Abstract
Background
Ganglion cysts are the most common soft tissue tumors of the hand and wrist. There is currently no data available for the recurrence or complication rate of patients that self treat ganglion cysts by using an extrinsic force. Despite this absence of evidence, patients are still using this mode of treatment.
Questions/Purposes
The purpose of the study is to evaluate the efficacy of blunt force as a treatment modality for disrupting ganglion cysts.
Methods
We analyzed videos of patients attempting to disrupt their ganglion cysts of the wrist by blunt force on Youtube.com and surveyed them anonymously. Candidates were contacted through YouTube’s email server and given a link to an online questionnaire.
Results
Two hundred fourteen individuals were reviewed with a total of 1,008,913 views. Eighty three percent of videos were effective in treating the cyst. All 38 individuals that responded to the survey reported that the blunt force was effective in immediate elimination of the cyst in an average of 1.6 attempts (range 1–5). A majority (N = 21, 55%) reported no recurrence since the initial disruption of the cyst at a follow-up of 24 months.
Conclusions
YouTube.com was found to be an effective outlet to study a treatment modality that would otherwise be limited by practical considerations. The study showed that a subset of patients is utilizing blunt force trauma to successfully treat wrist ganglion cysts.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9493-9) contains supplementary material, which is available to authorized users.
Keywords: cyst, ganglion, wrist ganglion, ganglion cyst, video
Introduction
Ganglion cysts are common benign soft tissue masses infrequently requiring treatment. While their etiology and true incidence are unknown, they represent 60% of hand and wrist tumors [25]. They are three times more prevalent in females than in males and, while they can occur in the elderly in children, they most often occur between the second to fourth decade of life [25]. When necessary, treatment options include aspiration and excision via open or arthroscopic techniques. Most treatment algorithms appropriately begin with nonsurgical management due to the limited morbidity and high potential for spontaneous resolution [10]. If aspiration proves ineffective and further intervention is required, open or arthroscopic surgical excision may be performed. While these are currently the only accepted treatments, a historical mantra for the management of a ganglion cyst is to disrupt its capsule using an extrinsic force (i.e., a blunt force applied by book) [5]. Such treatment has resulted in the ganglion cyst being coined “Giddeon’s disease” or a “Bible bump [9].”
Despite its historical use, limited research has been performed to study this potentially effective treatment. In 1972, Nelson et al. reported a cure rate of approximately 66% after a mean follow-up of 8.1 years following treatment with a blunt force [18]. We are not aware of any further studies that have used this technique since this report, likely due to practical considerations and the concern for iatrogenic trauma. Despite the absence of evidence for its effectiveness, we have had multiple patients who have self-treated using this technique.
With over 1 billion unique users from 56 different countries visiting each month, YouTube.com is the third most commonly visited website on the internet [27] and can provide a unique look at self-treatment methods such as this [23]. We believe that patients still use blunt force as a mode of treatment for ganglion cysts and that YouTube.com could be used to investigate recurrence rates following successful treatment.
Therefore, the aim of this study was to utilize YouTube.com to evaluate the efficacy of blunt force as a treatment modality for disrupting ganglion cysts.
Patients and Methods
We obtained institutional review board exemption before commencing the study. A retrospective analysis was done by accessing the website YouTube.com between July 1, 2013 and July 14, 2013 and searching combinations of the following terms: bump, ganglion, cyst, pop, and book. We reviewed all videos for the depiction of an attempt to disrupt a ganglion cyst of the wrist, either volar or dorsal, by blunt force. A video met inclusion criteria if it showcased an attempt to pop a cyst of the wrist using blunt force. Once we identified the videos, we recorded data on the location of the cyst (dorsal vs. volar) as well as the effectiveness (ability of blunt force to eliminate mass) of the treatment.
In addition to reviewing the videos, each potential study candidate was contacted through YouTube’s e-mail server up to three times regarding the purpose of the study. In the e-mail, they were given a link to an online patient questionnaire. Demographic data, including age, gender, and handedness, were recorded (Table 1). In addition, questions regarding outcomes following attempted treatment of the ganglion cyst were recorded. Participants were asked to include the URL of their YouTube video.
Table 1.
