Abstract
Although the benefits of wound care services and multidisciplinary team care have been well elaborated on in the literature, there is a gap in the actual practice of wound care and the establishment of an efficient referral system. The conceptual framework for establishing efficient wound management services requires elucidation.
A wound care center was established in a tertiary hospital in 2010, staffed by an integrated multidisciplinary team including plastic surgeons, a full-time coordinator, a physical therapist, occupational therapists, and other physician specialists. Referral patients were efficiently managed following a conceptual framework for wound care. This efficient wound management service consists of 3 steps: patient entry and onsite immediate wound debridement, wound re-evaluation, and individual wound bed preparation plan. Wound conditions were documented annually over 4 consecutive years.
From January 2011 to December 2014, 1103 patients were recruited from outpatient clinics or inpatient consultations for the 3-step wound management service. Of these, 62% of patients achieved healing or improvement in wounds, 13% of patients experienced no change, and 25% of patients failed to follow-up. The outcome of wound treatment varied by wound type. Sixty-nine percent of diabetic foot ulcer patients were significantly healed or improved. In contrast, pressure ulcers were the most poorly healed wound type, with only 55% of patients achieving significantly healed or improved wounds.
The 3-step wound management service in the wound care center efficiently provided onsite screening, timely debridement, and multidisciplinary team care. Patients could schedule appointments instead of waiting indefinitely for care. Further wound condition follow-up, education, and prevention were also continually provided.
INTRODUCTION
Chronic wounds significantly influence patients’ quality of life by restricting mobility (eg, pain, multilayer bandages),1 increasing social isolation,2 and presenting negative psychological impacts (eg, depression, anxiety, and low self-esteem).3,4 Nevertheless, wound care procedures vary between hospitals. For example, ∼70% of chronic leg ulcers are venous ulcers for which compression therapy is the gold standard treatment.5 However, a US study found that only 17% of patients with venous leg ulcers received compression therapy.6
Wound management difficulties can be attributed to 3 main problems. First, there is no standardization. The lack of information and skill can result from poor access to evidence-based guidelines.6 Nonstandardized, inaccurate, and nonreproducible pathways increase the difficulties related to tracking wound healing and providing continuity of care. Second, multidisciplinary teams are not well integrated. Many health care specialists (eg, general practitioners, pharmacists, skin/vascular specialists, and outpatient clinicians) find it difficult and confusing to know who to ask for help with managing wound care across different departments. In addition, health care systems lack integration of chronic disease primary care, health promotion, illness prevention, and early intervention.7 Third, there is no specific unit that is responsible for wound care and multidisciplinary integration. The absence of a specific unit can result in the dispersion of responsibility for wound care among specialists, inconsistency of wound service, and complexity of budgetary and financial cost.
Wound management services provide care for patients with chronic wounds resulting from diabetes, poor circulation, improper off-loading, and immune-compromising conditions. The goals of wound management services are to treat chronic wounds through the stages of healing, reduce infections or complications, and prevent future chronic wounds as well as restore the functional activities of daily life.8
Although the benefits of wound care services and multidisciplinary team care have been thoroughly discussed,9–11 there is a functional gap concerning the establishment of an efficient referral system. Patients are often confused regarding whom to see for wound care, and healthcare providers (plastic specialists, dermal specialists, general practitioners, and nurses) find it difficult to manage wound care across disparate levels of departments. Therefore, we intended to organize the conceptual framework of a multidisciplinary wound care center, which provides the efficient clinical referral path to wound healing.
