Abstract
Objectives
Prior studies have observed a high prevalence of psychosocial distress, including depression, in patients with voice problems. However, these studies have largely been performed in care-seeking patients identified in tertiary care voice clinics. The objective of this study was to examine the association between depression and voice problems in the United States population.
Study Design
Cross-sectional analysis of National Health Interview Survey (NHIS) data.
Methods
We identified adult cases reporting a voice problem in the preceding 12 months in the 2012 NHIS. Self-reported demographics and data regarding healthcare visits for voice problems, diagnoses given, severity of the voice problem, and depression symptoms were analyzed.
Results
The total weighted sample size was 52,816,364. The presence of depressive symptoms was associated with a nearly two-fold increase (OR=1.89, 95% CI=1.21-2.96) in the likelihood of reporting a voice problem in the past year. Patients who reported feeling depressed were less likely to receive care for the voice problem, and less likely to report that treatment had helped, than those who did not feel depressed.
Conclusions
These findings indicate that the co-occurrence of voice problems and depressive symptoms is observed in the general population, not only in care-seeking patients, and that depressive symptoms may influence reported likelihood of receiving voice treatment and effectiveness. This suggests that voice care providers should take mental health symptoms into account when treating patients, and also indicates a need for further investigation.
Level of Evidence
NA
Keywords: voice problems, dysphonia, depression, population-based, NHIS
INTRODUCTION
Voice disorders are common, with a lifetime prevalence of 29%,1 and costly, with an annual estimated $2B US cost in lost work productivity.2 Among patients who seek care at specialty voice centers, psychosocial distress (e.g., depression, anxiety) is prevalent and severe.3-8 However, it is unknown whether this association is limited to care-seeking adults.
Using data from the National Health Interview Survey (NHIS), which reports information about the health of the civilian non-institutionalized US general population, Bhattacharyya reported in 2014 that only 10% of patients who reported a voice problem in the prior year sought care for that voice problem.9 This indicates that studies completed in the care-seeking population may not accurately represent the status of those who have a voice problem but have not sought or received care. We therefore utilized data from the 2012 NHIS survey, which included a supplement asking about adult voice disorders as well as questions about mental health symptoms, to determine whether the association between mental health symptoms and voice problems was observed in the US population.
Based on previous studies in care-seeking populations, we hypothesized that a concurrent report of depression symptoms would be more common in those reporting a voice problem in the past year than in those reporting no voice problems in the past year. We also hypothesized that concurrent self-reported depression and voice symptoms would be associated with differences in treatment-seeking behaviors and treatment effectiveness compared to those without depression symptoms.
METHODS
Data Source and Sample
We utilized a population-based cross-sectional analysis of national survey data for adults (18-85) in the US using the National Health Interview Survey. In the 2012 cycle of the NHIS, a supplement was contained within the survey specifically pertaining to adult voice, speech, and language disorders, with specific questions related to voice problems. The NHIS also includes questions about depression in the Quality of Life supplement (administered to approximately a quarter of sample adults). The NHIS data were obtained from the Integrated Health Interview Series (IHIS), a web-based data resource containing NHIS data.10,11 The complex, multistage probability sampling used by NHIS incorporates stratification, clustering, and oversampling of some racial subpopulations (Black, Hispanic, and Asian). In order to account for this complex sample design the NHIS provides sampling weights to produce representative estimates of a total weighted sample.12 The unweighted sample size for this study was 7,708 persons, representing a total weighted sample of 52,816,364. Because these data are available to the public in a de-identified format, this study was exempt from Institutional Review Board review.
Measures
The outcome of interest for this study was depression within a representative sample of the US population with voice problems. We used responses to the question, “During the past 12 months, have you had any problems or difficulties with your voice?” to identify NHIS respondents who reported having a voice problem or difficulties with voice in the past year. The question solicited information on problems such as hoarseness, raspy, or strained voice, or difficulty speaking loud enough to be heard. We assigned the IHIS variable “Voice problem past 12 months” a binary response, with Yes indicating the response, “Yes, I have a voice problem,” and No indicating the response “No, I do not have a voice problem.”