Questionnaire to YouTube contributors
| Question | Answer choices | Answers |
|---|---|---|
| What is your age? | Open-ended | Mean 32 Range 16–49 |
| What is your gender? | Male | N = 23 (61%) |
| Female | N = 15 (39%) | |
| Are you right handed or left handed? | Right | N = 35 (92%) |
| Left | N = 3 (8%) | |
| On which hand did you have the ganglion/bible cyst? | Same hand | N = 20 (56%) |
| Different hand | N = 18 (44%) | |
| What did you use to pop your cyst? | Open-ended | |
| Did it work? | Yes | N = 38 |
| No | N = 0 | |
| How many tries did it take to successfully pop the cyst? | Open-ended | Mean 1.6 Range 1–5 |
| Did the cyst recur? | Yes | N = 16 |
| No | N = 22 | |
| If this cyst did recur, how long did it take? | Open-ended | Mean 8months Range 1week–3years |
| Did you undergo any previous or subsequent medical treatment? (e.g., surgical excision or aspiration) | Yes | N = 3 (8%) |
| No | N = 35 (92%) | |
| If so, what was it? | Open-ended | Aspiration prior to blunt force destruction (N = 3) |
| Is there anything else you feel that we should know? | Open-ended |
Summary of questions asked to YouTube contributors
Search queries yielded a total of 214 videos that depicted an individual attempting to disrupt a cyst with blunt force. The reviewers analyzed these videos, and the respective contributors were contacted. The 214 videos had a total of 1,008,913 views. In the 214 videos, 43% were female and 57% were male. One hundred and seventy-five (82%) of the wrist cysts were on the dorsal and 39 (18%) were volar.
The 214 contributors contacted, and 38 responded to the survey request (18% response rate). Twenty-three were male, and 15 were female. The mean age was 32 years (range 16–49). Thirty-five were right-handed, and three were left-handed. Twenty (56%) had the cyst on their dominant hand.
Results
Blunt force disruption of the cyst was judged effective following review of the videos and survey responses. The average number of blunt forces required to disrupt the cyst, based on review of video, was 1.77 (range 1–7). Eighty three percent were observed to have immediate and complete resolution.
All survey respondents found the blunt force effective in immediate elimination of the cyst in an average of 1.6 attempts (range 1–5), which was confirmed by observation of videos. Thirty-seven reported that the mechanism of blunt force was a book. One reported using a frying pan. A majority (N = 22, 58%) reported no recurrence since the initial disruption of the cyst. Of those who reported a recurrence (N = 16), the mean time to recurrence was 8 months (range 1 week–3 years). Of those that did not report recurrence, the mean time since treatment was 24 months (N = 12, range = 4–39). No participants reported any complications as a result of the procedure. Three participants had previously been treated. One self-treated with a sterile piercing needle, one had it aspirated by a medical professional, and one had it surgically excised. No one reported receiving treatment after blunt force. Notably, in the open-ended question inquiring about any other relevant information, four of the participants stated that their primary care doctor had suggested this treatment, and two stated they tried this method because their primary doctor stated that current treatments have high recurrence rates.
Discussion
Ganglion cysts are the most common soft tissue tumors of the hand and wrist. There is extensive literature describing the recurrence and complications rates of aspiration, open excision, and arthroscopic excision of the masses. However, there has been little investigation of the effectiveness of blunt force. This study aims to evaluate the efficacy of blunt force as a treatment modality for disrupting ganglion cysts.
Our study has limitations and weaknesses. There was selection bias in the sampled population. In order to post these videos, participants need to have had access to the internet and familiarity with YouTube.com. Those who found the treatment to be effective may be more likely to upload a video depicting their treatment and may be more willing to discuss their treatment. There may be an additional sampling bias given the low response rate. However, it is important to note that patients needed to access the YouTube message server in order to response. A recent study showed that only 24% of YouTube users are considered “active” [17], and one can presume even fewer utilize the messaging function of the website. In addition, it is worth noting that the patient’s whom we defined as having a ganglion cyst was self-reported and confirmed via video. This is in contrast to the studies to which we compare our results, which reported physician-diagnosed ganglion cysts. These limitations are exacerbated by the retrospective nature of the study and the reliance of participant response for data. Despite these drawbacks, YouTube.com provided us with a glimpse of how patients self-treat their ganglion cysts and how effective they feel this treatment is.
Our survey found that most responders reported immediate resolution of the cyst after application of a blunt force. A minority of patients reported a recurrence, which occurred after an average of 8 months. No participants reported any complications from the blunt force applied.
