Abstract
Background
Fatty infiltration (FI) of the muscle as graded by the Goutallier classification (GC) is a well-known sequela following rotator cuff injury. The degree to which this predicts the success of rotator cuff repair is unknown.
Questions/Purposes
We conducted a systematic review to address the following questions: (1) Does the grade of FI of the rotator cuff muscles present preoperatively predict retear rates postoperatively? (2) Are amounts of preoperative FI predictive of functional outcomes following repair?
Methods
Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and the Cochrane Central Register of Controlled Trials online databases were searched for all literature published between January 1966 and March 2015. Keywords were chosen to achieve a broad search category. All articles were reviewed by three of the authors, and those meeting the study inclusion criteria were selected for data abstraction.
Results
The systematic literature review yielded 11 studies reporting on a total of 925 shoulders. Rotator cuffs with moderate or significant FI preoperatively (grades 2–4) had a significantly higher retear rate than those with no or minimal FI (grades 0–1) (59 vs. 25%, p = 0.045). Four studies reported postoperative Constant scores and preoperative GC scores. One study found that lower GC scores were associated with higher Constant scores postoperatively, one found no association, and the data was inconclusive in the other two.
Conclusions
While lower preoperative GC scores are associated with lower rates of rotator cuff retear following repair, there is insufficient data to make conclusions on the effects of FI on functional outcomes following repair.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-015-9465-5) contains supplementary material, which is available to authorized users.
Keywords: massive rotator cuff tears, rotator cuff tears, fatty infiltration, Goutallier score, functional outcomes, retear rates, preoperative evaluation
Introduction
Rotator cuff tears are a common musculoskeletal problem. Recent studies show the prevalence of rotator cuff tears to be between 15 and 51% of the population with the highest incidence in persons older than 50 years of age [35]. While not all rotator cuff tears are painful or debilitating, those that are often require surgical repair. While repair can be effective at treating pain and disability, a large number of rotator cuff repairs go on to retear [2, 21].
Most research on rotator cuff healing has focused on ways to alter and strengthen the bone-tendon interface. However, there is an increasing awareness that muscle physiology, specifically the presence of fatty infiltration (FI), can have a significant effect on the mechanical and biologic properties of the rotator cuff. When it occurs, FI can be found in multiple locations within the muscle including intramuscular and extramuscular compartments as well as the tendons themselves [11]. Multiple hypotheses have been generated to explain why FI occurs following a rotator cuff tear [6, 13] but, as of yet, no one theory explains its pathophysiology.
The staging of FI involving the rotator cuff muscles was originally described by Goutallier in 1994 using computerized tomography (CT) with contrast [15]. He described a five-stage grading system (Table 1) that could be used to predict the outcomes of rotator cuff repair and also determine which rotator cuff tears would likely be irreparable. While the original staging system was described using CT, it has since been applied to magnetic resonance imaging (MRI) which has become the standard modality in the USA when grading the presence of FI [9, 32]. Both classification systems compare the ratio of fat to muscle on sagittal oblique images: stage 0–1 is considered normal and has no (0) to trace (1) amounts of fat investing the muscle bellies. Stages 2–4 are considered pathologic: more muscle than fat (2), equal muscle to fat (3), and more fat than muscle (4).
Table 1.
Goutallier grading of fatty infiltration
| Stage 0 | Normal muscle; no fatty streak |
| Stage 1 | Some fatty streaks |
| Stage 2 | Fatty infiltration important; more muscle than fat |
| Stage 3 | As much fat as muscle |
| Stage 4 | More fat than muscle |
While studies have suggested that the presence of FI can have a negative impact on outcomes following rotator cuff repair [5, 15, 16, 23, 26, 30], the extent to which this is true remains controversial. We performed a systematic review of the scientific literature to answer the following questions: (1) Does the amount of FI of the rotator cuff musculature present preoperatively predict retear rates postoperatively? (2) Do rotator cuffs with less FI present preoperatively achieve higher functional status after repair?