METHODS
Organization of the Wound Care Center
The wound care center was established in August 2010 in Chang Gung Memorial Hospital, Chiayi, Taiwan, providing 1339 beds for patient care with a large rural referral and catchment area in a township area. The members of the wound care center and other specialists from different departments are integrated into a multidisciplinary team that works on individual cases, general protocols, and education and prevention in the community. The center's medical director is the department chief of plastic surgery; the director and another plastic surgeon, rather than a training resident, provide patient consultations for potential wound intervention candidates. Vascular or orthopedic surgeons, podiatrists, internists, infectious disease specialists, and prosthetists are also available for consultation as needed. A full-time licensed nurse practitioner (coordinator) of wound care is also responsible for wound management assistance, scheduling, photography, and documentation. Physical therapists and occupational therapists provide rehabilitation programs within the center, such as offloading therapy and scar care education, to help the patients attain functional restoration earlier. Furthermore, improvement in physical appearance is emphasized through processes such as scar care, which can improve a patient's quality of life. The aesthetic medical center is located right beside our wound care center, which can provide laser therapy or any other cosmetic procedures as necessary.
Wound Management Pathway
The conceptual framework for wound management service consists of 3 steps (Fig. 1). The first step is patient entry and onsite immediate wound debridement, which indicates the patient referral process where wound center clients are referred from outpatient clinics and inpatient consultation. Outpatient clinics can be wound care clinics or combined clinics (plastic or orthopedic surgeon or endocrinologist). For inward consultation (inpatient) (Fig. 2), the wound care service is initiated once the physician from any other department considered wound care service necessary. The patient is scheduled for a visit to the wound care center by the coordinator; the appointed doctor can meet the patient and family on the arranged day to discuss the wound condition with them. Without an uncertain waiting period, senior consultants can approach patients in person with professional wound assessments and perform immediate debridement onsite as needed. For example, if ambulation is possible, staff will examine the patient at the wound care center as scheduled, and onsite debridement or wound care advice is performed immediately. If the patient is not ambulatory, staff (visiting and resident staff) proceed to the bedside for further management the next morning, providing the same debridement or wound care advice. If anesthesia is necessary depending on wound severity, the staff can set the debridement schedule in the operation room for the next day.
FIGURE 1.
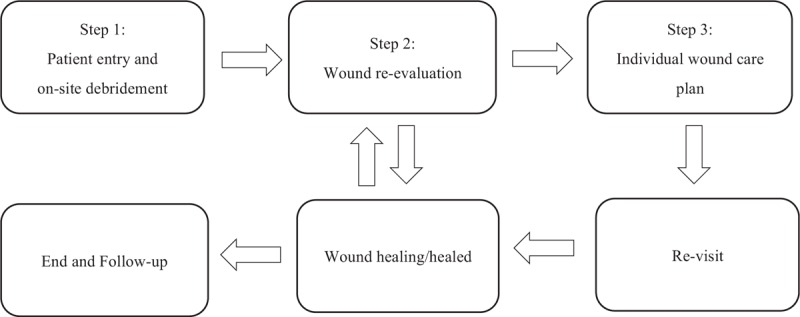
The conceptual framework for wound management service contains 3 steps, including patient entry/onsite debridement, wound re-evaluation, and individual wound bed preparation.
FIGURE 2.
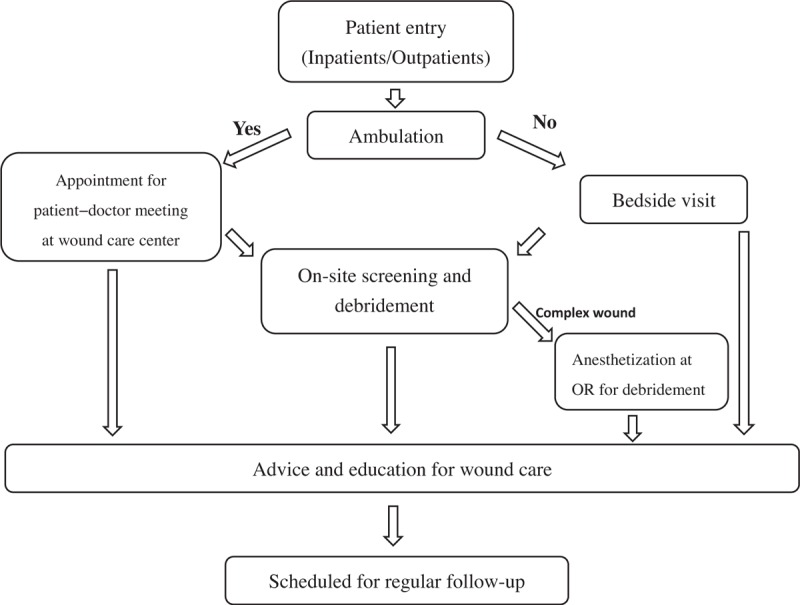
Step 1: patient entry and onsite debridement. After initiation of the wound care service, the physician will meet the patient at the wound care center or bedside. Depending on the patient's wound condition, wound screening, debridement, wound care advice, and education will be provided step-by-step. OR = operation room.
