Abstract
Intravenous administration of vitamin C has been shown to decrease oxidative stress and, in some instances, improve physiological function in adult humans. Oral vitamin C administration is typically less effective than intravenous, due in part to inferior vitamin C bioavailability. The purpose of this study was to determine the efficacy of oral delivery of vitamin C encapsulated in liposomes. On 4 separate randomly ordered occasions, 11 men and women were administered an oral placebo, or 4 g of vitamin C via oral, oral liposomal, or intravenous delivery. The data indicate that oral delivery of 4 g of vitamin C encapsulated in liposomes (1) produces circulating concentrations of vitamin C that are greater than unencapsulated oral but less than intravenous administration and (2) provides protection from ischemia–reperfusion-mediated oxidative stress that is similar to the protection provided by unencapsulated oral and intravenous administrations.
Keywords: liposome, oral, intravenous, oxidative stress, thiobarbituric acid reactive substances
Introduction
Infusion of vitamin C, via arteries or veins, has been reported to decrease oxidative stress1–3 and, in many instances, improve physiological function in adult humans. Reported beneficial effects include, but are not limited to, increased baroreflex sensitivity,4 improved endothelial function and vascular conductance,5–8 augmented inotropic and thermogenic response to beta-adrenergic stimulation,9,10 decreased systemic inflammation and reduced fluid requirements during recovery from thermal injury,11 fatigue resistance in clinical populations,3 and cancer cell-specific toxicity.12 Compared with vitamin C infusion, oral vitamin C administration is typically less effective, in part due to inferior vitamin C bioavailability.13,14
Following ingestion, subsequent vitamin C bioavailability is largely determined by rates of intestinal absorption and further influenced by renal reabsorption and excretion.14–16 Sodium-dependent vitamin C transporters 1 and 2 are the primary mediators of intestinal absorption and renal reabsorption;14–16 Sodium-dependent vitamin C transporter 2 also facilitates entry of vitamin C into most metabolically active cells and tissues.17 Direct infusion of vitamin C bypasses the dependency on intestinal absorption; thus, high circulating concentrations are achieved soon after administration.13 Infusion of vitamin C is an impractical mode of administration for most of the general public and also carries a risk of infection, discomfort, and phlebitis. Accordingly, an alternative mode of effective vitamin C delivery is of obvious interest. In this regard, oral consumption of vitamin C encapsulated in liposomes may hold promise.
Liposomes are manufactured microscopic, hollow spherical vesicles composed of a lipid bilayer. When loaded with pharmaceuticals and/or dietary supplements, liposomes are a very effective method of drug/supplement delivery. When ingested, the pharmacokinetic properties of liposome intestinal absorption override the usual absorption pattern of the encapsulated drug. That is, the delivery of a drug/supplement with a typically slow or regulated pattern of absorption, such as vitamin C, may be accelerated when encapsulated within a liposome.18,19 Consistent with this idea, the purpose of the current investigation was to compare the circulating concentrations of vitamin C following oral ingestion of vitamin C encapsulated within liposomes and oral ingestion of unencapsulated vitamin C. To provide a point of reference, we have also quantified circulating concentrations of vitamin C following intravenous administration of an equivalent dose. We hypothesized that the ingestion of vitamin C encapsulated within liposomes would evoke greater circulating concentrations of vitamin C than ingestion of an equivalent dose of unencapsulated vitamin C. Furthermore, to investigate a functional implication of enhanced vitamin C delivery, we have quantified the magnitude of increase in circulating concentrations of a biomarker of oxidative stress following a forearm ischemia–reperfusion injury. Consistent with increasing bioavailability, we hypothesized that liposomal vitamin C would better attenuate oxidative stress induced by ischemia–reperfusion compared with unencapsulated vitamin C.
Methods
Research participants
We studied 11 adult humans, and selected physical characteristics of research participants are presented in Table 1. Inclusion criteria included age within the range of 45–70 years and overweight or obese as defined by body mass index (>25 kg/m2). Baseline oxidative stress is typically high in overweight/obese adults within this age range.20,21 Exclusion criteria included use of vitamins, supplements, or medications known to decrease oxidative stress during the three months prior to initiation of participation, pregnant or nursing, history of allergic reaction or hypersensitivity to vitamin supplements, history of kidney stones, current or past use (previous two years) of tobacco products, and concurrent participation in another study. The experimental protocol conformed to the standards set by the Declaration of Helsinki of 1975, as revised in 1983, and was approved by the Institutional Review Board at Colorado State University. The nature, purpose, and risks of the study were explained to each research participant before written informed consent was obtained.
Table 1.
