Abstract
Introduction
Neuroretinitis (NR) is considered to be an inflammatory condition which is characterized by optic disc edema and, as a result, formation of a macular star figure. NR is an atypical presentation of toxoplasmosis infection, and such cases are quite rare.
Case Presentation
A 13-year-old girl presented with painless subacute visual loss in her right eye for a week at Khatam-Al-Anbia eye hospital in Mashhad, Iran. Following comprehensive evaluation, a diagnosis of toxoplasmic NR was made. The NR favorably responded to classic anti-toxoplasmosis treatment. A juxtapapillary retinochoroidal scar appeared after disc swelling resolution.
Conclusions
Although toxoplasmosis NR is rare, it should be considered in the differential diagnoses of NR.
Keywords: Neuroretinitis, Ocular Toxoplasmosis, Optic Neuropathy
1. Introduction
Neuroretinitis (NR) is considered an inflammatory condition which is characterized by optic disc edema and, as a result, formation of a macular star figure (1). This disorder is possibly caused by an infectious process affecting the disc; in other instances, a post-viral or autoimmune mechanism seems to be a more probable cause (1). Furthermore, some instances of NR have been reported to be accompanied by a wide spectrum of infectious pathogens (1).
The most common case reported so far is the result of cat scratch disease (CSD), accounting for two-thirds of cases in one study (2). However, there are other infectious etiologies of neuroretinitis, including rubeola, toxoplasmosis, herpes simplex, varicella, tuberculosis, Lyme disease, leptospirosis, syphilis, various fungi, and multiple viral illnesses (1). Additionally, sporadic cases of NR may occur owing to noninfectious forms of uveitis, such as sarcoidosis and periarteritis nodosa (3, 4). Optic disc edema with a macular star may also occur as a result of other factors such as diabetic papillopathy, hypertensive neuropathy, and anterior ischemic optic neuropathy papilledema (1).
To determine the relevant history of patients with NR, the practitioner needs to concentrate on plausible risk factors for specific infectious parameters, such as travelling to areas where Lyme disease or tuberculosis (for example) are endemic, exposure to waste material (e.g., leptospirosis), animal exposure (especially cats), and sexual contact that may have resulted in the contraction of syphilis. The clinician should investigate patients for systemic symptoms such as lymphadenopathy, headache, fever, and skin rash. Laboratory tests ought to be customized for the individuals on the basis of information from both their reported history and the examination. Serologic tests for most cases may include the fluorescent treponemal antibody absorption test (FTA-ABS), cat scratch titers (Bartonella species), and a tuberculosis skin test (purified protein derivative, or PPD) (1).
In this study, we present a case of unilateral neuroretinitis in which the serology result was apparently negative for acute infection of toxoplasmosis (negative IgM titer for toxoplasmosis, but positive for IgG). Based on anti-toxoplasma treatment that was administered for the positive IgG levels, the condition responded well with near optimal visual recovery.
2. Case Presentation
A 13-year-old girl was referred to the ophthalmic emergency department of Khatam-Al-Anbia eye hospital, Mashhad, Iran, which is affiliated with Mashhad University of Medical Sciences (MUMS), in May of 2013 with painless subacute visual loss in her right eye for one week. She denied any focal neurologic condition, pain on eye movement or ophthalmodynia, or any other systemic symptom. She also stated that she had not engaged in outdoor camping or any other related activity. Furthermore, she had no remarkable past medical and ophthalmologic history, and she had no contact or proximity to pets, especially cats.
