety. The finding that overall anxiety increases as the proportion of females in a sample increases is consistently supported by research.66 Research examining anxiety in HF samples and after acute cardiac events identifies female patients as significantly more anxious than males.45,46,50,67 Whether this difference in prevalence rates reflects a behavioral, social, or physiological propensity toward anxiety in females is still unclear. Alternatively, or in addition, higher rates of anxiety identified in females may reflect a higher frequency in reporting in females compared with males. An increase in anxiety in younger samples is not reflected in the literature, with evidence from general population samples indicating that anxiety increases with age, with up to 17% of elderly men and 21.5% of elderly women experiencing severe anxiety, although the term elderly is not defined but does support research conducted with HF samples.68 It is unknown whether the difference in prevalence rates reflects a “real” variation in the prevalence of anxiety in younger and older aged adults or whether anxiety is underdiagnosed in elderly patients with HF. Alternatively, the mental health of elderly patients in general is overlooked by clinicians.69
The upper range of prevalence estimates found could indicate that levels of anxiety are higher in samples of patients with HF compared with many other cardiovascular conditions, with the exception of samples immediately after invasive procedures. However, the instruments used to measure anxiety symptoms and thresholds used to identify caseness of anxiety have played a crucial role in determining the levels of anxiety identified in the current review. Variations in prevalence estimates may not always reflect true differences in anxiety between different patient populations, but they may be an artifact of measurement.
Measurement and Relevance for Clinical Practice
Anxiety was measured using 11 different questionnaires or interviews methods. Scores on questionnaire measures were interpreted using a variety of different threshold to define anxiety, making synthesis of outcome data difficult, across and within measurement instruments. The quality of measurement instruments varied. Only some have been evaluated by the review team as appropriate for use in cardiac, elderly samples and are able to distinguish between anxiety and depression.
Only 1 study used a criterion standard diagnostic tool the Structured Clinical Interview for Diagnostic Statistical Manual I57 to diagnose specific anxiety disorders,16 corresponding to United Kingdom’s National Institute of Care and Health Excellence (NICE) guidelines for the assessment of generalized anxiety disorder in primary, secondary, and community care.67 Although this method of assessing patients is considered robust, it can take more than an hour to assess patients and involves subjective interpretation of self-reported symptoms by a skilled interviewer. This instrument is unlikely to be appropriate for routine use to screen patients with HF for mental health complaints in clinical practice owing to the time taken to complete the assessment and the training required to conduct the interview. Table 2 presents other measures identified from the review and highlights key characteristics of interest for clinical practice. The HADs was the most frequently used measurement instrument in the studies included in the review, followed by the State Trait Anxiety Inventory and the BSI-A. The HADs was used mainly in studies from the United Kingdom and Europe, with the majority of studies applying a threshold of 8 to identify mild anxiety, which has been supported through psychometric testing of specificity and sensitivity.70 The instrument is routinely used in both primary and secondary care in the United Kingdom, which makes the choice of this measure appropriate in the United Kingdom context; however, issues with the language used in the measure has reduced its application in the United States.71 The majority of studies conducted since the start of 2010 used the HADs to screen for mild, moderate, and severe levels of anxiety symptoms. Indeed, many of the studies chose to present the prevalence of anxiety for more than 1 level of anxiety severity, which mirrors the use of the HADs in clinical practice and the ability of the instrument to match patients to “stepped care” treatment options.
Both the BSI-A72,73 and the Multiple Affect Adjective Checklist (MAACL)74 were used to measure symptoms of anxiety and identify anxious cases with reference to data from general population samples. All of the studies using these measures originated from the United States, which likely explains the higher rates of anxiety found by country in the meta-regression. Although it may be suggested that higher rates of anxiety identified in US studies could reflect differences in care patterns. The BSI-A and the MAACL are not widely used in the United Kingdom, where the HADs and GAD-7 currently meet the needs of assessing anxiety in an elderly cardiac population. The use of the BSI-A and MAACL and the interpretation of scores derived from them based on comparison with general population norms produced the highest levels of anxiety observed in the review. Increases in the level of anxiety on the BSI-A and MAACL are difficult to interpret clinically because no thresholds have been identified to indicate mild/moderate or severe levels of anxiety. Because these instruments identify individuals with elevated symptoms of anxiety using low thresholds (general population norms), it is not surprising that they identify extremely high prevalence estimates of anxiety. However, the clinical relevance of identifying such a wide range in the levels of anxiety is unknown, as is the ability to target patients at the right treatment using either the BSI-A or the MAACL.