We used responses to the question “How often do you feel depressed?” to identify survey participants who reported feeling depressed. We created a binary depression variable and coded responses “Yes, I am depressed” (daily, weekly, monthly, a few times a year) as positive and negative for the response “No, I am not depressed (never).” It is important to note that this was based on self-report, not a formal DSM-IV diagnosis. To avoid introducing bias related to our own opinions about what frequency of depression symptoms would be meaningful, and because the question did not specify duration or severity of depression symptoms, we were inclusive in defining this depression symptoms variable. Symptom scale measures were not available for this sample.
Additional covariates were defined as follows. For race, we used a set of indicator variables for self-reported non-Hispanic Asian; non-Hispanic American Indian/Alaskan Native; non-Hispanic Black; Hispanic; and non-Hispanic White. We divided age and educational attainment into categories shown in Table 1. Finally, we defined poverty levels using the NHIS income variable,13,14 categorizing respondents as less than or equal 100 percent of the Federal Poverty Level (FPL), 101–199 percent FPL, 200-399 percent FPL, and 400 percent or more of the FPL.
Table 1.
Selected characteristics of the US civilian, non-institutionalized populations and voice problem past 12 months, 2012 NHIS
| Voice Problem | ||||
|---|---|---|---|---|
| Yes (%) | No (%) | SE | p value | |
| Gender | 0.001 | |||
| Male | 38 | 49 | 0.42 | |
| Female | 62 | 51 | 0.47 | |
| Age Categories | <.0001 | |||
| 18-30 | 25 | 24 | 0.63 | |
| 31-45 | 24 | 27 | 0.68 | |
| 46-65 | 32 | 35 | 1.16 | |
| 65+ | 19 | 14 | 0.14 | |
| Race | <.0001 | |||
| White Non-Hispanic | 74 | 67 | 1.49 | |
| Black Non-Hispanic | 12 | 11 | 1.13 | |
| Non-Hispanic American Indian/Alaskan Native & other | 3 | 2 | 0.11 | |
| Asian Non-Hispanic | 4 | 5 | 0.27 | |
| Hispanic | 7 | 15 | 0.75 | |
| Education | <.0001 | |||
| Less than high school graduation | 4 | 4 | 0.16 | |
| High school graduate | 36 | 35 | 0.80 | |
| Some college | 29 | 32 | 0.69 | |
| College graduate | 31 | 29 | 1.47 | |
| Employment Status | <.0001 | |||
| Working | 56 | 62 | 0.57 | |
| Not Working | 44 | 38 | 0.57 | |
| Income | <.0001 | |||
| Less than 100% of FPL | 15 | 15 | 0.08 | |
| 100-199% FPL | 15 | 14 | 0.75 | |
| 200-399% FPL | 38 | 35 | 0.59 | |
| ≥400 | 32 | 36 | 0.07 | |
| Depression symptoms | <.0001 | |||
| Yes | 52 | 35 | 1.45 | |
| No | 48 | 65 | 1.45 | |
| Total Weighted Sample 52,816,364 | 4,032,106 | 48,784,258 | ||
Analytic Methods
Bivariate comparisons were used to evaluate how sociodemographic factors and depression were distributed among those with and without self-reported voice problems. We then assessed the extent to which self- report of voice problems was associated with the depression symptoms variable, controlling for age, sex, race, educational attainment, and poverty status using multivariate logistic regression. All analyses were conducted with SAS version 9.3 (Statistical Analysis Software Institute, Cary, NC, USA). Variance estimates were produced using Taylor series linearization.15
RESULTS
A total of 8% (4,032,106) of the weighted sample reported a voice problem within the prior 12 months. Most sampled adults reporting a voice problem were female (62%), of working age (ages 18-65) (81%), and/or of White non-Hispanic (74%) race. Bivariate analyses showed important differences in the sociodemographic characteristics of voice problems and of voice problems by depression symptoms, with 52% of the population that reported a voice problem also reporting depression symptoms, compared to 35% of the population that did not report a voice problem (p<0.0001, Table 1).
Using multivariate logistic regression, we evaluated the effects of patient and socio-demographic characteristics on the odds of voice problems for US adults (Table 2). Female gender and white non-Hispanic race were associated with greater likelihood of reporting a voice problem. Unemployed job status was associated with a slightly higher likelihood of reporting a voice problem. When controlling for all other patient factors, reported depression was associated with a nearly two-fold higher likelihood of a reported voice problem (OR=1.89, 95% CI=1.21-2.96).
