Abstract
This is a review education paper on the current ophthalmology simulators utilized worldwide for undergraduate and postgraduate training. At present, various simulators such as the EYE Exam Simulator (Kyoto Kagaku Co. Ltd., Kyoto, Japan), Eyesi direct ophthalmoscope simulator (VRmagic, GmbH, Mannheim, Germany), Eyesi indirect ophthalmoscope simulator (VRmagic, GmbH, Mannheim, Germany) and Eyesi cataract simulators (VRmagic, GmbH, Mannheim, Germany). These simulators are thought to be able to reduce the initial learning curve for the ophthalmology training but further research will need to be conducted to assess the effectiveness of the simulation-assisted Ophthalmology training. Future research will be of great value to assess the medical students and residents' responses and performance regarding the usefulness of the individual eye simulator.
Keywords: ophthalmology simulator, cataract simulator, ophthalmology residency training, direct ophthalmoscopy simulator
INTRODUCTION
To date, the use of simulation is becoming increasingly popular in ophthalmology[1]. It has been shown that technology-enhanced simulation training is associated with large effects for outcomes of knowledge, skills and behaviors and moderate effects for patient-related outcomes[2]. In the past, the clinical teaching was often conducted using real patients and this method sometimes can be very challenging due to patients' comfort or time constraint in a busy clinic. The change of this teaching paradigm mainly arises from various factors including increased public expectation on doctors' performance in diagnosis and management, changes in working practice, advancement in technological developments and opportunities and shortening of the training time for the residents.
Due to the increased health consciousness and awareness in the public, many patients will research their conditions extensively on the internet prior to their presentation to the hospital. They often expect the doctors to know what the immediate clinical findings and diagnoses are instead of being treated as “guinea pigs” for those who have just entered the residency training or still in the medical schools. Some of them are often shocked and upset to learn that the examiners are conducting the clinical examination for the first time on them. The simulations are good platforms for the medical students and residents to practice and refine their clinical or surgical technique as they can make mistakes on simulations without jeopardizing patients' care[3]–[4]. It is a dress rehearsal for a real event, during which mistakes can be made and lessons learned[5]. Nevertheless, the simulations should only be used as a method to enhance and supplement the learning experience as it will not supplant the learning experience from real patients in the clinical setting[6].
Various forms of medical simulation such as wet laboratories, mannequins[7], animal and cadavers[8], simulated patients, simulated hospital environments, simulated laser or surgical models[9]–[10], virtual reality[11]–[19] are designed to enhance the students' and residents' learning experience. The purpose of this article is to describe the various ophthalmology simulators that could be potentially utilized for the medical students and ophthalmology residency training.
Direct Fundoscopy Examination
Direct ophthalmoscopy or fundoscopy is a fundus examination skill that has been incorporated into medical school curriculum as it is an important clinical skill that allows non-ophthalmology trained physicians to diagnose retinal pathology without needing to utilize expensive equipment such as slit lamp biomicroscopy with hand held lends or indirect BIO ophthalmoscopy[20]–[23]. Through the direct ophthalmoscopic examination, one can detect many of the sight-threatening conditions (e.g. proliferative diabetic retinopathy, glaucomatous optic neuropathy) and life-threatening conditions (e.g. optic disc swelling secondary to space occupying lesions, malignant hypertension, meningitis and etc.). However, many students and physicians still had major difficulties to perform a proficient fundsocopy examination[24]–[25]. Besides, it is difficult to teach this skill effectively during the initial phase and for the tutors, it is hard to guide the students while they are performing the examination due to lack of monitor screen attached to the direct ophthalmoscope.
Several methods have been described to supplement the training of medical students in acquiring this skill. The EYE Exam Simulator (Kyoto Kagaku Co. Ltd., Kyoto, Japan) is an innovative mannequin (Figure 1) for fundus examination, designed to allow examination of fundus using the physician's own ophthalmoscope. The pupil aperture is adjustable to simulate both dilated and undilated pupils and the image of the fundus is created by a set of slides depicting common pathology (Figure 2). The use of this simulator has been shown to correlate with users' experience[26] and the accuracy of the examination decreased with smaller pupil diameters of 2 and 3.5 mm (as opposed to more than 5 mm). It will be of great value to utilize this device in the practical examination to evaluate direct ophthalmoscopy skills of medical students and junior residents.