The GAD-7 offers a solution to the problem of assessing anxiety using criteria of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, in a very short space of time. The GAD-732 is one of the minimum data set requirements used by the Increasing Access to Psychological Treatment (IAPT) program in the United Kingdom to screen for and identify caseness of anxiety (mild/moderate).75 Although widely used in the United Kingdom primary care settings, it was interesting to note that no studies conducted in the United Kingdom included in the current review used the instrument. This is likely to be due to the fact that the IAPT program is a relatively new national initiative, running in primary care services. Many of the studies included in the review would have been conducted before its initiation, and the majority of research to date has sampled outpatients, primarily from secondary services. The GAD-7 and its predecessor, the PHQ, were used in research from the United States and Germany in the current review. The instrument is free to use and very brief (7 items). It contains no questions relating to somatic complaints and can distinguish between anxiety and depression, making its use in cardiac populations appropriate.32 Scores higher than 10 have been found to correspond to caseness of moderate to severe anxiety32 that can impact an individual’s ability to perform everyday activities and cause marked distress but responds well to psychological interventions (NICE, 2011; IAPT Toolkit, 2008). The use of the instrument should be encouraged within the United Kingdom and internationally as large amounts of data are being routinely collected using this instrument. In addition, the instrument is open source and free to use.
Methodological Considerations
Although this review is comprehensive and the first of its kind, several limitations exist, including the exclusion of non-English language articles and dissertations. Although studies were excluded from the review if they did not use a validated measure of anxiety signs and symptoms, study design was not an exclusion criterion and the review may contain studies considered to be of lower quality, which could have an impact on the robustness of reported prevalence rates and precision of estimates. However, the use of observational studies in systematic reviews and meta-analyses is fairly common and has increased noticeably in the last 2 decades, particularly in areas where little randomized controlled trial or effectiveness research exists.76,77 To increase precision in prevalence estimates, studies were clustered according to the manner in which they conceptualized and measured anxiety, which should go some way to increasing the precision of estimates. Study design was included as a variable in meta-regression, but it was not found to be associated with variance in prevalence estimates.
For synthesis and appraisal purposes, the manner in which studies have conceptualized and measured anxiety has been subjectively categorized in this review into the following categories: anxiety disorder (studies that measured specific anxiety disorders), probable clinical anxiety (studies that used measures to screen for levels of probable anxiety above a given threshold), and elevated symptoms of anxiety (studies that used questionnaires to measure anxiety symptoms that reached levels above the norm for the general population). This clustering of measures was subjective, and the decision taken was pragmatic to capture a comprehensive range of data. We have been transparent in regard to this decision and welcome debate. The validity or appropriateness of measurement instruments has been subjectively evaluated as part of the quality assessment on the basis of available empirical evidence and in consultation with the review team. It is hoped that transparency with regard to the appraisal process of measures should allow decisions to be scrutinized.
The percentage of males in the included studies was high, which may reflect the inclusion of studies of veterans in the review with predominantly male samples. Although the findings are representative of the academic literature, this may reduce the ability to extrapolate from the data to clinical populations. The findings from the review should be interpreted with caution in light of this.
Furthermore, high levels of heterogeneity were found between studies and small numbers of observations involved in meta-regression analyses. However, when using the I2 test, substantial variability exists in the literature with regard to acceptable upper limits,78 making it difficult to determine just how much heterogeneity is acceptable between studies. Further exploration of sources of heterogeneity in anxiety prevalence estimates and subgroup analysis within concepts of anxiety was often not possible owing to the small number of observations and collinearity of data. No clear consensus exists regarding the lower limit to the number of studies that a meta-regression should be performed on. Simulations to test the stability of parameter estimates indicate that fewer than 10 studies produce unstable estimates, a problem exacerbated further when sample sizes are small.79 The reader is advised to interpret findings from meta-regression with caution. More stringent inclusion criteria may have improved the issue of variability; however, substantial heterogeneity existed even within studies grouped by specific measurement instruments.