Previous studies suggest that approximately 45% of ganglion cysts resolve spontaneously after a mean follow-up of 64 months (Table 2) [2, 6, 7, 16, 26, 28]. For those that do not, patients are often offered an attempt at aspiration, which is currently the mainstay of nonsurgical treatment [11]. However, aspiration has shown limited efficacy with a recurrence rate of 53% (Table 3) [6, 12, 19, 22, 24, 29]. Furthermore, Dias et al. report that 5% of patients suffer complications like numbness, infection, and hypertrophic scar [6]. Zubowicz et al. estimate that aspiration costs over 32,000 US dollars per 100 patients [29].
Table 2.
Ganglion cyst spontaneous resolution
| Author | Patients (N) | Spontaneous resolution (N) | Follow-up (months) |
|---|---|---|---|
| Dias et al. [8] | 55 | 23 (41.8%) | 70 |
| Zachariae and Vibe-Hansen [12] | 101 | 40 (39.6%) | 72 |
| Westbrook et al. [11] | 11 | 5 (45.5%) | 4 |
| McEvedy [10] | 21 | 10 (47.6%) | 144 |
| Carp and Stout [6] | 12 | 7 (58.3%) | 36 |
| Dias and Buch [7] | 38 | 20 (52.6%) | 60 |
| Overall | 238 | 105 (44.1%) | 64.3 |
A summary of published ganglion cyst spontaneous resolution rates. The frequency weighted average was 44.1%
Table 3.
Ganglion cyst recurrence following aspiration
| Author | Number of Patients | Recurrences |
|---|---|---|
| Ho et al.[14] | 78 | 45 (58%) |
| Nield and Evans [17] | 34 | 20 (58.8%) |
| Zubowicz [18] | 47 | 12 (25.5%) |
| Dias and Buch [7] | 39 | 19 (48.7%) |
| Stephen et al.[16] | 198 | 96 (48.5%) |
| Rollins et al.[15] | 21 | 13 (61.9%) |
| Overall | 270 | 144 (53.3%) |
A summary of published recurrence rates after aspiration of ganglion cysts of the wrist. The frequency weighted average was 53.3%
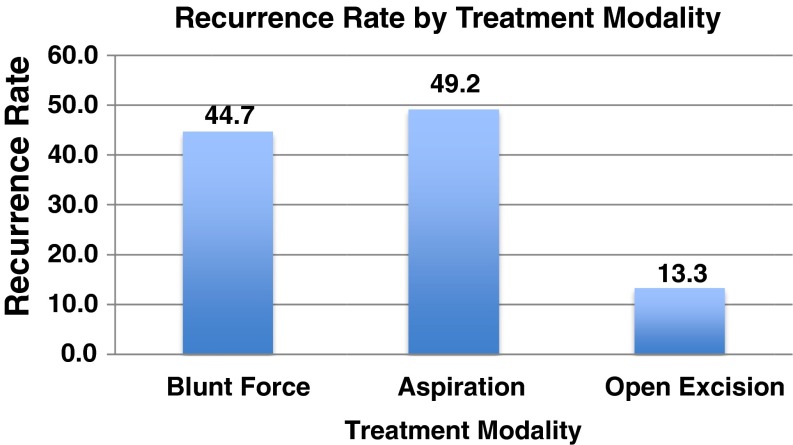
Surgical treatment produces the lowest recurrence rate (Fig. 1), with an average of 13% (Table 4), but has a higher incidence of complications [1, 3, 4, 8, 12–15, 20–22] and cost. Zubowicz et al. estimated surgical management of patients costs 120,000 US dollars per 100 patients [29]. Given the potential for nonoperative solutions for this relatively benign condition, McEvedy argued open excisions “take up the time of the competent surgeons who might be more usefully engaged [16].”
Fig. 1.
Recurrence rate by treatment modality.
Table 4.
