Abstract
Several studies have shown the existence of an obesity paradox after Percutaneous Coronary Intervention (PCI). However, other studies have shown its absence. This study sought to perform a systematic review and meta-analysis of studies comparing the mortality risk between high body mass index patients and normal weight patients after PCI.
We have searched PubMed, Embase, and Chinese medical journal for randomized controlled trials (RCTs) and observational studies published between the year 2000 and 2015 by typing the keywords “percutaneous coronary intervention” and “obesity paradox.” The main outcome was “all-cause mortality”. RevMan 5.3 software was used to calculate the risk ratio (RR) with 95% confidence interval (CI) to express the pooled effect on discontinuous variables.
Twenty-two studies have been included in this meta-analysis consisting of a total of 242,377 patients with 73,143 normal weight patients, 103,608 overweight, and 65,626 obese patients. Younger age, higher cardiovascular risk factors and the intensive use of medications have mainly been observed among obese patients followed by overweight and normal weight patients respectively. In-hospital, 12 months and ≥ 1 year (long-term) mortality risks were significantly lower in the overweight and obese groups with (RR: 0.67; 95% CI: 0.63–0.72, P < 0.00001) and (RR: 0.60; 95% CI: 0.56–0.65, P < 0.00001) respectively in the in-hospital follow-up (RR: 0.62; 95% CI: 0.55–0.71 and 0.57; 95% CI: 0.52–0.63, P < 0.00001) at 12 months, and (RR: 0.70; 95% CI: 0.64–0.76; P < 0.00001) and (RR: 0.80; 95% CI: 0.71–0.91, P = 0.0006) respectively for the long-term follow-up after PCI.
This “obesity paradox” does exist after PCI. The mortality in overweight and obese patients is really significantly lower compared to the normal weight patients. However, the exact reasons for this phenomenon need further exploration and research in the future.
INTRODUCTION
Nowadays, in a world where fast food has taken a huge position in people's lifestyle, where tasty and unhealthy food is becoming a priority, and where exercise and physical activities have been restricted due to limited free times, obesity is increasing at a faster rate.1–2 People are becoming overweight and obese at a younger age and these people are commonly exposed to several cardiovascular risk factors such as hypertension, Diabetes Mellitus (DM), smoking, and hyperlipidemia.3 Most of these people suffer from coronary artery diseases (CAD) which can, in a more advanced stage, result in acute coronary syndrome.4 In most cases, percutaneous coronary intervention (PCI) is the choice of treatment for these patients. These high body mass index (BMI) patients are considered to be at high risk for cardiovascular disorders and hence, several precautions and care have to be taken in their management and treatment, both in the hospital and during the post-discharge period compared to normal weight patients with similar conditions.5
Several researches have been carried out and surprisingly, many have shown that after cardiac interventions, the in-hospital and long-term (≥ 1 year) mortality risks in these high BMI patients are lower compared to normal weight patients. Hence, a specific term called the “obesity paradox” has been reserved for this unexpected condition.6 Many studies have supported the fact of the existence of this phenomenon. For example, the article published by Lancefield et al in 2010 showed that compared to normal weight patients, overweight and obese patients had a lower in-hospital and 1 year mortality rate after PCI.7
However, the existence of this “obesity paradox” is still not so clear. The results and conclusion from a meta-analysis published by Oreopoulos et al in 2008 were still not so clear about the presence of this phenomenon after coronary revascularization.8 Several studies have also shown the absence of such a phenomenon after PCI. For example, the article published by Akin et al in 2012 challenged this phenomenon by revealing no evidence of this “obesity paradox” and stated that it may in fact not exist at all.9
In recent years, many newer Randomized Controlled Trials (RCTs) and observational studies comparing the mortality rate in overweight and obese patients with that of normal weight patients after PCI have been published. Therefore, by combining previous researches with new ones (from year 2000 to 2015), we aim to perform a meta-analysis to show whether this “obesity paradox” exists or not.
METHODS
Data Sources and Searches
We have searched PubMed, Embase, and Chinese medical journal for RCTs and observational studies by typing the words “obesity paradox and percutaneous coronary intervention,” and also replacing the word “obesity paradox” by the word “obesity,” “overweight” or, “high BMI.” To further enhance this search, the term “mortality” has also been used. No language restriction was applied.
STUDY SELECTION
Inclusion and Exclusion Criteria
RCTs and observational studies were included if:
They consisted of overweight, obese, and normal weight patients, (b) they reported mortality after cardiac interventions, (c) they were published between the year 2000 and 2015.
RCTs and observational studies were excluded if:
They did not include overweight and/or obese patients together with normal weight patients, (b) they did not compare normal weight patients with overweight and/or obese ones, (c) mortality rate was not among the reported clinical end points, (d) only their abstracts were made available.
DEFINITIONS
According to the World Health Organization and National Heart, Lung, and Blood Institute, the patient population was divided into
-Normal weight patients with a BMI of 18.5 to 24.9 kg/m2
-Overweight patients with a BMI of 25.0 to 29.9 kg/m2
-Obese patients with a BMI of > 30 kg/m210
- High BMI patients included both overweight and obese patients.
- Mortality included both cardiac and noncardiac deaths; that is, all-cause death. All-cause death was assumed in studies where “death” had not well been classified or defined.
-In hospital mortality was defined as death within the period of stay in the hospital after cardiac interventions.
- Mortality during a follow-up period of 12 months described the number of death from the period after hospital discharge until 12 months. Mortality at 12 months was considered in the long-term category.
-Long-term mortality was defined as death at 1 year or more after cardiac interventions.
Data Extraction and Quality Assessment
The authors PKB and NL independently checked all the data and then the eligibility and methodological quality of each eligible study were assessed carefully. Several information have been retrieved, and information regarding those included studies and the characteristics/features of the patients involved, intervention strategies, and the corresponding clinical outcomes reported in these studies were systematically extracted. The follow-up periods have also been carefully classified or separated into in-hospital mortality, mortality during a 12-month period and long-term mortality. Any disagreement raised during this data extraction and quality assessment has been carefully discussed between these 2 authors, and if they could not reach a decision, it was discussed and resolved by the third author (MHC). Assessment of the bias risks within the studies were conducted with the components recommended by the Cochrane Collaboration.11
OUTCOME
In-hospital mortality, mortality during a 12 months follow-up period and, long-term (≥1 year) mortality were considered as the main outcomes for this study.
Methodological and Data Analyses
Recommendations of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement have been used during the study selection, data collection, data analysis, and, reporting of the results. The assessment of heterogeneity across the studies was performed using the (a) Cochrane Q-statistic whereby a “P value” <0.05 was considered statistically significant and, (b) Cochrane I2-statistic which represented the percentage of the total variation across studies that is due to heterogeneity rather than chance whereby an I2 value of 0% indicated no heterogeneity, and an increased heterogeneity was indicated by a larger value. If I2 was < 50%, a fixed effect was used. However, if I2 was >50%, a random effect has been used. Funnel plots were assessed for publication bias. We calculated weighted risk ratios (RR) and 95% confidence intervals (CIs) for categorical variables. The pooled analyses were performed with RevMan 5.3 software. Ethical approval was not necessary as this study is a Systematic Review and Meta-Analysis.