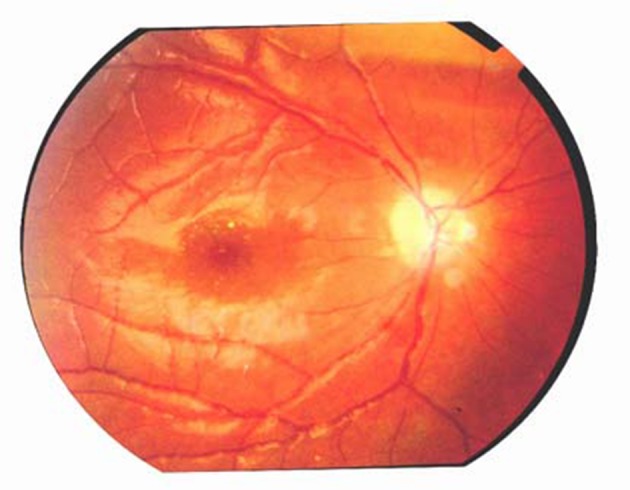
Upon examination, the best corrected visual acuity (BCVA) was 20/250 in the right eye and 20/20 in the left eye. Moreover, the patient had a grade 2+ relative afferent papillary defect (RAPD) in the right eye. An examination of the anterior segment demonstrated 2+ cells in the anterior chamber (A/C) and 1+ vitreous reaction with normal intraocular pressure (IOP) in the right eye. The investigation of the right fundus revealed optic disc swelling, macular star lipid (hard exudates) deposition, and peripapillary vascular sheathing (Figure 1). The examination of the left eye proved to be fully normal. Many tests were performed for the patient, including the erythrocyte sedimentation rate (ESR), complete blood count differential (CBC diff.), C-reactive protein (CRP), toxoplasmosis serology, purified protein derivative (PPD), angiotensin converting enzyme (ACE), FTA-ABS, brain and orbital MRI, chest x-ray, and infectious and rheumatologic consultation. Bartonella henselae serology was not available in our ophthalmology center, nor in any other nearby neighborhood.
Figure 1. Fundus Photograph of the Right Eye on Presentation.

Based on our clinical results, neuroretinitis etiology revealed CSD as the most common infectious etiology, along with the negative systemic and ocular history, and empirical treatment commenced including azithromycin 500 mg daily, trimethoprim/sulfamethoxazole, and the application of a topical steroid.
After 72 hours, all the above-mentioned laboratory indices returned to the normal level, except for the toxoplasmosis serology. Furthermore, the serologic test for toxoplasmosis was negative for IgM antibody whereas the IgG antibody titer was > 100 IU/mL. Relying on the positive IgG toxoplasmosis serology and the absence of any response to initial treatment, we embarked on shifting to classic anti-toxoplasmosis treatment, i.e., sulfadiazine 500 mg qid (four times a day), pyrimethamine 50 mg/day, and folinic acid. After 72 hours had passed, prednisolone 1mg/kg/day was added and thereafter tapered during the treatment.
The disc edema diminished over the course of a week. Also, visual acuity gradually improved and the A/C inflammatory reaction faded away. After the decrease in disc swelling, a very small hyperpigmented focus appeared in the juxtapapillary position. The patient then received a 6-week course of toxoplasmosis treatment. Gradually, over the next two months, the patient’s visual acuity improved to 9/10 and the optic disc swelling and macular exudates resolved (Figure 2).
Figure 2. Fundus Photograph After Treatment.
3. Discussion
The clinical syndrome of idiopathic stellate maculopathy accompanied by optic nerve edema was first identified by Leber in 1916 (5). Later on, this syndrome was renamed as Leber’s stellate neuroretinitis. As is now known, the most common form of infectious NR results from CSD (1). The engagement of the optic nerve suggests the need for urgent intervention. In spite of the lack of evidence either for animal exposure or any other systemic condition for this case, empirical CSD treatment was instituted as lab tests were pending and given that cat scratch serology was not accessible.
