Abstract
The aim of this study was to determine reliability and validity of the Spanish version of the Disability Assessment for Dementia Scale (DAD-E) in the following areas: content, response process, internal structure, and relation to other constructs.
We designed a cross-sectional observational study. The DAD-E was administered to 132 participants diagnosed with mild cognitive decline, prodromal Alzheimer disease, Alzheimer disease, or no cognitive decline. For the reliability study, we performed analyses of internal consistency, test–retest, and equivalent measures. To study validity, we performed item analysis, principal components analysis, and correlations with other measures.
The sample was composed of 37 healthy participants (28%) and 95 patients (72%). In the total scale, Cronbach alpha was 0.963, intraclass correlation coefficient in the test–retest analysis was 0.983 (95% CI [95% confidence interval] = 0.969–0.991), and the analysis for equivalent measures was 0.949 (95% CI = 0.897–0.975). Out of the 40 items, we found that 37 presented a correlation index with the total score above 0.40. The principal components analysis suggests that 61.7% of the variance is explained by a single component that groups all scores on Activities of Daily Living. The DAD total score presents correlations with Barthel's Index of 0.882 (P = 0.000) and with Lawton and Brodie's Index of 0.877 (P = 0.000) and with the Mini Mental State Examination of 0.679 (P = 0.000).
The DAD-E is a reliable and valid instrument to assess functional disability in people with cognitive decline in Spanish population.
INTRODUCTION
Dementias represent an important socio-sanitary problem for developed countries due to their high prevalence; it is estimated that currently 17.01 million people suffer from Alzheimer disease (AD) in the world1 due to their impact on the individual and their socio-familiar environment. The economic cost per individual case is high, oscillating between 18,000 and 30,000 Euros a year; the care-taking responsibility of most patients in Spain falls on the family, who adopt 72% of care taking.2
Cognitive decline, along with behavioral and psychological alterations, is responsible for the patient's functional decline, losing the ability to carry out activities of daily living (ADLs) and becoming dependent on their surroundings and on others to care for them. Functional decline is progressive, and usually follows a hierarchical pattern; the study of this pattern is one of the key elements of the assessment of dementia patients.
The Disability Assessment for Dementia Scale (DAD) Scale3 is an instrument used to assess functional capacity by assessing Basic Activities of Daily Living (BADL) as well as Instrumental activities of daily living (IADL) and leisure. In comparison to other specific functional scales for dementia, the DAD assesses each ADL not only by gathering information about whether the patient is able to execute it but also if the patient shows initiative and if the patient is able to plan for it and organize it. Thus, it provides information about the cognitive dimensions of the functional disability in terms of executive functioning.
The original version of the DAD has demonstrated good psychometric properties.3 Adaptations to other countries do exist that also have good psychometric data,4–9 and a reduced 6-item version has also been developed.10
For the development of the Spanish version of the DAD (DAD-E), a first phase of linguistic and cultural adaptation was carried out, using a double translation process, back-translation, and pilot study.11 The DAD-E contains all of the 40 original items, some of them modified so as to maintain the conceptual equivalence. The instructions were changed and extended so as to increase content validity. Finally, it also maintained the original way in which the answers are coded and scored whilst adding 4 new codes and 8 new scores that aim to detect functional disability caused by cognitive decline so as to not confuse it with other causes.11
The current study aims to analyze reliability and validity on the basis of content, response process, internal structure, and relation to other constructs of the Spanish version of the Disability Assessment of Dementia Scale (DAD-E).
MATERIALS AND METHODS
Design and Procedure
The study follows a descriptive, observational, cross-sectional design, in which 95 patients and 37 healthy volunteers participated. The patients all were recruited from the Dementia Department of the Neurology Service at the Hospital General Universitario in Alicante (HGUA). The diagnoses included mild cognitive decline (MCD)12; prodromal Alzheimer disease (AD),13 and AD.14 Participants had to be living in the community and with a reliable Spanish-speaking carer. Informed consent was obtained from both patients and carers.