Selected physical characteristics of research participants (n = 11).
| MEAN ± SE | |
|---|---|
| Sex (M/F) | 2/9 |
| Age (years) | 53 ± 2 |
| Height (m) | 1.62 ± 0.02 |
| Body mass (kg) | 89.0 ± 2.9 |
| Body mass index (kg/m2) | 34.1 ± 1.0 |
| Baseline plasma vitamin C (mg/dL)a | 0.84 ± 0.05 |
| Baseline TBARS (μM MDA)a | 5.82 ± 0.81 |
Note:
After 12-hour fast, prior to placebo treatment administration.
Abbreviations: TBARS, thiobarbituric acid reactive substances; MDA, malondialdehyde.
Experimental design and overview
Following screening, research participants reported to the laboratory on four randomly ordered separate occasions, separated by a minimum of seven days. Research participants were administered an oral placebo or 4 g of vitamin C encapsulated within liposomes, unencapsulated, or via intravenous infusion. The rationale for 4 g dose of vitamin C was based on previous studies that have demonstrated favorable outcomes pertinent to oxidative stress and physiological function.1,4,5,9,22 Three hours after administration, participants completed a forearm ischemia–reperfusion protocol. Venous blood was sampled at baseline and throughout the experimental visit for the determination of circulating concentrations of vitamin C and markers of oxidative stress.
Screening
The screening visit comprised completion of a medical history questionnaire, measurement of height (via a stadiometer) and body mass (via a physician’s scale), calculation of body mass index [body mass/height2 (kg/m2)], and familiarization with the forearm ischemia–reperfusion protocol.
Treatment visits
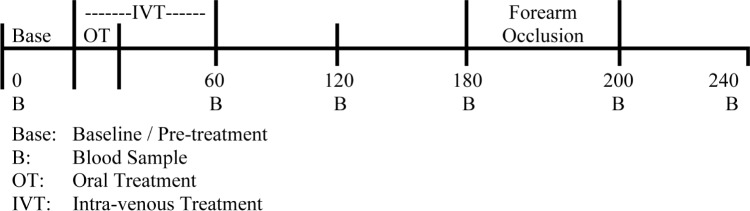
Participants reported to the laboratory on four randomly ordered separate occasions, separated by a minimum of seven days, each following a 12-hour fast and 24-hour abstention from exercise (Fig. 1). An intravenous catheter was placed in an antecubital vein for repeated blood sampling. The catheter was kept patent with a saline drip. Following baseline blood collection, participants were administered one of the following four treatments: (1) placebo, oral consumption of 16 mL of water; (2) oral consumption of unencapsulated vitamin C, 4.25 g of 94% sodium ascor-bate (equivalent to 4 g of vitamin C) dissolved in 16 mL of water; (3) oral consumption of vitamin C encapsulated in liposomes (equivalent to 4 g of vitamin C) suspended in 16 mL of ultrahigh purity water (see below for more details); and (4) intravenous administration of vitamin C (Bioniche Pharma), 4 g dissolved in 100 mL of saline and administered by automated infusion pump (Harvard Apparatus) over one hour (1.667 mL/min, equivalent to 67 mg/min).22
Figure 1.
Schematic representation of protocol. On four separate occasions, following baseline blood collection, participants were administered either an oral placebo or 4 g of vitamin C via oral, oral liposomal, or intravenous delivery. Three hours after initiation of treatment, a blood pressure cuff was placed around the upper arm and inflated to 200 mmHg for 20 minutes.
Three hours after initiation of treatment, a blood pressure cuff was placed around the upper arm (proximal to the venous catheter) and inflated to 200 mmHg for 20 minutes using a rapid cuff inflator system (Hokanson). Venous blood was sampled at baseline and at minutes 60, 120, 180 (precuff inflation), 200 (postcuff inflation), and 240.
Preparation of liposomes
The liposomes were provided by Empirical Labs. The formula consisted of 136 mg of mixed natural phospholipids and 284 mg of USP sodium ascorbate (NaA), in a total volume of 1 mL with ultrahigh purity water (conductivity <0.065 μS/cm). All of the ingredients used in the formulation were classified by the United States Food and Drug Administration as Generally Recognized as Safe and had no known toxicity. Particle size was determined via microparticle tracking (Microtrac S3500; Microtrac) and confirmed with dynamic light scattering.
Plasma vitamin C
Venous blood (~5 mL) was collected in prechilled heparin-coated tubes, placed immediately on ice, centrifuged within 30 minutes (3600 rpm for 10 minutes at 4°C) to isolate plasma, and then transferred to opaque tubes and stored at −80°C. During the laboratory visit when vitamin C was intravenously administered, extreme caution was used when collecting blood immediately postinfusion to avoid the contamination of samples with vitamin C. Preventive measures included flushing of the stopcock with ~10 mL of saline and discarding the first ~8 mL of blood. Within seven days of collection, plasma vitamin C concentration was determined via high-performance liquid chromatography with electrochemical detection by a commercial laboratory (Laboratory Corporation of America). Noteworthy, the personnel of the commercial laboratory was naive as to treatments and conditions under which the samples were collected.