Finally, the use of meta-analysis with studies that contain significant amounts of heterogeneity with respect to outcomes, sample characteristics, and study design is controversial. However, the use of meta-analysis and meta-regression is considered justifiable, if not essential for exploration of stratified prevalence estimates.78
Conclusions
The current review provides researchers and clinicians with more precise estimates for the prevalence of anxiety in populations of patients with HF. The mental health of patients with a long term condition including those with HF, is often neglected in clinical practice.78,79 What is evident from the review is that a proportion of individuals with a diagnosis of HF are experiencing symptoms of anxiety that may impair their health and well-being. If identified, these patients may benefit from clinical interventions. Future research should consider the overlap in symptoms for patients with both physical and emotional conditions and help to guide appropriate screening of common mental health conditions in this patient population. Access to psychological services can be limited and waiting lists long. Therefore, it is important to target available services to those most in need. The clinical utility of some measurement instruments that have been identified in the review has been questioned. Clinicians must select measurement instruments with service provisions in mind.
What’s New and Important?
Anxiety prevalence estimates range from 6.3% to 72.3%. The review offers insight into variances with regard to demographics and measurement.
A random effects pooled prevalence of 13.1% for anxiety disorders, 28.79% for probable clinically significant anxiety, and 55.5% for elevated symptoms of anxiety was identified. Rates of anxiety were highest when measured by the BSI-A and lowest when using the Hamilton Anxiety Rating Scale measured.
Anxiety was assessed using 11 different measurement instruments, not all of which may be considered appropriate for use in the given clinical population.
The review is the most comprehensive and methodologically rigorous on this subject matter.
Footnotes
The research was funded through an interdisciplinary doctoral studentship jointly funded by the Medical Research Council and the Economics and Social Research Council.
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jcnjournal.com).
REFERENCES
- 1.Cimpean D, Drake R. Treating co-morbid medical conditions and anxiety/depression. Epidemiol Psychiatr Sci. 2011;20(2):141–150. [DOI] [PubMed] [Google Scholar]
- 2.Naylor C, Parsonage M, McDaid D, Knapp M, Fossey M, Galea A. Long-term conditions and mental health: the cost of co-morbidity [report]. The King’s Fund and Centre for Mental Health. 2012. [Google Scholar]
- 3.Vaccarino V, Kasl V. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol. 2001;38(1):199–205. [DOI] [PubMed] [Google Scholar]
- 4.Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161(15):1849–1856. [DOI] [PubMed] [Google Scholar]
- 5.Hallas CN, Wray J, Andreou P, Banner NR. Depression and perceptions about heart failure predict quality of life in patients with advanced heart failure. Heart Lung. 2011;40(2):111–121. [DOI] [PubMed] [Google Scholar]
- 6.Cully JA, Phillips LL, Kunik ME, Stanley MA, Deswal A. Predicting quality of life in veterans with heart failure: the role of disease severity, depression, and comorbid anxiety. Behav Med. 2010;36(2):70–76. [DOI] [PubMed] [Google Scholar]
- 7.Rutledge T, Reis SE, Olson MB, et al. Depression symptom severity and reported treatment history in the prediction of cardiac risk in women with suspected myocardial ischemia: The NHLBI-Sponsored WISE Study. Arch Gen Psychiatry. 1996;63(8):874–880. [DOI] [PubMed] [Google Scholar]
- 8.Konstam V, Salem D, Pouleur H, et al. Baseline quality of life as a predictor of mortality and hospitalization in 5,025 patients with congestive heart failure. SOLVD Investigations. Studies of Left Ventricular Dysfunction Investigators. Am J Cardiol. 1996;78(8):890–895. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence. Clinical Guideline 90. Depression: The Treatment and Management of Depression in Adults. London, England: National Collaborating Centre for Mental Health; 2009. [Google Scholar]
- 10.Konstam V, Moser DK, De Jong MJ. Depression and anxiety in heart failure. J Card Fail. 2005;11(6):455–463. [DOI] [PubMed] [Google Scholar]
- 11.Merikangas K, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community sample: The Zurich Cohort Study. Arch Gen Psychiatry. 2003;60:993–1000. [DOI] [PubMed] [Google Scholar]