In patients suffering from AD, we frequently find multiple pathologies as well as depression.15 Therefore, their presence has not been considered part of the exclusion criteria.
Healthy participants were recruited from the Experience Lectures of the Universidad Miguel Hernández. People independent in their ADLs and with no disorders that would contaminate the results or interfere with the tests were included.
The study was approved by the Ethics Committees of the Hospital and the University Miguel Hernandez.
INSTRUMENTS
The DAD-E11 is composed by 40 items that assess 4 basic ADLs (BADL: hygiene, dressing, continence, and eating; 17 items), and 6 instrumental activities (preparing of meals, use of telephone, finance and correspondence, medication, and leisure and domestic activities; 23 items). The items also reflect cognitive dimensions of functional capacity in terms of executive functioning: Initiative (13 items), planning and organization (10 items), and execution (17 items) (Annex 1, http://links.lww.com/MD/A487). The scale is administered through an interview with the main caretaker, who provides information about the patient's ADLs, using the 2 previous weeks as reference. The mean administration time is 9.5 minutes.
Answers are coded as: Yes, No, or Nonapplicable (never, no opportunity), just as in the original version; the DAD-E also includes Nonapplicable due to sensory or motor deficit, sensory, and motor deficit or due to other noncognitive causes. The total scores (0–40) and subscores are obtained by adding the scores in the corresponding items, and increase according to functional ability. The relative scores in percentages take into account the number of items that are applicable.
Barthel's Index (BI) is the measure most frequently used for ADLs16 and it is used as a golden standard. It assesses 10 different areas of BADL: eating, transfers between bed and chair, grooming, use of toilet, bathing, mobility, use of stairs, dressing and undressing, bowel control, and bladder control.
The Lawton and Brodie Index (LI) assesses functional capacity in instrumental ADLs. Its use is extended and includes use of the phone, shopping, food preparation, caring of the house, washing of clothes, use of transport, medication, and financial matters.17
The Mini Mental State Examination (MMSE) is the most frequently used test for short assessments of cognitive abilities.18 It includes spatial and temporal orientation, memory, attention and calculus, recall, language, and constructive praxis.
Statistical Procedure
All data were processed using SPSS version 21.0. We performed descriptive analysis, association analysis between qualitative variables (Pearson χ2), and mean comparisons (Student t test, analysis of variance [ANOVA], and analysis of covariance [ANCOVA], Mann–Whitney U or K-W); we also analyzed response patterns for all items.
Internal consistency reliability was assessed calculating Cronbach alpha and Guttman coefficients. Using a test–retest design, the same interviewer applied the DAD twice, with a mean of 32 days between administrations (N = 41). Using an equivalent measures design (inter-rater agreement), 2 interviewers administered the DAD independently, in a mean period of 1.2 days. In both designs, we obtained the intra-class correlation coefficients (model of 2 factors with random effects) for the scales, and Kappa coefficients for the items, by applying a specific macro,19 which also provides confidence intervals (CIs).
For the validity analysis based on the internal structure, we calculated item-scale (Spearman) and inter-scale (Pearson) correlation coefficients. Also, we performed a principal components analysis (PCA), obtaining a Kaiser-Meyer-Olkin index and performing Bartlett sphericity test. The components were grouped using a Varimax-rotated components matrix with Kaiser.
Validity based on the relation to other constructs was analyzed by calculating Pearson correlation coefficients and CI at 95% between the DAD and BI and Lawton and Brodie's Index (convergent validity), which were administered by occupational therapists who were blind to the patient's diagnosis. Also, Pearson coefficients were also calculated with the MMSE (divergent validity), which was administered by a neurologist, who also diagnosed and classified the participants into all 4 categories. The primary data and the database used for the analysis is available upon request from the first author.
