Highlights
-
•
On rare occasions, apparently spontaneous regression of unknown etiology is observed in a neoplasm.
-
•
We report a series of 4 patients with apparent spontaneous regression of malignant neoplasms after radiography.
-
•
Apparently spontaneous regression of these malignant lymphomas and cancers was caused by the small radiation doses received in the radiographic examinations.
Keywords: Spontaneous regression, Malignant lymphoma, Cancer, Radiography, Case report
Abstract
Introduction
On rare occasions, an apparently spontaneous regression of unknown etiology is observed in a neoplasm. We report a series of 4 patients with apparent spontaneous regression of malignant lymphomas after radiography.
Presentation of case
All four of the tumors were malignant lymphomas. The regressions occurred between 1 and 2 months after the radiographic examinations. All four patients later underwent relapse and needed additional treatments: surgery, chemotherapy and/or radiation.
Discusssion
Four cases had the following features in common: (1) the neoplasms were radiosensitive, (2) the regression occurred after radiography, (3) none of the neoplasms was in the advanced stage, and (4) the doses received through radiographic exposure were a little higher than usual because CT was included for most of the patients.
Conclusion
We suspect that the apparently spontaneous regression of malignant lymphomas was caused by the small radiation doses received in the radiographic examinations.
1. Introduction
In very rare cases, the seemingly unprompted healing of malignant lymphoma or cancer has been observed. This kind of regression of a neoplasm without treatment is generally defined as complete or incomplete, as general or local, and as temporary or permanent. The cause of this apparently unprompted process is as yet unknown. Four malignant lymphoma patients were seen in our clinic; this phenomenon had occurred in each of them, in each case after radiography. The relationship between the apparently spontaneous regression and the radiography that had been performed was investigated, and the literature was examined for comparable cases.
2. Presentation of case
Four patients exhibiting apparently spontaneous regression of their cases were seen in our clinic between 1972 and 2015. They were investigated clinically and histologically, and the types of malignant lymphoma found were categorized according to the World Health Organization (WHO) classification. The normal ranges of the antibodies are given in below parentheses. Levels of anti-thyroglobulin antibody (TgAb; <0.3 U/ml), and anti-thyroid peroxidase antibody (TPOAb; <0.3 U/ml) were determined with RIA kits (Cosmic Corporation, Tokyo, Japan).
2.1. Patient 1
A 69-year-old woman noticed a tumor in the front of her neck 2 weeks before she visiting our clinic. The tumor grew rapidly. The left lobe of the thyroid was hard and was enlarged to 3 × 5 cm, and it exhibited the following characteristics: a smooth surface, with a silhouette defect appearing in the 131I scintigram; a solid homogenous low-density area in the ultrasound; and a low-density area in the CT. Two adjacent, enlarged lymph nodes were palpated. Thyroid cancer with lymph node metastases was suspected, but a fine needle aspiration biopsy (FNAB) revealed no cancer cells. Many radiographic procedures (e.g., chest X-rays, soft X-rays, and tracheal tomography, etc.) were performed to obtain more information about the tumor, but nothing further was discovered. These findings still suggested that the tumor was a malignant thyroid lymphoma (Fig. 1A). Two months later, the tumor shrank to about half of its original size, which was unexpected (Fig. 1B). Some connection was suspected between the tumor’s shrinkage and the large number of radiographic examination. Regular radiotherapy sessions were recommended as additional treatment, but the radiologist refused to perform such procedures because the core biopsy diagnosis was Hashimoto’s disease. After another month, the tumor had grown again, reaching approximately its former maximum size. A left hemithyroidectomy with dissection of the cervical lymph nodes was performed. The thyroid was observed to adhere to the surrounding tissues while it was being removed. Histological examination revealed a medium-sized diffuse malignant B cell lymphoma with lymph node metastases. Fibrosis, perhaps a result of the radiation, was found in this lymphoma. Forty gray (Gy) of postoperative radiation was administered. Twenty-one years later, as this report is being written, the patient is healthy and has not suffered any recurrences.