Table 2.
Odds of the US civilian, non–institutionalized populations aged 18 years responding yes to the question “Have you had any problems or difficulties with your voice in the past year?” in 2012 NHIS
| Odds Ratio | 95% CI | |||
|---|---|---|---|---|
| Gender | ||||
| Female | 1.00-REF | |||
| Male | 0.64 | 0.59 | 0.69 | |
| Age Categories | ||||
| 18-30 | 0.82 | 0.22 | 3.02 | |
| 31-45 | 0.68 | 0.23 | 1.96 | |
| 46-65 | 0.65 | 0.26 | 1.63 | |
| 65+ | 1.00-REF | |||
| Race | ||||
| White NH | 1.00-REF | |||
| Black NH | 1.03 | 0.73 | 1.46 | |
| AIAN NH & Other | 1.51 | 1.14 | 1.99 | |
| Asian NH | 0.74 | 0.73 | 0.74 | |
| Hispanic | 0.45 | 0.25 | 0.82 | |
| Education | ||||
| Less than high school graduate | 1.01 | 0.95 | 1.07 | |
| High school graduate | 0.91 | 0.81 | 1.04 | |
| Some college | 0.77 | 0.42 | 1.41 | |
| College graduate | 1.00-REF | |||
| Income | ||||
| Less than 100% FPL vs 400% and above | 1.17 | 0.65 | 1.07 | |
| 100-200% FPL vs 400% and above | 1.09 | 0.72 | 1.62 | |
| 200-400% FPL vs 400% and above | 1.25 | 0.87 | 1.79 | |
| 400% and above | 1.00-REF | |||
| Depression symptoms | ||||
| No | 1.00-REF | |||
| Yes | 1.89 | 1.21 | 2.96 | |
Abbreviations: REF: reference. NH: Non-Hispanic. AIAN: American Indian/ Alaskan Native. FPL: Federal Poverty Line. Bold text indicates significance at p<0.05.
Voice problem diagnoses among adults with depression symptoms
Sample adults who received a diagnosis for a voice problem that lasted a week or longer were asked, “What diagnoses or reasons were you told caused your voice problems?” and responses were categorized by NHIS (Table 3). A high proportion of respondents, both with and without concurrently reported depression symptoms, indicated that “something else” caused their voice problem. Among adults reporting depression symptoms, most reported reflux, allergies and/or head/neck injuries as voice-related diagnoses. Non-depressed adults most commonly reported vocal nodules/polyps, head/neck cancer, and allergies.
Table 3.
Self-reported voice problem diagnosis by self-reported depression symptom status in 2012 NHIS
| Depression symptoms | |||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Reported diagnosis | (%)^ | SE | (%)^ | SE | p |
| Laryngitis (voice misuse, abuse, overuse) | 2 | 0.84 | 4 | 0.74 | 0.04 |
| Laryngitis caused by colds/strep | 8 | 0.19 | 10 | 1.23 | <.0001 |
| Vocal nodules or polyps | 1 | 1.13 | 24 | 4.1 | 0.01 |
| Gastroesophageal reflux disease | 22 | 0.13 | 2 | 1.46 | 0.03 |
| Allergies | 23 | 1.37 | 13 | 3.22 | 0.09 |
| Airborne irritants or environmental pollutants | - | 2 | 1.56 | NA | |
| Head/neck injury | 10 | 1.19 | - | NA | |
| Cancer anywhere in the head, neck, or throat | 4 | 1.07 | 17 | 0.61 | 0.01 |
| Neurological cause | - | 2 | 1.67 | NA | |
| Effect of prescription medication or drugs | 2 | 2.72 | - | NA | |
| Something else | 41 | 3.25 | 39 | 6.58 | 0.39 |
Note: Column may add up to more than 100% because more than one diagnosis may be mentioned per case.
SE=standard error. NA= not applicable.