The therapeutic process lags and can be delayed because a chronic wound may need a series of debridement and regular follow-up. The coordinator (nursing staff) also assists the consultant in scheduling follow-up appointments at the center as clinically needed. The wound care center provides not only 1-time wound care, but also a complete program of care including further education and prevention for patients and families.
After being referred and completing the first visit and debridement, the patients proceeded to step 2, wound re-evaluation (Fig. 3). For example, a leg ulcer is evaluated using multiple tools, including neurologic evaluation, vascular evaluation (Ankle–Brachial Index), and the TIME concept (Tissue, Infection/Inflammation, Moisture imbalance and Edge of wound).12 Wound size is measured by the longest length and width of the wound. All individual patient wound profiles are organized into our data bank, which can be analyzed for wound care efficacy and follow-up.
FIGURE 3.
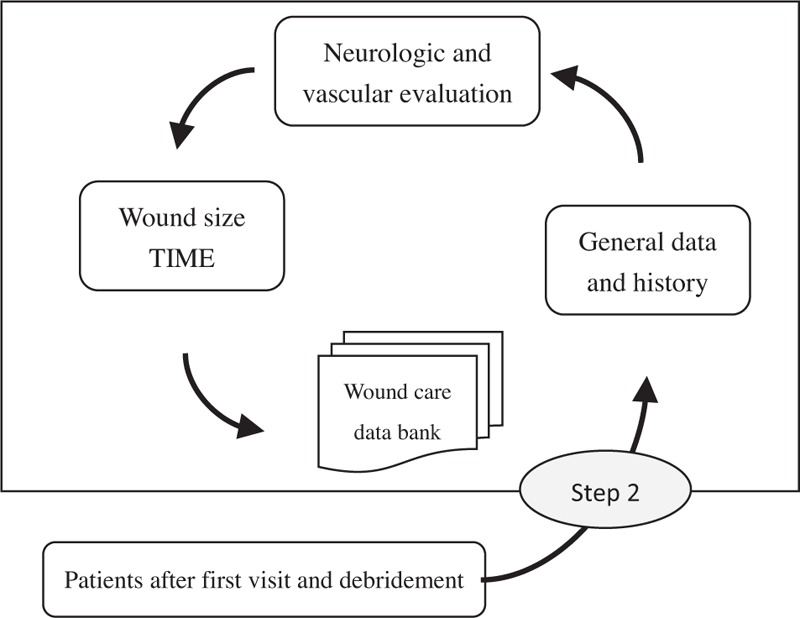
Step 2: wound re-evaluation. After completing the first visit and debridement, patients proceeded to wound re-evaluation, in which the wound is evaluated using multiple tools, including neurologic evaluation and/or vascular evaluation. All individual patient wound profiles are organized into a wound care data bank.
The third step (Fig. 4) includes setting up the individual wound care plan based on the results of wound re-evaluation in step 2. Emphasis is placed on the importance of wound bed preparation (using TIME), early referral between members of the multidisciplinary team, such as the vascular team, hyperbaric oxygenation therapy, further education, and prevention. Offloading must therefore be addressed in a timely manner. There are a number of offloading modalities available for the management of chronic wounds in our multidisciplinary wound care team. Physical and occupational therapists assist the plastic surgeon in handling the offloading issue. The offloading protocol will start after early debridement or at the initial visit for those who need no amputation. The choice of modality will depend on patient-related conditions, for example, concordance with the device, the patient's mobility and their regular activities of daily living, and will be discussed in the regular follow-up out-patient department.