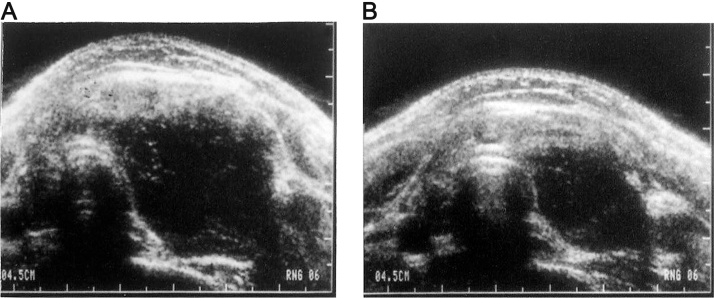
Fig. 1.
Clinical course of patient 1. (A) This nodule appears as a solid, low-echoic mass in the ultrasound images. (B) 2 months later, the nodule was reduced in size by half. Malignant lymphoma was suspected.
2.2. Patient 2
An 83-year-old woman noticed a tumor in the front of her neck. It was found to be a hard 2.5 × 3.0 cm nodule located in the right thyroid lobe. Anti-thyroid antibodies were present (TGAb, RIA, 32.2 U/ml; TPOAb, RIA, 63.1 U/ml). CT revealed a slightly heterogeneous solid tumor in the right thyroid lobe. A 201Tl scintigram showed no silhouette defect. Thyroid cancer combined with Hashimoto’s disease was suspected, but an FNAB detected no cancer cells, so no treatment was given. Unexpectedly, the tumor had disappeared one month after the first visit, and the patient therefore thought the lesion had healed. Another 8 months later, however, the tumor reappeared, so the patient returned to our clinic. The right thyroid lobe was hard and smooth, and had grown to 3 × 5 cm in size. The second FNAB diagnosis was of non-Hodgkin lymphoma or small-cell carcinoma. The serum was positive for soluble IL-2 receptor antibody (701 U/ml, normal range: 191–650 U/ml). A final diagnosis of malignant lymphoma of the thyroid was made. One month after a total of 40 Gy of X-ray treatment, the tumor had disappeared. The patient died naturally nine years later, at the age of 89, with no tumor recurrence.
2.3. Patient 3
A 51-year-old woman came to our clinic, one day after she noticed a tumor on the front of her neck. The left lobe of the thyroid was hard and smooth and had become enlarged to 5 × 8 cm. A malignant thyroid lymphoma was suspected, but the FNAB diagnosis was class II. A thyroid adenoma was diagnosed. The nodule was very large and was located inferiorly, so CT was carried out to confirm the extent of the goiter; the CT showed that the goiter was situated partially intrathoracically. Because of the nodule’s size, surgery was recommended, but it had unexpectedly shrunk and had disappeared 2 months after the CT, so the patient thought it was completely healed and deemed surgery unnecessary. However, the lesion reappeared 7 months after the CT, (i.e., 5 months after the tumor disappeared), so she returned to our clinic when it had regrown and had become slightly larger than its original size. A second FNAB revealed a potentially malignant lymphoma. A total thyroidectomy was performed 7 months after the first visit. The histological diagnosis was malignant diffuse large-cell lymphoma. A fibrosis, possibly a consequence of the X-ray radiation, was found by microscopy. Postoperative chemotherapy (6 courses of R-THP-COP) was given. Now, 8 years after the operation, the patient is well, with no recurrence of the tumor.
2.4. Patient 4
A 60-year-old man noticed a fist-sized hard fixed tumor in the ileocecal region, where it was found to have caused an incomplete obstruction of the intestine. He was admitted to a nearby hospital. Ten plain abdominal X-ray examinations were performed, and ileocecal cancer was at first suspected. Upon instillation of barium through a Denis tube performed concurrently with a barium enema, a slight narrowing of the ileum due to the presence of the tumor was seen, but no shadow defect and no “apple core” sign were detected. Superior mesenteric arteriography revealed no vascular connection between the tumor and the intestine. The tumor had shrunk and disappeared one month later, but the subileus remained. Laparotomy was therefore performed, and it revealed a hemispherical tumor that was 3 cm thick, hard, and fixed to both the retroperitoneum and the intestine. The tumor was unresectable, and so ileo-colostomy was carried out. Biopsy of the tumor revealed a malignant lymphoma. The patient was reported later to have died as a result of tumor recurrence.