Toxoplasmosic retinochoroiditis is rendered as one of the most frequent causes of posterior uveitis, specifically in young patients (6). However, toxoplasmic optic neuropathy is an infrequent condition and is often characterized by subacute visual loss and optic nerve swelling, and is sometimes associated with a macular star (neuroretinitis) (7). The engagement of the optic nerve most commonly encountered in ocular toxoplasmosis is optic nerve edema with a simultaneous distant active lesion. Also, juxtapapillary retinochoroiditis is ranked as the second most common type of lesion. Other types of optic nerve involvement include pure papillitis presented as optic disc swelling, associated with peripapillary vascular sheathing close to the healed lesion, and neuroretinitis, i.e., optic disc swelling with macular hard exudate deposition. Additionally, monocular involvement has been observed in most cases with favorable visual prognosis (8).
Considering the positive toxoplasmosis serology in this patient, toxoplasmosis neuroretinitis was suspected, hence prompting the specified treatment. This case disclosed optic disc involvement and neuroretinitis owing to juxtapapillary chorioretinitis reactivation. In some cases, the juxtapapillary chorioretinal scar cannot be found in the acute stage of disease due to disc and peripapillary edema.
Although toxoplasmosis neuroretinitis is rare, it should be still considered in any suspected case of neuroretinitis. This case re-emphasizes the necessity of considering toxoplasmosis in the differential diagnosis of neuroretinitis. Awareness of this potential cause and prompt treatment after positive testing may therefore result in a good visual outcome.
Footnotes
Authors’ Contribution:Nasser Shoeibi prepared the manuscript, helped in the follow-up examinations of the patient and the acquisition of data, and finally revised the manuscript. Seyedeh Maryam Hosseini developed the original idea, revised the manuscript, supervised the treatment, and served as guarantor. Razie Bayani helped in the follow ups of the patient and the acquisition of the data, and abstracted the findings.
References
- 1.Purvin V, Sundaram S, Kawasaki A. Neuroretinitis: review of the literature and new observations. J Neuroophthalmol. 2011;31(1):58–68. doi: 10.1097/WNO.0b013e31820cf78a. [DOI] [PubMed] [Google Scholar]
- 2.Suhler EB, Lauer AK, Rosenbaum JT. Prevalence of serologic evidence of cat scratch disease in patients with neuroretinitis. Ophthalmology. 2000;107(5):871–6. doi: 10.1016/s0161-6420(00)00002-6. [DOI] [PubMed] [Google Scholar]
- 3.Kosmorsky GS, Prayson R. Primary optic pathway sarcoidosis in a 38-year-old white man. J Neuroophthalmol. 1996;16(3):188–90. [PubMed] [Google Scholar]
- 4.Matsuda A, Chin S, Ohashi T. A case of neuroretinitis associated with long-standing polyarteritis nodosa. Ophthalmologica. 1994;208(3):168–71. doi: 10.1159/000310477. [DOI] [PubMed] [Google Scholar]
- 5.Leber T. Die pseudonephritischen Netzhauterkrankungen, die Retinitis stellata: Die Purtschersche Netzhautaffektion nack schwerer Schadelverletzung [in German]. In: Graefe AC, Saemische T, editors. Graefe-Saemisch Handbuch der Augerheilkunde. 2 ed. Leipzig, Germany: Engelmann; 1916. p. 1319. [Google Scholar]
- 6.Khairallah M, Yahia SB, Zaouali S, Jenzeri S, Attia S, Messaoud R. Acute choroidal ischemia associated with toxoplasmic retinochoroiditis. Retina. 2007;27(7):947–51. doi: 10.1097/IAE.0b013e3180653d0d. [DOI] [PubMed] [Google Scholar]
- 7.Eckert GU, Melamed J, Menegaz B. Optic nerve changes in ocular toxoplasmosis. Eye (Lond). 2007;21(6):746–51. doi: 10.1038/sj.eye.6702319. [DOI] [PubMed] [Google Scholar]
- 8.Alipanahi R, Sayyahmelli S. Acute papillitis in young female with toxoplasmosis. Middle East Afr J Ophthalmol. 2011;18(3):249–51. doi: 10.4103/0974-9233.84060. [DOI] [PMC free article] [PubMed] [Google Scholar]