RESULTS
Study and Patients Characteristics
Based upon titles and abstracts, we have identified 3564 publications from PubMed, Embase, and Chinese medical journal. After excluding the duplicates, 2522 articles were remaining. A total of 2400 publications have been eliminated since they were irrelevant to our topic. However, 122 full-text articles were assessed for eligibility. Another 100 articles were eliminated because they were either meta-analyses, case reports, or letters to the editor, data for the control/normal weight patients were not available, mortality was not among the reported outcomes or discontinuous data were not available. Finally, 22 articles that satisfied our inclusion criteria were selected for this meta-analysis. The study selection including the flow of the process for identifying potentially eligible trials and the reasons for inclusion and exclusion has been represented in Figure 1.
FIGURE 1.
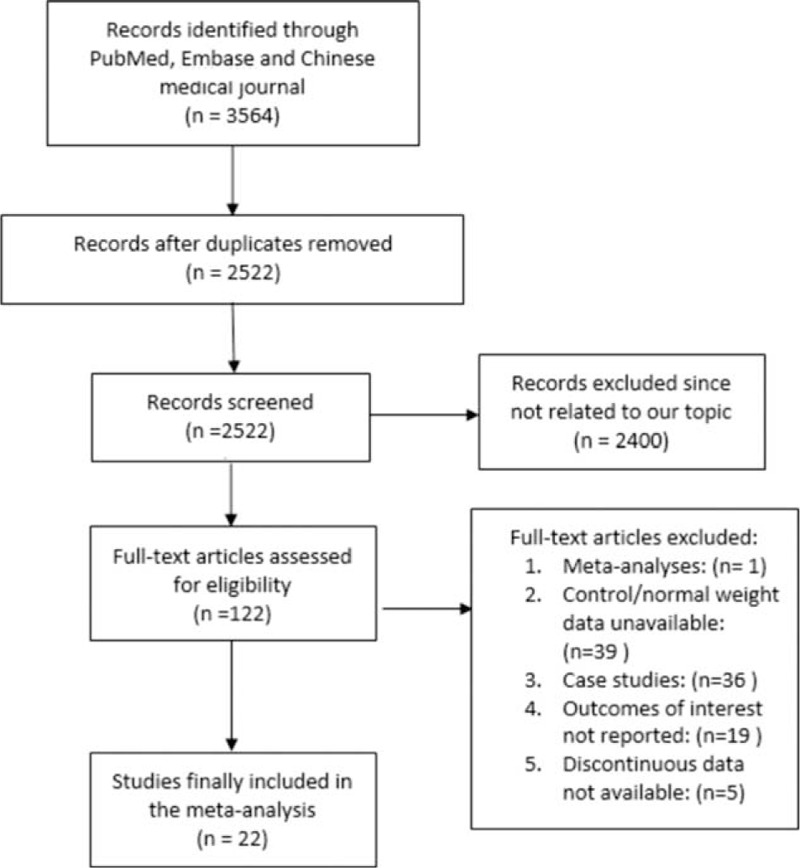
The flow diagram of the study selection. The study selection including the flow of the process for identifying potentially eligible trials and the reasons for inclusion and exclusion has been represented. We have followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement for our study. From 3564 articles, 122 full-text articles were assessed eligible for this meta-analysis. After strictly considering the inclusion and exclusion criteria, 22 articles were finally selected for this systematic review and meta-analysis. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
The characteristics of the 22 studies that met the eligibility criteria are displayed in Tables 1 and 2. Table 1 shows the baseline features and Table 2 shows the criteria for the inclusion and exclusion of patients in these 22 studies. Table 2 also shows the reported outcomes and follow-up periods of each study. This meta-analysis consists of a total of 242,377 patients with 73,143 normal weight patients, 103,608 overweight, and 65,626 obese patients.
TABLE 1.
Baseline Characteristics of Patients from the Included Studies