Methods
Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and the Cochrane Central Register of Controlled Trials were searched for all literature published from January 1966 to March 2015 using the following keywords: rotator cuff, rotator cuff tear, rotator cuff repair, fat, degeneration, fatty degeneration, atrophy, Goutallier, muscle, fat infiltration, and fatty infiltration. General search terms were chosen to prevent the possibility of missing potential studies. No restrictions were placed on study types during the initial screening phase.
In order to be included in analysis, the identified study had to include either postoperative retear rates (as measured radiographically) or functional outcomes for shoulders classified preoperatively by amount of FI present. Importantly, studies were excluded if they made statements regarding the effect of preoperative FI on postoperative outcomes but did not provide objective data relating retear rates or postoperative functional outcome scores to the preoperative Goutallier score. Additionally, studies were excluded if they used the Goutallier classification system and then treated the data as continuous rather than categorical data. The authors feel that this is an important distinction, as, by definition, the Goutallier classification is a categorical grading system.
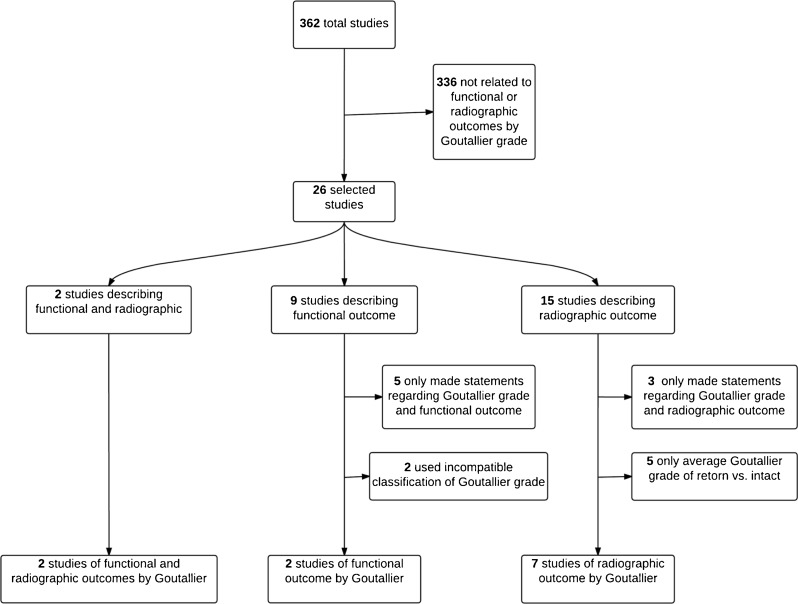
There were 362 articles found with all of the general search terms. The abstracts of each of the combined searches were then reviewed by three authors (MK, JL, NT) to determine appropriateness for inclusion in the study. Any discrepancies in evaluation were resolved with input by the senior author (LG). After initial review, there were 26 articles that were deemed appropriate for the analysis. Of the 26 articles, 15 were excluded after a full-text review. Three studies were excluded because they made statements regarding preoperative Goutallier grade and retear rates but did not provide retear rates for each Goutallier grade individually [30, 31, 36]. Five studies that only compared the average Goutallier grades for intact versus retorn cuffs were excluded [10, 29, 33, 37, 38]. An additional seven studies analyzing the effect of preoperative FI on functional outcome were also excluded. Five of those studies made statements regarding the effects of preoperative Goutallier grade on postoperative functional outcome scores but did not provide data for each Goutallier grade individually [14, 16, 18, 19, 26]. One of those studies, by Goutallier et al. [17], provided functional outcome scores by preoperative Goutallier classification (GC) score but used classifications of Goutallier grade that did not allow for direct comparison with other reports (i.e., <1, 1–1.49, and ≥1.5). This was similar to another excluded study, by Burkhart et al. [1], which compared functional outcome data of rotator cuffs with 50–75 and >75% FI. There were seven studies that met the inclusion criteria and compared retear rates by Goutallier grade [4, 7, 8, 14, 16, 24, 26] and two studies that met the inclusion criteria and compared functional outcome by Goutallier grade [20, 28]. Two studies met the criteria for both retear rates and functional outcomes [3, 12]. The four studies that compared functional outcome to Goutallier grade used the Constant-Murley scoring system. This was the most prevalently used validated scoring system in the studies that met the inclusion criteria. The search criteria gave a total of 11 studies that were included in the final data analysis (Fig. 1).