FIGURE 4.
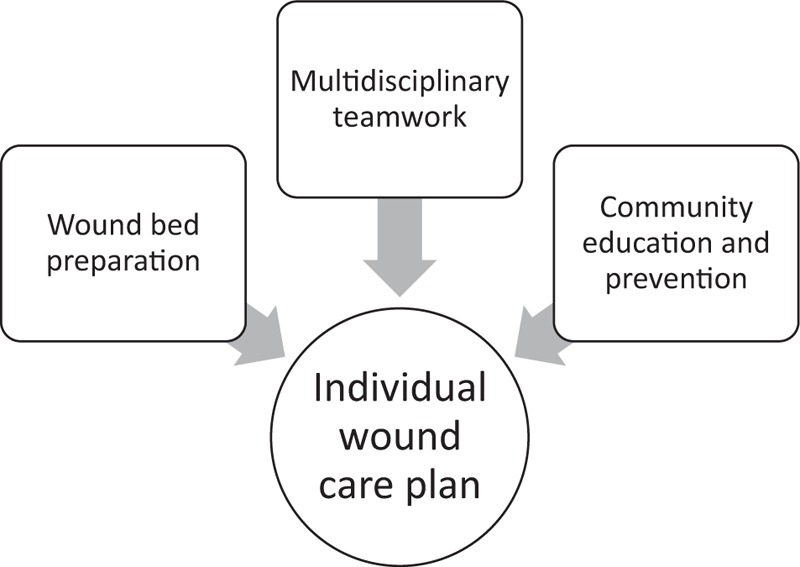
Step 3: individual wound care plan. Based on the results of wound re-evaluation, patients proceeded to an individual wound care plan, in which wound bed preparation, multidisciplinary teamwork, and community education and prevention are provided.
Ethical Approval
This study was approved by the Chang Gung Memorial Hospital–Institutional Review Board (101–3743B).
RESULTS
Type of Wounds
From January 2011 to December 2014, 1103 patients were recruited from wound care management outpatient clinics or inpatient consults. Each patient had regular follow-up for at least 4 months. The most common types of wound encountered were pressure ulcers (45%), followed by diabetic foot ulcers (42%), venous stasis ulcers (7%), and arterial ulcers (6%) (Table 1).
TABLE 1.
Results of Wound Management
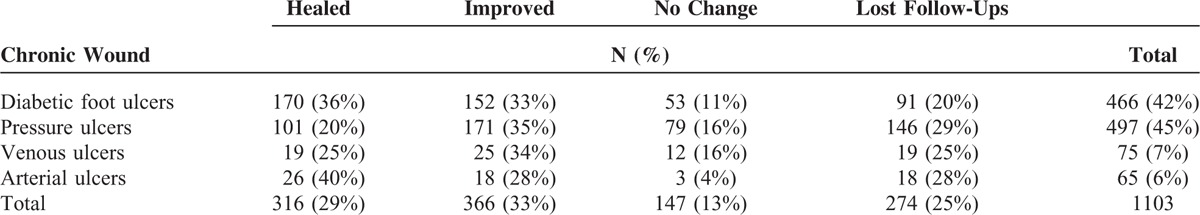
Outcome
After wound care management in our wound care center, 62% of patients achieved significant healing or improvement in wounds, 13% of patients experienced no change, and 25% of patients failed to follow-up. The outcome of wound treatment varied by wound type. Sixty-nine percent (322/466) of diabetic foot ulcer patients were significantly healed or improved. In contrast, pressure ulcers were the least healed wound type, with only 55% (272/497) of patients achieving obviously healed or improved wounds (Table 1). After establishment of a wound care center, we can identify an increased proportion of healed/improved wounds and a decreased proportion of no change/lost follow-up in different wound types from 2011 to 2014 (Fig. 5A–D). Data from 2011 and 2012 were merged because of fewer cases in the first 2 years after the foundation of the wound care center, compared with the most recent 2 years.