Figure 1. The EYE Exam Simulator (Kyoto Kagaku Co. Ltd., Kyoto, Japan).
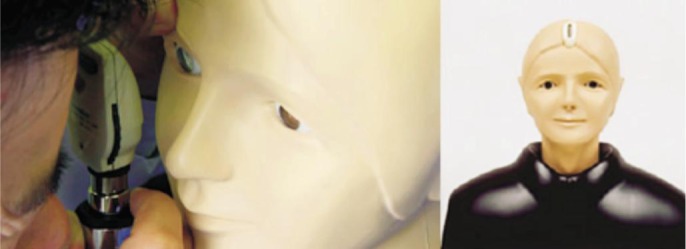
Figure 2. Changes of the retinal pathologies using different slides in the EYE Exam Simulator (Kyoto Kagaku Co. Ltd., Kyoto, Japan).

In addition, Eyesi direct ophthalmoscope simulator (VRmagic, GmbH, Mannheim, Germany) is a new device that has recently been released into the market (Figure 3). It uses virtual reality to enhance the teaching of the essential diagnostic skill of direct ophthalmoscopy. The simulator has an incorporated curriculum that allows independent learning by the trainee. It is able to provide prompt feedback on the user's view, the examined area and whether the abnormal retinal pathology has been detected in the simulator. From the monitor screen connected to the direct ophthalmoscope, the trainer can also evaluate and offer guidance during the process of examination. In training mode, the findings will be displayed immediately on the screen as soon as they have been detected and if the trainee tap on the screen, some relevant information related to the pathology will be shown. On the other hand, this simulator can also be utilized for assessment purposes with the quiz mode available in the device and the result can be generated at the end of the exercise. Whether the skills acquired with the use of these simulators are translated into clinical practice has yet to be proven. Further research can be conducted to assess the medical students' and physicians' confidence and competence level in performing direct ophthalmoscopy. Apart from the abovementioned methods, the Wisconsin School of Medicine has also described a method for direct ophthalmoscopy training purposes using a canister or a tin can to simulate an eye-with a fundus photograph stuck to its base, and a hole drilled into its cap to simulate a pupil[27]. It has been found to be an inexpensive but effective way in complementing the direct ophthalmoscopy skills, as compared to the mannequins and Eyesi direct ophthalmoscope simulators.
Figure 3. Eyesi direct (VRmagic, GmbH, Mannheim, Germany).

Indirect BIO Ophthalmoscope
The indirect ophthalmoscopy, first devised in 1861 by Felix Giraud Teulon, is an important diagnostic tool for ophthalmologists. It permits viewing of the fundus at a wider angle which allows for thorough examination of the peripheral retina and also viewing through lens opacities. Unlike the direct ophthalmoscope, the indirect ophthalmoscopy confers binocularity by the use of mirrors in the instrument to reduce the pupillary distance of the observer to about 15 mm. The instrument is attached onto a headband or spectacle frame worn by the examiner, and with the use of a condensing lens (usually +20 D to +30 D) held in front of the patient's eye, an aerial image of the fundus is formed, magnified, inverted and laterally reversed. Proficiency in the indirect ophthalmoscopy requires painstaking practice and junior ophthalmology residents often struggle with maintaining stability of the instrument and lens and the patient's eye and difficulty in lens control[28].
In the past decades, several training methods, both simple and complex, have been developed to aid with the training of junior residents in mastering the indirect ophthalmoscopy[29]–[30]. A simple inexpensive setup with the use of a rubber ball or marble held in place by a Styrofoam head carved out to house a slide holder has been used to simulate the eye and its anatomic obstacles (e.g. the eyelids and nose) with the insertion of wide-angle clinical photographs consisting of various retinal pathologies[31].