Ganglion cyst recurrence following surgical excision
| Author | Number of Patients | Number of patients with recurrence |
|---|---|---|
| Ho et. al [14] | 103 | 40 (39.0%) |
| Faithful and Seeto [26] | 59 | 6 (10.0%) |
| Clay and Clement [22] | 62 | 2 (3.2%) |
| Kang et al. [21] | 23 | 2 (8.7%) |
| Povlsen and Tacakkolizadeh [20] | 8 | 0 (0%) |
| Angelides [27] | 346 | 3 (0.9%) |
| Rocchi [19] | 15 | 1 (6.7%) |
| Craik et al. [25] | 48 | 4 (8.3%) |
| Lidder et al. [24] | 117 | 49 (48.9%) |
| Khan and Hayat [23] | 18 | 1 (5.6%) |
| Rollins et al. [15] | 26 | 2 (7.7%) |
| Overall | 825 | 110 (13.3%) |
Summary of published recurrence rates after open-excision of ganglion cysts of the wrist. The frequency weighted average was 13.3%
While the current study had several limitations, we hope it stimulates interest and further study of this treatment modality. We hope future studies can observe the treatment in a more controlled manner, allowing comparison of complication and recurrence rates in a setting that parallels those of past studies of surgical excision and aspiration. Furthermore, we hope future studies examine primary care physician opinions of our current treatments. Our survey showed that some participants were advised to self-treat by their primary care physicians, who cited high recurrence rates and unnecessary costs of current treatment options. We need to ensure that our patients’ first-line providers are appropriately educated and are able to give patients the most up-to-date and accurate information.
With internet use for medical advice growing more than ever, it is important that we study the techniques most available to the general population so that we may effectively counsel them. YouTube.com provided a means of investigating a treatment modality for wrist ganglia that has previously been seldom reported. To our knowledge, the present study is the first evaluation of blunt force destruction since Nelson et al. in 1972. In this retrospective review, we found that patients are reporting results similar to those of currently accepted treatment modalities with lower cost.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 98 kb)
Compliance with Ethical Standards
Conflict of Interest
Nikunj N. Trivedi, BS, Joseph J. Schreiber, MD, and Aaron Daluiski, MD, have declared that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level IV case series
Work was performed at Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, NY.
References
- 1.Angelides AC, Wallace PF. The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg Am. 1976;1(3):228–235. doi: 10.1016/S0363-5023(76)80042-1. [DOI] [PubMed] [Google Scholar]
- 2.Carp L, Stout AP. Branchial anomolies and neoplasms: A report of thirty-two cases with follow-up results. Ann Surg. 1928;87(2):186–209. doi: 10.1097/00000658-192802000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clay NR, Clement DA. The treatment of dorsal wrist ganglia by radical excision. J Hand Surg Br. 1988;13(2):187–191. doi: 10.1016/0266-7681(88)90135-0. [DOI] [PubMed] [Google Scholar]
- 4.Craik JD, Walsh SP. Patient outcomes following wrist ganglion excision surgery. J Hand Surg Eur Vol. 2012;37(7):673–677. doi: 10.1177/1753193411434376. [DOI] [PubMed] [Google Scholar]
- 5.Dacombe PJ, Robinson J. Falling up the stairs: the equivalent of ‘bashing it with a bible’ for an ACL ganglion cyst of the knee. BMJ Case Rep. 2012; 2012. [DOI] [PMC free article] [PubMed]
- 6.Dias J, Buch K. Palmar wrist ganglion: does intervention improve outcome? A prospective study of the natural history and patient-reported treatment outcomes. J Hand Surg Br. 2003;28(2):172–176. doi: 10.1016/S0266-7681(02)00365-0. [DOI] [PubMed] [Google Scholar]
- 7.Dias JJ, Dhukaram V, Kumar P. The natural history of untreated dorsal wrist ganglia and patient reported outcome 6 years after intervention. J Hand Surg Eur Vol. 2007;32(5):502–508. doi: 10.1016/j.jhse.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Faithfull DK, Seeto BG. The simple wrist ganglion--more than a minor surgical procedure? Hand Surg. 2000;5(2):139–143. doi: 10.1142/S0218810400000235. [DOI] [PubMed] [Google Scholar]
- 9.Ganglion Cysts. http://www.eatonhand.com/hw/hw013.htm. Accessed August 22, 2013.