FIGURE 5.
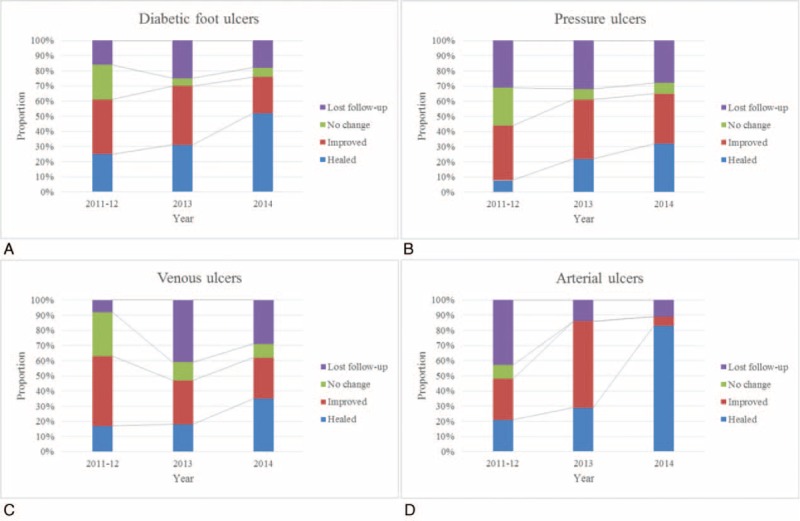
Wound condition from 2011 to 2014. The proportion of healed/improved wounds increased with the decreased proportion of no change/lost follow-up wounds from 2011 to 2014: (a) diabetic foot ulcers; (b) pressure ulcers; (c) venous ulcers; (d) arterial ulcers.
DISCUSSION
Multiple studies have supported the efficacy of protocol-based treatment for pressure ulcers, venous stasis ulcers, and diabetic foot ulcers.13–16 Edwards et al confirmed that the implementation of evidence-based protocols for wound assessment and treatment was significantly related to improved healing outcomes.17 The principle of the wound care protocol is easy to comprehend, but the execution of the clinically efficient wound management service is complicated and needs a standardized and well-integrated multidisciplinary team with specific capacity. The main reason for the difficulty experienced in wound care is a poor referral system, which may be attributed to the inability of the physician to identify and diagnose the wound, patients’ refusal to see the doctor, patients’ refusal to be referred to a wound care center, and the absence of a highly efficient wound care center. The lack of education and routine training for professional wound care and the huge variety of wound care products, procedures, and treatments pose a potential problem for the implementation of wound care as well.
Our wound care center provides a structure to integrate the outpatient clinic, inpatient ward, operation room, rehabilitation center, aesthetic medical center, and other specialized professionals into 1 structure to provide holistic care. There were no conflicts between different departments, which still provided their specialty under a well-integrated referral system. The efficient 3-step wound management path has the advantage that all involved specialists from different departments in the hospital can continue to trace the patient's condition in the same pre-existing unit of the healthcare system.
A few studies have shown improvement of clinical outcomes following the implementation of wound care protocols.18–20 A 6-month review of the outcomes of 115 patients with chronic wounds at the Baystate Medical Center reported healing rates (38%) related to wound etiology with venous ulcers having the most successful healing rates.21 A 7-year study of 2685 chronic wound patients demonstrated 38% of patients with overall wound closure, 9% with significant improvement in wounds, and 45% of patients did not complete the treatment.22 In our data collected over a 4-year period, we achieved higher rates (62%) of wound healing or improvement. Because wound care is a continuous process, wound healing and a better prognosis are more likely to be achieved in a wound with improvement than in 1 with stasis. We observed a trend in the 13% of patients who experienced stasis in their wounds. They tended to have a weaker understanding of wound care at home and poor compliance related to a lack of knowledge. Most of them in this region are fishermen and farmers. Furthermore, we had fewer patients who failed to follow-up. We investigated the reasons for 25% of patients losing follow-up. Many of them changed to other health facilities due to accessibility or long distance. This better compliance can be attributed to our efficient wound management model, which contains active follow-up, education, and prevention. Importantly, we have basically provided an original wound management model, which includes a standardized wound management pathway and an integrated multidisciplinary team combined in a specific wound care center.