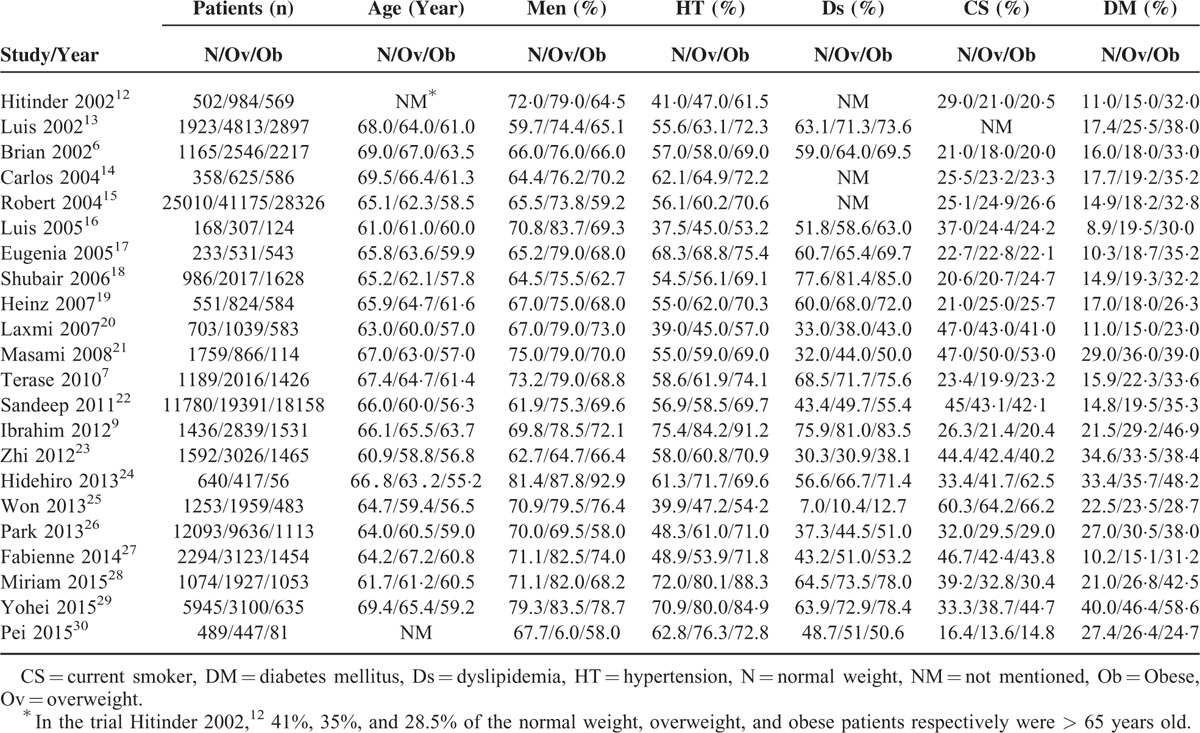
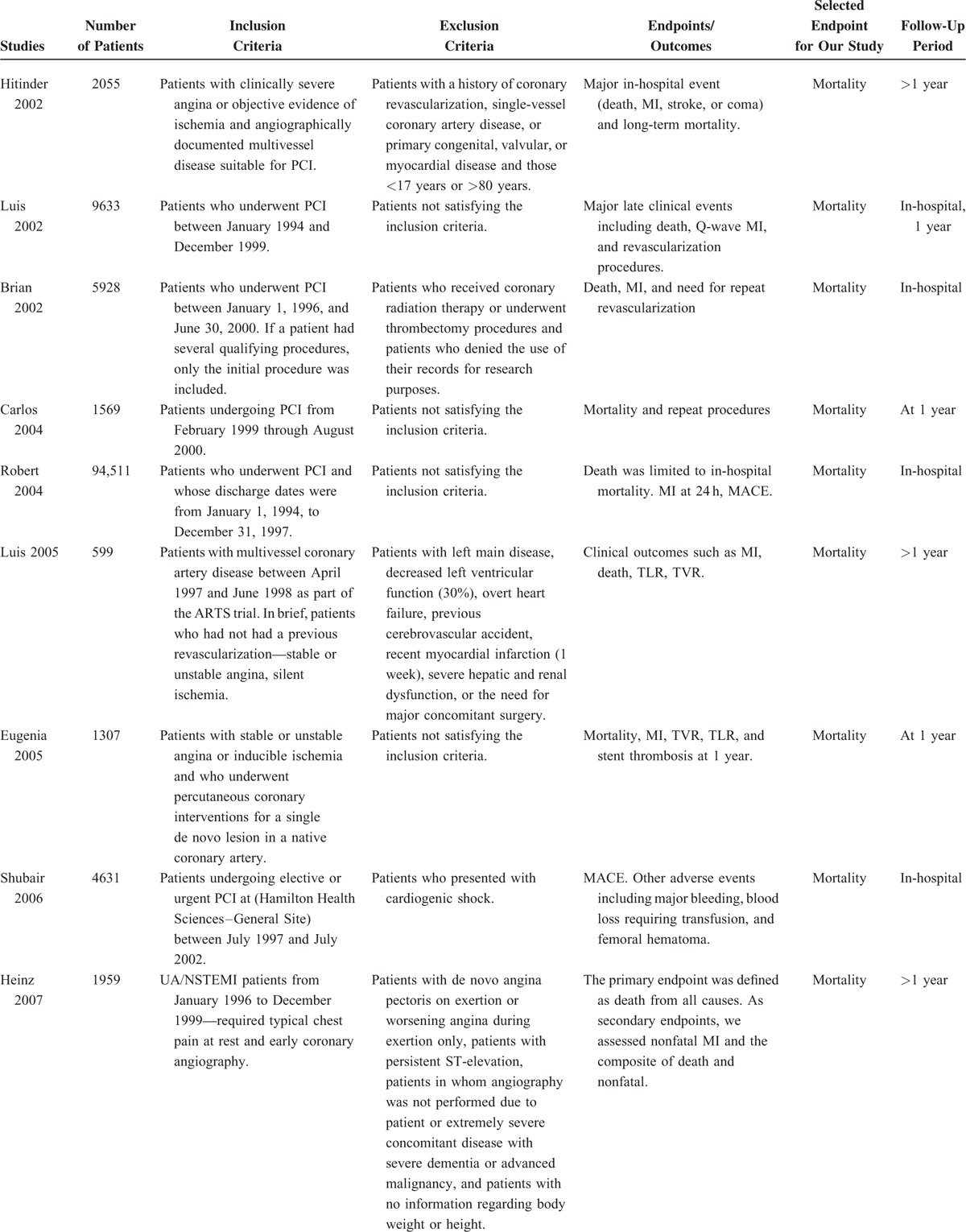
TABLE 2.
The Inclusion and Exclusion Criteria, Total Participants, and Follow-Up Period of Each Study Included in Our Meta-Analysis
Two studies, Minutello (2004) 15 and Das (2012),22 consisted of the highest population of overweight and obese patients among all of the trials with a total of 69,501 and 37,549 patients respectively. Obese patients were the youngest among all the other categories of patients in all of the studies. Moreover, male patients were higher in all of the studies as compared to female patients. One study (Ibrahim 2012) had the highest number of hypertensive obese patients (91.2%).9 Most of the obese patients suffered from diabetes mellitus. The baseline features of the included studies have been represented in Table 1.
The inclusion and exclusion criteria, total number of participants, and follow-up period of each study included in our meta-analysis have been shown in Table 2 .
Total number of patients has been calculated as the normal weight + overweight + obese patients.
The follow-up period was during the stay in hospital (in-hospital follow-up), follow-up during a 12 months period, and a long-term follow-up of ≥ 1 year. Hitinder2002,12 Luis2005,16 Zhi2012,23 Heinz2007,19 and Miriam2015 28 had a follow-up period of 3 and 5 years, 3 years, 3 years, 17 months, and 12 years respectively.
Several outcomes have been reported in these studies. However, since our meta-analysis is concerned with the mortality rate, we have only used data reporting mortality.
Risk Factors Among the Different Groups of Patients
Age, hypertension, dyslipidemia, smoking, DM, and male gender act as risk factors for cardiovascular diseases. Overweight and obese patients are at higher risk of exposure to these cardiovascular risk factors.
The detailed risk factors reported in these patients have been shown in Table 3.
TABLE 2 (Continued).
The Inclusion and Exclusion Criteria, Total Participants, and Follow-Up Period of Each Study Included in Our Meta-Analysis
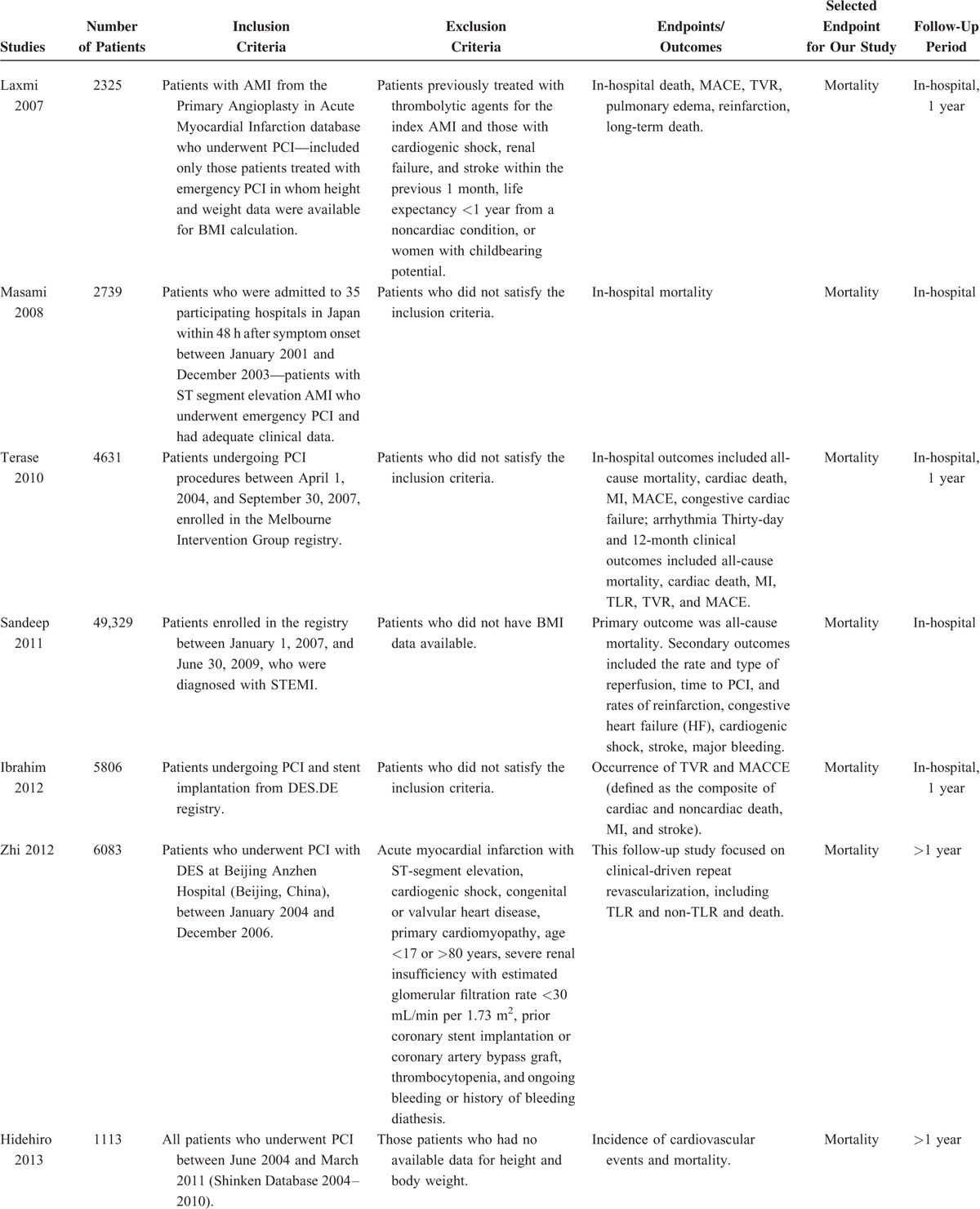
TABLE 3.