Fig. 1.
Flow chart showing methodology of literature search. Literature search: There were 362 articles found with all of the general search terms. The abstracts of each of the combined searches were then reviewed to determine appropriateness for inclusion in the study. There were 26 articles that were deemed appropriate for the analysis. Of the 26 articles, 15 were excluded after a full-text review. Three studies were excluded because they made statements regarding preoperative Goutallier grade and radiographic outcomes but did not provide retear rates for each Goutallier grade individually [26, 29, 34]. Five studies that only compared the average Goutallier grades for intact versus retorn cuffs were excluded [8, 26, 31, 35, 36]. An additional seven studies analyzing the effect of preoperative fatty infiltration on functional outcome were also excluded. Five studies made statements regarding the effects of preoperative Goutallier grade on postoperative functional outcome scores but did not provide data for each Goutallier grade individually [13–16, 25]. One study, by Goutallier et al. [19], provided Constant-Murley scores by preoperative Goutallier grade but used classifications of Goutallier grade that did not allow for direct comparison with other reports (i.e., <1, 1–1.49, and ≥1.5). This was similar to another excluded study, by Burkhart et al. [1], which compared functional outcome data of rotator cuffs with 50–75 and >75% fatty infiltration. There were seven studies that met the inclusion criteria and compared radiographic outcome (intact versus retorn) by Goutallier grade [4, 6, 7, 13, 14, 22, 25] and two studies that met the inclusion criteria and compared functional outcome by Goutallier grade [18, 27]. Two studies met the criteria for both radiographic and functional outcomes [3, 11]. This gave a total of 11 studies that were included in the final data analysis (Fig. 1).
The amount of rotator cuff FI present preoperatively was categorized according to the GC system. In analyzing radiographic outcome (postoperative retear rates), rotator cuffs were divided into two groups: those with Goutallier scores of 0 or 1 and those with scores of 2 to 4. Out of the eight studies that compared retear rates by Goutallier grade, four used the same partition [4, 14, 16, 27]. Two studies did not report any patients with a Goutallier grade above 2 [12, 24]. The remaining three studies did not provide substantial data to segment the ranges further [3, 7]. In analyzing functional outcome (by postoperative Constant score), rotator cuffs were divided into five groups (Goutallier score of 0, 1, 2, 3, or 4).
Each of the studies that met the inclusion criteria was analyzed for the following: type of study, level of evidence, number of patients enrolled, number of patients in the final follow-up, and the mean length of follow-up. Surgical technique was classified as open, mini-open, or arthroscopic. The type of imaging modality used both preoperatively and postoperatively was also recorded (Table 2). Information was collected in table format, and the difference between retear rates by preoperative Goutallier score was evaluated using a one-tailed, paired Student t test. Statistical significance was set at p < 0.05 (Table 3).
Table 2.