Our wound management system provides not only onsite screening, but also real-time wound management with early intervention and instant education for the caregiver. The Team Resources Management (TRM) concept, drawn from Crew (Cockpit) Resource Management originating from a 1979 NASA workshop focused on improving air safety,23,24 has been utilized in our center to pursue better outcomes.25 By applying the TRM concept in our wound care center, we can increase efficient communication and coordination across a multidisciplinary team as well as implement advances in wound assessment and treatment.
In addition to improving the quality of wound care, we hope that the establishment of a wound care center will not only improve patients’ pain and activities of daily life, but also achieve biopsychosocial healthcare, an approach believed to have positive effects on reducing costs and relieving the burden on the healthcare system. We believe that the function of community healthcare centers and patient education, as well as the health practitioner at home, are all relevant factors in the final clinical outcome of the chronic wound patient. But a randomized, controlled study showed the wound center treatment to be more cost-effective and to have better healing rates than home health nursing without protocol.26,27 Although we did not perform an analysis of cost-effectiveness, our wound care center obviously achieved improvement of wound healing and can therefore relieve the burden on both patients’ and caregivers’ daily lives.
We do perform soft tissue reconstructions in our hospital. However, we could see that patients with these chronic wounds are often complicated with underlying systemic diseases. Many of them are either not good candidates for flap reconstructions, or they refuse the possible risks of major reconstructive procedures. No matter whether the team decides on reconstruction procedures or debridement with wound care, the clinical path for efficient wound management service is concordant. Because our team leader is set to be a plastic surgeon, more treatment options can be conducted for our patients on an individualized basis.
Limitations
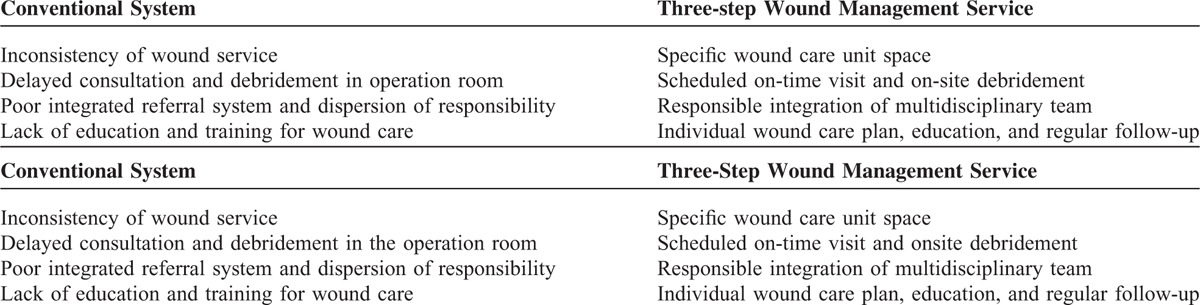
This study has some limitations. First, before the establishment of a wound care center, wound care data were not recorded; hence, we could not compare the efficacy of wound healing between our 3-step wound management service and the conventional system. However, we have identified a trend of increased healing/improvement rates in different types of chronic wound throughout the 4 years after establishment of the wound care center, although a longer follow-up period may be needed. What we provide is responsible, timely wound care in a specific unit. The comparison between wound management service and the conventional system is presented in Table 2. Second, wound healing could be influenced by age, gender, comorbidity, or geographic location, and we did not discuss our patient profiles according to these factors. However, the majority of patients in our study were elderly with comorbidities (Suppl. 1, http://links.lww.com/MD/A496), and 16.04% of population was >65 years in Chiayi, Taiwan.28 The average age of patients with diabetic ulcer was 66.5 years, and the average age of those with pressure ulcer was even higher up to 74.6 years in our population (Suppl. 1). In addition, the provision of wound care service for the elderly is much more challenging than for the younger population due to the accompanying comorbidities or chronic diseases. The administration of such an efficient wound care service to the general population can be predicted to achieve an even and satisfactory wound healing rate. Third, the wound healing processes after wound management, such as time to healing, complications, recurrences, and re-ulceration, were not shown in this study.