- 12.MacMahon KM, Lip GY. Psychological factors in heart failure: a review of the literature. Arch Intern Med. 2002;162(5):509–516. [DOI] [PubMed] [Google Scholar]
- 13.Haworth JE, Moniz-Cook E, Clark AL, Wang M, Waddington R, Cleland JGF. Prevalence and predictors of anxiety and depression in a sample of chronic heart failure patients with left ventricular systolic dysfunction. Eur J Heart Fail. 2005;7(5):803–808. [DOI] [PubMed] [Google Scholar]
- 14.Shen BJ, Eisenberg SA, Maeda U, et al. Depression and anxiety predict decline in physical health functioning in patients with heart failure. Ann Behav Med. 2011;41(3):373–382. [DOI] [PubMed] [Google Scholar]
- 15.Volz A, Schmid JP, Zwahlen M, Kohls S, Saner H, Barth J. Predictors of readmission and health related quality of life in patients with chronic heart failure: a comparison of different psychosocial aspects. J Behav Med. 2011;34(1):13–22. [DOI] [PubMed] [Google Scholar]
- 16.Haworth JE, Moniz-Cook E, Clark AL, Wang M, Cleland JGF. An evaluation of two self-report screening measures for mood in an out-patient chronic heart failure population. Int J Geriatr Psychiatry. 2007;22(11):1147–1153. [DOI] [PubMed] [Google Scholar]
- 17.Evangelista LS, Ter-Galstanyan A, Moughrabi S, Moser DK. Anxiety and depression in ethnic minorities with chronic heart failure. J Card Fail. 2009;15(7):572–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Jong MJ, Moser DK, Chung ML. Anxiety, depression, and functional status are the best predictors of health status for patients with heart failure. J Card Fail. 2004;10(4):014. [Google Scholar]
- 19.Heo S, Moser DK, Lennie TA, Zambroski CH, Chung ML. A comparison of health-related quality of life between older adults with heart failure and healthy older adults. Heart Lung. 2007;36(1):16–24. [DOI] [PubMed] [Google Scholar]
- 20.Singleton N, Bumpstead R, O’Brien M, et al. Psychiatric Morbidity Among Adults Living in Private Households, 2000. London, England: The Stationery Office; 2001. [DOI] [PubMed] [Google Scholar]
- 21.Easton K. An Investigation Into the Nature, Prevalence and Severity of Anxiety in Heart Failure Patients: The Association Between Anxiety and Patient’ Health Outcomes [doctoral thesis]. United Kingdom: The University of Manchester; 2013. https://www.escholar.manchester.ac.uk/uk-ac-man-scw:212272. Accessed March 27, 2015. [Google Scholar]
- 22.Zigmond AS, Snaith R. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. [DOI] [PubMed] [Google Scholar]
- 23.Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry. 2010;25(12):1209–1221. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. 4th ed Washington, DC: American Psychiatric Association; 2004. [Google Scholar]
- 25.Ware J, Sherbourne C. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 26.Gellatly J, Bower P, Hennessy S, Richards D, Gilbody S, Lovell K. What makes self-help interventions effective in the management of depressive symptoms? Meta-analysis and meta-regression. Psychol Med. 2007;37(9):1217–1228. [DOI] [PubMed] [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simunovic N. Methodological issues in systematic reviews and meta-analyses of observational studies in orthopaedic research. J Bone Joint Surg Am. 2009. 1;91(suppl 3):87–94. [DOI] [PubMed] [Google Scholar]
- 29.Deeks J, Dinnes J, D’Amico R, Sowden A, Sakarovitch C. Evaluating non-randomised intervention studies. Health Technol Assess. 2003;7(27):186. [DOI] [PubMed] [Google Scholar]
- 30.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. PLoS Med. 2007;4:e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boyle MH. Guidelines for evaluating prevalence studies. Evid Based Ment Health. 1998;1(2):37–39. [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 33.Crawford J, Henry J, Crombie C, Taylor EP.Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol. 2001;40(4):429–434. [DOI] [PubMed] [Google Scholar]
- 34.Jiang W, Kuchibhatla M, Cuffe MS, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110(22):3452–3456. [DOI] [PubMed] [Google Scholar]
- 35.Clarke SP, Frasure-Smith N, Lesperance F, Bourassa MG. Psychosocial factors as predictors of functional status at 1 year in patients with left ventricular dysfunction. Res Nurs Health. 2000;23(4):290–300. [DOI] [PubMed] [Google Scholar]
- 36.Sutton A. Systematic reviews of trials and other studies. Health Technol Assess. 1998;2(19):1–276. [PubMed] [Google Scholar]
- 37.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 39.Thompson SG, Higgins JPT. How should meta-regression analyses be undertaken and interpreted? Stat Med. 2002;21(11):1559–1574. [DOI] [PubMed] [Google Scholar]