RESULTS
Sample
The sample included 132 participants: 37 healthy participants (28%) and 95 patients, diagnosed with MCD (N = 27; 20.5%), prodromal AD (N = 13; 9.8%), or AD (N = 55; 41.7%). The sample was composed by 64.4% of women (N = 85). There was no difference in the distribution of diagnoses between the genders (χ2 = 1.365; P = 0.714) (Table 1).
TABLE 1.
Demographic and Clinical Characteristics of the Sample
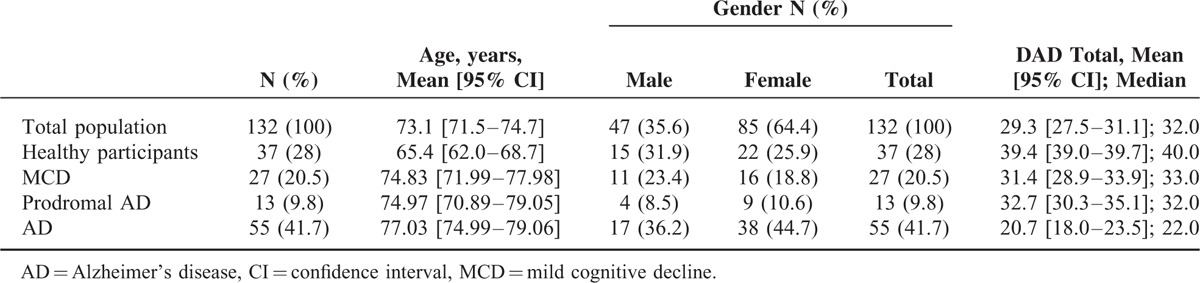
Mean age was 73.1 years (95% CI 71.5–74.7; Median: 76.0). The median age among the healthy sample was 64.0 (Mean = 65.4; 95% CI 62.0–68.7), while the median age for the patient sample was 77.2 (Mean = 76.1; 95% CI 74.6–77.6), with differences (t = 5.893; P = 0.000; fd = 51.347).
VALIDITY BASED ON CONTENT AND RESPONSE PROCESS
Description of DAD Total
The DAD total has a theoretical range between 0 and 40 points. The mean score is 29.3 (Table 2). Men's mean score is 30.4 (95% CI 27.8–33.0; Median: 31.0) and for women it is 28.7 (95% CI 26.2–31.2; Median: 33.0), with no differences (t = 0.951; P = 0.344; fd = 117.01).
TABLE 2.
Description of Scores for DAD Total and Subscales
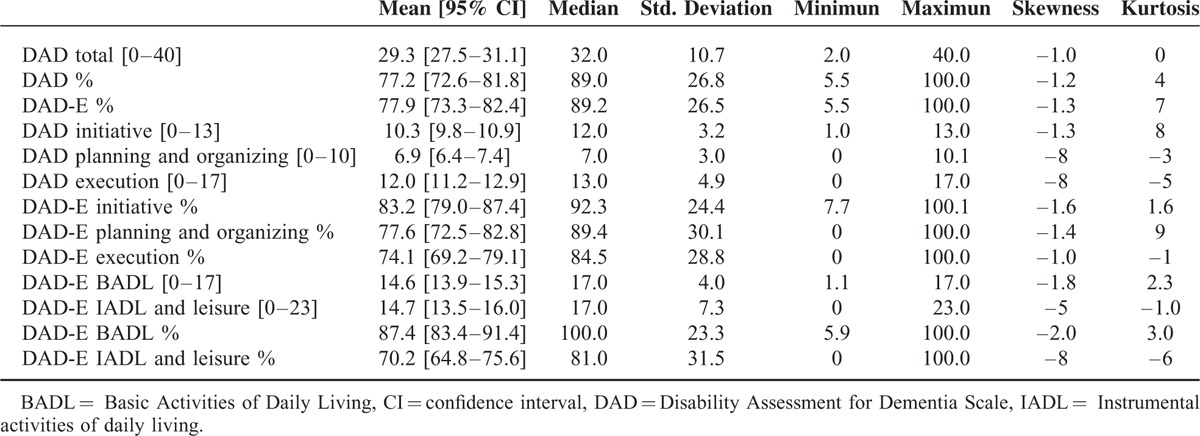
Men score higher in the DAD% (t = 2.313; P = 0.022; fd = 121.8), DAD-E in % (t = 1.969; P = 0.003; fd = 130), and in the DAD subscales of Execution (t = 1.992; P = 0.049; fd = 118.8), DAD Execution % (t = 2.642; P = 0.009; fd = 119.7), and in the DAD-E IADL subscale and Leisure % (t = 2.359; P = 0.020; fd = 118.4). There are no differences based on the gender of the carer.