Patient and study demographics for studies comparing retear rates and clinical outcomes of rotator cuff repair by preoperative Goutallier classification
| Source | Study | Level of evidence | Total no. of shoulders | No. of shoulders evaluated | Type of imaging | Surgical technique | Mean follow-up (months) | |
|---|---|---|---|---|---|---|---|---|
| Preop | Postop | |||||||
| Castagna et al. [3] | Case series | IV | 29 | 29 | MRI | US | Arthroscopic | 30 |
| Cho et al. [4] | Case series | IV | 169 | 169 | MRI | MRI | Arthroscopic | 39 |
| Demirors et al. [7] | Case series | IV | 26 | 21 | MRI | MRI | Open | 32 |
| Deniz et al. [8] | Case series | IV | 102 | 87 | MRI | MRI | Arthroscopic | 30 |
| Gerber et al. [13] | Case series | IV | 13 | 13 | MRI | MRI | ? | ∼12 |
| Gladstone et al. [14] | Prospective cohort | II | 38 | 38 | MRI | MRI | Open (15); arthroscopic (23) | 12–15b |
| Goutallier et al. [17] | Retrospective review | II | 220 | 220 | CT | MRI (116); CT (104) | ? | 37 |
| Grasso et al. [20] | RCT | I | 80 | 72 | MRI | – | Arthroscopic | 25 |
| Liem et al. [24] | Case series | IV | 53 | 45 | MRI | MRI | Arthroscopic | 26 |
| Mellado et al. [27] | Case series | IV | 78 | 71 | MRI | MRI | Open (37); mini-open (14); arthroscopic (27)a | 48 |
| Milano et al. [28] | RCT | I | 110 | 101 | MRI | – | Arthroscopic | 24 |
MRI magnetic resonance imaging, CT computed tomography
aData is for 78 total shoulders evaluated. Surgical technique for 71 evaluated shoulders is unavailable
bNo mean reported; this is the range of follow-up
Table 3.
Retear rates of rotator cuff repairs by preoperative Goutallier classification
| Study | No. of shoulders evaluated | No. of cuffs with preoperative GC of 0–1 | No. of retears in cuffs with preoperative GC of 0–1 (%) | No. of cuffs with preoperative GC of 2–4 | No. of retears in cuffs with preoperative GC of 2–4 (%) | p value with significance at p < 0.05 |
|---|---|---|---|---|---|---|
| Castagna et al. [3] | 29 | 15 | 3 (20) | 14 | 8 (57) | |
| Cho et al. [4] | 169 | 130 | 13 (10) | 39 | 25 (64) | |
| Demirors et al. [7] | 21 | 16 | 6 (38) | 5 | 4 (80) | |
| Deniz et al. [8] | 87 | 43 | 7 (16) | 44 | 19 (43) | |
| Gerber et al. [13] | 13 | 9 | 4 (44) | 4 | 1 (25) | |
| Gladstone et al. [14] | 38 | 28 | 8 (29) | 10 | 7 (70) | |
| Goutallier et al. [17] | 220 | 173 | 49 (28) | 47 | 30 (64) | |
| Liem et al. [24] | 45 | 35 | 6 (17) | 10 | 4 (40) | |
| Mellado et al. [27] | 71 | 59 | 30 (51) | 12 | 11 (92) | |
| Total | 693 | 508 | 126 (25) | 185 | 109 (59) | p value = 0.045 |
GC Goutallier classification
The total number of shoulders evaluated in these studies ranged from 13 to 220 with an average of 77 shoulders. Six of the 11 included studies used arthroscopic rotator cuff repair exclusively [3, 4, 8, 20, 23, 28]. Three studies used only open repair techniques [7, 12, 16]. One study included both patients having undergone arthroscopic repair and those having undergone open repair [14]. Finally, one study used all three surgical techniques: arthroscopic, mini-open, and open repair [27]. Average length of follow-up in the 11 included studies ranged from 12 to 48 months. Of the 11 studies included, ten used MRI to determine the amount of FI (and corresponding Goutallier grade) present preoperatively [3, 4, 7, 8, 12, 14, 20, 24, 27, 28]. The other study used CT for this purpose [16]. Of the eight studies that analyzed rotator cuff integrity postoperatively, seven of the groups of investigators used MRI [4, 7, 8, 12, 14, 27], ultrasound was used exclusively in one study [3], and both CT and MRI were used in another study [16].