- 40.Eisenberg SA, Shen BJ, Schwarz ER, Mallon S. Avoidant coping moderates the association between anxiety and patient-rated physical functioning in heart failure patients. J Behav Med. 2012;35(3):253–261. [DOI] [PubMed] [Google Scholar]
- 41.Peters-Klimm F, Muller-Tasch T, Schellberg D, et al. Rationale, design and conduct of a randomised controlled trial evaluating a primary care-based complex intervention to improve the quality of life of heart failure patients: HICMan (Heidelberg Integrated Case Management). BMC Cardiovasc Disord. 2007;7:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muller-Tasch T, Frankenstein L, Holzapfel N, et al. Panic disorder in patients with chronic heart failure. J Psychosom Res. 2008;64(3):299–303. [DOI] [PubMed] [Google Scholar]
- 43.Abrams TE, Vaughan-Sarrazin M, Rosenthal GE. Variations in the associations between psychiatric comorbidity and hospital mortality according to the method of identifying psychiatric diagnoses. J Gen Intern Med. 2008;23(3):317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kulcu DG, Kurtais Y, Tur BS, Gulec S, Seckin B. The effect of cardiac rehabilitation on quality of life, anxiety and depression in patients with congestive heart failure. A randomized controlled trial, short-term results. Eura Medicophys. 2007;43(4):489–497. [PubMed] [Google Scholar]
- 45.Schweitzer RD, Head K, Dwyer JW. Psychological factors and treatment adherence behavior in patients with chronic heart failure. J Cardiovasc Nurs. 2007;22(1):76–83. [DOI] [PubMed] [Google Scholar]
- 46.Moser DK, Dracup K, Evangelista LS, et al. Comparison of prevalence of symptoms of depression, anxiety, and hostility in elderly patients with heart failure, myocardial infarction, and a coronary artery bypass graft. Heart Lung. 2010;39(5):378–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Serafini G, Pompili M, Innamorati M, Iacorossi G, Cuomo I, Vista MD, et al. The impact of anxiety, depression, and suicidality on quality of life and functional status of patients with congestive heart failure and hypertension: an observational cross-sectional study. Prim Care Companion J Clin Psychiatry. 2010;12(6):e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schiffer AA, Pedersen SS, Broers H, Widdershoven JW, Denollet J. Type-D personality but not depression predicts severity of anxiety in heart failure patients at 1-year follow-up. J Affect Disord. 2008;106(1–2):73–81. [DOI] [PubMed] [Google Scholar]
- 49.Kostis JB, Rosen RC, Cosgrove NM, Shindler DM, Wilson AC. Non-pharmacologic therapy improves functional and emotional status in congestive heart failure. Chest. 1994;106(4):996–1001. [DOI] [PubMed] [Google Scholar]
- 50.Paukert AL, LeMaire A, Cully JA. Predictors of depressive symptoms in older veterans with heart failure. Aging Ment Health. 2009;13(4):601–610. [DOI] [PubMed] [Google Scholar]
- 51.Corvera-Tindel T, Doering LV, Roper J, Dracup K. Emotional functioning drives quality of life in men with heart failure. Prog Cardiovasc Nurs. 2009;24(1):2–11. [DOI] [PubMed] [Google Scholar]
- 52.Dracup K, Westlake C, Erickson VS, Moser DK, Caldwell ML, Hamilton MA. Perceived control reduces emotional stress in patients with heart failure. J Heart Lung Transplant. 2003;22(1):90–93. [DOI] [PubMed] [Google Scholar]
- 53.Dracup K, Evangelista LS, Hamilton MA, et al. Effects of a home-based exercise program on clinical outcomes in heart failure. Am Heart J. 2007;154(5):877–883. [DOI] [PubMed] [Google Scholar]
- 54.Moser DK, Doering LV, Chung ML. Vulnerabilities of patients recovering from an exacerbation of chronic heart failure. Am Heart J. 2005;150(5):984. [DOI] [PubMed] [Google Scholar]
- 55.Doering LV, Dracup K, Caldwell MA, et al. Is coping style linked to emotional states in heart failure patients? J Card Fail. 2004;10(4):344–349. [DOI] [PubMed] [Google Scholar]
- 56.Sullivan MJ, Wood L, Terry J, et al. The Support, Education, and Research in Chronic Heart Failure Study (SEARCH): a mindfulness-based psychoeducational intervention improves depression and clinical symptoms in patients with chronic heart failure. Am Heart J. 2009;157(1):84–90. [DOI] [PubMed] [Google Scholar]
- 57.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV). Washington, DC: American Psychiatric Press, Inc; 1996. [Google Scholar]
- 58.Spitzer RL, Williams JW, Kroenke K. Utility of a new procedure for diagnosing mental disorders in primary care: The prime-md 1000 study. JAMA. 1994;272(22):1749–1756. [PubMed] [Google Scholar]
- 59.World Health Organization. World Health Organisation (2010) ICD 10: Version 10. http://appswho int/classifications/icd10/browse/2010/en 2014.