Depending on the diagnostic group, there were significant differences between groups for DAD Total scores (F = 50.136; P = 0.000; fd = 3128). As the average age of healthy participants differs very much among the patients, we entered age into the analysis as a covariate. Again, we found a significant effect of diagnostic group on DAD scores after controlling for the effect of participants’ age (F = 37.952; P = 0.000; fd = 3.127). Contrast analysis showed that healthy participants had significantly higher DAD scores than the other 3 groups of patients, and AD subjects had the lowest (P = 0.000). No differences were found between MCD and prodromal AD patients (Table 1).
We also selected 2 subgroups, 1 made up of healthy participants and the other of patients; we were able to match these for age (range 60–69). The analysis of the differences in Total DAD scores showed similar results to those obtained with the total sample: the participants who obtained the highest scores on Total DAD were the healthy participants (N = 17), followed by those with MCD (N = 7), prodromal AD (N = 3), and finally by patients suffering from Alzheimer type dementia (N = 2) (K-W = 21.95; P < 0.000) (Graph 1, http://links.lww.com/MD/A487).
Item Analysis
Out of 40 items, there were instances wherein 31 of these did not apply.
The answer “Never” appears in 4.8% of all possible responses to 14 of the items. Out of them, 36.9% belong to the finance and correspondence subscale, and mostly to women (N = 66; 71.0%); 29.8% belong to items from the Leisure and domestic activities subscales; all were men.
The answer “No opportunity” appears in 0.5% of 11 items, especially in the IADL “going on outings” (40%), and most frequently among women (N = 6; 60%).
The answer “Motor Deficit” appears in 0.7% in 18 items, mostly regarding the BADL “dressing,” and mostly among women (N = 9; 90%).
The answer “Sensory Deficit” appears 0.02% in the IADL “use of the telephone” and was associated with hypoacusia.
The answer “Other non-cognitive causes” appeared 0.04% of the time. It appeared in the IADL “going on outings,” in item 29 and it was due to fatigue, and in the IADL “Medication,” in item 35, the cause was that the patient was illiterate.
RELIABILITY OF THE SPANISH VERSION OF THE DAD SCALE
Internal Consistency Analysis
Cronbach alpha for the scale is 0.963 and does not vary if some of the items are deleted [0.961–0.963] (N = 40). Both for the executive functioning scales (DAD initiation, DAD planning and organizing and DAD execution) and for the ADLs (DAD-E BADL and DAD-E IADL and leisure), the range obtained is between 0.875 and 0.947 and does not vary significantly, if one of the elements is deleted.
Regarding the ADL subscales, the internal consistency results for 6 of 10 scales was above 0.80; in 3 of the subscales (dressing, continence, and use of the phone), the coefficient ranges between 0.70 and 0.78, and the subscale “Eating” is the one that presents the lowest score (0.56).
The Guttman coefficient presents similar results.
Test–Retest Analysis
The intraclass correlation coefficients show high values for the DAD Total (ICCA = 0.983; 95% CI = 0.969–0.991) as well as for the rest of the total scores and subscales [0.863–0.984] (N = 23). The results of the analysis of variance show the lack of bias in all scales and subscales because the mean scores on baseline and retest show no statistically significant differences, except for the DAD-E “Execution” subscale % (F = 4.756; P = 0.035).