More recently, the Eyesi indirect ophthalmoscope simulator (Figure 4) has been invented to provide residents with an augmented reality training which encompasses elements of a physical real-world environment (hand-to-head coordination, anatomic obstacles) supplemented by a computer generated input (digital fundus photograph, real-time evaluation andetc)[32]. Eyesi indirect ophthalmoscope can provide the trainee evaluations of both procedural and diagnostic skills by assessing the time needed for examination, and percentage of retina examined properly, which translates into critical information in assessing a trainee's proficiency in the indirect ophthalmoscope.
Figure 4. Eyesi indirect (VRmagic, GmbH, Mannheim, Germany).
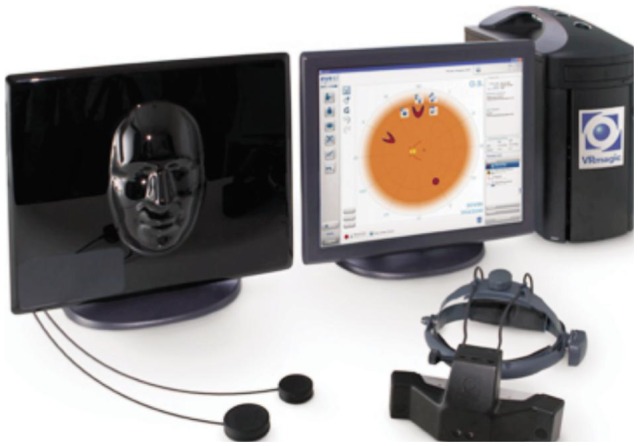
It is a good educational tool given its ability to educate trainees on specific clinical findings for a given pathology and through a multiple-choice diagnosis specification tool, trainees are made to describe their findings in detail. The information captured will then be evaluated by the system for immediate feedback to the trainee. The information also allows the educator to assess the trainee's progress as all performance data is stored in the Eyesi Indirect database.
Leitritz et al[33] conducted a study involving 37 medical students with no prior experience in performing binocular indirect ophthalmoscopy and randomised them into either training in the conventional way, or with augmented reality ophthalmoscopy (Eyesi indirect). It has been shown that the group of medical with single training using the augmented reality ophthalmoscopy is better in improving ophthalmoscopy skills[33]. Despite the study limitations (small number of students and absence of crossover design), it holds promise that augmented reality training provides an efficient learning platform for medical students interested in Ophthalmology and junior residents. The question, however, remains if the use of such expensive simulators is translated into measurable clinical advantages and thus, further studies are required to determine the efficiency and effectiveness of these simulators and its translation into clinical practice.
Cataract Simulator
Phacoemulsification training has always been challenging for the junior residents during the initial period[34]–[36]. Cataract simulators have been shown to offer various training advantages to the ophthalmology residents[37] and these include shortening the time of feeling confident to operate operation duration[34],[38] and improvement on capsulorrhexis technique[39]. Several types of cataract simulators are currently available in the market: Eyesi (VRmagic, GmbH, Mannheim, Germany), PhacoVision (Melerit Medical), and MicrovisTouch (ImmersiveTouch)[13].
The cataract simulator-Eyesi (VRmagic, GmbH, Mannheim, Germany) (figure 5) is a high-end virtual reality simulator for intraocular surgical training and it simulates a life-like learning environment[12],[40]. The simulator consists of different parts including microscope, handheld instruments, a mannequin head with a virtual eye, foot pedals for microscope and phacoemulsification machine and a touch-screen monitor on which a supervisor can watch the surgeon perform. For the hand pieces, they are all colored-coded using optical tracking systems for conversion of movement to electrical signals then sent to the simulator after being inserted into the artificial eye. The presence of sophisticated algorithms in the machine helps to create accurate tissue characteristics and hence, allowing simulation of procedures such as capsulorrhexis creation[41].
Figure 5. Eyesi cataract simulator (VRmagic, GmbH, Mannheim, Germany).

In order to offer an immersive surgical simulation environment, the Eyesi consists of different learning modules including anti-tremor training, bimanual training, capsulorhexis, cracking and chopping training, forceps training, hydrodissection maneuvers, intracapsular anti-tremor training and navigation training, intraocular lens insertion, irrigation and aspiration, navigation training, phacoemulsification chopping training and phacoemulsification divide and conquer. The setting of the machine can also be modified to simulate different surgical environment using various parameters including phacoemulsification power, vacuum level and flow rate. In order to assess the residents' performance on the simulator, the training history including the number of attempts and the scores for a particular module, time taken to complete a task, incidence of corneal touch and etc. can be extracted from the machine.