Oxidative stress
Blood samples to be used for measuring a marker of oxidative stress were collected in prechilled tubes containing ethylenediamine tetraacetic acid, placed immediately on ice, and centrifuged within 30 minutes (3600 rpm for 10 minutes at 4°C) to isolate plasma. Plasma was stored at −80°C until analysis. Plasma concentrations of thiobarbituric acid reactive substances (TBARS) were determined using calorimetric detection (Cayman Chemical). All samples were coded such that the research personnel analyzing the plasma was naive as to treatments and conditions under which the plasma was collected.
Statistical analysis
This was a randomized, placebo-controlled, repeated measures experimental design. Accordingly, analysis of variance (treatment × time) with repeated measures was used to examine the changes in circulating concentrations of vitamin C and MDA. Multiple comparisons of factor means were performed using Newman–Keuls test. One-way analysis of variance with repeated measures was used to compare areas under the circulating vitamin C and TBARS concentration curves. Areas under the curve were calculated via the trapezoidal rule. The level of statistical significance was set at P < 0.05. Data are reported as mean ± SE.
Results
Research participants
All 11 of the enrolled research participants completed the study. The vitamin C, irrespective of mode of delivery, was well tolerated, and there were no adverse events. Selected physical characteristics of the research participants are presented in Table 1. As a group, the research participants were obese, middle-aged, and older men and women.
Plasma vitamin C concentration
Baseline circulating concentrations of vitamin C did not differ between treatments. On average, the baseline concentrations were slightly lower than recommended values.15,23 Circulating concentrations of vitamin C prior to and following administration are presented in Figure 2A and B. Plasma vitamin C concentrations were greatest following intravenous administration at all time points compared with each of the other modes of delivery (P < 0.001). At two, three, and four hours, plasma vitamin C concentrations were greater after oral administration of vitamin C encapsulated in liposomes compared with placebo and unencapsulated vitamin C (P < 0.01); and unencapsulated vitamin C produced greater concentrations than placebo (P < 0.01). Consistent with these data, oral delivery of vitamin C encapsulated in liposomes (10.3 ± 0.9 mg/dL h) evoked a greater (P = 0.002) area under the curve than unencapsulated vitamin C (7.6 ± 0.4 mg/dL h) that in turn was greater (P < 0.001) than placebo (3.1 ± 0.4 mg/dL h).
Figure 2.
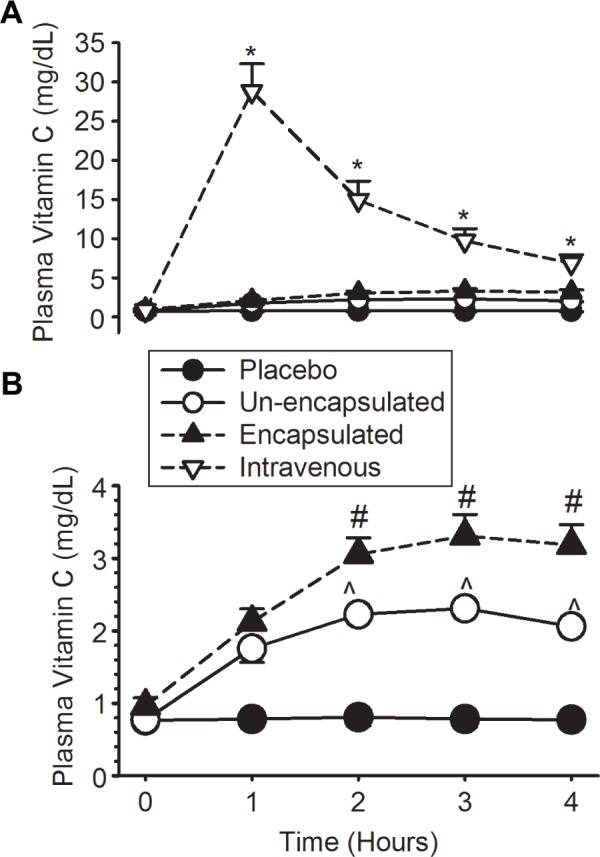
Plasma concentrations of vitamin C (ascorbic acid) before (time = 0 minute) and after: (1) oral administration of placebo, (2) oral administration of 4 g of vitamin C encapsulated in liposomes, (3) oral administration of 4 g of unencapsulated vitamin C, and (4) intravenous administration of 4 g of vitamin C. (A) All treatments. (B) All treatments excluding intravenous administration. Twenty minutes of forearm ischemia was initiated at three hours. *P < 0.001 vs all other treatments; #P < 0.001 vs unencapsulated oral and placebo; and ^P < 0.001 vs placebo. Data are mean ± SE (plasma vitamin C: 1 mg/dL = 56.78 μmol/L).