The Mean Values for the Risk Factors for Cardiovascular Diseases
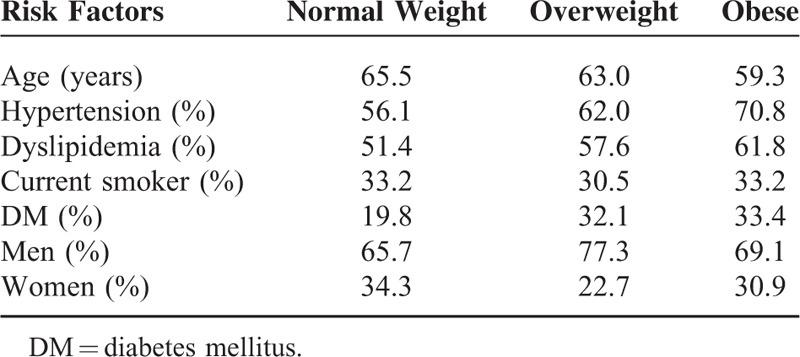
In this meta-analysis, obese patients were youngest with an average age of 59.3 years whereas the normal weight patients were the eldest with an average age of 65.5 years. Hypertension and dyslipidemia also mainly affected the obese patients with a mean percentage of 70.8 and 61.8 respectively whereas the mean percentages of these same 2 risk factors in the normal weight patients were 56.1 and 51.4 respectively. Of the obese and normal weight patients 33.2% were current smokers. The percentage of obese patients suffering from DM was also the highest with a mean value of 33.4. 65.7% of the normal weight patients, 77.3% of the overweight patients, and 69.1% of the obese patients were males. If considered as a whole, younger age and a higher rate of certain cardiovascular risk factors were observed among the overweight and obese patients. However, there was no significant difference in the percentage of patients who smoke, among all the 3 groups. No significant differences in the risk factors between the overweight and the obese patients have been observed. The detailed risk factors and their corresponding percentages among the different groups of patients have been mentioned in Table 3.
Medications at Discharge and During the Follow-Up Period
Data from study Sandeep 2011,22 Won 2010,25 Hidehiro 2013,24 Ibrahim 2012 9, Pei 2015,30 Yohei 2015,29 Zhi 2012,23 Heinz 2007 19 and, Shubair 2006 18 have been used to calculate the percentage of patients with their corresponding medications during the follow-up period and have been represented in Table 4. Studies that have not been included in this section have been ignored because they did not report the medications being prescribed at hospital discharge or during the follow-up period.
TABLE 2 (Continued).
The Inclusion and Exclusion Criteria, Total Participants, and Follow-Up Period of Each Study Included in Our Meta-Analysis
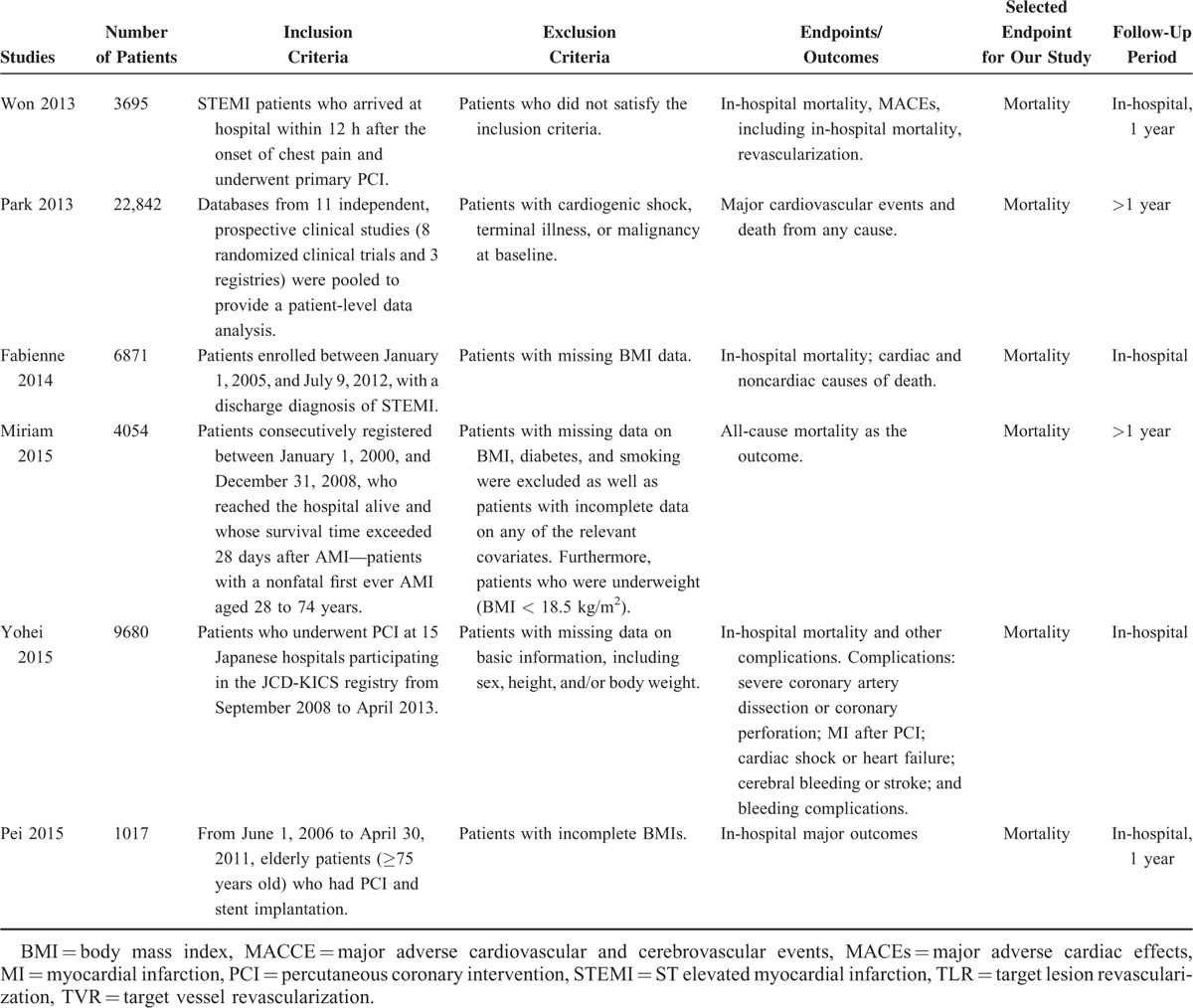
TABLE 4.