Results
Nine studies reported rotator cuff retear rates by amount of preoperative FI. Patients were combined into two categories for comparison: those with Goutallier grade of 0 or 1 and those with Goutallier grade of 2 to 4 (Table 3) [3, 4, 7, 12, 14, 16, 24, 27]. Five hundred eight shoulders had a preoperative Goutallier grade of 0–1, and 185 shoulders were graded 2–4, for a total of 693 evaluated shoulders. Rotator cuffs with moderate or significant FI preoperatively (Goutallier grades of 2–4) had a significantly higher rate of retear on postoperative imaging than those with no or minimal FI (Goutallier grade of 0–1) (59 vs. 25%; p = 0.04). Retear rates in shoulders with scores of 0 or 1 ranged from 10 to 51% in the studies included. Shoulders with preoperative scores of 2–4 had retear rates between 25 and 92%. However, data was more limited in this segment. The study that reported a retear rate of 25%, Gerber et al., only had four patients with Goutallier grades of 2–4 [12]. In the other eight included studies, the average retear rates for shoulders with preoperative Goutallier grades of 2–4 were 37% higher than the average retear rates for shoulders graded as 0 or 1 preoperatively [3, 4, 7, 8, 14, 16, 24, 27].
Four studies provided data that allowed preoperative GC score to be correlated with postoperative Constant score [3, 12, 20, 28]. The studies by Castagna et al. and Gerber et al. provided data but did not directly compare the Goutallier scores with Constant scores, but rather compared the predefined groups of grades 0 and 1 and grades 2–4 with the Constant scores. In the study by Castagna et al., shoulders with a preoperative GC of 0 or 1 had postoperative Constant scores of 29.2 ± 11.9 and 32 ± 14.8, respectively, at an average of 30 months postoperatively. Shoulders with a GC of 2 and 3 had Constant scores of 48.9 ± 28.2 and 37.2 ± 16, respectively. In the study by Gerber et al., a GC of 0 provided an average Constant score of 69.7 ± 5.7 12 months after surgery. A GC of 1 or 2 was associated with average postoperative Constant scores of 50.3 ± 16.2 and 53 ± 2.8, respectively. The study did not contain any patients with GC scores of 3 or 4. Grasso et al. and Milano et al. correlated preoperative GC scores and postoperative Constant scores. In the study by Grasso et al., the authors did not find a positive correlation between preoperative GC and postoperative function. Using their modified Constant score as an outcome measure, they found there to be no significant difference in functional outcome between those patients with less FI in their preoperative MRIs and those with higher GC scores (Table 4). Alternatively, Milano et al., in their series of 101 shoulders, did find that a lower GC score was associated with a higher Constant score at 2-year follow-up (Table 4).
Table 4.
Functional outcome of rotator cuff repairs by preoperative Goutallier classification as measured by Constant-Murley score
| Study | No. of shoulders evaluated | GC = 0 | GC = 1 | GC = 2 | GC = 3 | GC = 4 | Difference between groups? | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of shoulders | Postop Constant score mean ± SD | No. of shoulders | Postop Constant score mean ± SD | No. of shoulders | Postop Constant score mean ± SD | No. of shoulders | Postop Constant score mean ± SD | No. of shoulders | Postop Constant score mean ± SD | |||
| Castagna et al. [3] |
29 | 5 | 29.2 ± 11.9 | 10 | 32.0 ± 14.8 | 8 | 48.9 ± 28.2 | 6 | 37.2 ± 16.0 | 0 | – | |
| Gerber et al. [15] |
13 | 3 | 69.7 ± 5.7 | 8 | 50.3 ± 16.2 | 2 | 53.0 ± 2.8 | 0 | – | 0 | – | |
| Grasso et al. [20] |
72 | 0 | – | 25 | 99.9 ± 18.7 | 28 | 102.7 ± 24.0 | 17 | 106.4 ± 14.9 | 2 | 104.3 ± 4.0 | No |
| Milano et al. [28] |
101 | 0 | – | 23 | 110.5 ± 9.5 | 34 | 104.4 ± 12.5 | 29 | 91.3 ± 25.3 | 15 | 100.3 ± 11.2 | Yes |
In Gerber et al., an individual Goutallier score was given for the supraspinatus, infraspinatus, and subscapularis muscle in each patient. In this table, the Goutallier score of the three muscles was averaged together and rounded to the nearest whole number
GC Goutallier classification, SD standard deviation
Discussion
This study was designed as a systematic review of the published literature to determine if preoperative FI, as measured by the GC score, can predict postoperative retear rates and functional outcomes following rotator cuff repair. The authors’ hypothesis was that higher Goutallier scores would lead to higher retear rates as well as worse clinical outcomes following rotator cuff repair. The results of this review indicate that the preoperative quality of the rotator cuff muscles plays an important role in predicting healing rates following rotator cuff repairs. However, the role that preoperative FI plays in predicting clinical outcomes as determined by Constant scores remains difficult to determine. In this review, it is clear that lower GC scores (0–1) preoperatively are associated with a lower rate of retear (25%) than are repairs done on rotator cuffs with a higher (2–4) GC score (59%). The ability of preoperative GC scores to predict postoperative function as measured by the Constant score is difficult to assess based on the current published literature. In the four studies that met the inclusion criteria for this study, one found no significant difference in postoperative functional outcome when stratifying by GC score, and another found that lower preoperative GC score was predictive of higher postoperative Constant scores. While there have been studies published that describe a significant inverse correlation between preoperative GC score and postoperative shoulder function [14, 16–19, 26], the data that those studies presented did not meet the inclusion criteria for this review.