Regarding the agreement between items, most kappa coefficients (N = 35) range between 0.77 and 1. The remaining 5 items (items 1, 8, 15, 24, and 25) present moderate agreement (0.54–0.72).
Equivalent Measures Analysis: Inter-Rater Agreement
Inter-rater reliability for the DAD Total shows a very high level of agreement (ICCA = 0.949; 95% CI = 0.897–0.975). The values obtained for DAD %, DAD-E %, and subscale scores range between 0.775 and 0.996, except for the DAD-E “Telephone” subscale (0.671) and DAD-E “Finance” (0.643). There was absence of bias in for all subscales except for the DAD “Planning and Organizing” subscale (0.048) (N = 23).
Kappa indexes show that 17 of the items maintain an agreement ranging from 0.76 to 1; 19 between 0.47 and 0.74; and 4 between 0.26 and 0.35 (items 23, 24, 25, 36).
VALIDITY BASED ON INTERNAL STRUCTURE
Item-Scale Correlation Analysis
The majority of items (N = 37) correlate with the total score with a coefficient above 0.40 [0.419–0.762]. Coefficients below 0.40 are obtained for item 15 (ρ = 0.251), item 8 (ρ = 0.333), and item 17 (ρ = 0.373).
The correlation coefficients are higher for the items within the subscales they belong to [ρ = 0.282–0.805] than with the ones that they do not belong to [ρ = 0.224–0720], except for items 4, 20, and 39 for the DAD subscales of “Planning and organizing” and “Execution” and for items 8 and 10 from DAD “Dressing.”
Subscale–Scale Correlation Analysis
All scores from the subscales correlate with DAD Total above 0.75, except for subscales DAD-E “Eating” (r = 0.580) and DAD-E “Continence” (r = 0.679).
The DAD-E BADL subscale presents correlation coefficients that are higher with the BADL subscales [r = 0.773–0.963] than with IADL [r = 0.542–0.694], except for with the subscale “Eating” (0.641). The DAD-E IADL subscale correlates highest with the IADL subscales [r = 0.754–0.870] than with the BADL subscales [r = 0.496–0.736].
Principal Component Analysis of ADL Subscales
For the PCA of the ADL scales, nonsphericity is demonstrated (χ2 = 944,072, fd = 45; P = 0.000) as well as excellent values for the Kaiser-Meyer-Olkin index (KMO = 0.919). The PCA groups all the scores on the ADL subscales in a single component, explaining 61.7% of the variance (Graph 2, http://links.lww.com/MD/A487).
VALIDIDTY BASED ON THE RELATIONSHIP WITH CONSTRUCTS: CONVERGENT AND DISCRIMINATING CRITERION VALIDITY
The correlation between the DAD Total and the BI is 0.882, and between the DAD Total and the LI is 0.877. These coefficients are higher between the DAD-E BADL subscale and the BI (r = 0.942; P = 0.000) and between the DAD-E IADL and “Leisure” and LI (r = 0.900; P = 0.000). The correlation between the DAD Total and MMSE is 0.679 (P = 0.000).
DISCUSSION
This study has aimed to validate the DAD for Spanish population. This process has confirmed the content validity and adequacy of the response process of the DAD-E. No atypical response patterns have been detected. As was expected, no participants showing difficulties in BADL were able to independently carry out IADLs. The lower scores, which indicate higher functional disability, were obtained by patients diagnosed with AD, and the higher scores by the healthy participants.
Scores on the DAD-E do not vary on the basis of the gender of the carer, but do vary on the basis of the gender of the patient. Men score higher on DAD %, DAD-E % and for the DAD-E “Execution” % subscale and the DAD IADL and Leisure %. These differences can be explained by the high number of “Never” responses on the items regarding housework, food preparation, and shopping. It would be convenient to establish different cut-off points depending on the gender of the patient for future studies.
The frequency of responses Nonapplicable, motor deficit, sensory deficit, sensory, and motor deficit, and other noncognitive causes has been low, but has increased the precision of the assessment of functional deficits due to cognitive decline.