Lipid peroxidation
Baseline concentrations of plasma TBARS were not different between treatments, but they were somewhat variable. To better illustrate the influence of ischemia–reperfusion and/or vitamin C administration, these data have been presented as change in TBARS relative to baseline (Fig. 3). Forearm ischemia–reperfusion (20 minutes of occlusion) increased circulating TBARS 40 minutes postreperfusion (P < 0.03); this increase was prevented by all of the vitamin C treatments and was unaffected by mode of delivery.
Figure 3.
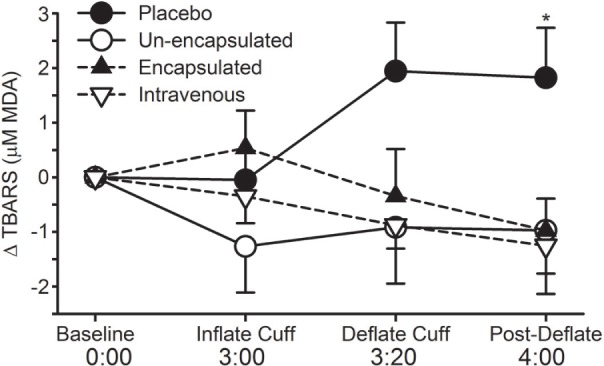
Change in circulating concentrations of TBARS from baseline (before) and after: (1) oral administration of placebo, (2) oral administration of 4 g of vitamin C encapsulated in liposomes, (3) oral administration of 4 g of unencapsulated vitamin C, and (4) intravenous administration of 4 g of vitamin C. Twenty minutes of forearm ischemia was initiated at three hours. *P < 0.046 vs all other treatments. Data are mean ± SE.
Discussion
The new findings of this investigation were that the oral delivery of vitamin C encapsulated in liposomes: (1) produced circulating concentrations of vitamin C greater than those elicited by oral delivery of unencapsulated vitamin C but less than those following intravenous vitamin C administration and (2) provided protection from ischemia–reperfusion that was similar to the protection provided by oral unencapsulated vitamin C and intravenous vitamin C administrations.
To our knowledge, there has been only one other published human study evaluating oral delivery of vitamin C encapsulated in liposomes, and this was a pilot study with only two research participants.23 Circulating concentrations of vitamin C following oral delivery of 5 g of vitamin C encapsulated in liposomes were compared with concentrations following 5 g of unencapsulated vitamin C. No discernable differences were detected between the plasma concentrations; however, in light of its status as a pilot study, and with only two research participants, this lack of difference could be attributed to insufficient statistical power, that is, a type 2 error.
While human studies of liposomal vitamin C may be lacking, the concept and utilization of liposomes for pharmaceutical delivery are well established.19,24–26 At the time of submission, there were at least 15 medications currently approved for liposomal delivery, with several hundred clinical trials currently underway.18 The cancer drug, doxorubicin, is one example of a reasonably well-known medication routinely delivered via liposomal encapsulation. Advantages of liposomal encapsulation include accelerated intestinal absorption, increased stability of the pharmaceutical, protection of the gut from potentially irritating agents, and greater bioavailability of the pharmaceutical.18
In the current investigation, we demonstrated greater bioavailability of vitamin C when delivered via liposomes compared with unencapsulated vitamin C. Blood is the primary transport medium of vitamin C, between the gut and the target tissues, thus circulating concentrations have long been accepted as a suitable expression of bioavailability.27 However, contingent on the dependent variable of interest and/or the specific role of vitamin C under investigation, in some instances, tissue/cellular concentrations may be more relevant than circulating concentrations. In light of the cost benefit and degree of invasiveness required for tissue sampling, we chose to analyze circulating concentrations.