Duration and severity of voice problem and depression status
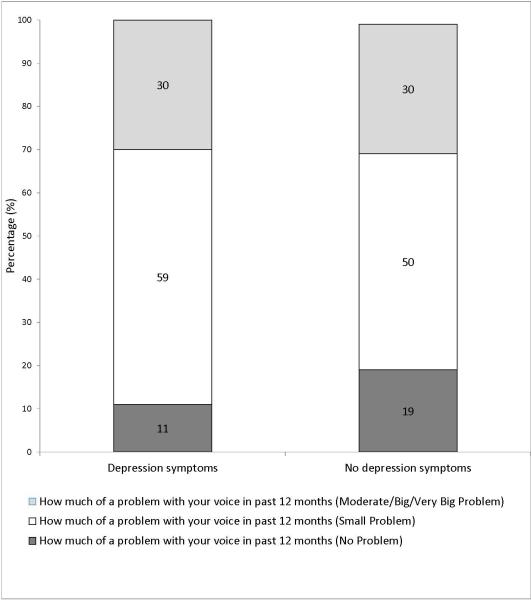
The total self-reported mean number of days with a voice problem total was 56 days (Standard Error (S.E.) 0.1, 95% confidence interval (CI) 54-57 days). When stratified by the presence of depression symptoms, the mean number of days with a voice problem was 55 days (S.E. 0.67, 95%CI 46-63 days) for adults with depression symptoms and 56 days (S.E. 0.70, 95%CI 48-65 days) for adults reporting none. Adults who reported a voice problem in the past 12 months for a week or longer were asked, “During the past 12 months, how much of a problem did you have with your voice? (No problem, a small problem, moderate problem, a big problem, a very big problem).” The presence of depression symptoms did not affect the distribution of responses (p=0.06), with the majority of respondents describing the voice problem as a “small problem” and 30% describing it as a moderate or greater problem (Figure 1).
Figure 1.
Voice problem severity percentage among United States adults with and without depression symptoms in 2012 NHIS.
There was no difference in the distribution of voice problem severity between those with and without depression symptoms (p = 0.06).
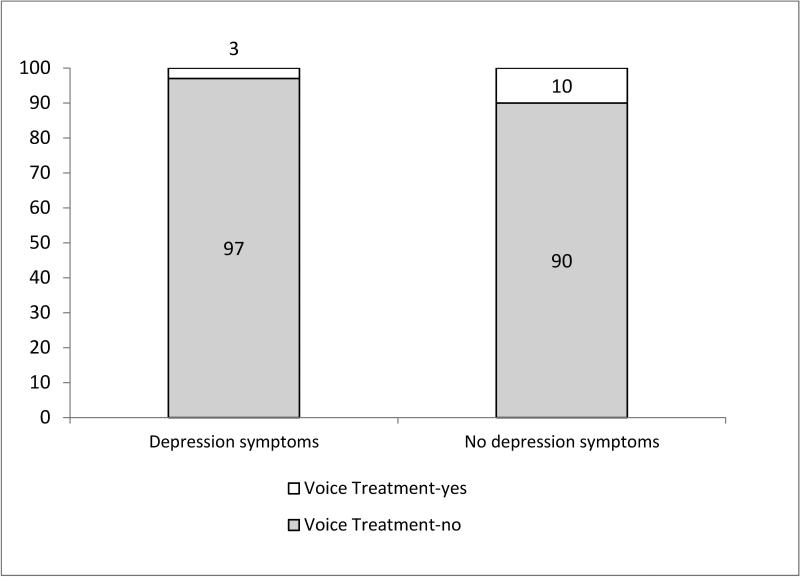
Voice problem treatment by depression status
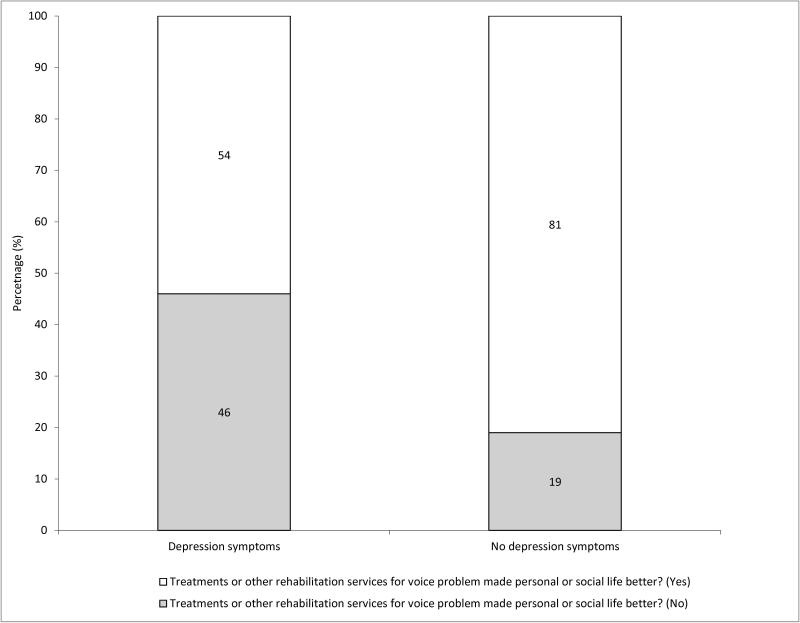
Sample adults that reported a voice problem in the past 12 months for a week or longer were asked, ”During the past 12 months, have you received treatments, therapy, or other rehabilitation services for your voice problems?” Only 3% of adults with depression symptoms reported receiving voice treatment, compared to 10% without depression (Figure 2, p=0.02). Adults who reported treatment or rehabilitative services for a voice problem in the past 12 months were also asked, “Did the treatments or other rehabilitation services for your voice problems make your personal or social life better? (yes/no).” Fifty four percent of adults with depression symptoms reported that voice treatment improved their personal/social life, compared to 81% of adults without depression symptoms (Figure 3, p=0.04).