The DAD-E has been shown to be a highly reliable instrument. In first place, the internal consistency indexes are excellent, similar to the original version and above the validations conducted in other countries.
In second place, both in the application of the test–retest design and the inter-rater reliability study, the intra-class correlation indexes for the DAD total and the subscales show a very good level of agreement.20 These results support the stability of the assessment of functional disability of the patients and the equivalence between different interviewers. These data are similar to what has been found in other studies in relation to the total scores and, in particular, to the subscales (Italian version).
Regarding the validity based on the internal structure, in first place, we analyzed the structure of the relationships between the items, the total score, and the subscales and between the subscales.
With only a few exceptions, the items show high correlations with the total scores and with the score of the subscale they belong to, and only moderate with the rest of the scales. Also, the correlations of the subscales are higher with the total score than with the other subscales. These data support the existence of the executive functioning subscales and of ADL type as independent constructs in the DAD-E scale. Therefore, we can use the subscales of these 2 dimensions separately and assess the different types of cognitive decline in different stages of the disorder.
Finally, the PCA performed with the scores of the 10 ADL subscales shows that they all saturate on a single component, which explains 61.7% of the variance. These data support the idea that the internal structure of the DAD scale is a measure for functional decline.
In spite of our good results, the behavior of items 8, 15, and 17 has not been optimal in the different validity and reliability analysis. These items refer to very basic ADLs, such as eating and dressing, which most participants show to be intact; therefore, they show a very low variability. In future studies, their performance should be tested with a sample of patients that includes those suffering from advanced AD.
Items 23, 24, 25, and 36 have shown poor results in the equivalent measures analysis. It is possible that their content is perceived as ambiguous (eg, “appropriate and adequate”) or because they include more than 1 activity; therefore, the answers could be relating to different activities in each assessment.
Regarding the validity based on the relation to other constructs, the results support the convergent validity of the DAD-E. On the one hand, we found high coefficients between the DAD Total and the other scales that also measure functional capacity. These coefficients are even higher between the DAD-E BADL and BI, which assesses BADL specifically, and between the DAD-E IADL and Leisure and the LI, which assesses IADLs. On the other hand, the moderate correlation we found between the DAD-E and the MMSE supports discriminating validity, as the course of cognitive decline and functional decline are associated but not parallel, as well as being different constructs. Similar results have been found in other validation studies (Chinese and Turkish versions on the DAD).
The DAD-E has been shown to be a valid and reliable instrument to assess functional capacity in non-institutionalized patients suffering from cognitive decline. The DAD-E can be used in studies following the development of cognitive decline, assessment of therapeutic efficacy in our specific environment, and in routine neurology consultations as an instrument aiding the diagnosis of AD.
Acknowledgments
We are grateful for the support provided by the Neurology Service of the Hospital General Universitario in Alicante and Pathology and Surgery Department of Miguel Hernandez University of Elche, and really thank the patients and their families for participating in this study.
Footnotes
Abbreviations: AD = Alzheimeŕs disease, ADL = Activities of Daily Living, BADL = Basic Activities of Daily Living, BI = Barthel's Index, DAD = Disability Assessment for Dementia Scale, DAD-E = Spanish version of the Disability Assessment for Dementia Scale, HGUA = Hospital General Universitario in Alicante, IADL = Instrumental activities of daily living, LI = Lawton and Brodie Index, MCD = Mild cognitive decline, MMSE = Mini Mental State Examination.
Supplemental Digital Content is available for this article.