To investigate a functional implication of enhanced vitamin C delivery/bioavailability, we quantified the magnitude of increase in circulating concentrations of biomarkers of oxidative stress following a forearm ischemia–reperfusion injury. Forearm ischemia–reperfusion injury has become an accepted model of oxidative stress-mediated damage, and several previous studies have examined the ability of antioxidant administration to attenuate increased oxidative stress following reperfusion.28–30 In the current study, forearm ischemia–reperfusion (20 minutes of occlusion) increased circulating TBARS 40 minutes postreperfusion; this increase was prevented by all of the vitamin C treatments and was unaffected by mode of delivery. While the protection provided by vitamin C was expected, we did not anticipate a similar degree of protection from all vitamin C treatments. The absence of difference in protection may, in part, be attributed to the magnitude of the vitamin C dose. A single (bolus) dose of 4 g of vitamin C is not trivial (approximately 40-fold greater than the minimum Recommended Dietary Allowance) and resulted in appreciably increased circulating concentrations of vitamin C (~3–30-fold) above baseline. The rationale for the 4 g dose was based on prior studies in which systemic doses ranging from 2 to 5 g were administered, and favorable outcomes reported pertinent to oxidative stress and/or physiological function.1,4,5,9,22 However, it may be that the exact dose required for protection from ischemia–reperfusion injury is less than 4 g. In the current study, a smaller dose of vitamin C may have produced discernable differences between modes of delivery. Future studies should incorporate consideration of a dose–response relationship.
We chose circulating TBARS as our expression of oxidative damage following ischemia–reperfusion. Recently, TBARS has been criticized for being a nonspecific marker of lipid peroxidation. We feel that TBARS was an appropriate outcome for the current study because: (1) the increase in TBARS is well correlated with the increase in isoprostanes, generally considered as a more specific marker of lipid peroxidation, during copper-mediated oxidative modification of low-density lipoprotein and peroxidation of docosahexaenoic acid31,32 and (2) TBARS proved to be of sufficient sensitivity to illustrate circulating responses to ischemia–reperfusion and an interaction between vitamin C and ischemia–reperfusion.
Noteworthy, in addition to its antioxidant properties, vitamin C has multiple other beneficial physiological effects. These include synthesis of catecholamines, formation of collagen, facilitation of iron absorption, and support with the processing of many hormones, enzymes, and amino acids.33–37 It is feasible that modes of delivery of vitamin C might influence one or more of these functions; however, detailed examination of these additional functions was beyond the scope of the current study.
In the current study, vitamin C was encapsulated in liposomes with a phospholipid bilayer composed of phosphatidylcholine. It is possible that the liposome itself, irrespective of its contents, may have some health benefits as phosphatidycholine has been proposed to attenuate dementia progression,38–40 facilitate structure and function of the endoplasmic reticulum,41 and play a protective role during myocardial disease development.42 Again, detailed examination of these additional functions/benefits was beyond the scope of the current study. Future studies should incorporate an empty liposome as a control/comparison treatment.
We have demonstrated that oral delivery of vitamin C encapsulated in liposomes promotes greater bioavailability than unencapsulated vitamin C, while avoiding the risks associated with intravenous administration. This observation has favorable implications for both scientific study and clinical use. From a research tool perspective, several studies have shown that the physiological benefits of intravenous vitamin C administration are not always reproduced with oral administration, on account of lower bioavailability.1,5 Oral administration of encapsulated vitamin C may abrogate this limitation. From a clinical perspective, older adults and adults who smoke may have a greater need for vitamin C than their younger, nonsmoking counterparts.27 Oral administration of encapsulated vitamin C may easily meet this need while decreasing the risk of gastrointestinal upset. Further, oxidative stress has been proposed as a contributing factor to delayed recovery from elective surgeries, such as knee arthroplasty43,44 and some cardiac procedures.45,46 Presurgery ingestion of encapsulated vitamin C may help alleviate/prevent oxidative stress-mediated damage and promote accelerated recovery.
In summary, we have demonstrated that oral delivery of vitamin C encapsulated in liposomes (1) produced circulating concentrations of vitamin C greater than those elicited by oral delivery of unencapsulated vitamin C but less than those following intravenous vitamin C administration and (2) provided protection from ischemia–reperfusion that was similar to the protection provided by oral unencapsulated vitamin C and intravenous vitamin C administration.
Acknowledgments
Plasma vitamin C concentrations were analyzed by Laboratory Corporation of America (LabCorp), Fort Collins, CO, USA.
Footnotes
ACADEMIC EDITOR: Joseph Zhou, Editor in Chief
PEER REVIEW: Four peer reviewers contributed to the peer review report. Reviewers’ reports totaled 717 words, excluding any confidential comments to the academic editor.
FUNDING: Empirical Labs, Fort Collins, CO, USA, provided financial support for this study. The authors confirm that the funder had no influence over the study design, content of the article, or selection of this journal.
COMPETING INTERESTS: EB is the owner of Valimenta, which produces and sells liposomal vitamin C. Nutritional Biomimetics LLC, also owned by EB, receives royalties from Empirical Labs for limited access to a trade secret manufacturing technology. EB has a provisional patent regarding liposomal dissolvable strips. Other authors disclose no potential conflicts of interest.