3. Discussion
The cause of the apparently spontaneous regression of certain neoplasms is unknown. These 4 cases suggest, however, that the small doses of radiation used in radiographic procedures may be capable of reducing the number and size of these neoplasms. Four cases had the following features in common (Table 1): (1) the neoplasms were radiosensitive, (2) the regression occurred after radiography, (3) none of the neoplasms was in the advanced stage, and (4) the doses received through radiographic exposure were a little higher than usual because CT was included for most of the patients. Because most of the regressions were temporary, and were visible only for limited periods, observation of the regression was possible only at certain times. These facts suggest that because the malignant lymphomas were radiosensitive, they were reduced in size by the small-dose radiation of the radiographic procedures themselves. It is well known, and well supported by the literature, that apparently spontaneous regression is somewhat common in cases of malignant lymphoma. Gattika et al. [1] reported that spontaneous regression apparently occurred in 9.6% of a total of 209 malignant lymphoma patients (nodular type 18/140 = 12.9%, diffuse type 2/69 = 2.9%). Horning et al. [2] reported that apparently spontaneous regression occurred in 19 (23%) of a total of 83 patients with malignant lymphoma. Accounts of another 62 cases in which the apparently spontaneous regression of malignant lymphoma occurred have stated that diagnostic radiography was performed in a total of 56 patients. These 62 case reports were made by a total of 24 authors (with the exception of 5 cases that were reported by three other authors) [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]. In the first group of these reports, the dates of radiography and regression in 30 patients were given. Regression after the radiography had occurred in each of these 30 patients.
Table 1.
Clinical course of the 4 patients whose malignant neoplasms regressed after radiography.
| Patient No., Age Gender | Diagnosis | Type of radiography |
Time between radiography and regression |
Duration of regression |
Additional treatment |
Outcome |
|---|---|---|---|---|---|---|
| 1. 69 yrs Female | Malignant thyroid lymphoma | CT, 131I scintigram, soft X-ray, tracheotomography | 2 months | 1 month | Hemithyroidectomy, 40 Gy radiation | Healthy 22 yrs. later |
| 2. 83 yrs Female |
Malignant thyroid lymphoma |
CT, 201Tl scintigram, soft X-ray | 1 month | 8 months | 40 Gy radiation | Died at an advanced age 9 yrs. later |
| 3. 51 yrs Female |
Malignant thyroid lymphoma |
CT | 2 months | 4 months | Total thyroidectomy | Healthy 8 yrs. later |
| 4. 50 yrs Male |
Malignant retroperitoneal lymphoma | Plain abdominal X-P, mesenteric arterio-graphy, barium enema, barium enterography | 1 months | Unknown | Ileo-colostomy for ileus | Died after relapse |
Because malignant lymphoma is known to be an extremely radiosensitive neoplasm, it is possible that even the small radiation dose resulting from a radiographic procedure could have caused the tumor regression. It is quite possible that the radiation doses used for some malignant lymphomas were strong enough to terminate the malignant process completely or to redirect it into a lasting regression, as in the case of Matsuo’s patients [13]. Matsuo et al. reported on 13 patients with malignant conjunctival lymphoma. Seven of these tumors underwent an apparently spontaneous regression. There was no recurrence in these 7 patients in the first 11 years after diagnosis, during which time gallium scintigraphy and MRI were performed. Thus, it is possible that the tumor reduction in the 7 patients was caused by the small-dose radiation of gallium scintigraphy and MRI. If the radiation dose is not enough to destroy the tumor completely, a relapse may occur, as it did in patients 1, 2 and 3, or the patient may die. In the cases in the literature, 10 authors reported on 14 patients (22.6%) out of a total of 62 patients with malignant lymphoma who subsequently relapsed or died after a temporary regression [3], [5], [6], [7], [14], [18], [25], [26], [27]. Heterogeneous regression of multiple malignant lymphoma has sometimes been observed in a clinical setting. We, however, have not yet encountered such a case. Krikorian et al. [10] diagnosed 44 patients with nodal malignant lymphoma, 9 of whom had experienced regressions after several radiological examinations. In six out of these 9 patients, heterogeneous regression occurred. In patient 3, for example, only the hilar and pelvic lymph node swellings regressed after a chest X-ray, a lung tomogram, a pelvic lymphogram and an intravenous pyelogram were performed. These findings suggested that small-dose radiation to localized areas as a result of radiographic examinations could have caused the heterogeneous regression. These unexpected clinical course due to apparent spontaneous regression undercut the diagnosis and delayed the final treatment. Everson and Cole’s 1966 textbook [27], titled Spontaneous Regression of Cancer, provides the most extensive documentation of apparently spontaneous regressions to date; it describes 219 cases. Of these 219 patients, 153 underwent radiological examinations, and the regressions all occurred after the radiography. Only one thyroid cancer case was treated successfully by Portine in 1958, an account of which appears in Spontaneous Regression of Cancer. This case suggested that the patient was suffering from an undifferentiated cancer that was known to be radiosensitive. Although the patient had been in the final stage of the disease, he recovered completely. It is therefore considered likely that the X-ray examination itself brought about the healing of the malignancy, because no treatment was administered. Regrettably, the spontaneous regression of malignant lymphoma is not included in Everson and Cole’s collection of cases; this is because WHO had not yet established the malignancy grades of the disease in 1966. As stated by Everson and Cole, the frequency of spontaneous regression of cancer is extremely low in comparison with that of malignant lymphoma. As stated in Rae’s report [28], Bashford estimated that such a regression occurs in only one out of around 10 million cases of malignant neoplasms. Boyers estimated the ratio to be one in about 8 million cases. It is therefore likely that the frequency of extremely radiosensitive cancer—that is, cancer that can be caused to regress by the small-dose radiation stemming from radiographic procedures—is extremely rare [29].
Ono’s case of a germinoma of the pineal body that regressed after repeated radiographies led the author to speculate that the tumor was hypersensitive to X-ray irradiation and, that the marked regression was caused by cumulative diagnostic irradiation [30]. We agree with this speculation.
4. Comments
This study examined four cases of apparently spontaneous regression of malignant lymphomas. Malignant lymphoma is known to be a highly radiation-sensitive neoplasm. The regressions always followed radiological examinations, as has been reported in the other studies. Most of the tumors documented in the literature were radiation-sensitive malignant neoplasms. The spontaneous regression of malignant lymphoma is widely known to be somewhat common, and the accounts presented in this report suggest that one of the causes of the apparently spontaneous regression of malignant lymphomas is the small-dose radiation administered for diagnostic radiography.
Conflict of interests
None.
Funding
None.
Ethical approval
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author’s contributions
All authors conceived the study and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Guarantor
Akira Sasaki.
Acknowledgement
We thank Reynolds CWP, Department of International Medical Communications, Tokyo Medical University, for editing the manuscript.
Contributor Information
Jun Sasaki, Email: junshuku@zoo.email.ne.jp.
Hideo Kurihara, Email: kclinic@rnac.ne.jp.
Yoshishige Nakano, Email: sakira@iwate-med.ac.jp.
Kohji Kotani, Email: sakirasimu@gmail.com.
Eisuke Tame, Email: komaki-hosp@med-junseikai.or.jp.
Akira Sasaki, Email: sakira.iwate.med.u@gmail.com.