- 60.Bryant C, Jackson H, Ames D. The prevalence of anxiety in older adults: methodological issues and a review of the literature. J Affect Disord. 2008;109(3):233–250. [DOI] [PubMed] [Google Scholar]
- 61.Januzzi JL, Jr, Stern TA, Pasternak RC, DeSanctis RW. The influence of anxiety and depression on outcomes of patients with coronary artery disease. Arch Intern Med. 2000;160(13): 1913–1921. [DOI] [PubMed] [Google Scholar]
- 62.Moser DK, Dracup K. Is anxiety early after myocardial infarction associated with subsequent ischemic and arrhythmic events? Psychosom Med. 1996;58(5):395–401. [DOI] [PubMed] [Google Scholar]
- 63.Sear S, Conti J. Quality of life and psychological functioning of ICD patients. Heart. 2002;87(5):488–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yu DS, Thompson DR, Yu CM, Oldridge NB. Assessing HRQL among Chinese patients with coronary heart disease: angina, myocardial infarction and heart failure. Int J Cardiol. 2009;131(3):384–394. [DOI] [PubMed] [Google Scholar]
- 65.Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152(5):940. [DOI] [PubMed] [Google Scholar]
- 66.Brown T, O’Leary T, Barlow D. Generalised anxiety disorder. In: Barlow DH. ed. Clinical handbook of psyhcological disorders: a step-by-step treatment manual. 3rd ed New York, NY: Guilford Press; 2001. [Google Scholar]
- 67.Moser DK. “The rust of life”: impact of anxiety on cardiac patients. Am J Crit Care. 2007;16(4):361–369. [PMC free article] [PubMed] [Google Scholar]
- 68.Heo S, Moser DK, Widener J. Gender differences in the effects of physical and emotional symptoms on health-related quality of life in patients with heart failure. Eur J Cardiovasc Nurs. 2007;6(2):146–152. [DOI] [PubMed] [Google Scholar]
- 69.Lenze EJ, Mulsant BH, Shear MK, Alexopoulos GS, Frank E, Reynolds CF. Comorbidity of depression and anxiety disorders in later life. Depress Anxiety. 2001;14(2):86–93. [DOI] [PubMed] [Google Scholar]
- 70.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77. [DOI] [PubMed] [Google Scholar]
- 71.Coyne J, Van Sonderen E. The Hospital Anxiety and Depression Scale (HADS) is dead, but like Elvis, there will still be citings. J Psychosom Res. 2012;73(1):77–78. [Google Scholar]
- 72.Ruz A, Lennie T, Reigalel B, McKinley S, Doering L, Moser D. Evidence that the brief symptom inventory can be used to measure anxiety quickly and reliably in patients hospitalized for acute myocardial infarction. J Cardiovasc Nurs. 2010;25(5):117–123. [DOI] [PubMed] [Google Scholar]
- 73.Derogatis R, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- 74.Zuckerman M, Lubin B. Manual for the Multiple Affect Adjective Check List-Revised (MAACL-R). San Diego, CA: Educational and Industrial Testing Service; 1985. [Google Scholar]
- 75.National IAPT Programme Team. The IAPT Data Handbook. 2011. http://www.iapt.nhs.uk/silo/files/the-iapt-data-handbook.pdf. Accessed March 27, 2015.
- 76.Dickersin K. Systematic reviews in epidemiology: why are we so far behind? Int J Epidemiol. 2002;31(1):6–12. [DOI] [PubMed] [Google Scholar]
- 77.Egger M, Davey Smith G, Altman D. Systematic Reviews in Health Care: Meta-analysis in Context. 2nd ed. London, England: BMJ; 2001. [Google Scholar]
- 78.Ioannidis J, Patsopoulos N, Rothstein H. Reasons or excuses for avoiding meta-analysis in forest plots. BMJ. 2008;336(1413):1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Morton S. Meta-regression approaches: what, why, when and how? Rockville, MD: Agency for Healthcare Research and Quality. Technical Review 8. AHRQ Publication No 04–0033; 2004. [PubMed] [Google Scholar]