While higher GC scores are correlated to the incidence of a recurrent rotator cuff defect following attempted repair, it has proven difficult to associate recurrent defects with worse function postoperatively. There are several possible explanations for this difficult correlation. One is that rotator cuff tears, even those that have never been treated, do not necessarily correlate with worse shoulder function. Second, there is a detection bias as only symptomatic retears present for repeat imaging, leading us to believe that a retear is more significant than it may actually be. Patients who have undergone rotator cuff repair might have a recurrent defect but not present with any disability and therefore might not have any further imaging done. Despite this difficulty, several studies have attempted to correlate recurrent defects with shoulder function. Harryman et al. [21] evaluated 105 operative repairs of rotator cuff tears in 89 patients at an average follow-up of 5 years following the attempted rotator cuff repair using ultrasonography to evaluate the status of the cuff. They found that shoulders with an intact rotator cuff had better function during activities of daily living and better shoulder range of motion. They also found that in shoulders with residual defects, the size of the defect predicts the degree of shoulder dysfunction; i.e., larger defects gave rise to worse shoulder function.
Since Goutallier first introduced his scoring system for measuring FI in 1994, it has been shown that the preoperative status of the rotator cuff muscles has an impact on the success of rotator cuff repair regardless of whether it is done through an arthroscopic, mini-open, or open approach [22, 25, 34]. Despite this knowledge, much of the outcome research on rotator cuff repair healing and function does not include information on preoperative FI of the rotator cuff muscles. Rather, studies tend to focus on the size of rotator cuff tears as a significant predictor of outcome. Size, however, may not always be an accurate predictor of outcome, as large acute tears that present with good muscle and tendon quality can often be more successfully repaired. While not directly evaluated in this study, the authors believe that the reparability of “massive rotator cuff tears” has more to do with the chronicity of the tear and how it relates to muscle and tendon quality than it has to do with the size of the tear. This systematic review suggests that there is sufficient evidence to suggest that FI corresponds to healing rates to argue in favor of its inclusion as a variable in future studies that evaluate the results of rotator cuff repair.
The strengths of this study include the generation of a working hypothesis that was used to formulate a research plan with very specific inclusion and exclusion criteria. The criteria were applied to multiple large databases in order to capture all of the literature published to date that examines the ability of preoperative GC scores to predict postoperative rotator cuff retear rates and functional outcomes. The main weakness of this study, like all systematic reviews, is that the conclusions that the authors have drawn were limited by the quality of the current literature. While this review is able to correlate GC scores with retear rates, the limited and heterogeneous data that is available regarding functional outcome limited our ability to make a definitive statement regarding FI and functional outcome following rotator cuff repair.
In conclusion, lower preoperative GC scores are associated with lower rates of rotator cuff retear following repair. There was insufficient data to make conclusions on the effects of FI on functional outcomes following repair. Research examining outcomes of rotator cuff repair should measure preoperative FI and report on its association with the outcome of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Disclosures
Conflict of Interest
M. Michael Khair, MD, Jason Lehman, MD and Nicholas Tsouris, BS have declared that they have no conflict of interest. Lawrence V. Gulotta, MD reports personal fees from Biomet, Inc., outside the work.