Limited publication is available on Phacovision and MicrovisTouch. Compared to Eyesi and Phacovision, MircovisTouch, MicrovisTouch offers users' tactile feedback interface, hence providing them with more realistic operative experience[13]. In addition, it also provides a virtual experience that includes the instruments, head and eye of the patients. The simulator head and eye in Eyesi and Phacovision are immobile and this does not simulate the real experience for cataract surgery.
A recent systematic review showed that the methodology and validation of various ophthalmology simulators is yet to be improved[8]. Most of the trials did not utilize the validity of the simulation models for assessment purposes. The efficacy of training models only satisfy Kirkpatrick model 1 or 2, mainly evaluating the trainees' satisfaction with the training model and the extent of the training increased skills. It is recommended that the skills assessment should be evaluated using different models with validated scoring system to ensure appropriate interpretation of results[8].
In conclusion, the use of simulation carries substantial advantages in the education of medical students and in-training ophthalmology residents, especially for those who are relatively junior. More research should be conducted to assess the clinical and cost-effectiveness of these simulators in enhancing the quality of the clinical service as well as learning experience of the juniors.
Acknowledgments
Conflicts of Interest: Ting DSW, None; Sim SSKP, None; Yau CWL, None; Rosman M, None; Aw AT, None; Yeo IYS, None.
REFERENCES
- 1.Wallace BS, Sabates NR. Simulation in ophthalmology. Mo Med. 2013;110(2):152–153. [PMC free article] [PubMed] [Google Scholar]
- 2.Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, Erwin PJ, Hamstra SJ. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978–988. doi: 10.1001/jama.2011.1234. [DOI] [PubMed] [Google Scholar]
- 3.Gillan SN, Saleh GM. Ophthalmic surgical simulation: a new era. JAMA ophthalmol. 2013;131(12):1623–1624. doi: 10.1001/jamaophthalmol.2013.1011. [DOI] [PubMed] [Google Scholar]
- 4.Grodin MH, Johnson TM, Acree JL, Glaser BM. Ophthalmic surgical training: a curriculum to enhance surgical simulation. Retina. 2008;28(10):1509–1514. doi: 10.1097/IAE.0b013e31818464ff. [DOI] [PubMed] [Google Scholar]
- 5.Deanery L. Using simulation in clinical education. URL: http://www.faculty.londondeanery.ac.uk/e-learning/using-simulation-in-clinical-education.
- 6.Solverson DJ, Mazzoli RA, Raymond WR, Nelson ML, Hansen EA, Torres MF, Bhandari A, Hartranft CD. Virtual reality simulation in acquiring and differentiating basic ophthalmic microsurgical skills. Simul healthc. 2009;4(2):98–103. doi: 10.1097/SIH.0b013e318195419e. [DOI] [PubMed] [Google Scholar]
- 7.Xie P, Hu Z, Zhang X, Li X, Gao Z, Yuan D, Liu Q. Application of 3-dimensional printing technology to construct an eye model for fundus viewing study. PLoS One. 2014;9(11):e109373. doi: 10.1371/journal.pone.0109373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomsen AS, Subhi Y, Kiilgaard JF, la Cour M, Konge L. Update on simulation-based surgical training and assessment in ophthalmology: a systematic review. Ophthalmology. 2015;122(6):1111–1130.e1. doi: 10.1016/j.ophtha.2015.02.028. [DOI] [PubMed] [Google Scholar]
- 9.Moisseiev E, Michaeli A. Simulation of neodymium:YAG posterior capsulotomy for ophthalmologists in training. J Cataract Refract Surg. 2014;40(2):175–178. doi: 10.1016/j.jcrs.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Selvander M, Asman P. Stereoacuity and intraocular surgical skill: effect of stereoacuity level on virtual reality intraocular surgical performance. J Cataract Refract Surg. 2011;37(12):2188–2193. doi: 10.1016/j.jcrs.2011.05.048. [DOI] [PubMed] [Google Scholar]