- 10.Gant J, Ruff M, Janz BA. Wrist ganglions. J Hand Surg Am. 2011;36(3):510–512. doi: 10.1016/j.jhsa.2010.11.048. [DOI] [PubMed] [Google Scholar]
- 11.Gude W, Morelli V. Ganglion cysts of the wrist: pathophysiology, clinical picture, and management. Curr Rev Musculoskelet Med. 2008;1(3–4):205–211. doi: 10.1007/s12178-008-9033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ho MW, Singh R, Dias JJ. Re: The natural history of untreated dorsal wrist ganglia and patient reported outcome 6 years after intervention. J Hand Surg Eur Vol. 2008;33(3):398–399. doi: 10.1177/1753193408090093. [DOI] [PubMed] [Google Scholar]
- 13.Kang L, Akelman E, Weiss AP. Arthroscopic versus open dorsal ganglion excision: a prospective, randomized comparison of rates of recurrence and of residual pain. J Hand Surg Am. 2008;33(4):471–475. doi: 10.1016/j.jhsa.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 14.Khan PS, Hayat H. Surgical excision versus aspiration combined with intralesional triamcinolone acetonide injection plus wrist immobilization therapy in the treatment of dorsal wrist ganglion; a randomized controlled trial. J Hand Microsurg. 2011;3(2):55–57. doi: 10.1007/s12593-011-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lidder S, Ranawat V, Ahrens P. Surgical excision of wrist ganglia; literature review and nine-year retrospective study of recurrence and patient satisfaction. Orthop Rev (Pavia) 2009;1(1):e5. doi: 10.4081/or.2009.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McEvedy B. The simple ganglion: a review of modes of treatment and an explanation of the frequent failures of surgery. Lancet. 1954;266(6803):135–6. doi: 10.1016/S0140-6736(54)90983-6. [DOI] [PubMed] [Google Scholar]
- 17.McGrath F. YouTube has 3.5x more Visitors than Active Usors. 2015; http://www.globalwebindex.net/blog/youtube-has-3x-more-visitors-than-active-users. Accessed May 28, 2015.
- 18.Nelson CL, Sawmiller S, Phalen GS. Ganglions of the wrist and hand. J Bone Joint Surg Am. 1972;54(7):1459–1464. [PubMed] [Google Scholar]
- 19.Nield DV, Evans DM. Aspiration of ganglia. J Hand Surg Br. 1986;11(2):264. doi: 10.1016/0266-7681(86)90278-0. [DOI] [PubMed] [Google Scholar]
- 20.Povlsen B, Tavakkolizadeh A. Outcome of surgery in patients with painful dorsal wrist ganglia and arthroscopic confirmed ligament injury: a five-year follow-up. Hand Surg. 2004; 9(2): 171-173. [DOI] [PubMed]
- 21.Rocchi L, Canal A, Fanfani F, Catalano F. Articular ganglia of the volar aspect of the wrist: arthroscopic resection compared with open excision. A prospective randomised study. Scand J Plast Reconstr Surg Hand Surg. 2008; 42(5): 253-259. [DOI] [PubMed]
- 22.Rollins KE, Ollivere BJ, Johnston P. Predicting successful outcomes of wrist and finger Ganglia. Hand Surg. 2013;18(1):41–44. doi: 10.1142/S021881041350007X. [DOI] [PubMed] [Google Scholar]
- 23.Schreiber JJ, Warren RF, Hotchkiss RN, Daluiski A. An online video investigation into the mechanism of elbow dislocation. J Hand Surg Am. 2013;38(3):488–494. doi: 10.1016/j.jhsa.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 24.Stephen A, Lyons A, Davis TR. A prospective study of two conservative treatments for ganglia of the wrist. J Hand Surg Br. 1999;24(1):104–5. doi: 10.1016/S0266-7681(99)90051-7. [DOI] [PubMed] [Google Scholar]
- 25.Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop Surg. 1999;7(4):231–238. doi: 10.5435/00124635-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Westbrook AP, Stephen AB, Oni J, Davis TR. Ganglia: the patient’s perception. J Hand Surg Br. 2000;25(6):566–567. doi: 10.1054/jhsb.2000.0504. [DOI] [PubMed] [Google Scholar]
- 27.YouTube. YouTube. About Ushttp://www.youtube.com/yt/about/. Accessed July 3, 2013.
- 28.Zachariae L, Vibe-Hansen H. Ganglia. Recurrence rate elucidated by a follow-up of 347 operated cases. Acta Chir Scand. 1973; 139(7): 625-628. [PubMed]
- 29.Zubowicz V, Ishii CH. Management of ganglion cysts of the hand by simple aspiration. J Hand Surg Am. 1987;12(4):618–2. doi: 10.1016/S0363-5023(87)80221-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 98 kb)