Human/Animal Rights
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
N/A
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Burkhart SS, Barth JR, Richards DP, Zlatkin MB, Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23(4):347–354. doi: 10.1016/j.arthro.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 2.Calvert PT, Packer NP, Stoker DJ, Bayley JI, Kessel L. Arthrography of the shoulder after operative repair of the torn rotator cuff. J Bone Joint Surg Br. 1986;68(1):147–150. doi: 10.1302/0301-620X.68B1.3941132. [DOI] [PubMed] [Google Scholar]
- 3.Castagna A, Conti M, Markopoulos N, et al. Arthroscopic repair of rotator cuff tear with a modified Mason-Allen stitch: mid-term clinical and ultrasound outcomes. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):497–503. doi: 10.1007/s00167-007-0461-2. [DOI] [PubMed] [Google Scholar]
- 4.Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009;1(2):96–104. doi: 10.4055/cios.2009.1.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung SW, Kim JY, Kim MH, Kim SH, Oh JH. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med. 2013;41(7):1674–1683. doi: 10.1177/0363546513485719. [DOI] [PubMed] [Google Scholar]
- 6.Coleman SH, Fealy S, Ehteshami JR, et al. Chronic rotator cuff injury and repair model in sheep. J Bone Joint Surg Am. 2003;85-A(12):2391–2402. doi: 10.2106/00004623-200312000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Demirors H, Circi E, Akgun RC, et al. Correlations of isokinetic measurements with tendon healing following open repair of rotator cuff tears. Int Orthop. 2010;34(4):531–536. doi: 10.1007/s00264-009-0827-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deniz G, Kose O, Tugay A, Guler F, Turan A. Fatty degeneration and atrophy of the rotator cuff muscles after arthroscopic repair: does it improve, halt or deteriorate? Arch Orthop Trauma Surg. 2014;134(7):985–990. doi: 10.1007/s00402-014-2009-5. [DOI] [PubMed] [Google Scholar]
- 9.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8(6):599–605. doi: 10.1016/S1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 10.Fuchs B, Gilbart MK, Hodler J, Gerber C. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006;88(2):309–316. doi: 10.2106/JBJS.E.00117. [DOI] [PubMed] [Google Scholar]
- 11.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Gerber C, Schneeberger AG, Hoppeler H, Meyer DC. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J Shoulder Elbow Surg. 2007;16(6):691–696. doi: 10.1016/j.jse.2007.02.122. [DOI] [PubMed] [Google Scholar]
- 13.Gerber C, Meyer DC, Frey E, et al. Neer award 2007: Reversion of structural muscle changes caused by chronic rotator cuff tears using continuous musculotendinous traction. An experimental study in sheep. J Shoulder Elbow Surg. 2009;18(2):163–171. doi: 10.1016/j.jse.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35(5):719–728. doi: 10.1177/0363546506297539. [DOI] [PubMed] [Google Scholar]
- 15.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;(304):78–83. [PubMed]
- 16.Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12(6):550–554. doi: 10.1016/S1058-2746(03)00211-8. [DOI] [PubMed] [Google Scholar]
- 17.Goutallier D, Postel JM, Van Driessche S, Godefroy D, Radier C. Tension-free cuff repairs with excision of macroscopic tendon lesions and muscular advancement: results in a prospective series with limited fatty muscular degeneration. J Shoulder Elbow Surg. 2006;15(2):164–172. doi: 10.1016/j.jse.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 18.Goutallier D, Postel JM, Radier C, Bernageau J, Zilber S. Long-term functional and structural outcome in patients with intact repairs 1 year after open transosseous rotator cuff repair. J Shoulder Elbow Surg. 2009;18(4):521–528. doi: 10.1016/j.jse.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 19.Goutallier D, Postel JM, Radier C, Bernageau J, Godefroy D, Zilber S. How repaired rotator cuff function influences constant scoring. Orthop Traumatol Surg Res. 2010;96(5):500–505. doi: 10.1016/j.otsr.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 20.Grasso A, Milano G, Salvatore M, Falcone G, Deriu L, Fabbriciani C. Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthroscopy. 2009;25(1):4–12. doi: 10.1016/j.arthro.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 21.Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73(7):982–989. [PubMed] [Google Scholar]