The Medications at Discharge and During Follow-Up Used by the Patients Within the Different BMI Groups
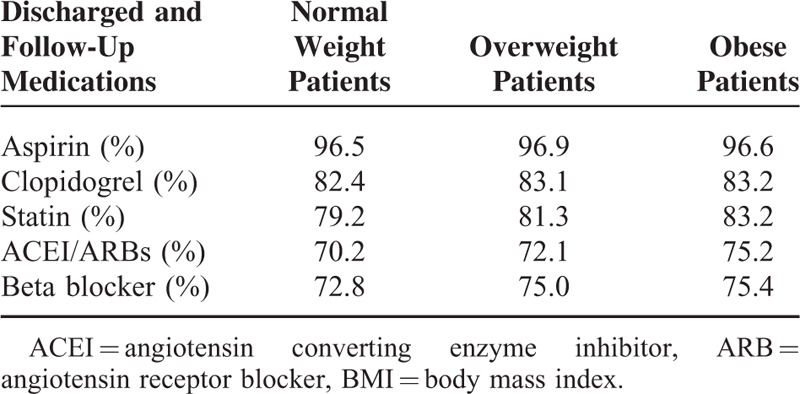
According to Table 4, 96.5% of normal weight patients, 96.9% of the overweight patients, and 96.6% of the obese patients used Aspirin. Medication use was higher among the overweight and highest among the obese patients. Overweight patients used more medications than normal weight patients whereas obese patients used more medications than overweight patients after PCI. Table 4 summarizes the percentage of patients on medications at discharge and during the follow-up period.
Main Results of the Meta-Analysis
The in-hospital mortality in these high BMI patients has been represented in Figure 2. There was evidence of a statistically significantly lower heterogeneity across the included studies. A low heterogeneity among the different subgroups has been observed during the in-hospital and long-term follow-up periods. According to this result, it can clearly be seen that the in-hospital mortality is significantly lower in overweight and obese groups (RR: 0.67; 95% CI: 0.63–0.72 and 0.60; 95% CI: 0.56–0.65, P < 0.00001) respectively as compared to the normal weight patients after PCI.
FIGURE 2.
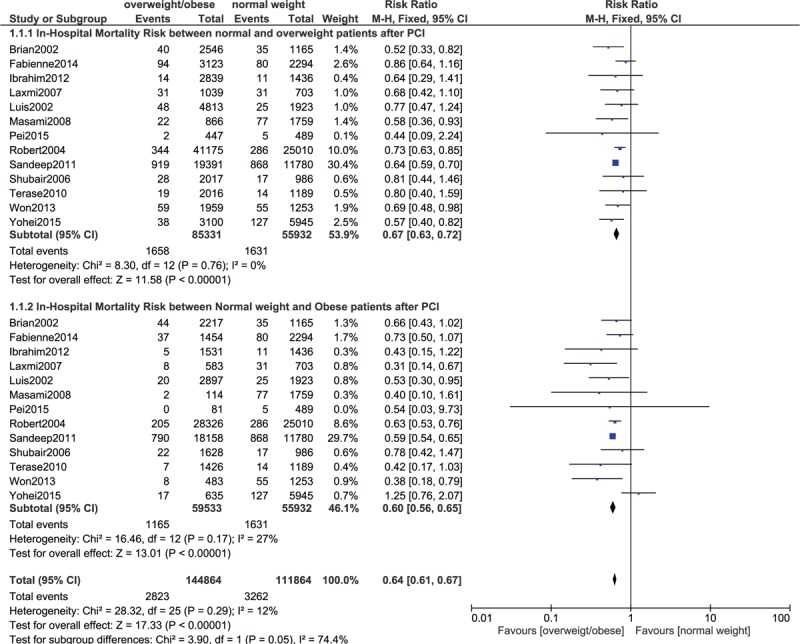
The in-hospital mortality risk among overweight and obese patients as compared to normal weight patients after percutaneous coronary intervention.
The 12 months follow-up for mortality in these high BMI groups has been represented in Figure 3. The result is in favor of the overweight and obese groups where the 1-year follow-up for mortality is significantly lower (RR: 0.62; 95% CI: 0.55–0·71 and 0.57; 95% CI: 0.52–0.63, P < 0.00001) respectively as compared to the normal weight patients after PCI.
FIGURE 3.
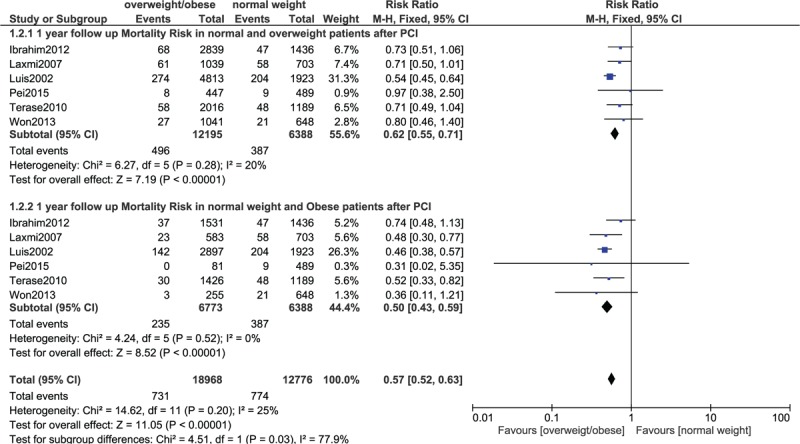
The 12 months follow-up for mortality risk among overweight and obese patients as compared to normal weight patients after percutaneous coronary intervention.
The long-term (≥ 1 year) mortality in these high BMI patients has been represented in Figure 4. Data from the result shows that the long-term mortality in the overweight and obese patients are still significantly lower (RR: 0.70; 95% CI: 0.64–0.76, P < 0.00001 and RR: 0.80; 95% CI: 0.71–0.91, P = 0.0006) respectively.
FIGURE 4.