- 11.Colt HG, Crawford SW, Galbraith O., 3rd Virtual reality bronchoscopy simulation: a revolution in procedural training. Chest. 2001;120(4):1333–1339. doi: 10.1378/chest.120.4.1333. [DOI] [PubMed] [Google Scholar]
- 12.Saleh GM, Theodoraki K, Gillan S, Sullivan P, O'Sullivan F, Hussain B, Bunce C, Athanasiadis I. The development of a virtual reality training programme for ophthalmology: repeatability and reproducibility (part of the International Forum for Ophthalmic Simulation Studies) Eye (Lond) 2013;27(11):1269–1274. doi: 10.1038/eye.2013.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sikder S, Tuwairqi K, Al-Kahtani E, Myers WG, Banerjee P. Surgical simulators in cataract surgery training. Br J Ophthalmol. 2014;98(2):154–158. doi: 10.1136/bjophthalmol-2013-303700. [DOI] [PubMed] [Google Scholar]
- 14.Lowry EA, Porco TC, Naseri A. Cost analysis of virtual-reality phacoemulsification simulation in ophthalmology training programs. J Cataract Refract Surg. 2013;39(10):1616–1617. doi: 10.1016/j.jcrs.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 15.Lam CK, Sundaraj K, Sulaiman MN. A systematic review of phacoemulsification cataract surgery in virtual reality simulators. Medicina (Kaunas) 2013;49(1):1–8. [PubMed] [Google Scholar]
- 16.Baxter JM, Lee R, Sharp JA, Foss AJ, Intensive Cataract Training Study Group Intensive cataract training: a novel approach. Eye (Lond) 2013;27(6):742–746. doi: 10.1038/eye.2013.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yong JJ, Migliori ME, Greenberg PB. A novel preclinical course in ophthalmology and ophthalmic virtual surgery. Med Health R I. 2012;95(11):345–348. [PubMed] [Google Scholar]
- 18.Le TD, Adatia FA, Lam WC. Virtual reality ophthalmic surgical simulation as a feasible training and assessment tool: results of a multicentre study. Can J Ophthalmol. 2011;46(1):56–60. doi: 10.3129/i10-051. [DOI] [PubMed] [Google Scholar]
- 19.Selvander M, Asman P. Virtual reality cataract surgery training: learning curves and concurrent validity. Acta Ophthalmol. 2012;90(5):412–417. doi: 10.1111/j.1755-3768.2010.02028.x. [DOI] [PubMed] [Google Scholar]
- 20.Ricci LH, Ferraz CA. Simulation models applied to practical learning and skill enhancement in direct and indirect ophthalmoscopy: a review. Arq Bras Oftalmol. 2014;77(5):334–338. doi: 10.5935/0004-2749.20140084. [DOI] [PubMed] [Google Scholar]
- 21.Kelly LP, Garza PS, Bruce BB, Graubart EB, Newman NJ, Biousse V. Teaching ophthalmoscopy to medical students (the TOTeMS study) Am J Ophthalmol. 2013;156(5):1056–1061.e10. doi: 10.1016/j.ajo.2013.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCarthy DM, Leonard HR, Vozenilek JA. A new tool for testing and training ophthalmoscopic skills. J Grad Med Educ. 2012;4(1):92–96. doi: 10.4300/JGME-D-11-00052.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Podbielski DW, Noble J, Gill HS, Sit M, Lam WC. A comparison of hand- and foot-activated surgical tools in simulated ophthalmic surgery. Can J Ophthalmol. 2012;47(5):414–417. doi: 10.1016/j.jcjo.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Wu EH, Fagan MJ, Reinert SE, Diaz JA. Self-confidence in and perceived utility of the physical examination: a comparison of medical students, residents, and faculty internists. J Gen Intern Med. 2007;22(12):1725–1730. doi: 10.1007/s11606-007-0409-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roberts E, Morgan R, King D, Clerkin L. Funduscopy: a forgotten art? Postgrad Med J. 1999;75(883):282–284. doi: 10.1136/pgmj.75.883.