Figure 2.
Self-reported percentage of sample that received treatments, therapy, or other rehabilitation services for voice problems in past 12 months, among respondents with and without depression symptoms in 2012 NHIS.
Percentage of those who reported voice-related treatment was lower in the group who also reported depression symptoms (p = 0.02).
Figure 3.
Self-reported percentage of sample reporting that voice treatment improved personal/social life, among respondents with and without depression symptoms in 2012 NHIS.
Percentage of those reporting that voice treatment improved personal/social life was lower among respondents with depression symptoms (p = 0.04).
DISCUSSION
Using US population-based survey data, we observed that self-reported depression symptoms were associated with a nearly doubled likelihood of reporting a voice problem. This suggests that the link between psychosocial distress and dysphonia is not unique to care-seeking populations.
Our findings raise some potentially concerning issues. It has been shown that only a small fraction of people in the general population with a voice problem report receiving care for it.1,16 We observed that this fraction was even smaller among those with concurrent voice problem and depression symptoms, even though reported voice problem severity was similar between those with and without depression symptoms. This is counter to literature suggesting that depression is associated with greater care utilization in the general population,17 but concordant with other studies that have identified decreased care receipt in adults with depression.18-21 These findings raise the possibility that those with concurrent depression symptoms and voice problems are an underserved population and may face barriers to seeking care for the voice problem; future studies are needed to examine the concordance and timing of depression and voice problems in a more formal way.1,22
Among those reporting treatment for the voice problem, those who also reported depression symptoms found voice treatment less effective in improving their personal/social life, suggesting that depression may be associated with lower treatment satisfaction in this population, as in others.23 Given the impact of patient satisfaction measures upon reimbursements24 and the high prevalence of depression in the otolaryngology patient population,25 this potential association of depression symptoms with lower patient satisfaction is important to recognize. Our findings are consistent with those in other areas, such as treatment of sinusitis26 and tinnitus27, showing that psychiatric distress is associated with greater symptom severity throughout the treatment course.
The presence or absence of depression symptoms was also associated with different voice-related diagnoses. That “something else” was the most common self-reported diagnosis in both groups necessitates caution when interpreting results, but reflux and allergies were most commonly reported in the depression symptoms group, and vocal nodules/polyps and head/neck cancer most common in the non-depression symptoms group. These differences seem to suggest that a laryngeal etiology for the voice problem is diagnosed more commonly among those without depression symptoms, although we are unable to ascertain whether these diagnoses were received from a primary care provider, general otolaryngologist, laryngologist, or other specialist. Future studies could investigate associated interesting questions, such as whether those with depression symptoms might be more likely to receive nonspecific voice-related diagnoses, or perhaps less likely to receive specialty care in which they might be given a more specific diagnosis.28
Although these findings are intriguing, they should be interpreted in the context of several important limitations. First, although patient self-report is critically valuable, this data source did not allow independent assessment or verification via medical or other records, and we did not have the benefit of using a symptom scale to assess severity or duration of depression, or the ability to assess for subtypes of depression or concurrent other psychiatric diagnoses. Similarly, no independent data source was available to assess the severity of the voice problem reported by respondents. Second, although studies in care-seeking voice patients have identified a high prevalence of anxiety,3-5 and anxiety may influence treatment outcomes in voice,29 data on anxiety were not available in this sample. Third, these data did not allow us to distinguish between access to care and desire to seek care, nor did they allow us to evaluate why the care received by patients who reported depression was felt to be less effective. Cross-sectional association of voice problems and depression symptoms also does not allow us to comment on causal mechanisms of voice problems and depression symptoms.30 Despite these limitations we believe our findings underscore an important potential relationship that deserves more attention.