References
- 1.Gattiker H.H., Wiltshaw E., Galton D.A.G. Spontaneous regression in non-Hodgkin’s lymphoma. Cancer. 1980;45:2627–2632. doi: 10.1002/1097-0142(19800515)45:10<2627::aid-cncr2820451023>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 2.Horning S.J., Rosenberg S.A. The natural history of initially untreated low-grade non-Hodgkin’s lymphomas. N. Engl. J. Med. 1984;311:1471–1475. doi: 10.1056/NEJM198412063112303. [DOI] [PubMed] [Google Scholar]
- 3.Blokx W.A.M. Initial spontaneous remission of posttransplantation Epstein-Barr virus-related B-cell lymph proliferative disorder of the skin in a renal transplant recipient. Am. J. Dermatol. 2002;24:414–422. doi: 10.1097/00000372-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Grem J.L., Hafez G.R., Brandenburg J.H., Carbone P.P. Spontaneous remission in diffuse large cell lymphoma. Cancer. 1986;57:2042–2044. doi: 10.1002/1097-0142(19860515)57:10<2042::aid-cncr2820571027>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 5.Heibel H., Knodgen R., Bredenfeld H., Wickenhauser C., Scheer M., Zoller J.E. Complete spontaneous remission of an aggressive non-Hodgkin’s lymphoma with primary manifestation in the oral cavity. Leukemia Lymphoma. 2004;45:171–174. doi: 10.1080/1042819031000139747. [DOI] [PubMed] [Google Scholar]
- 6.Jinnohara T., Tsujisaki M., Sasaki S., Hinoda Y., Imai K. Cytotoxic activity in a case of adult T-cell leukemia/lymphoma with spontaneous regression. Int. J. Hematol. 1997;65:293–298. doi: 10.1016/s0925-5710(96)00564-6. [DOI] [PubMed] [Google Scholar]
- 7.Kashiwabara K., Nakamura H., Kusama H., Kishi K., Yagyu H., Takagi S. Ki-1(CD30)-positive anaplastic large cell lymphoma sarcomatoid variant accompanied by spontaneous regressing lymphadenopathy. Int. Med. 1999;38:49–53. doi: 10.2169/internalmedicine.38.49. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi O., Ohno K., Nagai K., Abe A., Murakawa E., Ueno M. Primary malignant lymphoma of the lung (low-grade B-cell lymphoma of MALT type) occurring in a patient with bronchiolitis obliterans organizing pneumonia. Acta Med. Biol. 1996;44:163–168. [Google Scholar]
- 9.Kon T., Kakita A., Koide A., Mori H., Tanaka R., Takahashi H. A primary CNS lymphoma in spontaneous remission for 3.5 years after initial detection of the lesions by MRI. Brain Tumor Pathol. 2003;20:27–31. doi: 10.1007/BF02478944. [DOI] [PubMed] [Google Scholar]
- 10.Krikorian J.G., Portlock C.S., Cooney D.P., Rosenberg S.A. Spontaneous regression of non-Hodgkin’s lymphoma: a report of nine cases. Cancer. 1980;46:2093–2099. doi: 10.1002/1097-0142(19801101)46:9<2093::aid-cncr2820460931>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 11.Kumamoto M., Nakamine H., Hara T., Yokoya Y., Kawai J., Ito H. Spontaneous complete regression of high grade non-Hodgkin’s lymphoma. Cancer. 1994;74:3023–3028. doi: 10.1002/1097-0142(19941201)74:11<3023::aid-cncr2820741120>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 12.Lan C.E., Yu H., Chen S., Chen G. Relapsing ulcerative papules over bilateral hands and scrotum in an Asian man: an atypical manifestation of primary cutaneous CD 30-positive lymphoma. J. Dermatol. 2003;30:230–235. doi: 10.1111/j.1346-8138.2003.tb00377.x. [DOI] [PubMed] [Google Scholar]
- 13.Matsuo T., Yoshino T. Long-term follow-up results of observation or radiation for conjunctival malignant lymphoma. Ophthalmology. 2004;111:1233–1237. doi: 10.1016/j.ophtha.2003.09.049. [DOI] [PubMed] [Google Scholar]
- 14.Murase T., Inagaki H., Okabe M., Eimoto T. Nasal natural killer (NK)/T-cell lymphoma showing spontaneous regression and relapse in the uterine cervix. Pathol. Int. 2000;50(Suppl. A) 53. [Google Scholar]