TABLE 2.
Comparison of a Wound Management Service and the Conventional System
In the future, we would like to collect more data and perform a retrospective study in a larger population to investigate the effectiveness of wound healing services more specifically. We can use our wound management data bank to analyze predictive factors of wound condition. Beyond disease treatment, the final goal of setting up the wound care center will focus on disease prevention, education, and functional and cosmetic restoration, achieving holistic medical care.
CONCLUSION
We have integrated efficient, standardized multidisciplinary teams in a specific wound care center. Within our wound care center, patients can schedule appointments instead of waiting indefinitely for care. Staff can approach patients in person, administer an adequate wound assessment, and perform timely debridement. Further wound condition follow-up, education, and prevention are also continually provided. By implementing a 3-step wound management service and focusing on prevention and education for wound care, we can achieve biopsychosocial holistic care, which is believed to have a positive effect on relieving the burden on the healthcare system.
Footnotes
Abbreviations: NASA = National Aeronautics and Space Administration, OR = operating room, TIME = tissue infection/inflammation moisture imbalance and edge of wound, TRM = team resources management.
Supplemental Digital Content is available for this article.
Funding: this study was funded by Chang Gung Medical Research Program G6C0191 and G6C0192.
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Heinen MM, van Achterberg T, op Reimer WS, et al. Venous leg ulcer patients: a review of the literature on lifestyle and pain-related interventions. J Clin Nurs 2004; 13:355–366. [DOI] [PubMed] [Google Scholar]
- 2.Moffatt C, Price P, Morgan P. Meeting the psychosocial challenges of leg ulceration. Nurs Times 2006; 102:51–53. [PubMed] [Google Scholar]
- 3.Jones J, Barr W, Robinson J, et al. Depression in patients with chronic venous ulceration. Br J Nurs 2006; 15 (11 Suppl):17.S-23 S. [DOI] [PubMed] [Google Scholar]
- 4.Phillips T, Stanton B, Provan A, et al. A study of the impact of leg ulcers on quality of life: financial, social and psychological implications. J Am Acad Dermatol 1994; 31:49–53. [DOI] [PubMed] [Google Scholar]
- 5.O’Meara S, Cullum N, Nelson E. Compression for venous leg ulcers. Cochrane Database Syst Rev 2012; 11:CD000265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fife C, Carter MJ, Walker D. Why is it so hard to do the right thing in wound care? Wound Repair Regen 2010; 18:154–158. [DOI] [PubMed] [Google Scholar]
- 7.Coyer F, Edwards H, Courtney M. Best Practice Community Care for Clients with Chronic Venous Leg Ulcers: National Institute for Clinical Studies (NICS) Report for Phase I Evidence Uptake Network. Queensland University of Technology. http://eprints.qut.edu.au. Published 2005 Accessed February 10, 2015. [Google Scholar]
- 8.Olmsted MG, Geisen E, Murphy J, Bell D, Morley M, Stanley M. Methodology: U.S. News & World Report, Best Hospitals 2014–15. U.S. News & World Report Web site. http://www.usnews.com/pubfiles/BH_2014_Methodology_Report_Final_Jul14.pdf. Published July 14, 2014 Accessed February 10, 2015. [Google Scholar]
- 9.Doan-Johnson S. The growing influence of wound care teams. Editorial. Adv Skin Wound Care 1998; 11:54. [PubMed] [Google Scholar]
- 10.Steed DL, Edington H, Moosa HH, et al. Organization and development of a university multidisciplinary wound care clinic. Surgery 1993; 114:775-778.discussion 778-779. [PubMed] [Google Scholar]