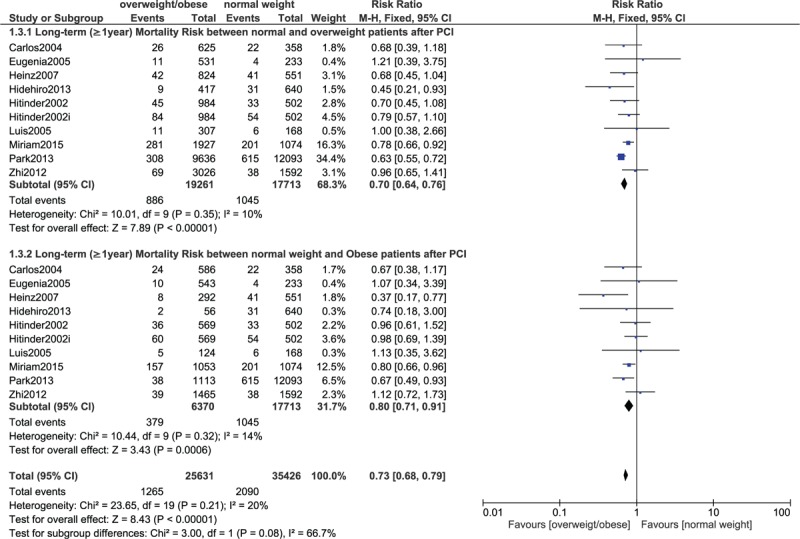
The long-term (≥1 year) mortality risk among overweight and obese patients as compared to normal weight patients after cardiovascular intervention.
DISCUSSION
We all know that high BMI patients have an increased risk of suffering from cardiovascular diseases.31–32 A large number of these patients are exposed to cardiovascular risk factors such as hypertension, DM, and hyperlipidemia as shown in this study too. Normally, these high BMI patients should have worse in-hospital and long-term adverse clinical outcomes after PCI. However, several studies have shown that overweight and obese patients have a lower in-hospital and long-term mortality rate as compared to normal weight patients after cardiac intervention.6–7
Similarly, results from our meta-analysis showed that the in-hospital and long-term (≥ 1 year) mortality in overweight and obese patients were significantly lower than that compared to the normal weight patients. The mortality in normal weight patients after PCI was significantly higher compared to that of the other 2 categories of patients confirming that the “obesity paradox” does exist after PCI.
Certain studies have mentioned that obesity paradox could be associated with several biases. For example, if the disease was diagnosed earlier, it could have been confused with prolonged or increased survival of the patient. This could give rise to a lead time bias. On the contrary, a lower pretest probability has been commonly observed among the lean or underweight individuals, and consequently, these people tend to have a more advanced disease, which could finally lead to a worse prognosis in these low BMI patients. Also, a publication bias which occurs when more positive studies are likely to be published compared to negative studies, and a confounding bias may also potentially exist.33 However, several recent meta-analyses have really shown the existence of an obesity paradox which could be associated to other reasons.
The suggested reasons mentioned in other studies, behind this “obesity paradox,” are still not so clear. Many hypotheses have been considered for this unexpected result. First of all, younger age could be one of the main factors contributing to this phenomenon. Even our study has shown that younger age was most obvious in the obese group followed by the overweight group.20,34 Younger patients have a stronger body function and still have the power to tolerate and fight serious health conditions and compensate to correct any abnormal condition affecting the body. As shown in our result, the obese patients had a mean age of 59.3 years while in normal weight patients, the mean age was 65.5 years. The recovering capability of older patients from cardiac complications, and their body's ability to compensate during disease condition is weak. Accompanied by co-morbidities, which render their immune system weaker could also be among the reasons for the in-hospital and long-term (≥ 1 year) mortality risks to be lower among these younger overweight and obese patients. Life-long and intensive medication use from an early age and for a longer period of time could be another reason responsible for this “obesity paradox.”7,35–38 As shown in our results, overweight and obese patients used more medications as compared to normal weight patients.
These patients are at a higher risk of cardiovascular diseases, and most of them are diabetics, or suffer from hypertension and dyslipidemia in their early 40s. They are treated for these conditions at an earlier age and they use several medications daily to control their high blood pressure and hyperglycemia. Sometimes, medications such as statin and aspirin are given to them as a measure of prevention and they are advised very often about regular exercise and healthy habits to keep them fit. Very few normal weight patients go through similar conditions and hence they even have less chance of being taught about these important health tips as compared to high BMI individuals.7 Being younger, obese patients may have received more aggressive or attentive care compared to underweight or normal weight patients. However, older patients, with a majority in the normal BMI group, may not have fared as well with the treatments provided and unfortunately showing a higher rate of mortality in the normal BMI category compared to the overweight and obese patients. Interestingly, studies have also shown that diabetic or nondiabetic overweight and obese patients on statin prior to acute coronary syndrome during their hospital stay and post discharged period, appeared to have a significant survival benefit.
Cessation of smoking, cardiac rehabilitation, and counseling about diet or healthy food consumption are more frequently enforced in overweight and obese patients than in normal weight patients.32 These could be among other reasons responsible for this “obesity paradox.”
Moreover, obese patients have a good storage for nutrients which is often required after surgery. This lack of nutrient could be another reason why the mortality rate is higher in normal weight patients after cardiac intervention. Furthermore, patients with a low BMI tend to be affected more by noncardiac mortality due to conditions such as cancer, smoking, chronic obstructive pulmonary disease, and insulin-dependent DM. These comorbidities have been suggested as a possible explanation for this “obesity paradox” too.
Size of the coronary blood vessels could also be considered as a reason to explain this “obesity paradox.” A study suggested that the size of the coronary arteries increases with increasing BMI. The study has observed a lower mortality rate among the overweight and obese patients because of their large coronary blood vessels. Underweight patients had the smallest coronary arteries and the highest in-hospital and long-term mortality rates were observed among this category of patients.7
Platelets seem to play a major role in the pathophysiology of acute coronary syndromes, as well as the outcome after PCI with stent implantation. Adverse conditions such as stent thrombosis can occur due to platelet dysfunction. Sudden death can also be induced by stent thrombosis. Interestingly, other studies indicate that obese patients have a significantly lower platelet count when compared with normal weight patients.39 So, this could also be a reason responsible for this lower in-hospital and long-term mortality risks among overweight and obese patients after cardiovascular interventions.