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akaishi Y, Otaki J, Takahashi O, Breugelmans R, Kojima K, Seki M, Komoda T, Nagata-Kobayashi S, Izumi M. Validity of direct ophthalmoscopy skill evaluation with ocular fundus examination simulators. Can J Ophthalmol. 2014;49(4):377–381. doi: 10.1016/j.jcjo.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Hoeg TB, Sheth BP, Bragg DS, Kivlin JD. Evaluation of a tool to teach medical students direct ophthalmoscopy. WMJ. 2009;108(1):24–26. [PubMed] [Google Scholar]
- 28.Kumar KS, Shetty KB. A new model eye system for practicing indirect ophthalmoscopy. Indian J Ophthalmol. 1996;44(4):233–234. [PubMed] [Google Scholar]
- 29.Ing EB, Ing TG. A method of teaching indirect ophthalmoscopy to beginning residents. Can J Ophthalmol. 1992;27(4):166–167. [PubMed] [Google Scholar]
- 30.Bartner H, Paton D. An improved model for instruction in binocular indirect ophthalmoscopy. Arch Ophthalmol. 1971;85(5):530–533. doi: 10.1001/archopht.1971.00990050532002. [DOI] [PubMed] [Google Scholar]
- 31.Dodaro NR, Maxwell DP., Jr An eye for an eye. A simplified model for teaching. Arch Ophthalmol. 1995;113(6):824–826. doi: 10.1001/archopht.1995.01100060150051. [DOI] [PubMed] [Google Scholar]
- 32.Schuppe O, Wagner C, Koch F, Manner R. EYESi ophthalmoscope - a simulator for indirect ophthalmoscopic examinations. Stud Health Technol Inform. 2009;142:295–300. [PubMed] [Google Scholar]
- 33.Leitritz MA, Ziemssen F, Suesskind D, Partsch M, Voykov B, Bartz-Schmidt KU, Szurman GB. Critical evaluation of the usability of augmented reality ophthalmoscopy for the training of inexperienced examiners. Retina. 2014;34(4):785–791. doi: 10.1097/IAE.0b013e3182a2e75d. [DOI] [PubMed] [Google Scholar]
- 34.Pokroy R, Du E, Alzaga A, Khodadadeh S, Steen D, Bachynski B, Edwards P. Impact of simulator training on resident cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2013;251(3):777–781. doi: 10.1007/s00417-012-2160-z. [DOI] [PubMed] [Google Scholar]
- 35.Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg. 2011;37(10):1756–1761. doi: 10.1016/j.jcrs.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 36.Ament CS, Henderson BA. Optimizing resident education in cataract surgery. Curr Opin Ophthalmol. 2011;22(1):64–67. doi: 10.1097/ICU.0b013e3283415040. [DOI] [PubMed] [Google Scholar]
- 37.Daly MK, Gonzalez E, Siracuse-Lee D, Legutko PA. Efficacy of surgical simulator training versus traditional wet-lab training on operating room performance of ophthalmology residents during the capsulorhexis in cataract surgery. J Cataract Refract Surg. 2013;39(11):1734–1741. doi: 10.1016/j.jcrs.2013.05.044. [DOI] [PubMed] [Google Scholar]
- 38.Selvander M, Asman P. Ready for OR or not? Human reader supplements Eyesi scoring in cataract surgical skills assessment. Clin Ophthalmol. 2013;7:1973–1977. doi: 10.2147/OPTH.S48374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCannel CA, Reed DC, Goldman DR. Ophthalmic surgery simulator training improves resident performance of capsulorhexis in the operating room. Ophthalmology. 2013;120(12):2456–2461. doi: 10.1016/j.ophtha.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 40.Selvander M, Asman P. Cataract surgeons outperform medical students in Eyesi virtual reality cataract surgery: evidence for construct validity. Acta Ophthalmol. 2013;91(5):469–774. doi: 10.1111/j.1755-3768.2012.02440.x. [DOI] [PubMed] [Google Scholar]
- 41.Grimm J. Tearing of membranes for interactive real-time surgical training. Stud Health Technol Inform. 2005;111:153–159. [PubMed] [Google Scholar]