The authors have no conflicts of interest to declare.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet 2005; 366:2112–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Comité ad hoc Sociedad Valenciana de Neurología. Plan de asistencia integral a los pacientes con enfermedad de alzheimer y otras demencias en la comunidad valenciana. 2002. Available at: http://svneurologia.org/paidem.htm [Accessed July 28, 2014]. [Google Scholar]
- 3.Gelinas I, Gauthier L, McIntyre M, et al. Development of a functional measure for persons with Alzheimer's disease: the disability assessment for dementia. Am J Occup Ther 1999; 53:471–481. [DOI] [PubMed] [Google Scholar]
- 4.Mok CC, Siu AM, Chan WC, et al. Functional disabilities profile of Chinese elderly people with Alzheimer's disease: a validation study on the Chinese version of the disability assessment for dementia. Dement Geriatr Cogn Disord 2005; 20:112–119. [DOI] [PubMed] [Google Scholar]
- 5.De Vreese LP, Caffarra P, Savare R, et al. Functional disability in early Alzheimer's disease: a validation study of the Italian version of the disability assessment for dementia scale. Dement Geriatr Cogn Disord 2008; 25:186–194. [DOI] [PubMed] [Google Scholar]
- 6.Suh GH. Development of the Korean version of disability assessment for dementia scale (DAD-K) to assess function in dementia. J Korean Geriatr Soc 2003; 7:278–287. [Google Scholar]
- 7.Carthery-Goulart MT, Areza-Fegyveres R, Schultz RR, et al. Cross-cultural adaptation of the disability assessment for dementia (DAD). Arq Neuropsiquiatr 2007; 65:916–919. [DOI] [PubMed] [Google Scholar]
- 8.Bahia VS, Carthery-Goulart MT, Novelli MM, et al. Functional disability in Alzheimer disease: a validation study of the Brazilian version of the disability assessment for dementia (DAD-br). Alzheimer Dis Assoc Disord 2010; 24:291–295. [DOI] [PubMed] [Google Scholar]
- 9.Tozlu M, Cankurtaran M, Yavuz BB, et al. Functional disability in Alzheimer disease: a validation study of the Turkish version of the disability assessment for dementia scale. J Geriatr Psychiatry Neurol 2014; 27:237–246. [DOI] [PubMed] [Google Scholar]
- 10.de Rotrou J, Wu YH, Hugonot-Diener L, et al. DAD-6: a 6-item version of the disability assessment for dementia scale which may differentiate Alzheimer's disease and mild cognitive impairment from controls. Dement Geriatr Cogn Disord 2012; 33:210–218. [DOI] [PubMed] [Google Scholar]
- 11.Sánchez-Pérez A. Adaptación y validación de la escala disability assessment for dementia (DAD) en la población española castellano hablante. Alicante: Universidad Miguel Hernández; 2013. [Google Scholar]
- 12.Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 1999; 56:303–308. [DOI] [PubMed] [Google Scholar]
- 13.Dubois B, Feldman HH, Jacova C, et al. Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 2007; 6:734–746. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM IV. 4th ed.Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 15.Fernandez M, Gobartt AL, Balana M. COOPERA Study Group. Behavioural symptoms in patients with Alzheimer's disease and their association with cognitive impairment. BMC Neurol 2010; 10:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Valverde M, Flórez M, Sánchez I. Activities of daily living scales. Rehabilitación 1994; 28:377–388. [Google Scholar]
- 17.Baztán J, González J, Del Ser T. Del Ser T, Peña-Casanova J. Escalas de actividades de la vida diaria. Evaluación neuropsicológica y funcional de la demencia. Barcelona: J. R. Prous Editores; 1994. 137–164. [Google Scholar]
- 18.Peña- Casanova J, Gramunt-Fombuena N, Gich-Fullá J. Test neuropsicológicos. Fundamentos para una neuropsicología clínica basada en evidencias. Barcelona: Masson S. A; 2004. [Google Scholar]
- 19.Domenech J, Granero R. Macro ¡KAPPA for SPSS Statistics. Weighted Kappa [computer program]. V2009.07.31. Available at: http://www.metodo.uab.cat/macros.htm (accessed 5 March 2013). [Google Scholar]
- 20.Fleiss J. Statistical Methods for Rates and Proportions. 2nd ed.New York: John Wiley; 1981. [Google Scholar]