The findings presented here highlight the importance of being sensitive to possible concurrent depression symptoms in patients who present with voice problems. These findings also identify a need to effectively reach a potentially underserved population. Further studies, potentially including qualitative and longitudinal approaches, may be helpful to clarify these associations, perhaps laying the groundwork for additional adjunctive treatment approaches to improve treatment outcomes.
CONCLUSIONS
We observed that self-reported depression symptoms were associated with an increased likelihood of reporting a voice problem in this examination of population-based survey data. Depression symptoms were also associated with more nonspecific voice-related diagnoses, a lower likelihood of reporting treatment of the voice problem, and a lower likelihood of finding treatment beneficial. The broader relationship between depression and voice problems remains complex, suggesting a need to identify specific factors that could be targeted to improve clinical and mental health outcomes for people with voice problems.
Acknowledgments
Research reported in this publication was supported by NIH UL1TR000114. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
No conflicts of interest or financial disclosures.
REFERENCES
- 1.Cohen SM. Self-reported impact of dysphonia in a primary care population: an epidemiological study. The Laryngoscope. 2010;120:2022–2032. doi: 10.1002/lary.21058. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz SR, Cohen SM, Dailey SH, et al. Clinical practice guideline: hoarseness (dysphonia). Otolaryngol Head Neck Surg. 2009;141:S1–S31. doi: 10.1016/j.otohns.2009.06.744. [DOI] [PubMed] [Google Scholar]
- 3.Dietrich M, Verdolini Abbott K, Gartner-Schmidt J, Rosen CA. The frequency of perceived stress, anxiety, and depression in patients with common pathologies affecting voice. Journal of voice : official journal of the Voice Foundation. 2008;22:472–488. doi: 10.1016/j.jvoice.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Siupsinskiene N, Razbadauskas A, Dubosas L. Psychological distress in patients with benign voice disorders. Folia Phoniatr Logop. 2011;63:281–288. doi: 10.1159/000324641. [DOI] [PubMed] [Google Scholar]
- 5.Misono S, Peterson CB, Meredith L, et al. Psychosocial distress in patients presenting with voice concerns. J Voice. 2014;28:753–761. doi: 10.1016/j.jvoice.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mirza N, Ruiz C, Baum ED, Staab JP. The prevalence of major psychiatric pathologies in patients with voice disorders. Ear Nose Throat J. 2003;82:808–810. 812, 814. [PubMed] [Google Scholar]
- 7.Willinger U, Volkl-Kernstock S, Aschauer HN. Marked depression and anxiety in patients with functional dysphonia. Psychiatry Res. 2005;134:85–91. doi: 10.1016/j.psychres.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Merrill RM, Anderson AE, Sloan A. Quality of life indicators according to voice disorders and voice-related conditions. Laryngoscope. 2011;121:2004–2010. doi: 10.1002/lary.21895. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharyya N. The prevalence of voice problems among adults in the United States. The Laryngoscope. 2014;124:2359–2362. doi: 10.1002/lary.24740. [DOI] [PubMed] [Google Scholar]
- 10.Johnson PJ, Blewett LA, Ruggles S, Davern ME, King ML. Four decades of population health data: the integrated health interview series as an epidemiologic resource. Epidemiology. 2008;19:872–875. doi: 10.1097/EDE.0b013e318187a7c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minnesota Population Center and State Health Access Data Assistance Center [2014];Integrated Health Interview Series: Version 5.0. 2012 Available at: http://www.ihis.us.
- 12.Minnesota Population Center User Notes: Use of Sampling Weights with IHIS. 2015 Available at: https://www.ihis.us/ihis/userNotes_weights.shtml.