The study published by Hastie et al in 2010 also supports our results.40 His study investigated the impact of body mass index on long-term all-cause mortality in patients following first-time elective PCI and it showed that increased BMI was associated with an improved 5-year survival rate. Another study published in 2009 by Oreopoulos et al showed that a paradoxical association between BMI and survival existed in patients with established CAD irrespective of treatment strategy and the author concluded that the reason behind this paradox could be that patients with obesity might be presenting earlier and receiving more aggressive treatments compared to those with normal BMI.41 The study published in 2013 by Hainer et al also supports the fact that this “obesity paradox” does exist.42 Furthermore, the meta-analysis by Sharma explaining the relationship of BMI with total mortality, after coronary revascularization (including PCI and CABG) showed a higher mortality rate among the underweight patients whereas a lower mortality rate was observed among the overweight patients.43 Another recent meta-analysis including 1,300,794 patients from 89 studies also showed a significantly lower short- and long-term mortality among the overweight and obese patients, whereas the rate of mortality among the underweight patients were significantly higher.44 The study by Lavie published in 2015 adds further support to this obesity paradox.45 The study dealing with obesity and cardiovascular diseases published by Lavie in 2014 also supports our results and the author concluded that although obesity is among one of the risk factors for cardiovascular disorders, an obesity paradox does exist showing that overweight and obese patients with cardiovascular diseases have a better prognosis compared to the nonobese/nonoverweight ones.46
Even though several studies show this obesity paradox to be present worldwide among obese patients from different ethnicities (observed in patients from Korea, Japan, America, and other European countries), the study conducted by He et al showed an absence of this paradox in Chinese patients above 75 years of age.30 This phenomenon was also not observed in 2 cohorts from a northern Chinese population.47–48
However, a few other studies from the Western regions also do not agree with this phenomenon. The study published by Akin et al in 2012 denies the existence of this “obesity paradox.”9 In his study, normal body weight patients and obese patients had similar rates of all-cause mortality; but in fact, his study dealt with the comparison of different types of coronary drug-eluting stents and their corresponding adverse clinical outcomes after PCI. Therefore, maybe that is why his results varied from our meta-analysis.
Oreopoulos et al meta-analysis published in 2008 compared the short- and long-term mortality in obese patients after cardiac interventions.8 His study included data from articles published almost 20 years ago, in the year 1996. His results supported the fact that the in-hospital and long-term mortality rates were similar or lower in obese patients compared to normal weight patients. Our result differs from his maybe because his study included not only post PCI patients but also post coronary artery bypass surgery patients.
Our meta-analysis is an updated version including studies published from the year 2000 to 2015 and consists mainly of post PCI patients. Consisting of the several obese groups, this current meta-analysis compares the mortality rate at different follow-up periods including (in-hospital, 1-year follow-up and ≥ 1-year mortality among the different categories of patients) after PCI. The medication use and risk factors prominent among these different BMI groups have also been shown in our study. The lower in-hospital and 1-year follow-up as well as ≥ 1-year mortality among the overweight and obese patients suggest that this “obesity paradox” still exists after PCI.
LIMITATIONS
Normally a patient with a BMI of >30 kg/m2 is considered as obese. However, in certain studies, patients with a BMI of >27.5 kg/m2 has been classified in the obese category. Similarly, the range for normal weight patients is supposed to be between 18.5 to <25 kg/m2 but in a few studies, a weight of <20 kg/m2 was considered underweight or a BMI of <25 kg/m2 was considered as normal weight patients (a BMI of <25 kg/m2 could also include underweight patients).
CONCLUSION
This “obesity paradox” does exist after PCI. The mortality in overweight and obese patients is indeed lower compared to the normal weight patients. However, the exact reasons for this phenomenon need further exploration and research in the future.
Footnotes
Abbreviations: BMI = body mass index, CAD = coronary artery diseases, DM = diabetes mellitus, PCI = percutaneous coronary intervention, RCTs = randomized controlled trials, RR = risk ratio.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Berghofer A, Pischon T, Reinhold T, et al. Obesity prevalence from a European perspective: a systematic review. BMC Public Health 2008; 8:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Yanovski SZ, Carroll MD, et al. The epidemiology of obesity. Gastroenterology 2007; 132:2087–2102. [DOI] [PubMed] [Google Scholar]
- 3.Wilson PW, D’Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Internal Med 2002; 162:1867–1872. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Graubard BI, Williamson DF, et al. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 2007; 298:2028–2037. [DOI] [PubMed] [Google Scholar]
- 5.Flegal KM, Graubard BI, Williamson DF, et al. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005; 293:1861–1867. [DOI] [PubMed] [Google Scholar]
- 6.Powell BD, Lennon RJ, Lerman A, et al. Association of body mass index with outcome after percutaneous coronary intervention. Am J Cardiol 2003; 91:472–476. [DOI] [PubMed] [Google Scholar]
- 7.Lancefield T, Clark DJ, Andrianopoulos N, et al. Is there an obesity paradox after percutaneous coronary intervention in the contemporary era? An analysis from a multicenter Australian registry. JACC Cardiovasc Interv 2010; 3:660–668. [DOI] [PubMed] [Google Scholar]
- 8.Oreopoulos A, Padwal R, Norris CM, et al. Effect of obesity on short- and long-term mortality postcoronary revascularization: a meta-analysis. Obesity 2008; 16:442–450. [DOI] [PubMed] [Google Scholar]
- 9.Akin I, Tolg R, Hochadel M, et al. No evidence of “obesity paradox” after treatment with drug-eluting stents in a routine clinical practice: results from the prospective multicenter German DES.DE (German Drug-Eluting Stent) Registry. JACC Cardiovasc Interv 2012; 5:162–169. [DOI] [PubMed] [Google Scholar]
- 10.National Heart L, and Blood Institute Expert Panel. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. http://www.nhlbi.nih.gov/guidelines/obesity (accessed April 3, 2011). [Google Scholar]
- 11.Higgins JPT AD. Cochrane handbook for systematic reviews of interventions: Wiley; 2008. [Google Scholar]
- 12.Gurm HS, Whitlow PL, Kip KE. The impact of body mass index on short- and long-term outcomes inpatients undergoing coronary revascularization. J Am College Cardiol 2002; 39:834–840. [DOI] [PubMed] [Google Scholar]
- 13.Gruberg L, Weissman NJ, Waksman R, et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol 2002; 39:578–584. [DOI] [PubMed] [Google Scholar]
- 14.Poston WS, Haddock CK, Conard M, et al. Impact of obesity on disease-specific health status after percutaneous coronary intervention in coronary disease patients. J Int Assoc Study Obes 2004; 28:1011–1017. [DOI] [PubMed] [Google Scholar]
- 15.Minutello RM, Chou ET, Hong MK, et al. Impact of body mass index on in-hospital outcomes following percutaneous coronary intervention (report from the New York State Angioplasty Registry). Am J Cardiol 2004; 93:1229–1232. [DOI] [PubMed] [Google Scholar]