Paper subject to independent expert single-blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: JLD, RLS, EB, and CB. Collected and analyzed the data: JLD, HLP, JWB, SEB, GRG, RLS, MMS, EB, and CB. Wrote the first draft of the article: JLD and CB. Contributed to the writing of the article: JLD, HLP, JWB, SEB, GRG, RLS, MMS, EB, and CB. Agreed the article results and conclusions: JLD, HLP, JWB, SEB, GRG, RLS, MMS, EB, and CB. Jointly developed the structure and arguments for the article: JLD, EB, and CB. Made the critical revisions and approved the final version: JLD, HLP, JWB, SEB, GRG, RLS, MMS, EB, and CB. All authors reviewed and approved the final article.
REFERENCES
- 1.Bell C, Carson JM, Motte NW, Seals DR. Ascorbic acid does not affect the age-associated reduction in maximal cardiac output and oxygen consumption in healthy adults. J Appl Physiol. 2005;98(3):845–849. doi: 10.1152/japplphysiol.00790.2004. [DOI] [PubMed] [Google Scholar]
- 2.Bell C, Jones PP, Seals DR. Oxidative stress does not modulate metabolic rate or skeletal muscle sympathetic activity with primary aging in adult humans. J Clin Endocrinol Metab. 2003;88(10):4950–4954. doi: 10.1210/jc.2003-030454. [DOI] [PubMed] [Google Scholar]
- 3.Rossman MJ, Garten RS, Groot HJ, et al. Ascorbate infusion increases skeletal muscle fatigue resistance in patients with chronic obstructive pulmonary disease. Am J Physiol Regul Integr Comp Physiol. 2013;305(10):R1163–R1170. doi: 10.1152/ajpregu.00360.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monahan KD, Eskurza I, Seals DR. Ascorbic acid increases cardiovagal baroreflex sensitivity in healthy older men. Am J Physiol Heart Circ Physiol. 2004;286(6):H2113–H2117. doi: 10.1152/ajpheart.01054.2003. [DOI] [PubMed] [Google Scholar]
- 5.Eskurza I, Monahan KD, Robinson JA, Seals DR. Effect of acute and chronic ascorbic acid on flow-mediated dilatation with sedentary and physically active human ageing. J Physiol. 2004;556(pt 1):315–324. doi: 10.1113/jphysiol.2003.057042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirashima O, Kawano H, Motoyama T, et al. Improvement of endothelial function and insulin sensitivity with vitamin C in patients with coronary spastic angina: possible role of reactive oxygen species. J Am Coll Cardiol. 2000;35(7):1860–1866. doi: 10.1016/s0735-1097(00)00616-1. [DOI] [PubMed] [Google Scholar]
- 7.Ling L, Zhao SP, Gao M, Zhou QC, Li YL, Xia B. Vitamin C preserves endothelial function in patients with coronary heart disease after a high-fat meal. Clin Cardiol. 2002;25(5):219–224. doi: 10.1002/clc.4950250505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taddei S, Virdis A, Ghiadoni L, Magagna A, Salvetti A. Vitamin C improves endothelium-dependent vasodilation by restoring nitric oxide activity in essential hypertension. Circulation. 1998;97(22):2222–2229. doi: 10.1161/01.cir.97.22.2222. [DOI] [PubMed] [Google Scholar]
- 9.Bell C, Stob NR, Seals DR. Thermogenic responsiveness to {beta}-adrenergic stimulation is augmented in exercising vs. sedentary adults: role of oxidative stress. J Physiol. 2006;570(3):629–653. doi: 10.1113/jphysiol.2005.098756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mak S, Newton GE. Vitamin C augments the inotropic response to dobutamine in humans with normal left ventricular function. Circulation. 2001;103(6):826–830. doi: 10.1161/01.cir.103.6.826. [DOI] [PubMed] [Google Scholar]
- 11.Sartor Z, Kesey J, Dissanaike S. The effects of intravenous vitamin C on point-of-care glucose monitoring. J Burn Care Res. 2015;36(1):50–56. doi: 10.1097/BCR.0000000000000142. [DOI] [PubMed] [Google Scholar]
- 12.Lipka D, Gubernator J, Filipczak N, et al. Vitamin C-driven epirubicin loading into liposomes. Int J Nanomedicine. 2013;8:3573–3585. doi: 10.2147/IJN.S47745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Padayatty SJ, Sun H, Wang Y, et al. Vitamin C pharmacokinetics: implications for oral and intravenous use. Ann Intern Med. 2004;140(7):533–537. doi: 10.7326/0003-4819-140-7-200404060-00010. [DOI] [PubMed] [Google Scholar]