- 13.Davern M, Rodin H, Beebe TJ, Call KT. The effect of income question design in health surveys on family income, poverty and eligibility estimates. Health services research. 2005;40:1534–1552. doi: 10.1111/j.1475-6773.2005.00416.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dzaijka JL, Denmead G. Income Data for Policy Analysis: A Comparative Assessment of Eight Surveys: Mathematica Policy Research. 2008 [Google Scholar]
- 15.SAS/STAT User's Guide Version 9.3. SAS Institute, Inc.; Cary, NC: 2004. [Google Scholar]
- 16.Bhattacharyya N. The prevalence of voice problems among adults in the United States. Laryngoscope. 2014;124:2359–2362. doi: 10.1002/lary.24740. [DOI] [PubMed] [Google Scholar]
- 17.Rowan PJ, Davidson K, Campbell JA, Dobrez DG, MacLean DR. Depressive symptoms predict medical care utilization in a population-based sample. Psychological medicine. 2002;32:903–908. doi: 10.1017/s0033291702005767. [DOI] [PubMed] [Google Scholar]
- 18.Levinson Miller C, Druss BG, Dombrowski EA, Rosenheck RA. Barriers to primary medical care among patients at a community mental health center. Psychiatr Serv. 2003;54:1158–1160. doi: 10.1176/appi.ps.54.8.1158. [DOI] [PubMed] [Google Scholar]
- 19.Carney CP, Jones LE. The influence of type and severity of mental illness on receipt of screening mammography. J Gen Intern Med. 2006;21:1097–1104. doi: 10.1111/j.1525-1497.2006.00565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thornicroft G, Rose D, Kassam A. Discrimination in health care against people with mental illness. International review of psychiatry. 2007;19:113–122. doi: 10.1080/09540260701278937. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. The British journal of psychiatry : the journal of mental science. 2009;194:491–499. doi: 10.1192/bjp.bp.107.045732. [DOI] [PubMed] [Google Scholar]
- 22.Gilman M, Merati AL, Klein AM, Hapner ER, Johns MM. Performer's attitudes toward seeking health care for voice issues: understanding the barriers. J Voice. 2009;23:225–228. doi: 10.1016/j.jvoice.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Bair MJ, Kroenke K, Sutherland JM, McCoy KD, Harris H, McHorney CA. Effects of depression and pain severity on satisfaction in medical outpatients: analysis of the Medical Outcomes Study. Journal of rehabilitation research and development. 2007;44:143–152. doi: 10.1682/jrrd.2006.06.0061. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Medicare and Medicaid Services [5/30/15];HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems): Patients’ Perspectives of Care Survey. Available at: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS.html.
- 25.Chandra RK, Epstein VA, Fishman AJ. Prevalence of depression and antidepressant use in an otolaryngology patient population. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2009;141:136–138. doi: 10.1016/j.otohns.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 26.Davis GE, Yueh B, Walker E, Katon W, Koepsell TD, Weymuller EA. Psychiatric distress amplifies symptoms after surgery for chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2005;132:189–196. doi: 10.1016/j.otohns.2004.09.135. [DOI] [PubMed] [Google Scholar]
- 27.Pinto PC, Marcelos CM, Mezzasalma MA, Osterne FJ, de Melo Tavares de Lima MA, Nardi AE. Tinnitus and its association with psychiatric disorders: systematic review. J Laryngol Otol. 2014;128:660–664. doi: 10.1017/S0022215114001030. [DOI] [PubMed] [Google Scholar]
- 28.Cohen SM, Dinan MA, Roy N, Kim J, Courey M. Diagnosis change in voice-disordered patients evaluated by primary care and/or otolaryngology: a longitudinal study. Otolaryngol Head Neck Surg. 2014;150:95–102. doi: 10.1177/0194599813512982. [DOI] [PubMed] [Google Scholar]
- 29.Ng JH, Lo S, Lim F, Goh S, Kanagalingam J. Association between anxiety, type A personality, and treatment outcome of dysphonia due to benign causes. Otolaryngol Head Neck Surg. 2013;148:96–102. doi: 10.1177/0194599812465592. [DOI] [PubMed] [Google Scholar]
- 30.Conture EG, Kelly EM, Walden TA. Temperament, speech and language: an overview. J Commun Disord. 2013;46:125–142. doi: 10.1016/j.jcomdis.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]