- 11.Jaramillo O, Elizondo J, Jones P, et al. Practical guidelines for developing a hospital-based wound and ostomy clinic. Wounds 1997; 9:94–102. [PubMed] [Google Scholar]
- 12.Chin GA, Schultz G, Stacey M. Principles of wound bed preparation and their application to the treatment of chronic wounds. Wound Practice Res 2004; 11:171–174. [Google Scholar]
- 13.Bond TK. Consistency in prevention & treatment of pressure ulcers through a wound care team. Nurse Case Manage 1997; 2:203–218. [PubMed] [Google Scholar]
- 14.Coerper S, Wicke C, Pfeffer F, et al. Documentation of 7051 chronic wounds using a new computerized system within a network of wound care centers. Arch Surg 2004; 139:251–258. [DOI] [PubMed] [Google Scholar]
- 15.Kjaer ML, Sorensen LT, Karlsmark T, et al. Evaluation of the quality of venous leg ulcer care given in a multidisciplinary specialist centre. J Wound Care 2005; 14:145–150. [DOI] [PubMed] [Google Scholar]
- 16.Frykberg RG. The team approach in diabetic foot management. Adv Skin Wound Care 1998; 71–77. [PubMed] [Google Scholar]
- 17.Edwards H, Finlayson K, Courtney M, et al. Health service pathways for patients with chronic leg ulcers: identifying effective pathways for facilitation of evidence based wound care. BMC Health Serv Res 2013; 13:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrison MB, Graham ID, Lorimer K, et al. Nurse clinic versus home delivery of evidence-based community leg ulcer care: A randomized health services trial. BMC Health Serv Res 2008; 8:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McGuckin M, Williams L, Brooks J, et al. Guidelines in practice: the effect on healing of venous leg ulcers. Adv Skin Wound Care 2001; 14:33–36. [DOI] [PubMed] [Google Scholar]
- 20.Moffatt CJ, Franks PJ. Implementation of a leg ulcer strategy. Br J Dermatol 2004; 151:857–867. [DOI] [PubMed] [Google Scholar]
- 21.Granowitz EV, Szostek R, Burns P, et al. Aetiologies and outcomes of wounds in an outpatient programme. J Wound Care 1998; 7:378–380. [PubMed] [Google Scholar]
- 22.Sholar AD, Wong LK, Culpepper JW. The Specialized Wound Care Center: a 7-year experience at a tertiary care hospital. Ann Plast Surg 2007; 58:279–284. [DOI] [PubMed] [Google Scholar]
- 23.Cooper GE, White MD, Lauber JK. Resource Management on the Flightdeck: Proceedings of a NASA/Industry Workshop. (NASA CP-2120). NASA Ames Research Center. http://ntrs.nasa.gov/archive/nasa/casi.ntrs.nasa.gov/19800013796.pdf. Published March, 1980 Accessed February 10, 2015. [Google Scholar]
- 24.Musson DM, Helmreich RL. Team training and resource management in health care: current issues and future directions. Harvard Health Policy Rev 2004; 5:25–35. [Google Scholar]
- 25.Neily J, Mills PD, Young-Xu Y, et al. Association between implementation of a medical team training program and surgical mortality. JAMA 2010; 304:1693–1700. [DOI] [PubMed] [Google Scholar]
- 26.Morrell CJ, Walters SJ, Dixon S, et al. Cost effectiveness of community leg ulcer clinics: randomised controlled trial. BMJ 1998; 1487–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Apelqvist J, Ragnarson-Tennvall G, Persson U, et al. Diabetic foot ulcers in a multidisciplinary setting: an economic analysis of primary healing and healing with amputation. J Intern Med 1994; 235:463–471. [DOI] [PubMed] [Google Scholar]
- 28.Report of Population Age Distribution by Counties. Department of Statistics, Ministry of the Interior, Taiwan: http://www.moi.gov.tw/files/news_file/week10429.pdf Published January 17, 2015 Accessed February 10, 2015. [Google Scholar]