- 14.Levine M, Padayatty SJ, Espey MG, Vitamin C. a concentration-function approach yields pharmacology and therapeutic discoveries. Adv Nutr. 2011;2(2):78–88. doi: 10.3945/an.110.000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levine M, Rumsey SC, Daruwala R, Park JB, Wang Y. Criteria and recommendations for vitamin C intake. JAMA. 1999;281(15):1415–1423. doi: 10.1001/jama.281.15.1415. [DOI] [PubMed] [Google Scholar]
- 16.Wang Y, Mackenzie B, Tsukaguchi H, Weremowicz S, Morton CC, Hediger MA. Human vitamin C (L-ascorbic acid) transporter SVCT1. Biochem Biophys Res Commun. 2000;267(2):488–494. doi: 10.1006/bbrc.1999.1929. [DOI] [PubMed] [Google Scholar]
- 17.Munoz-Montesino C, Roa FJ, Pena E, et al. Mitochondrial ascorbic acid transport is mediated by a low-affinity form of the sodium-coupled ascorbic acid transporter-2. Free Radic Biol Med. 2014;70:241–254. doi: 10.1016/j.freeradbiomed.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 18.Kraft JC, Freeling JP, Wang Z, Ho RJ. Emerging research and clinical development trends of liposome and lipid nanoparticle drug delivery systems. J Pharm Sci. 2014;103(1):29–52. doi: 10.1002/jps.23773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rogers JA, Anderson KE. The potential of liposomes in oral drug delivery. Crit Rev Ther Drug Carrier Syst. 1998;15(5):421–480. [PubMed] [Google Scholar]
- 20.Silver AE, Beske SD, Christou DD, et al. Overweight and obese humans demonstrate increased vascular endothelial NAD(P)H oxidase-p47(phox) expression and evidence of endothelial oxidative stress. Circulation. 2007;115(5):627–637. doi: 10.1161/CIRCULATIONAHA.106.657486. [DOI] [PubMed] [Google Scholar]
- 21.Stefanovic A, Kotur-Stevuljevic J, Spasic S, Bogavac-Stanojevic N, Bujisic N. The influence of obesity on the oxidative stress status and the concentration of leptin in type 2 diabetes mellitus patients. Diabetes Res Clin Pract. 2007;79(1):156–163. doi: 10.1016/j.diabres.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 22.Newsom SA, Paxton RJ, Rynn GM, Bell C. Influence of ascorbic acid on the thermic effect of feeding in overweight and obese adult humans. Obesity (Silver Spring) 2008;16(8):1749–1754. doi: 10.1038/oby.2008.304. [DOI] [PubMed] [Google Scholar]
- 23.Hickey S, Roberts HJ, Miller NJ. Pharmacokinetics of oral vitamin C. J Nutr Environ Med. 2008;17(3):169–177. [Google Scholar]
- 24.Woodley JF. Liposomes for oral administration of drugs. Crit Rev Ther Drug Carrier Syst. 1985;2(1):1–18. [PubMed] [Google Scholar]
- 25.Allen TM, Cullis PR. Liposomal drug delivery systems: from concept to clinical applications. Adv Drug Deliv Rev. 2013;65(1):36–48. doi: 10.1016/j.addr.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 26.Bangham AD, Standish MM, Watkins JC. Diffusion of univalent ions across the lamellae of swollen phospholipids. J Mol Biol. 1965;13(1):238–252. doi: 10.1016/s0022-2836(65)80093-6. [DOI] [PubMed] [Google Scholar]
- 27.Brubacher D, Moser U, Jordan P. Vitamin C concentrations in plasma as a function of intake: a meta-analysis. Int J Vitam Nutr Res. 2000;70(5):226–237. doi: 10.1024/0300-9831.70.5.226. [DOI] [PubMed] [Google Scholar]
- 28.Devan AE, Umpierre D, Harrison ML, et al. Endothelial ischemia–reperfusion injury in humans: association with age and habitual exercise. Am J Physiol Heart Circ Physiol. 2011;300(3):H813–H819. doi: 10.1152/ajpheart.00845.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Traustadottir T, Davies SS, Stock AA, et al. Tart cherry juice decreases oxidative stress in healthy older men and women. J Nutr. 2009;139(10):1896–1900. doi: 10.3945/jn.109.111716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pleiner J, Schaller G, Mittermayer F, et al. Intra-arterial vitamin C prevents endothelial dysfunction caused by ischemia–reperfusion. Atherosclerosis. 2008;197(1):383–391. doi: 10.1016/j.atherosclerosis.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 31.Gopaul NK, Nourooz-Zadeh J, Mallet AI, Anggard EE. Formation of PGF2-isoprostanes during the oxidative modification of low density lipoprotein. Biochem Biophys Res Commun. 1994;200(1):338–343. doi: 10.1006/bbrc.1994.1453. [DOI] [PubMed] [Google Scholar]