- 22.Ji X, Bi C, Wang F, Wang Q. Arthroscopic versus mini-open rotator cuff repair: an up-to-date meta-analysis of randomized controlled trials. Arthroscopy. 2015;31(1):118–124. doi: 10.1016/j.arthro.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 23.Jost B, Pfirrmann CW, Gerber C, Switzerland Z. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000;82(3):304–314. doi: 10.2106/00004623-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Liem D, Lichtenberg S, Magosch P, Habermeyer P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am. 2007;89(8):1770–1776. doi: 10.2106/JBJS.F.00749. [DOI] [PubMed] [Google Scholar]
- 25.Mall NA, Tanaka MJ, Choi LS, Paletta GA., Jr Factors affecting rotator cuff healing. J Bone Joint Surg Am. 2014;96(9):778–788. doi: 10.2106/JBJS.M.00583. [DOI] [PubMed] [Google Scholar]
- 26.Mellado JM, Calmet J, Olona M, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005;184(5):1456–1463. doi: 10.2214/ajr.184.5.01841456. [DOI] [PubMed] [Google Scholar]
- 27.Mellado JM, Calmet J, Olona M, et al. MR assessment of the repaired rotator cuff: prevalence, size, location, and clinical relevance of tendon rerupture. Eur Radiol. 2006;16(10):2186–2196. doi: 10.1007/s00330-006-0147-z. [DOI] [PubMed] [Google Scholar]
- 28.Milano G, Grasso A, Salvatore M, Saccomanno MF, Deriu L, Fabbriciani C. Arthroscopic rotator cuff repair with metal and biodegradable suture anchors: a prospective randomized study. Arthroscopy. 2010;26(9 Suppl):S112–S119. doi: 10.1016/j.arthro.2010.01.030. [DOI] [PubMed] [Google Scholar]
- 29.Nich C, Mutschler C, Vandenbussche E, Augereau B. Long-term clinical and MRI results of open repair of the supraspinatus tendon. Clin Orthop Relat Res. 2009;467(10):2613–2622. doi: 10.1007/s11999-009-0917-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009;25(1):30–39. doi: 10.1016/j.arthro.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 31.Park JY, Siti HT, Keum JS, Moon SG, Oh KS. Does an arthroscopic suture bridge technique maintain repair integrity?: a serial evaluation by ultrasonography. Clin Orthop Relat Res. 2010;468(6):1578–1587. doi: 10.1007/s11999-009-0990-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schiefer M, Mendonca R, Magnanini MM, et al. Intraobserver and interobserver agreement of Goutallier classification applied to magnetic resonance images. J Shoulder Elbow Surg. 2015;24(8):1314–1321. doi: 10.1016/j.jse.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 33.Sethi PM, Noonan BC, Cunningham J, Shreck E, Miller S. Repair results of 2-tendon rotator cuff tears utilizing the transosseous equivalent technique. J Shoulder Elbow Surg. 2010;19(8):1210–1217. doi: 10.1016/j.jse.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 34.Shan L, Fu D, Chen K, Cai Z, Li G. All-arthroscopic versus mini-open repair of small to large sized rotator cuff tears: a meta-analysis of clinical outcomes. PLoS One. 2014;9(4):e94421. doi: 10.1371/journal.pone.0094421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]
- 36.Yi JW, Cho NS, Cho SH, Rhee YG. Arthroscopic suture bridge repair technique for full thickness rotator cuff tear. Clin Orthop Surg. 2010;2(2):105–111. doi: 10.4055/cios.2010.2.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yoo JC, Ahn JH, Koh KH, Lim KS. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy. 2009;25(10):1093–1100. doi: 10.1016/j.arthro.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 38.Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90(11):2423–2431. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)