- 16.Gruberg L, Mercado N, Milo S, et al. Impact of body mass index on the outcome of patients with multivessel disease randomized to either coronary artery bypass grafting or stenting in the ARTS trial: the obesity paradox II? Am J Cardiol 2005; 95:439–444. [DOI] [PubMed] [Google Scholar]
- 17.Nikolsky E, Kosinski E, Mishkel GJ, et al. Impact of obesity on revascularization and restenosis rates after bare-metal and drug-eluting stent implantation (from the TAXUS-IV trial). Am J Cardiol 2005; 95:709–715. [DOI] [PubMed] [Google Scholar]
- 18.Shubair MM, Prabhakaran P, Pavlova V, et al. The relationship of body mass index to outcomes after percutaneous coronary intervention. J Intervent Cardiol 2006; 19:388–395. [DOI] [PubMed] [Google Scholar]
- 19.Buettner HJ, Mueller C, Gick M, et al. The impact of obesity on mortality in UA/non-ST-segment elevation myocardial infarction. Eur Heart J 2007; 28:1694–1701. [DOI] [PubMed] [Google Scholar]
- 20.Mehta L, Devlin W, McCullough PA, et al. Impact of body mass index on outcomes after percutaneous coronary intervention in patients with acute myocardial infarction. Am J Cardiol 2007; 99:906–910. [DOI] [PubMed] [Google Scholar]
- 21.Kosuge M, Kimura K, Kojima S, et al. Impact of body mass index on in-hospital outcomes after percutaneous coronary intervention for ST segment elevation acute myocardial infarction. Circ J 2008; 72:521–525. [DOI] [PubMed] [Google Scholar]
- 22.Das SR, Alexander KP, Chen AY, et al. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry). J Am Coll Cardiol 2011; 58:2642–2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang ZJ, Zhou YJ, Zhao YX, et al. Effect of obesity on repeat revascularization in patients undergoing percutaneous coronary intervention with drug-eluting stents. Obesity 2012; 20:141–146. [DOI] [PubMed] [Google Scholar]
- 24.Kaneko H, Yajima J, Oikawa Y, et al. Obesity paradox in Japanese patients after percutaneous coronary intervention: an observation cohort study. J Cardiol 2013; 62:18–24. [DOI] [PubMed] [Google Scholar]
- 25.Kang WY, Jeong MH, Ahn YK, et al. Obesity paradox in Korean patients undergoing primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. J Cardiol 2010; 55:84–91. [DOI] [PubMed] [Google Scholar]
- 26.Park DW, Kim YH, Yun SC, et al. Association of body mass index with major cardiovascular events and with mortality after percutaneous coronary intervention. Circu Cardiovasc Interv 2013; 6:146–153. [DOI] [PubMed] [Google Scholar]
- 27.Witassek F, Schwenkglenks M, Erne P, et al. Impact of Body Mass Index on mortality in Swiss hospital patients with ST-elevation myocardial infarction: does an obesity paradox exist? Swiss Med Weekly 2014; 144:w13986. [DOI] [PubMed] [Google Scholar]
- 28.Colombo MG, Meisinger C, Amann U, et al. Association of obesity and long-term mortality in patients with acute myocardial infarction with and without diabetes mellitus: results from the MONICA/KORA myocardial infarction registry. Cardiovasc Diabetol 2015; 14:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Numasawa Y, Kohsaka S, Miyata H, et al. Impact of body mass index on in-hospital complications in patients undergoing percutaneous coronary intervention in a Japanese real-world multicenter registry. PloS One 2015; 10:e0124399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He PY, Yang YJ, Qiao SB, et al. Impact of body mass index on the clinical outcomes after percutaneous coronary intervention in patients >/ = 75 years old. Chin Med J 2015; 128:638–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grover SA, Kaouache M, Rempel P, et al. Years of life lost and healthy life-years lost from diabetes and cardiovascular disease in overweight and obese people: a modelling study. Lancet Diab Endocrinol 2015; 3:114–122. [DOI] [PubMed] [Google Scholar]
- 32.Mongraw-Chaffin ML, Peters SA, Huxley RR, et al. The sex-specific association between BMI and coronary heart disease: a systematic review and meta-analysis of 95 cohorts with 1.2 million participants. Lancet Diab Endocrinol 2015; 3:437–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Schutter A, Lavie CJ, Milani RV. The impact of obesity on risk factors and prevalence and prognosis of coronary heart disease-the obesityparadox. Prog Cardiovasc Dis 2014; 56:401–408. [DOI] [PubMed] [Google Scholar]
- 34.Shiraishi J, Kohno Y, Sawada T, et al. Relation of obesity to acute myocardial infarction in Japanese patients. Circul J 2006; 70:1525–1530. [DOI] [PubMed] [Google Scholar]
- 35.Jaber WA, Lennon RJ, Mathew V, et al. Application of evidence-based medical therapy is associated with improved outcomes after percutaneous coronary intervention and is a valid quality indicator. J Am Coll Cardiol 2005; 46:1473–1478. [DOI] [PubMed] [Google Scholar]
- 36.Diercks DB, Roe MT, Mulgund J, et al. The obesity paradox in non-ST-segment elevation acute coronary syndromes: results from the Can Rapid risk stratification of Unstable angina patients Suppress Adverse outcomes with early implementation of the American College of Cardiology/American Heart Association Guidelines Quality Improvement Initiative. Am Heart J 2006; 152:140–148. [DOI] [PubMed] [Google Scholar]
- 37.Steinberg BA, Cannon CP, Hernandez AF, et al. Medical therapies and invasive treatments for coronary artery disease by body mass: the “obesity paradox” in the Get With The Guidelines database. Am J Cardiol 2007; 100:1331–1335. [DOI] [PubMed] [Google Scholar]
- 38.Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207. [DOI] [PubMed] [Google Scholar]
- 39.Corica F, Corsonello A, Buemi M, et al. Platelet magnesium depletion in normotensive and hypertensive obese subjects: the role of salt-regulating hormones and catecholamines. Magnes Res 1999; 12:287–296. [PubMed] [Google Scholar]
- 40.Hastie CE, Padmanabhan S, Slack R, et al. Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. Eur Heart J 2010; 31:222–226. [DOI] [PubMed] [Google Scholar]
- 41.Oreopoulos A, McAlister FA, Kalantar-Zadeh K, et al. The relationship between body mass index, treatment, and mortality in patients with established coronary artery disease: a report from APPROACH. Eur Heart J 2009; 30:2584–2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hainer V, Aldhoon-Hainerova I. Obesity paradox does exist. Diabetes care 2013; 36 Suppl 2:S276–S281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sharma A, Vallakati A, Einstein AJ, et al. Relationship of body mass index with total mortality, cardiovascular mortality, and myocardial infarction after coronary revascularization: evidence from a meta-analysis. Mayo Clin Proc 2014; 89:1080–1100. [DOI] [PubMed] [Google Scholar]
- 44.Wang ZJ, Zhou YJ, Galper BZ, et al. Association of body mass index with mortality and cardiovascular events for patients with coronary arterydisease: a systematic review and meta-analysis. Heart 2015; pii: heartjnl 2014-307119. [DOI] [PubMed] [Google Scholar]
- 45.Lavie CJ, De Schutter A, Milani RV. Body composition and the obesity paradox in coronary heart disease: can heavier really be healthier? Heart 2015; pii: heartjnl-2015 307966. [DOI] [PubMed] [Google Scholar]
- 46.Lavie CJ, McAuley PA, Church TS, et al. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am Coll Cardiol 2014; 63:1345–1354. [DOI] [PubMed] [Google Scholar]
- 47.Wang ZJ, Zhou YJ, Liu YY, et al. Obesity and cardiovascular thrombotic events in patients undergoing percutaneous coronary intervention with drug-eluting stents. Heart 2009; 95:1587–1592. [DOI] [PubMed] [Google Scholar]
- 48.Li Y, Wu C, Sun Y, et al. Obesity paradox: clinical benefits not observed in obese patients with ST-segment elevation myocardial infarction: a multicenter, prospective, cohort study of the northern region of China. Int J Cardiol 2013; 168:2949–2950. [DOI] [PubMed] [Google Scholar]