- 32.Nourooz-Zadeh J, Liu EH, Anggard E, Halliwell B. F4-isoprostanes: a novel class of prostanoids formed during peroxidation of docosahexaenoic acid (DHA) Biochem Biophys Res Commun. 1998;242(2):338–344. doi: 10.1006/bbrc.1997.7883. [DOI] [PubMed] [Google Scholar]
- 33.Gershoff SN, Vitamin C. (ascorbic acid): new roles, new requirements? Nutr Rev. 1993;51(11):313–326. doi: 10.1111/j.1753-4887.1993.tb03757.x. [DOI] [PubMed] [Google Scholar]
- 34.Weber P, Bendich A, Schalch W. Vitamin C and human health—a review of recent data relevant to human requirements. Int J Vitam Nutr Res. 1996;66(1):19–30. [PubMed] [Google Scholar]
- 35.Bendich A, Langseth L. The health effects of vitamin C supplementation: a review. J Am Coll Nutr. 1995;14(2):124–136. doi: 10.1080/07315724.1995.10718484. [DOI] [PubMed] [Google Scholar]
- 36.Lane DJ, Richardson DR. The active role of vitamin C in mammalian iron metabolism: much more than just enhanced iron absorption! Free Radic Biol Med. 2014;75:69–83. doi: 10.1016/j.freeradbiomed.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 37.Camarena V, Wang G. The epigenetic role of vitamin C in health and disease. Cell Mol Life Sci. 2016;73(8):1645–1658. doi: 10.1007/s00018-016-2145-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgins JP, Flicker L. Lecithin for dementia and cognitive impairment. Cochrane Database Syst Rev. 2003;3:CD001015. doi: 10.1002/14651858.CD001015. [DOI] [PubMed] [Google Scholar]
- 39.Chung SY, Moriyama T, Uezu E, et al. Administration of phosphatidylcholine increases brain acetylcholine concentration and improves memory in mice with dementia. J Nutr. 1995;125(6):1484–1489. doi: 10.1093/jn/125.6.1484. [DOI] [PubMed] [Google Scholar]
- 40.Hung MC, Shibasaki K, Yoshida R, Sato M, Imaizumi K. Learning behaviour and cerebral protein kinase C, antioxidant status, lipid composition in senescence-accelerated mouse: influence of a phosphatidylcholine-vitamin B12 diet. Br J Nutr. 2001;86(2):163–171. doi: 10.1079/bjn2001391. [DOI] [PubMed] [Google Scholar]
- 41.Lagace TA, Ridgway ND. The role of phospholipids in the biological activity and structure of the endoplasmic reticulum. Biochim Biophys Acta. 2013;1833(11):2499–2510. doi: 10.1016/j.bbamcr.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 42.Tappia PS, Dent MR, Dhalla NS. Oxidative stress and redox regulation of phospholipase D in myocardial disease. Free Radic Biol Med. 2006;41(3):349–361. doi: 10.1016/j.freeradbiomed.2006.03.025. [DOI] [PubMed] [Google Scholar]
- 43.Garcia-de-la-Asuncion J, Perez-Solaz A, Carrau M, Belda FJ, Perez-Griera J, Garriges B. Different oxidative stress marker levels in blood from the operated knee or the antecubital vein in patients undergoing knee surgery: a tourniquet-induced ischemia–reperfusion model. Redox Rep. 2012;17(5):194–199. doi: 10.1179/1351000212Y.0000000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hocker AD, Boileau RM, Lantz BA, Jewett BA, Gilbert JS, Dreyer HC. Endoplasmic reticulum stress activation during total knee arthroplasty. Physiol Rep. 2013;1(3):e00052. doi: 10.1002/phy2.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stanger O, Aigner I, Schimetta W, Wonisch W. Antioxidant supplementation attenuates oxidative stress in patients undergoing coronary artery bypass graft surgery. Tohoku J Exp Med. 2014;232(2):145–154. doi: 10.1620/tjem.232.145. [DOI] [PubMed] [Google Scholar]
- 46.Wang ZJ, Hu WK, Liu YY, et al. The effect of intravenous vitamin C infusion on periprocedural myocardial injury for patients undergoing elective percutaneous coronary intervention. Can J Cardiol. 2014;30(1):96–101. doi: 10.1016/j.cjca.2013.08.018. [DOI] [PubMed] [Google Scholar]