- 15.Notani K., Shindoh M., Takami T., Yamazaki Y., Kohgo T., Fukuda H. Anaplastic large cell lymphoma (ALCL) in the oral mucosa with repeating recurrence and spontaneous regression of ulceration: report of a case. Oral Med. Pathol. 2002;7:79–82. [Google Scholar]
- 16.Ogata M., Kikuchi H., Ono K., Otsuka E., Gamachi A., Kashima K. Spontaneous remission of Epstein-Barr virus-negative non-Hodgkin’s lymphoma after withdrawal of cyclosporine in a patient with refractory anemia. Int. J. Hematol. 2004;79:161–164. doi: 10.1532/ijh97.03095. [DOI] [PubMed] [Google Scholar]
- 17.Ohgi S., Ehara S., Sato T., Kato S., Shimosegawa K., Ishida Y. Spontaneous regression of malignant lymphoma of the lumbar spine. Skelet. Radiol. 2002;31:99–102. doi: 10.1007/s00256-001-0446-z. [DOI] [PubMed] [Google Scholar]
- 18.Partap S., Spence A.M. Spontaneously relapsing and remitting primary CNS lymphoma in an immunocompetent 45-year-old man. J. Neurooncol. 2006;80:305–307. doi: 10.1007/s11060-006-9192-3. [DOI] [PubMed] [Google Scholar]
- 19.Poppema S., Postma L., Brinker M., Jong B. Spontaneous regression of a small non-cleaved-cell malignant lymphoma (non-Burkitt’s lymphoblastic lymphoma): morphologic, immunohistochemical and immunoglobulin gene analysis. Cancer. 1988;62:791–794. doi: 10.1002/1097-0142(19880815)62:4<791::aid-cncr2820620425>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 20.Shigematsu A., Iida M., Lien G.S., Imamura T., Okada M., Fuchigami T. Spontaneous regression of primary malignant lymphoma of the stomach in two nontreated Japanese. J. Clin. Gastroenterol. 1989;11:511–517. doi: 10.1097/00004836-198910000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Strauchen J.A., Moran C., Goldsmith M., Greenberg M. Spontaneous regression of gastric lymphoma. Cancer. 1987;60:1872–1875. doi: 10.1002/1097-0142(19871015)60:8<1872::aid-cncr2820600833>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 22.Takenaka R., Tomoda J., Sakata T., Ichiba T., Motoi M., Mizuno M. Mucosa-associated lymphoid tissue lymphoma of the rectum that regressed spontaneously. J. Gastroenterol. Hepatol. 2000;15:331–335. doi: 10.1046/j.1440-1746.2000.02086.x. [DOI] [PubMed] [Google Scholar]
- 23.Tietjen G.W., McAllister F.F. Spontaneous regression of gastric reticulum-cell sarcoma. N. Y. State J. Med. 1974;74:680–683. [PubMed] [Google Scholar]
- 24.Watari J., Saitoh Y., Fujiya M., Nakamura K., Inaba Y., Okamoto K. Spontaneous remission of primary diffuse large B-cell gastric lymphoma. Gastroenterology. 2005;40:414–420. doi: 10.1007/s00535-004-1561-0. [DOI] [PubMed] [Google Scholar]
- 25.Weingarten K.L., Zimmerman R.D., Leeds N.E. Spontaneous regression of intracerebral lymphoma. Radiology. 1983;149:721–724. doi: 10.1148/radiology.149.3.6359262. [DOI] [PubMed] [Google Scholar]
- 26.Yasunaga T., Takahashi H., Uozumi H., Takada S., Kawano Y., Baba Y. Radiation therapy of primary malignant lymphoma of the brain. Acta Radiol. Oncol. 1986;25:23–28. doi: 10.3109/02841868609136372. [DOI] [PubMed] [Google Scholar]
- 27.Everson T.C., Cole W.H. W.B. Philadelphia and London: Saunders Co.; 1966. Spontaneous Regression of Cancer; pp. 1–529. [Google Scholar]
- 28.Rae M.V. Spontaneous regression of a hypernephroma. Am. J. Cancer. 1935;24:839–841. [Google Scholar]
- 29.Boyers L.M. Self-examination of the breasts. JAMA. 1953;152:986. [Google Scholar]
- 30.Ono H., Shin M., Takai K., Oya S., Mukasa A., Saito N. Spontaneous regression of germinoma in the pineal region before endoscopy for pineal germ cell tumors. J. Neurooncol. 2011;103:755–758. doi: 10.1007/s11060-010-0432-1. [DOI] [PubMed] [Google Scholar]